Heterogeneity of Endocrinologic and Metabolic Parameters in Reproductive Age Polycystic Ovary Syndrome (PCOS) Women Concerning the Severity of Hyperandrogenemia—A New Insight on Syndrome Pathogenesis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Assays
2.3. Studied Subgroups
2.4. Statistical Analysis
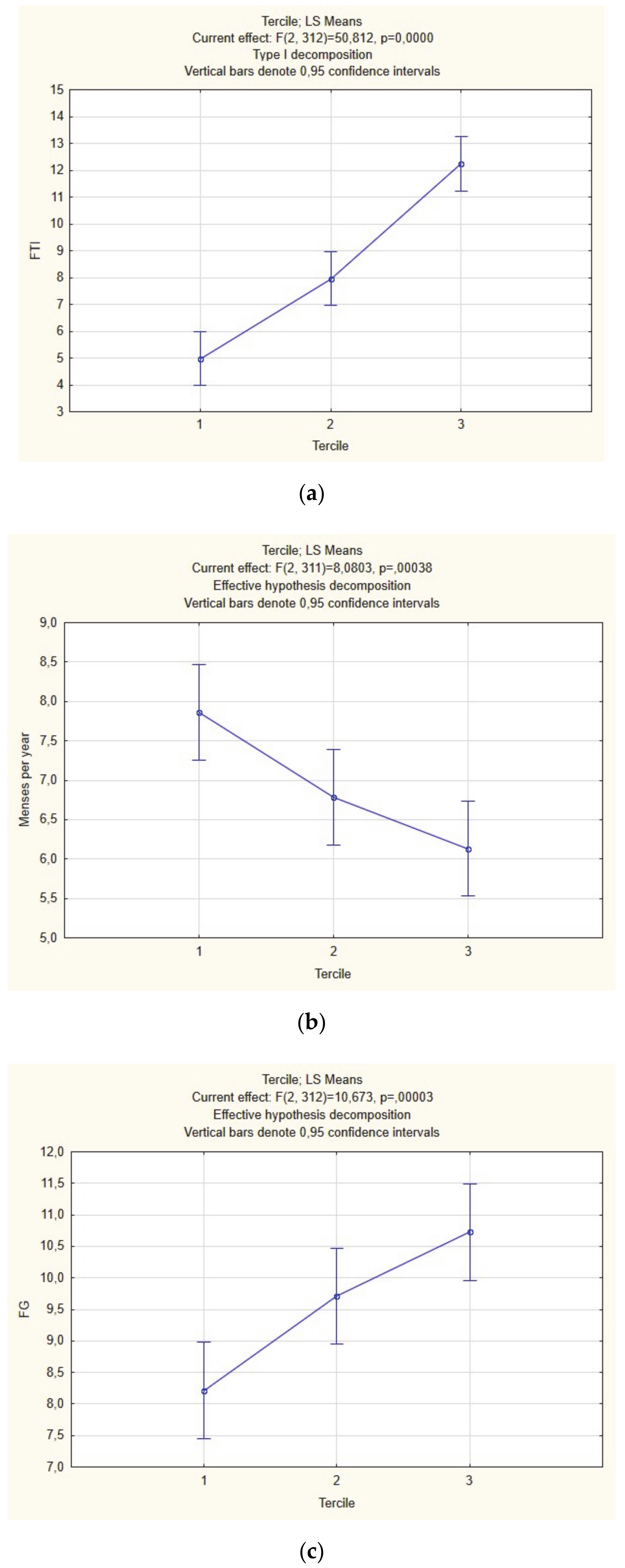
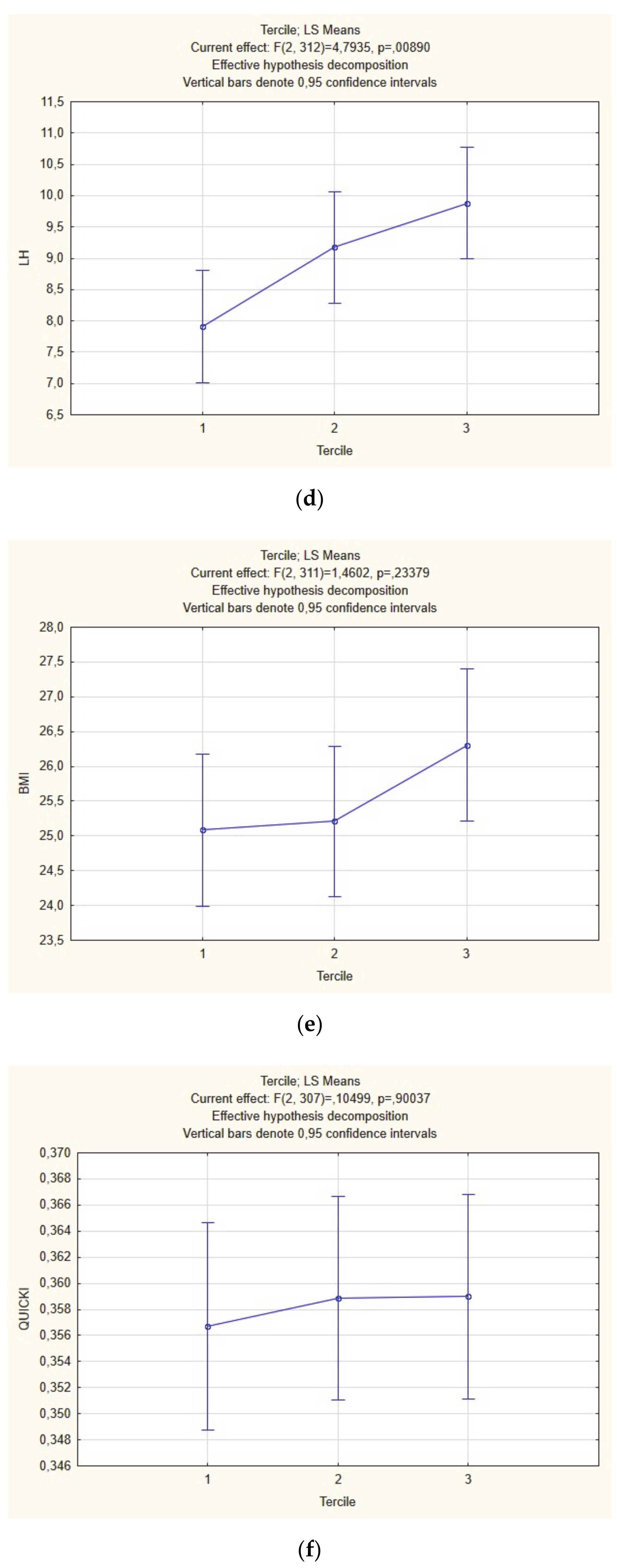
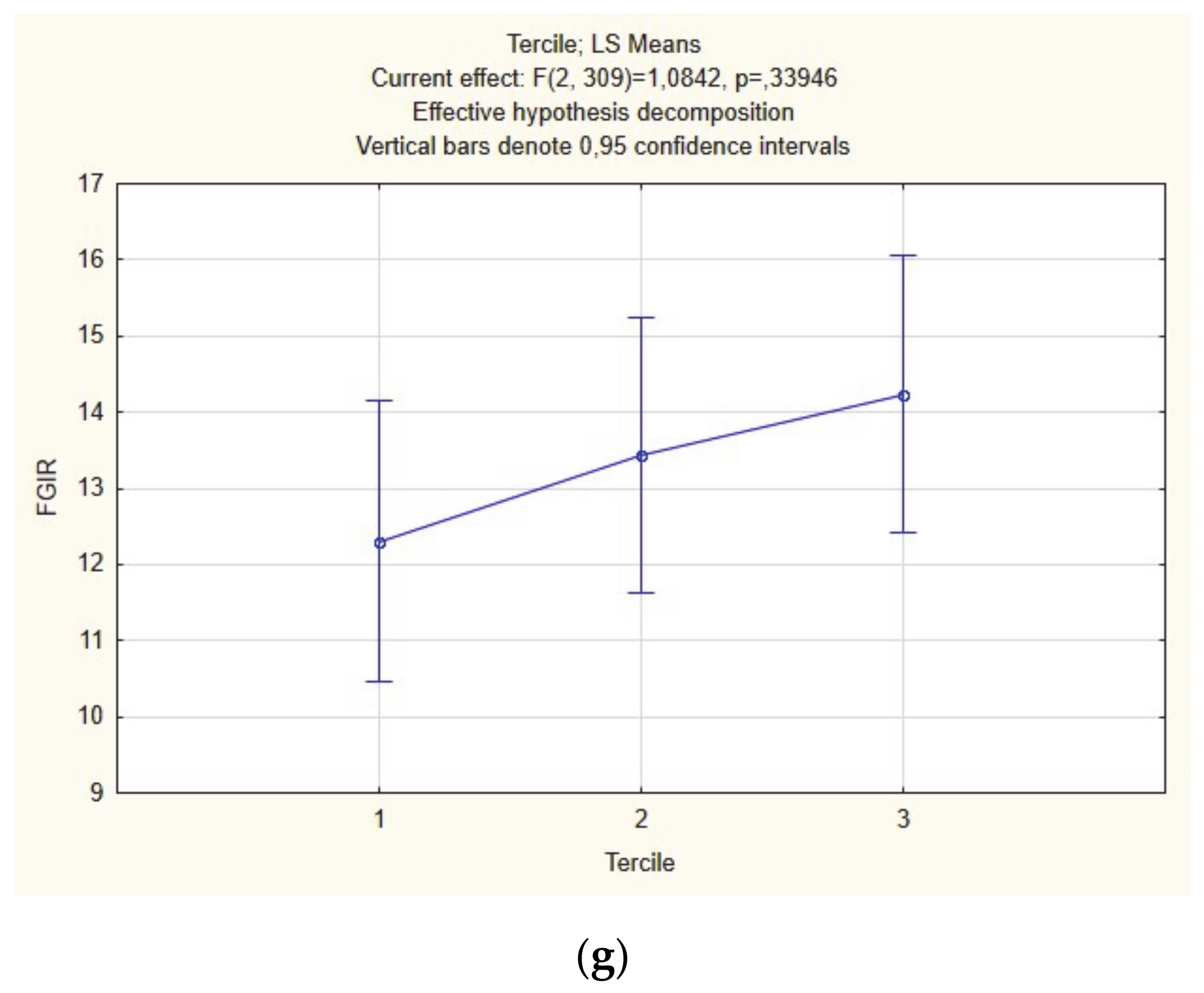
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Goodarzi, M.O.; Dumesic, D.A.; Chazenbalk, G.; Azziz, R. Polycystic ovary syndrome: Etiology, pathogenesis and diagnosis. Nat. Rev. Endocrinol. 2011, 7, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Diamanti-Kandarakis, E.; Kouli, C.R.; Bergiele, A.T.; Filandra, F.A.; Tsianateli, T.C.; Spina, G.G.; Zapanti, E.D.; Bartzis, M.I. A survey of the polycystic ovary syndrome in the Greek island of Lesbos: Hormonal and metabolic profile. J. Clin. Endocrinol. Metab. 1999, 84, 4006–4011. [Google Scholar] [CrossRef] [PubMed]
- Mikolajczyk, R.; Rauchfuss, M.; Lamm, D. Unplanned pregnancies in a developed society--a study on a maternity ward in Berlin. Zentralbl. Gynakol. 2001, 123, 578–584. [Google Scholar] [CrossRef] [PubMed]
- March, W.A.; Moore, V.M.; Willson, K.J.; Phillips, D.I.W.; Norman, R.J.; Davies, M.J. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum. Reprod. 2010, 25, 544–551. [Google Scholar] [CrossRef]
- Ma, Y.M.; Li, R.; Qiao, J.; Zhang, X.W.; Wang, S.Y.; Zhang, Q.F.; Li, L.; Tu, B.B.; Zhang, X. Characteristics of abnormal menstrual cycle and polycystic ovary syndrome in community and hospital populations. Chin. Med. J. 2010. [Google Scholar] [CrossRef]
- Boyle, J.A.; Cunningham, J.; O’Dea, K.; Dunbar, T.; Norman, R.J. Prevalence of polycystic ovary syndrome in a sample of Indigenous women in Darwin, Australia. Med. J. Aust. 2011, 196, 62–66. [Google Scholar] [CrossRef]
- Azziz, R.; Carmina, E.; Dewailly, D.; Diamanti-Kandarakis, E.; Escobar-Morreale, H.F.; Futterweit, W.; Janssen, O.E.; Legro, R.S.; Norman, R.J.; Taylor, A.E.; et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: The complete task force report. Fertil. Steril. 2009, 91, 456–488. [Google Scholar] [CrossRef]
- Asuncion, M.; Calvo, R.M.; San Millan, J.L.; Sancho, J.; Avila, S.; Escobar-Morreale, H.F. A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. J. Clin. Endocrinol. Metab. 2000, 85, 2434–2438. [Google Scholar] [CrossRef]
- Wild, R.A.; Carmina, E.; Diamanti-Kandarakis, E.; Dokras, A.; Escobar-Morreale, H.F.; Futterweit, W.; Lobo, R.; Norman, R.J.; Talbott, E.; Dumesic, A.D. Assessment of Cardiovascular Risk and Prevention of Cardiovascular Disease in Women with the Polycystic Ovary Syndrome: A Consensus Statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. J. Clin. Endocrinol. Metab. 2010, 95, 2038–2049. [Google Scholar] [CrossRef]
- Moran, L.J.; Misso, M.L.; Wild, R.A.; Norman, R.J. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. Update 2010, 16, 347–363. [Google Scholar] [CrossRef]
- Dunaif, A. Insulin resistance and the polycystic ovary syndrome: Mechanism and implications for pathogenesis. Endocr. Rev. 1997, 18, 774–800. [Google Scholar] [CrossRef] [PubMed]
- Azziz, R.; Carmina, E.; Dewailly, D.; Diamanti-Kandarakis, E.; Escobar-Morreale, H.F.; Futterweit, W.; Janssen, O.E.; Legro, R.S.; Norman, R.J.; Taylor, A.E.; et al. Position statement: Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: An androgen excess society guideline. J. Clin. Endocrinol. Metab. 2006. [Google Scholar] [CrossRef] [PubMed]
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. 2004, 19, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Ozegowska, K.; Pawelczyk, L. Cardiometabolic risk in patients with polycystic ovary syndrome. Ginekol. Pol. 2015, 86. [Google Scholar] [CrossRef] [PubMed]
- Boomsma, C.M.; Eijkemans, M.J.C.; Hughes, E.G.; Visser, G.H.A.; Fauser, B.C.J.M.; Macklon, N.S. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum. Reprod. Update 2006, 12, 673–683. [Google Scholar] [CrossRef]
- Palomba, S.; Falbo, A.; Russo, T.; Tolino, A.; Orio, F.; Zullo, F. Pregnancy in women with polycystic ovary syndrome: The effect of different phenotypes and features on obstetric and neonatal outcomes. Fertil. Steril. 2010, 94, 1805–1811. [Google Scholar] [CrossRef]
- Palomba, S.; De Wilde, M.A.; Falbo, A.; Koster, M.P.H.; La Sala, G.B.; Fauser, B.C.J.M. Pregnancy complications in women with polycystic ovary syndrome. Hum. Reprod. Update 2015, 21, 575–592. [Google Scholar] [CrossRef]
- Fica, S.; Albu, A.; Constantin, M.; Dobri, G.A. Insulin resistance and fertility in polycystic ovary syndrome. J. Med. Life 2008, 1, 415–422. [Google Scholar]
- Legro, R.S.; Kunselman, A.R.; Dunaif, A. Prevalence and predictors of dyslipidemia in women with polycystic ovary syndrome. Am. J. Med. 2001, 111, 607–613. [Google Scholar] [CrossRef]
- Carmina, E.; Orio, F.; Palomba, S.; Cascella, T.; Longo, R.A.; Colao, A.M.; Lombardi, G.; Lobo, R.A. Evidence for altered adipocyte function in polycystic ovary syndrome. Eur. J. Endocrinol. 2005, 152, 389–394. [Google Scholar] [CrossRef]
- Palomba, S.; Santagni, S.; Falbo, A.; La Sala, G.B. Complications and challenges associated with polycystic ovary syndrome: Current perspectives. Int. J. Womens Health 2015, 7, 745–763. [Google Scholar] [CrossRef] [PubMed]
- Ovalle, F.; Azziz, R. Insulin resistance, polycystic ovary syndrome, and type 2 diabetes mellitus. Fertil. Steril. 2002, 77, 1095–1105. [Google Scholar] [CrossRef]
- Amiri, M.; Ramezani Tehrani, F.; Behboudi-Gandevani, S.; Bidhendi-Yarandi, R.; Carmina, E. Risk of hypertension in women with polycystic ovary syndrome: A systematic review, meta-analysis and meta-regression. Reprod. Biol. Endocrinol. 2020, 18, 23. [Google Scholar] [CrossRef]
- Ramezani Tehrani, F.; Montazeri, S.A.; Hosseinpanah, F.; Cheraghi, L.; Erfani, H.; Tohidi, M.; Azizi, F. Trend of Cardio-Metabolic Risk Factors in Polycystic Ovary Syndrome: A Population-Based Prospective Cohort Study. PLoS ONE 2015, 10, e0137609. [Google Scholar] [CrossRef]
- Loverro, G.; Lorusso, F.; Mei, L.; Depalo, R.; Cormio, G.; Selvaggi, L. The plasma homocysteine levels are increased in polycystic ovary syndrome. Gynecol. Obstet. Investig. 2002, 53, 157–162. [Google Scholar] [CrossRef]
- Wild, S.; Pierpoint, T.; McKeigue, P.; Jacobs, H. Cardiovascular disease in women with polycystic ovary syndrome at long-term follow-up: A retrospective cohort study. Clin. Endocrinol. 2000, 52, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Carmina, E.; Koyama, T.; Chang, L.; Stanczyk, F.Z.; Lobo, R.A. Does ethnicity influence the prevalence of adrenal hyperandrogenism and insulin resistance in polycystic ovary syndrome? Int. J. Gynecol. Obstet. 1993. [Google Scholar] [CrossRef]
- DeUgarte, C.M.; Bartolucci, A.A.; Azziz, R. Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil. Steril. 2005. [Google Scholar] [CrossRef] [PubMed]
- Legro, R.S.; Castracane, V.D.; Kauffman, R.P. Detecting Insulin Resistance in Polycystic Ovary Syndrome: Purposes and Pitfalls. Obstet. Gynecol. Surv. 2004. [Google Scholar] [CrossRef] [PubMed]
- Nestler, J.E. Role of hyperinsulinemia in the pathogenesis of the polycystic ovary syndrome, and its clinical implications. Semin. Reprod. Endocrinol. 1997, 15, 111–122. [Google Scholar] [CrossRef]
- Wood, J.R.; Dumesic, D.A.; Abbott, D.H.; Strauss, J.F. Molecular abnormalities in oocytes from women with polycystic ovary syndrome revealed by microarray analysis. J. Clin. Endocrinol. Metab. 2007. [Google Scholar] [CrossRef] [PubMed]
- Dumesic, D.A.; Abbott, D.H. Implications of polycystic ovary syndrome on oocyte development. Semin. Reprod. Med. 2008. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brewer, C.J.; Balen, A.H. The adverse effects of obesity on conception and implantation. Reproduction 2010, 140, 347–364. [Google Scholar] [CrossRef] [PubMed]
- Giudice, L.C. Endometrium in PCOS: Implantation and predisposition to endocrine CA. Best Pract. Res. Clin. Endocrinol. Metab. 2006, 20, 235–244. [Google Scholar] [CrossRef]
- Legro, R.S.; Finegood, D.; Dunaif, A. A fasting glucose to insulin ratio is a useful measure of insulin sensitivity in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1998. [Google Scholar] [CrossRef]
- Katz, A.; Nambi, S.S.; Mather, K.; Baron, A.D.; Follmann, D.A.; Sullivan, G.; Quon, M.J. Quantitative insulin sensitivity check index: A simple, accurate method for assessing insulin sensitivity in humans. J. Clin. Endocrinol. Metab. 2000, 85, 2402–2410. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Azziz, R. Androgen excess is the key element in polycystic ovary syndrome. Fertil. Steril. 2003, 80, 252–254. [Google Scholar] [CrossRef]
- Walters, K.A.; Paris, V.R.; Aflatounian, A.; Handelsman, D.J. Androgens and ovarian function: Translation from basic discovery research to clinical impact. J. Endocrinol. 2019, 242, R23–R50. [Google Scholar] [CrossRef]
- Jeanes, Y.M.; Reeves, S. Metabolic consequences of obesity and insulin resistance in polycystic ovary syndrome: Diagnostic and methodological challenges. Nutr. Res. Rev. 2017, 30, 97–105. [Google Scholar] [CrossRef]
- Poretsky, L.; Cataldo, N.A.; Rosenwaks, Z.; Giudice, L.C. The insulin-related ovarian regulatory system in health and disease. Endocr. Rev. 1999, 20, 535–582. [Google Scholar] [CrossRef] [PubMed]
- Wallace, I.R.; McKinley, M.C.; Bell, P.M.; Hunter, S.J. Sex hormone binding globulin and insulin resistance. Clin. Endocrinol. 2013. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, R.L. The diagnosis of polycystic ovary syndrome in adolescents. Pediatrics 2015, 136, 1154–1165. [Google Scholar] [CrossRef] [PubMed]
- Lewy, V.D.; Danadian, K.; Witchel, S.F.; Arslanian, S. Early metabolic abnormalities in adolescent girls with polycystic ovarian syndrome. J. Pediatr. 2001, 138, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Goodarzi, M.O.; Carmina, E.; Azziz, R. DHEA, DHEAS and PCOS. J. Steroid Biochem. Mol. Biol. 2015, 145, 213–225. [Google Scholar] [CrossRef]
- Macut, D.; Antić, I.B.; Nestorov, J.; Topalović, V.; Macut, J.B.; Panidis, D.; Kotlica, B.K.; Papadakis, E.; Matić, G.; Milutinović, D.V. The influence of combined oral contraceptives containing drospirenone on hypothalamic-pituitary-adrenocortical axis activity and glucocorticoid receptor expression and function in women with polycystic ovary syndrome. Hormones 2015, 14, 109–117. [Google Scholar] [CrossRef]
- Vettor, R.; Macor, C.; Novo, F.; Gottardo, C.; Zovato, S.; Simoncini, M.; Federspil, G.; Armanini, D. Corticosteroid receptors in mononuclear leucocytes of obese subjects. J. Endocrinol. 1998, 156, 187–194. [Google Scholar] [CrossRef][Green Version]
- Cheng, T.; Dimitrov, S.; Pruitt, C.; Hong, S. Glucocorticoid mediated regulation of inflammation in human monocytes is associated with depressive mood and obesity. Psychoneuroendocrinology 2016, 66, 195–204. [Google Scholar] [CrossRef]
- O’Shaughnessy, P.J.; Antignac, J.P.; Le Bizec, B.; Morvan, M.L.; Svechnikov, K.; Söder, O.; Savchuk, I.; Monteiro, A.; Soffientini, U.; Johnstonid, Z.C.; et al. Alternative (Backdoor) androgen production and masculinization in the human fetus. PLoS Biol. 2019, 17, e3000002. [Google Scholar] [CrossRef]
- Ehrmann, D.A.; Rosenfield, R.L.; Barnes, R.B.; Brigell, D.F.; Sheikh, Z. Detection of functional ovarian hyperandrogenism in women with androgen excess. Obstet. Gynecol. Surv. 1992, 327, 157–162. [Google Scholar] [CrossRef]
- Carey, A.H.; Waterworth, D.; Patel, K.; White, D.; Little, J.; Novelli, P.; Franks, S.; Williamson, R. Polycystic ovaries and premature male pattern baldness are associated with one allele of the steroid metabolism gene CYP17. Hum. Mol. Genet. 1994, 3, 1873–1876. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, F.; Luo, S.; Hu, H.; Li, X.H.; Li, S.W. Polymorphism T→C of gene CYP17 promoter and polycystic ovary syndrome risk: A meta-analysis. Gene 2012, 495, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Ajmal, N.; Khan, S.Z.; Shaikh, R. Polycystic ovary syndrome (PCOS) and genetic predisposition: A review article. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2019, 3. [Google Scholar] [CrossRef] [PubMed]
- Diamanti-Kandarakis, E.; Papavassiliou, A.G.; Kandarakis, S.A.; Chrousos, G.P. Pathophysiology and types of dyslipidemia in PCOS. Trends Endocrinol. Metab. 2007, 18, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Sidhwani, S.; Scoccia, B.; Sunghay, S.; Stephens-Archer, C.N.; Mazzone, T.; Sam, S. Polycystic ovary syndrome is associated with atherogenic changes in lipoprotein particle number and size independent of body weight. Clin. Endocrinol. 2011, 75, 76–82. [Google Scholar] [CrossRef]
- Moran, L.J.; Mundra, P.A.; Teede, H.J.; Meikle, P.J. The association of the lipidomic profile with features of polycystic ovary syndrome. J. Mol. Endocrinol. 2017, 59, 93–104. [Google Scholar] [CrossRef]
- Coyle, C.; Campbell, R.E. Pathological pulses in PCOS. Mol. Cell. Endocrinol. 2019, 498, 11056. [Google Scholar] [CrossRef]
- Blank, S.K.; McCartney, C.R.; Marshall, J.C. The origins and sequelae of abnormal neuroendocrine function in polycystic ovary syndrome. Hum. Reprod. Update 2006, 12, 351–361. [Google Scholar] [CrossRef]
- Chhabra, S.; McCartney, C.R.; Yoo, R.Y.; Eagleson, C.A.; Chang, R.J.; Marshall, J.C. Progesterone inhibition of the hypothalamic gonadotropin-releasing hormone pulse generator: Evidence for varied effects in hyperandrogenemic adolescent girls. J. Clin. Endocrinol. Metab. 2005, 90, 2810–2815. [Google Scholar] [CrossRef]
- McGee, W.K.; Bishop, C.V.; Bahar, A.; Pohl, C.R.; Chang, R.J.; Marshall, J.C.; Pau, F.K.; Stouffer, R.L.; Cameron, J.L. Elevated androgens during puberty in female rhesus monkeys lead to increased neuronal drive to the reproductive axis: A possible component of polycystic ovary syndrome. Am. J. Physiol. Endocrinol. Metab. 2014, 306, E1292–E1304. [Google Scholar] [CrossRef]
- Bishop, C.V.; Mishler, E.C.; Takahashi, D.L.; Reiter, T.E.; Bond, K.R.; True, C.A.; Slayden, O.D.; Stouffer, R.L. Chronic hyperandrogenemia in the presence and absence of a western-style diet impairs ovarian and uterine structure/function in young adult rhesus monkeys. Hum. Reprod. 2018, 33, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Franks, S.; McCarthy, M.I.; Hardy, K.; Skakkebæk, N.E.; Aitken, R.J.; Swan, S.; De Muinck Keizer-Schrama, S. Development of polycystic ovary syndrome: Involvement of genetic and environmental factors. Int. J. Androl. 2006, 29, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, S.S.; Beverley, R.; Barnard, E.; Baradaran-Shoraka, M.; Sanfilippo, J.S. Polycystic ovary syndrome in adolescents. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 48, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Zumoff, B.; Freeman, R.; Coupey, S.; Saenger, P.; Markowitz, M.; Kream, J. A Chronobiologic Abnormality in Luteinizing Hormone Secretion in Teenage Girls with the Polycystic-Ovary Syndrome. N. Engl. J. Med. 1983, 309, 1206–1209. [Google Scholar] [CrossRef] [PubMed]
- Barnes, R.B.; Rosenfield, R.L.; Ehrmann, D.A.; Cara, J.F.; Cuttler, L.; Levitsky, L.L.; Rosenthal, I.M. Ovarian hyperandrogynism as a result of congenital adrenal virilizing disorders: Evidence for perinatal masculinization of neuroendocrine function in women. J. Clin. Endocrinol. Metab. 1994, 79, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, S.; Sirisha, P.V.S.; Neelaveni, K.; Anuradha, K.; Sudhakar, G.; Reddy, B.M. Role of luteinizing hormone β-subunit gene variants among South Indian women with polycystic ovary syndrome. Gene 2012, 494, 51–56. [Google Scholar] [CrossRef]
- Pisprasert, V.; Ingram, K.H.; Lopez-Davila, M.F.; Munoz, A.J.; Garvey, W.T. Limitations in the use of indices using glucose and insulin levels to predict insulin sensitivity: Impact of race and gender and superiority of the indices derived from oral glucose tolerance test in African Americans. Diabetes Care 2013, 36, 845–853. [Google Scholar] [CrossRef]
- Ozegowska, K.; Bogacz, A.; Bartkowiak-Wieczorek, J.; Seremak-Mrozikiewicz, A.; Pawelczyk, L. Is there an association between the development of metabolic syndrome in PCOS patients and the C677T MTHFR gene polymorphism? Ginekol. Pol. 2016, 87, 246–253. [Google Scholar] [CrossRef]
- Ozegowska, K.E.; Pawelczyk, L.A. The role of insulin and selected adipocytokines in patients with polycystic ovary syndrome (PCOS)—A literature review. Ginekol. Pol. 2015, 86. [Google Scholar] [CrossRef]
| Variable | PCOS (n = 694) |
|---|---|
| Age (years) | 27.0 (24.0–31.0) |
| T (ng/mL) | 0.54 (0.39–0.75) |
| Insulin | 7.86 (5.30–11.97) |
| Glucose | 88.0 (82.0–94.2) |
| HOMA-IR | 1.74 (1.10–2.68) |
| FTI | 4.90 (2.738.23) |
| MPR | 7.0 (5.0–9.0) |
| FG | 9.0 (4.0–11.0) |
| BMI (kg/m2) | 24.2 (21.3–29.1) |
| LH (mIU/mL) | 7.94 (5.49–11.42) |
| DHEA-S (umol/L) | 6.01 (3.49–8.85) |
| FGIR | 11.07 (7.42–16.27) |
| QUCIKI | 0.35 (0.33–0.38) |
| CHOL (mg/dL) | 182.0 (161.6–205.0) |
| HDL (mg/dL) | 60.45 (49.90–72.00) |
| TG (mg/dL) | 76.5 (58.0–110.0) |
| LDL (mg/dL) | 103.0 (85.0–123.6) |
| TC/HDL | 2.98 (2.43–3.66) |
| TG/HDL | 1.21 (0.86–2.10) |
| Variable | Group 1 (n = 294) | Group 2 (n = 261) | Group 3 (n = 139) | p# |
|---|---|---|---|---|
| Age (years) | 27.5 (24.0–31.0) | 27.0 (24.0–31.0) | 27.0 (24,0–30.0) | 0.66 |
| Insulin | 7.6 (5.3–11.0) | 8.4 (5.4–12.6) | 7.8 (5.2–13.2) | 0.25 |
| Glucose | 88.0 (82.0–94.0) | 88.6 (83.0–95.0) | 89.0 (81.0–95.0) | 0.46 |
| HOMA-IR | 1.7 (1.1–2.4) | 1.8 (1.1–2.8) | 1.7 (1.1–2.9) | 0.24 |
| FTI | 2.7 (1.6–4.5) | 5.7 (3.9–8.6) | 10.1 (6.1–15.5) | <0.000001 |
| MPR | 9.6 (7.0–12.0) | 7.1 (5.0–9.0) | 7.0 (4.0–8.0) | <0.00001 |
| FG | 5.0 (1.0–10.0) | 9.0 (7.0–11.0) | 10.0 (8.0–12.0) | <0.000001 |
| BMI (kg/m2) | 23.7 (20.8–28.2) | 25.0 (21.6–30.0) | 24.1 (21.6–30.1) | 0.03 |
| LH (mIU/mL) | 6.8 (5.2–9.9) | 8.4 (5.7–11.8) | 9.6 (6.4–13.3) | <0.000001 |
| DHEA-S (umol/L) | 4.4 (1.1–6.50 | 6.8 (4.0–9.2) | 9.7 (6.8–12.4) | <0.000001 |
| FGIR | 11.6 (8.1–16.3) | 10.7 (7.0–15.9) | 10.9 (6.9–16.6) | 0.23 |
| QUCIKI | 0.2 (0.3–0.4) | 0.4 (0.3–0.4) | 0.4 (0.3–0.4) | 0.22 |
| CHOL (mg/dL) | 178.8 (157.0–204.0) | 184.4 (165.3–204.3) | 184.9 (164.1–208.0) | 0.1 |
| HDL (mg/dL) | 60.6 (49.0–72.0) | 60.2 (49.8–72.5) | 60.6 (50.1–71.3) | 0.9 |
| TG (mg/dL) | 73.0 (57.7–105.5) | 78.3 (60.2–117.2) | 77.7 (55.9–105.3) | 0.49 |
| LDL (mg/dL) | 101.0 (85.8–122.0) | 103.0 (85.0–122.0) | 108.0 (79.3–126.4) | 0.75 |
| TC/HDL | 2.95 (2.4–3.6) | 3.0 (2.4–3.7) | 3.0 (2.4–3.6) | 0.56 |
| TG/HDL | 1.2 (0.9–2.0) | 1.3 (0.9–2.2) | 1.2 (0.9–2.0) | 0.54 |
| Variable | # | T | FTI | MPR | FG | BMI | LH | DHEA | FGIR | QUICKI | Chol | HDL | LDL | TC/HDL | TG | HOMA-IR | TG/HDL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T (ng/mL) | r | 0.626 | −0.355 | 0.326 | 0.105 | 0.188 | 0.518 | 0.001 | −0.021 | 0.054 | −0.017 | 0.012 | 0.061 | 0.046 | 0.05 | 0.035 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.0058 | <0.0001 | <0.0001 | 0.97 | 0.5914 | 0.1577 | 0.6614 | 0.7474 | 0.1111 | 0.2247 | 0.19 | 0.36 | ||
| FTI | r | 0.626 | −0.238 | 0.304 | 0.377 | 0.012 | 0.366 | −0.204 | −0.271 | 0.05 | −0.266 | 0.089 | 0.271 | 0.258 | 0.322 | 0.32 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.7431 | <0.0001 | <0.0001 | <0.0001 | 0.1871 | <0.0001 | 0.0201 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| MPR | r | −0.355 | −0.238 | −0.106 | −0.061 | −0.121 | −0.175 | −0.033 | −0.011 | −0.116 | 0.039 | −0.103 | −0.093 | −0.087 | −0.006 | −0.13 | |
| p | <0.0001 | <0.0001 | 0.0241 | 0.1942 | 0.0097 | 0.0002 | 0.4904 | 0.8139 | 0.0139 | 0.4096 | 0.0286 | 0.0491 | 0.0658 | 0.89 | <0.01 | ||
| FG | r | 0.326 | 0.304 | −0.106 | 0.157 | 0.013 | −0.004 | −0.051 | −0.107 | 0.227 | −0.04 | 0.169 | 0.159 | 0.096 | 0.104 | 0.029 | |
| p | <0.0001 | <0.0001 | 0.0241 | <0.0001 | 0.7234 | 0.9238 | 0.1822 | 0.0051 | <0.0001 | 0.3001 | <0.0001 | <0.0001 | 0.0116 | 0.007 | 0.45 | ||
| BMI (kg/m2) | r | 0.105 | 0.377 | −0.061 | 0.157 | −0.176 | −0.029 | −0.445 | −0.556 | 0.181 | −0.449 | 0.294 | 0.492 | 0.402 | 0.587 | 0.523 | |
| p | 0.0058 | <0.0001 | 0.1942 | <0.0001 | <0.0001 | 0.4451 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| LH (mIU/mL) | r | 0.188 | 0.012 | −0.121 | 0.013 | −0.176 | 0.069 | 0.091 | 0.106 | −0.004 | 0.172 | −0.084 | −0.133 | −0.065 | −0.156 | −0.174 | |
| p | <0.0001 | 0.7431 | 0.0097 | 0.7234 | <0.0001 | 0.0715 | 0.0169 | 0.0056 | 0.9082 | <0.0001 | 0.027 | 0.0005 | 0.088 | <0.0001 | <0.0001 | ||
| DHEA-S (umol/L) | r | 0.518 | 0.366 | −0.175 | −0.004 | 0.069 | 0.013 | 0.023 | −0.062 | −0.002 | −0.068 | −0.028 | −0.051 | −0.0023 | −0.018 | ||
| p | <0.0001 | <0.0001 | 0.0002 | 0.9238 | 0.4451 | 0.0715 | 0.7247 | 0.5467 | 0.1057 | 0.961 | 0.0764 | 0.4696 | 0.1815 | 0.54 | 0.63 | ||
| FGIR | r | 0.001 | −0.204 | −0.033 | −0.051 | −0.445 | 0.091 | 0.013 | 0.903 | −0.087 | 0.326 | −0.176 | −0.319 | −0.281 | −0.94 | −0.48 | |
| p | 0.97 | <0.0001 | 0.4904 | 0.1822 | <0.0001 | 0.0169 | 0.7247 | <0.0001 | 0.0232 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| QUICKI | r | −0.021 | −0.271 | −0.011 | −0.107 | −0.556 | 0.106 | 0.023 | 0.903 | −0.146 | 0.386 | −0.239 | −0.408 | −0.379 | −1 | −0.507 | |
| p | 0.5914 | <0.0001 | 0.8139 | 0.0051 | <0.0001 | 0.0056 | 0.5467 | <0.0001 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| Chol (mg/dL) | r | 0.054 | 0.05 | −0.116 | 0.227 | 0.181 | −0.004 | −0.062 | −0.087 | −0.146 | 0.124 | 0.849 | 0.463 | 0.342 | 0.166 | 0.196 | |
| p | 0.1577 | 0.1871 | 0.0139 | <0.0001 | <0.0001 | 0.9082 | 0.1057 | 0.0232 | 0.0001 | 0.0011 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| HDL (mg/dL) | r | −0.017 | −0.266 | 0.039 | −0.04 | −0.449 | 0.172 | −0.002 | 0.326 | 0.386 | 0.124 | −0.232 | −0.752 | −0.437 | −0.428 | −0.777 | |
| p | 0.6614 | <0.0001 | 0.4096 | 0.3001 | <0.0001 | <0.0001 | 0.961 | <0.0001 | <0.0001 | 0.0011 | <0.0001 | <0.0001 | <0.0001 | 0.0001 | <0.001 | ||
| LDL (mg/dL) | r | 0.012 | 0.089 | −0.103 | 0.169 | 0.294 | −0.084 | −0.068 | −0.176 | −0.239 | 0.849 | −0.232 | 0.676 | 0.298 | 0.27 | 0.362 | |
| p | 0.7474 | 0.0201 | 0.0286 | <0.0001 | <0.0001 | 0.027 | 0.0764 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TC/HDL | r | 0.061 | 0.271 | −0.093 | 0.159 | 0.492 | −0.133 | −0.028 | −0.319 | −0.408 | 0.463 | −0.752 | 0.676 | 0.611 | 0.489 | 0.815 | |
| p | 0.1111 | <0.0001 | 0.0491 | <0.0001 | <0.0001 | 0.0005 | 0.4696 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TG (mg/dL) | r | 0.046 | 0.258 | −0.087 | 0.096 | 0.402 | −0.065 | −0.051 | −0.281 | −0.379 | 0.342 | −0.437 | 0.298 | 0.611 | 0.445 | 0.916 | |
| p | 0.2247 | <0.0001 | 0.0658 | 0.0116 | <0.0001 | 0.088 | 0.1815 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| HOMA-IR | r | 0.05 | 0.322 | −0.006 | 0.104 | 0.587 | −0.156 | −0.0023 | −0.94 | −1 | 0.166 | −0.428 | 0.27 | 0.489 | 0.445 | 0.504 | |
| p | 0.19 | <0.0001 | 0.89 | 0.007 | <0.0001 | <0.0001 | 0.54 | <0.0001 | <0.0001 | <0.0001 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TG/HDL | r | 0.035 | 0.32 | −0.13 | 0.029 | 0.523 | −0.174 | −0.018 | −0.48 | −0.507 | 0.196 | −0.777 | 0.362 | 0.815 | 0.916 | 0.504 | |
| p | 0.36 | <0.0001 | <0.01 | 0.45 | <0.0001 | <0.0001 | 0.63 | <0.0001 | <0.0001 | <0.0001 | <0.001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Variable | # | T | FTI | BMI | FGIR | QUICKI | Chol | HDL | LDL | TC/HDL | TG | HOMA-IR | TG/HDL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T (ng/mL) | r | 0.586 | 0.093 | −0.088 | −0.059 | −0.006 | −0.1 | 0.051 | 0.098 | 0.062 | 0.065 | 0.077 | |
| p | <0.0001 | 0.1163 | 0.1315 | 0.3116 | 0.9232 | 0.0856 | 0.3791 | 0.0932 | 0.2901 | 0.2672 | 0.1857 | ||
| FTI | r | 0.586 | 0.433 | −0.417 | −0.417 | 0.076 | −0.428 | 0.22 | 0.458 | 0.294 | 0.419 | 0.395 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.199 | <0.0001 | 0.0002 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| BMI (kg/m2) | r | 0.093 | 0.433 | −0.518 | −0.545 | 0.235 | −0.461 | 0.383 | 0.586 | 0.425 | 0.548 | 0.511 | |
| p | 0.1163 | <0.0001 | <0.0001 | <0.0001 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| FGIR | r | −0.088 | −0.417 | −0.518 | 0.945 | −0.106 | 0.439 | −0.247 | −0.481 | −0.368 | −0.945 | −0.451 | |
| p | 0.1315 | <0.0001 | <0.0001 | <0.0001 | 0.0706 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| QUICKI | r | −0.059 | −0.417 | −0.545 | 0.945 | −0.148 | 0.447 | −0.29 | −0.513 | −0.408 | −1 | −0.48 | |
| p | 0.3116 | <0.0001 | <0.0001 | <0.0001 | 0.0116 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TC (mg/dL) | r | −0.006 | 0.076 | 0.235 | −0.106 | −0.148 | 0.22 | 0.839 | 0.398 | 0.358 | 0.163 | 0.152 | |
| p | 0.9232 | 0.199 | 0.0001 | 0.0706 | 0.0116 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0052 | 0.0092 | ||
| HDL (mg/dL) | r | −0.1 | −0.428 | −0.461 | 0.439 | 0.447 | 0.22 | −0.161 | −0.778 | −0.449 | −0.44 | −0.763 | |
| p | 0.0856 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0001 | 0.0057 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| LDL (mg/dL) | r | 0.051 | 0.22 | 0.383 | −0.247 | −0.29 | 0.839 | −0.161 | 0.686 | 0.384 | 0.303 | 0.351 | |
| p | 0.3791 | 0.0002 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0057 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TC/HDL | r | 0.098 | 0.458 | 0.586 | −0.481 | −0.513 | 0.398 | −0.778 | 0.686 | 0.636 | 0.518 | 0.805 | |
| p | 0.0932 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TG (mg/dL) | r | 0.062 | 0.294 | 0.425 | −0.368 | −0.408 | 0.358 | −0.449 | 0.384 | 0.636 | 0.403 | 0.905 | |
| p | 0.2901 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| HOMA-IR | r | 0.065 | 0.419 | 0.548 | −0.945 | −1 | 0.163 | −0.44 | 0.303 | 0.518 | 0.403 | 0.475 | |
| p | 0.2672 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0052 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TG/HDL | r | 0.077 | 0.395 | 0.511 | −0.451 | −0.48 | 0.152 | −0.763 | 0.351 | 0.805 | 0.905 | 0.475 | |
| p | 0.1857 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0092 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Variable | # | BMI | FGIR | QUICKI | HDL | LDL | TC/HDL | TG | HOMA-IR | TG/HDL |
|---|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | r | −0.578 | −0.621 | −0.451 | 0.246 | 0.515 | 0.48 | 0.605 | 0.535 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| FGIR | r | −0.578 | 0.953 | 0.373 | −0.253 | −0.451 | −0.466 | −0.952 | −0.495 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| QUICKI | r | −0.621 | 0.953 | 0.385 | −0.23 | −0.451 | −0.496 | −1 | −0.521 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.0002 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TC (mg/dL) | r | 0.158 | −0.175 | −0.155 | 0.132 | 0.8 | 0.374 | 0.331 | 0.137 | 0.158 |
| p | 0.0115 | 0.0052 | 0.0134 | 0.0348 | <0.0001 | <0.0001 | <0.0001 | 0.0291 | 0.0112 | |
| HDL (mg/dL) | r | −0.451 | 0.373 | 0.385 | −0.244 | −0.841 | −0.48 | −0.368 | −0.783 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| LDL (mg/dL) | r | 0.246 | −0.253 | −0.23 | −0.244 | 0.678 | 0.309 | 0.229 | 0.334 | |
| p | 0.0001 | <0.0001 | 0.0002 | 0.0001 | <0.0001 | <0.0001 | 0.0002 | <0.0001 | ||
| TC/HDL | r | 0.515 | −0.451 | −0.451 | −0.841 | 0.678 | 0.616 | 0.445 | 0.813 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TG (mg/dL) | r | 0.48 | −0.466 | −0.496 | −0.48 | 0.309 | 0.616 | 0.484 | 0.909 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| HOMA-IR | r | 0.605 | −0.952 | −1 | −0.368 | 0.229 | 0.445 | 0.484 | 0.519 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0002 | <0.0001 | <0.0001 | <0.0001 | ||
| TG/HDL | r | 0.535 | −0.495 | −0.521 | −0.783 | 0.334 | 0.813 | 0.909 | 0.519 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Variable | # | BMI | FGIR | QUICKI | Chol | HDL | LDL | TC/HDL | TG | HOMA-IR | TG/HDL |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | r | −0.647 | −0.643 | 0.117 | −0.59 | 0.283 | 0.544 | 0.431 | 0.637 | 0.544 | |
| p | <0.0001 | <0.0001 | 0.1733 | <0.0001 | 0.0008 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| FGIR | t | −0.647 | 0.908 | −0.145 | 0.486 | −0.24 | −0.453 | −0.433 | −0.907 | −0.5 | |
| p | <0.0001 | <0.0001 | 0.093 | <0.0001 | 0.0048 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| QUICKI | r | −0.643 | 0.908 | −0.202 | 0.516 | −0.278 | −0.504 | −0.459 | −1 | −0.528 | |
| p | <0.0001 | <0.0001 | 0.0183 | <0.0001 | 0.0011 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TC (mg/dL) | r | 0.117 | −0.145 | −0.202 | −0.062 | 0.883 | 0.567 | 0.449 | 0.202 | 0.334 | |
| p | 0.1733 | 0.093 | 0.0183 | 0.4683 | <0.0001 | <0.0001 | <0.0001 | 0.0186 | 0.0001 | ||
| HDL (mg/dL) | r | −0.59 | 0.486 | 0.516 | −0.062 | −0.347 | −0.837 | −0.547 | −0.517 | −0.798 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.4683 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| LDL (mg/dL) | r | 0.283 | −0.24 | −0.278 | 0.883 | −0.347 | 0.749 | 0.43 | 0.277 | 0.443 | |
| p | 0.0008 | 0.0048 | 0.0011 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.0011 | <0.0001 | ||
| TC/HDL | r | 0.544 | −0.453 | −0.504 | 0.567 | −0.837 | 0.749 | 0.683 | 0.504 | 0.832 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| TG (mg/dL) | r | 0.431 | −0.433 | −0.459 | 0.449 | −0.547 | 0.43 | 0.683 | 0.459 | 0.932 | |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| HOMA-IR | r | 0.637 | −0.907 | −1 | 0.202 | −0.517 | 0.277 | 0.504 | 0.459 | 0.529 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.0186 | <0.0001 | 0.0011 | <0.0001 | <0.0001 | <0.0001 | ||
| TG/HDL | r | 0.544 | −0.5 | −0.528 | 0.334 | −0.798 | 0.443 | 0.832 | 0.932 | 0.529 | |
| p | <0.0001 | <0.0001 | <0.0001 | 0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozegowska, K.; Korman, M.; Szmyt, A.; Pawelczyk, L. Heterogeneity of Endocrinologic and Metabolic Parameters in Reproductive Age Polycystic Ovary Syndrome (PCOS) Women Concerning the Severity of Hyperandrogenemia—A New Insight on Syndrome Pathogenesis. Int. J. Environ. Res. Public Health 2020, 17, 9291. https://doi.org/10.3390/ijerph17249291
Ozegowska K, Korman M, Szmyt A, Pawelczyk L. Heterogeneity of Endocrinologic and Metabolic Parameters in Reproductive Age Polycystic Ovary Syndrome (PCOS) Women Concerning the Severity of Hyperandrogenemia—A New Insight on Syndrome Pathogenesis. International Journal of Environmental Research and Public Health. 2020; 17(24):9291. https://doi.org/10.3390/ijerph17249291
Chicago/Turabian StyleOzegowska, Katarzyna, Marcin Korman, Agnieszka Szmyt, and Leszek Pawelczyk. 2020. "Heterogeneity of Endocrinologic and Metabolic Parameters in Reproductive Age Polycystic Ovary Syndrome (PCOS) Women Concerning the Severity of Hyperandrogenemia—A New Insight on Syndrome Pathogenesis" International Journal of Environmental Research and Public Health 17, no. 24: 9291. https://doi.org/10.3390/ijerph17249291
APA StyleOzegowska, K., Korman, M., Szmyt, A., & Pawelczyk, L. (2020). Heterogeneity of Endocrinologic and Metabolic Parameters in Reproductive Age Polycystic Ovary Syndrome (PCOS) Women Concerning the Severity of Hyperandrogenemia—A New Insight on Syndrome Pathogenesis. International Journal of Environmental Research and Public Health, 17(24), 9291. https://doi.org/10.3390/ijerph17249291





