Hearing the Voices of Wingless Angels: A Critical Content Analysis of Nurses’ COVID-19 Experiences
Abstract
1. Introduction
2. Methodology
2.1. Ethical Statement
2.2. Data Collection
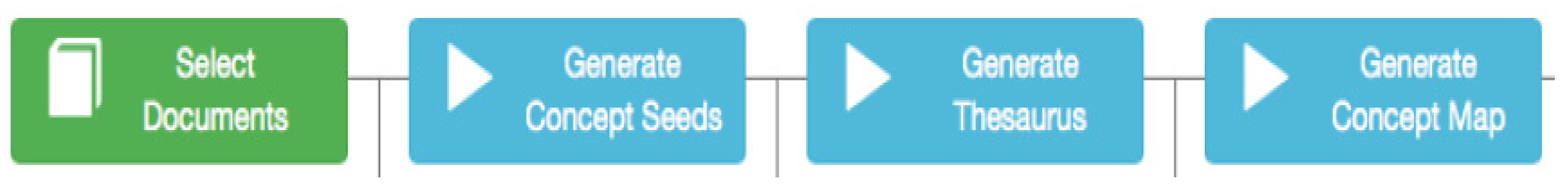
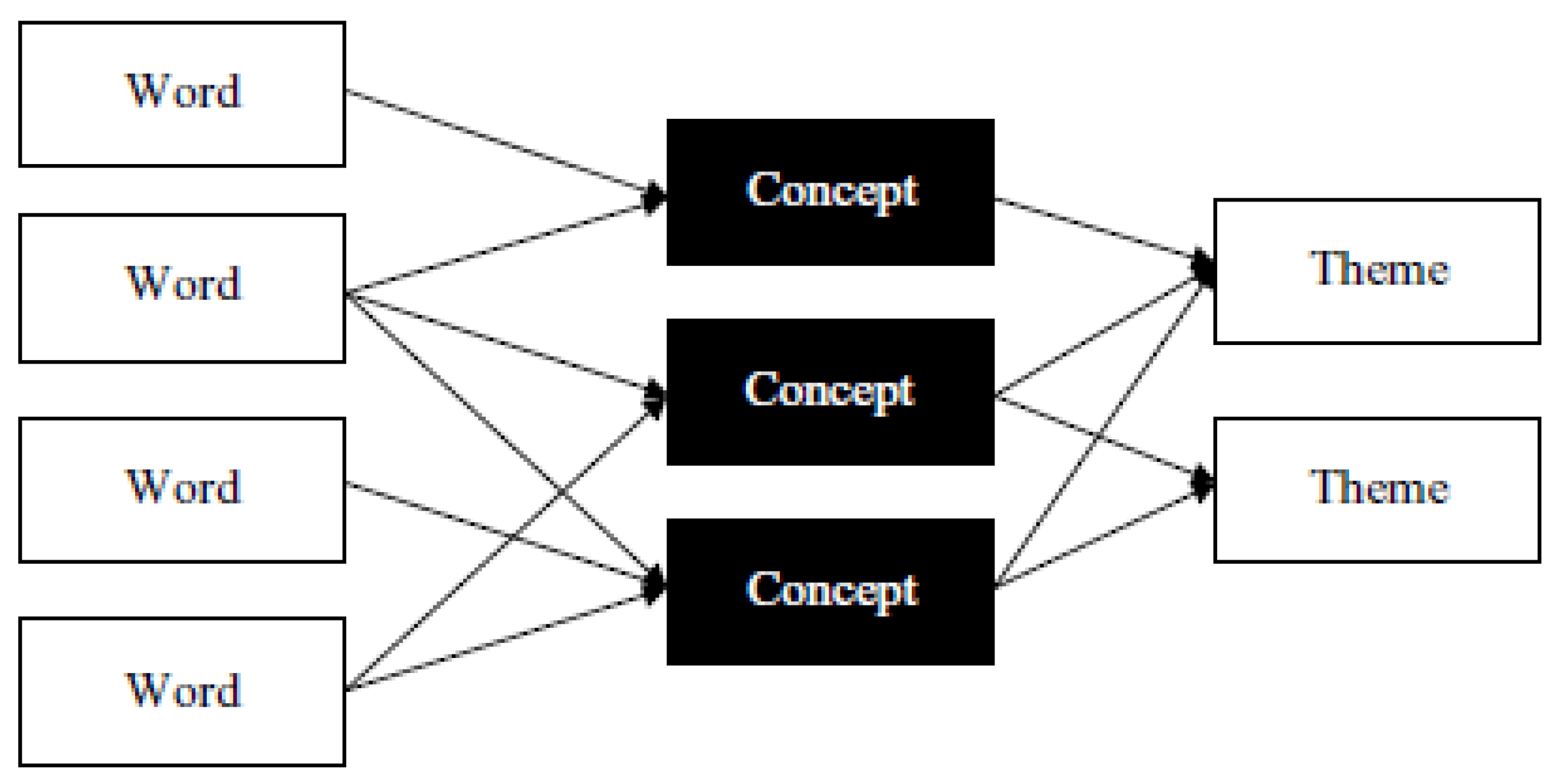
2.3. Data Treatment
3. Results
4. Discussion
5. Conclusions
5.1. Theoretical Contributions
5.2. Practical Implications
5.3. Limitations and Avenues for New Research
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Williams, C.C.; Kayaoglu, A. COVID-19 and undeclared work: Impacts and policy responses in Europe. Serv. Ind. J. 2020, 40, 914–931. [Google Scholar]
- Kim, Y.J.; Cho, J.H. Correlation between Preventive Health Behaviors and Psycho-Social Health Based on the Leisure Activities of South Koreans in the COVID-19 Crisis. Int. J. Environ. Res. Public Health 2020, 17, 4066. [Google Scholar]
- Cohen, J.; Kupferschmidt, K. Countries test tactics in ‘war’ against COVID-19. Science 2020, 367, 1287–1288. [Google Scholar] [PubMed]
- de Vera, J.D.C.P.; Alcalde, S.R.; Carretero, J.C.; García, M.B. The preventive effect of hydrocolloid dressing to prevent facial pressure and facial marks during use of medical protective equipment in Covid-19 pandemic. Br. J. Oral Maxillofac. Surg. 2020, 58, 723–725. [Google Scholar]
- Wańkowicz, P.; Szylińska, A.; Rotter, I. Assessment of Mental Health Factors among Health Professionals Depending on Their Contact with COVID-19 Patients. Int. J. Environ. Res. Public Health 2020, 17, 5849. [Google Scholar]
- Shahzad, F.; Du, J.; Khan, I.; Fateh, A.; Shahbaz, M.; Abbas, A.; Wattoo, M.U. Perceived Threat of COVID-19 Contagion and Frontline Paramedics’ Agonistic Behaviour: Employing a Stressor–Strain–Outcome Perspective. Int. J. Environ. Res. Public Health 2020, 17, 5102. [Google Scholar]
- Lázaro-Pérez, C.; Martínez-López, J.Á.; Gómez-Galán, J.; López-Meneses, E. Anxiety about the Risk of Death of Their Patients in Health Professionals in Spain: Analysis at the Peak of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5938. [Google Scholar]
- Buselli, R.; Corsi, M.; Baldanzi, S.; Chiumiento, M.; Del Lupo, E.; Dell’Oste, V.; Carmassi, C. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19). Int. J. Environ. Res. Public Health 2020, 17, 6180. [Google Scholar]
- Nowell, A. Hospice Nurse Describes How Covid-19 Has Changed Her Work. Wigan Today. Available online: https://www.wigantoday.net/health/hospice-nurse-describes-how-covid-19-has-changed-her-work2886454 (accessed on 20 August 2020).
- Choi, K.R.; Jeffers, K.S.; Logsdon, M.C. Nursing and the Novel Coronavirus: Risks and Responsibilities in a Global Outbreak. J. Adv. Nurs. 2020, 76, 1486–1487. [Google Scholar]
- Jiang, F.; Deng, L.; Zhang, L.; Cai, Y.; Cheung, C.W.; Xia, Z. Review of the clinical characteristics of coronavirus disease 2019 (COVID-19). J. Gen. Intern. Med. 2020, 35, 1545–1549. [Google Scholar]
- Pan, L.; Wang, L.; Huang, X. How to face the novel coronavirus infection during the 2019–2020 epidemic: The experience of Sichuan Provincial People’s Hospital. Intensive Care Med. 2020, 46, 573–575. [Google Scholar] [CrossRef] [PubMed]
- Hartley, D.M.; Perencevich, E.N. Public health interventions for COVID-19: Emerging evidence and implications for an evolving public health crisis. JAMA 2020, 323, 1908–1909. [Google Scholar] [CrossRef] [PubMed]
- Bacaksiz, F.E.; Eskici, G.T.; Seren, A.K.H. “From my Facebook profile”: What do nursing students share on Timeline, Photos, Friends, and About sections? Nurse Educ. Today 2020, 86, 104326. [Google Scholar] [CrossRef] [PubMed]
- Zugai, J.S.; Stein-Parbury, J.; Roche, M. Therapeutic alliance in mental health nursing: An evolutionary concept analysis. Issues Ment. Health Nurs. 2015, 36, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Liu, S. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Su, T.P.; Lien, T.C.; Yang, C.Y.; Su, Y.L.; Wang, J.H.; Tsai, S.L.; Yin, J.C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007, 41, 119–130. [Google Scholar] [CrossRef]
- Smith, M.W.; Smith, P.W.; Kratochvil, C.J.; Schwedhelm, S. The psychosocial challenges of caring for patients with Ebola virus disease. Health Secur. 2017, 15, 104–109. [Google Scholar] [CrossRef]
- Halcomb, E.; McInnes, S.; Williams, A.; Ashley, C.; James, S.; Fernandez, R.; Calma, K. The experiences of primary healthcare nurses during the COVID-19 pandemic in Australia. J. Nurs. Scholarsh. 2020, 52, 553–563. [Google Scholar] [CrossRef]
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Zumla, A. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Cheng, Z. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- The New York Times. Nurses Share Coronavirus Stories Anonymously in an Online Document. 2020. Available online: https://www.nytimes.com/2020/03/25/business/media/coronavirus-nurses-stories-anonymous.html (accessed on 22 July 2020).
- Independent. Coronavirus: Instagram Photo Posted by Italian Nurse Shows Effects of Virus on Medical Staff. 2020. Available online: https://www.independent.co.uk/life-style/health-and-families/coronavirus-nurse-italy-photo-milan-a9399656.html (accessed on 13 March 2020).
- Gitto, S.; Mancuso, P. Improving airport services using sentiment analysis of the websites. Tour. Manag. Perspect. 2017, 22, 132–136. [Google Scholar] [CrossRef]
- Martin-Domingo, L.; Martín, J.C.; Mandsberg, G. Social media as a resource for sentiment analysis of Airport Service Quality (ASQ). J. Air Transp. Manag. 2019, 78, 106–115. [Google Scholar] [CrossRef]
- Shepherd, A.; Sanders, C.; Doyle, M.; Shaw, J. Using social media for support and feedback by mental health service users: Thematic analysis of a twitter conversation. BMC Psychiatry 2015, 15, 29. [Google Scholar] [CrossRef] [PubMed]
- El-Awaisi, A.; O’Carroll, V.; Koraysh, S.; Koummich, S.; Huber, M. Perceptions of who is in the healthcare team? A content analysis of social media posts during COVID-19 pandemic. J. Interprofessional Care 2020, 1–11. [Google Scholar] [CrossRef]
- Smith, S.P. Instagram abroad: Performance, consumption and colonial narrative in tourism. Postcolonial Studies 2018, 21, 172–191. [Google Scholar] [CrossRef]
- Statista. 2020. Available online: https://www.statista.com/statistics/183585/instagram-number-of-global-users/#statisticContainer (accessed on 22 April 2020).
- Guo, Y.F.; Plummer, V.; Lam, L.; Wang, Y.; Cross, W.; Zhang, J.P. The effects of resilience and turnover intention on nurses’ burnout: Findings from a comparative cross-sectional study. J. Clin. Nurs. 2019, 28, 499–508. [Google Scholar] [CrossRef]
- Glerean, N.; Hupli, M.; Talman, K.; Haavisto, E. Young peoples’ perceptions of the nursing profession: An integrative review. Nurse Educ. Today 2017, 57, 95–102. [Google Scholar] [CrossRef]
- Hoeve, Y.T.; Jansen, G.; Roodbol, P. The nursing profession: Public image, self-concept and professional identity. A discussion paper. J. Adv. Nurs. 2014, 70, 295–309. [Google Scholar] [CrossRef]
- Stoleriu, O.M.; Brochado, A.; Rusu, A.; Lupu, C. Analyses of Visitors’ Experiences in a Natural World Heritage Site Based on TripAdvisor Reviews. Visit. Stud. 2019, 22, 192–212. [Google Scholar] [CrossRef]
- Rodrigues, H.; Brochado, A.; Troilo, M.; Mohsin, A. Mirror, mirror on the wall, who’s the fairest of them all? A critical content analysis on medical tourism. Tour. Manag. Perspect. 2017, 24, 16–25. [Google Scholar] [CrossRef]
- Brochado, A.; Rita, P.; Oliveira, C.; Oliveira, F. Airline passengers’ perceptions of service quality: Themes in online reviews. Int. J. Contemp. Hosp. Manag. 2019, 31, 855–873. [Google Scholar] [CrossRef]
- Pearce, P.L.; Wu, M.Y. Tourists’ evaluation of a romantic themed attraction: Expressive and instrumental issues. J. Travel Res. 2016, 55, 220–232. [Google Scholar] [CrossRef]
- Tseng, C.; Wu, B.; Morrison, A.M.; Zhang, J.; Chen, Y.C. Travel blogs on China as a destination image formation agent: A qualitative analysis using Leximancer. Tour. Manag. 2015, 46, 347–358. [Google Scholar] [CrossRef]
- NurseJournal. 20 Instagram and Twitter Accounts for Nurses (Plus Hashtags!). 2020. Available online: https://nursejournal.org/community/20-instagram-and-twitter-accounts-for-nurses-plus-hashtags/ (accessed on 18 June 2020).
- Ayres, L. Qualitative research proposals—Part I: Posing the problem. J. Wound Ostomy Cont. Nurs. 2007, 34, 30–32. [Google Scholar] [CrossRef]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181. [Google Scholar] [CrossRef]
- Powers, B.A.; Knapp, T.; Knapp, T.R. Dictionary of Nursing Theory and Research; Springer Publishing Company: New York, NY, USA, 2010. [Google Scholar]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Krippendorff, K. The Content Analysis Reader; Sage: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Salsali, M.; Ahmadi, F. Nurses’ experiences of uncertainty in clinical practice: A descriptive study. J. Adv. Nurs. 2011, 67, 991–999. [Google Scholar] [CrossRef]
- Lupu, C.; Brochado, A.; Stoleriu, O.M. Experiencing Dracula’s homeland. Tour. Geogr. 2017, 19, 756–779. [Google Scholar] [CrossRef]
- Angus, D.; Smith, A.; Wiles, J. Conceptual recurrence plots: Revealing patterns in human discourse. IEEE Trans. Vis. Comput. Graph. 2011, 18, 988–997. [Google Scholar] [CrossRef]
- Leximancer, P.L. Available online: https://mcrc.journalism.wisc.edu/files/2018/04/Manual_Leximancer.pdf (accessed on 18 March 2020).
- Crofts, K.; Bisman, J. Interrogating accountability. Qual. Res. Account. Manag. 2010, 7, 180–207. [Google Scholar] [CrossRef]
- Zhang, Y.; Cole, S.T. Dimensions of lodging guest satisfaction among guests with mobility challenges: A mixed-method analysis of web-based texts. Tour. Manag. 2016, 53, 13–27. [Google Scholar] [CrossRef]
- Arasli, H.; Saydam, M.B.; Kilic, H. Cruise Travelers’ Service Perceptions: A Critical Content Analysis. Sustainability 2020, 12, 6702. [Google Scholar] [CrossRef]
- Fernandez, R.; Lord, H.; Halcomb, E.; Moxham, L.; Middleton, R.; Alananzeh, I.; Ellwood, L. Implications for COVID-19: A systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. Inte. J. Nurs. Stud. 2020, 103637. [Google Scholar] [CrossRef] [PubMed]
- Martino Maze, C.D. Registered nurses’ personal rights vs. professional responsibility in caring for members of underserved and disenfranchised populations. J. Clin. Nurs. 2005, 14, 546–554. [Google Scholar]
- Sibbald, B. Right to refuse work becomes another SARS issue. Can. Med Assoc. J. 2003, 169, 141. [Google Scholar]
- Andrewin, A.; Chien, L.Y. Stigmatization of patients with HIV/AIDS among doctors and nurses in Belize. Aids Patient Care Stds 2008, 22, 897–906. [Google Scholar] [CrossRef]
- Beltrami, E.M.; Williams, I.T.; Shapiro, C.N.; Chamberland, M.E. Risk and management of blood-borne infections in health care workers. Clin. Microbiol. Rev. 2000, 13, 385–407. [Google Scholar] [CrossRef]
- Ishimaru, T.; Wada, K.; Hoang, H.T.X.; Bui, A.T.M.; Nguyen, H.D.; Le, H.; Smith, D.R. Nurses’ willingness to care for patients infected with HIV or Hepatitis B/C in Vietnam. Environ. Health Prev. Med. 2017, 22, 1–7. [Google Scholar] [CrossRef]
- Naidoo, P. Barriers to HIV Care and Treatment by Doctors: A review of the literature. S. Afr. Fam. Pract. 2006, 48, 55-16e. [Google Scholar] [CrossRef]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003, 168, 1245–1251. [Google Scholar] [PubMed]
- Tzeng, H.M. Nurses’ professional care obligation and their attitudes towards SARS infection control measures in Taiwan during and after the 2003 epidemic. Nurs. Ethics 2004, 11, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.C.; Lee, W.C.; Lin, R.S. Are employees more committed and willing to accept critical assignments during a crisis? A study of organizational commitment, professional commitment and willingness to care during the SARS outbreak in Taiwan. Int. J. Hum. Resour. Manag. 2012, 23, 2698–2711. [Google Scholar] [CrossRef]
- Min, A.; Min, H.; Hong, H.C. Psychometric properties of the Korean version of the Occupational Fatigue Exhaustion Recovery Scale in a nurse population. Res. Nurs. Health 2019, 42, 358–368. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kim, Y.I.; Park, S.J.; Kim, I.K.; Choi, Y.K.; Kim, S.H. Safe, high-throughput screening of natural compounds of MERS-CoV entry inhibitors using a pseudovirus expressing MERS-CoV spike protein. Int. J. Antimicrob. Agents 2018, 52, 730. [Google Scholar] [CrossRef]
- Lehmann, M.; Bruenahl, C.A.; Löwe, B.; Addo, M.M.; Schmiedel, S.; Lohse, A.W.; Schramm, C. Ebola and psychological stress of health care professionals. Emerg. Infect. Dis. 2015, 21, 913. [Google Scholar] [CrossRef]
- Yıldırım, M.; Solmaz, F. COVID-19 burnout, COVID-19 stress and resilience: Initial psychometric properties of COVID-19 Burnout Scale. Death Stud. 2020, 1–9. [Google Scholar] [CrossRef]
- Sung, C.W.; Chen, C.H.; Fan, C.Y.; Su, F.Y.; Chang, J.H.; Hung, C.C.; Lee, T.S.H. Burnout in Medical Staffs During a Coronavirus Disease (COVID-19) Pandemic. 2020. Available online: https://ssrn.com/abstract=3594567 (accessed on 9 June 2020).
- Sheng, Q.; Zhang, X.; Wang, X.; Cai, C. The influence of experiences of involvement in the COVID-19 rescue task on the professional identity among Chinese nurses: A qualitative study. J. Nurs. Manag. 2020, 28, 1662–1669. [Google Scholar] [CrossRef]
- Fiksenbaum, L.; Marjanovic, Z.; Greenglass, E.R.; Coffey, S. Emotional exhaustion and state anger in nurses who worked during the SARS outbreak: The role of perceived threat and organizational support. Can. J. Community Ment. Health 2007, 25, 89–103. [Google Scholar] [CrossRef]
- Chandra, A. Why do nurses leave and what can health organizations do to retain them? Hosp. Top. 2003, 81, 33–36. [Google Scholar]
- Hausknecht, J.P.; Rodda, J.; Howard, M.J. Targeted employee retention: Performance-based and job-related differences in reported reasons for staying. Hum. Resour. Manag. 2009, 48, 269–288. [Google Scholar] [CrossRef]
- Koh, D.; Lim, M.K.; Chia, S.E.; Ko, S.M.; Qian, F.; Ng, V.; Ng, W. Risk Perception and Impact of Severe Acute Respiratory Syndrome (SARS) on Work and Personal Lives of Healthcare Workers in Singapore What Can We Learn? Med. Care 2005, 43, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.M.; Kwong-Lo, R.S.; Mak, C.W.; Wong, J.S. Fear of severe acute respiratory syndrome (SARS) among health care workers. J. Consult. Clin. Psychol. 2005, 73, 344. [Google Scholar] [CrossRef] [PubMed]
- Mok, E.; Chung, B.P.; Chung, J.W.; Wong, T.K. An exploratory study of nurses suffering from severe acute respiratory syndrome (SARS). Int. J. Nurs. Pract. 2005, 11, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Chung, B.P.M.; Wong, T.K.S.; Suen, E.S.B.; Chung, J.W.Y. SARS: Caring for patients in Hong Kong. J. Clin. Nurs. 2005, 14, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, H.M.; Yin, C.Y. Nurses’ fears and professional obligations concerning possible human-to-human avian flu. Nurs. Ethics 2006, 13, 455–470. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Tan, H. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Galedar, N.; Toulabi, T.; Kamran, A.; Heydari, H. Exploring nurses’ perception of taking care of patients with coronavirus disease (COVID-19): A qualitative study. Nurs. Open 2020. [Google Scholar] [CrossRef]
- Labrague, L.J.; De los Santos, J. Fear of Covid-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2020. [Google Scholar] [CrossRef]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef]
- Corley, A.; Hammond, N.E.; Fraser, J.F. The experiences of health care workers employed in an Australian intensive care unit during the H1N1 Influenza pandemic of 2009: A phenomenological study. Int. J. Nurs. Stud. 2010, 47, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Sage, S.; Samolyk, M.; Nair, D. Mask-related skin injury during a respiratory pandemic: A wound CNC perspective. Aust. Nurs. Midwifery J. 2020, 27, 24–25. [Google Scholar]
- Leigh, J.P.; Wiatrowski, W.J.; Gillen, M.; Steenland, N.K. Characteristics of persons and jobs with needlestick injuries in a national data set. Am. J. Infect. Control 2008, 36, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Lan, J.; Song, Z.; Miao, X.; Li, H.; Li, Y.; Dong, L.; Zhou, N. Skin damage among health care workers managing coronavirus disease-2019. J. Am. Acad. Dermatol. 2020, 82, 1215–1216. [Google Scholar] [CrossRef]
- Atzori, L.; Ferreli, C.; Atzori, M.G.; Rongioletti, F. COVID-19 and impact of personal protective equipment use: From occupational to generalized skin care need. Dermatol. Ther. 2020, e13598. [Google Scholar] [CrossRef]
- Bonias, D.; Bartram, T.; Leggat, S.G.; Stanton, P. Does psychological empowerment mediate the relationship between high performance work systems and patient care quality in hospitals? Asia Pac. J. Hum. Resour. 2010, 48, 319–337. [Google Scholar] [CrossRef]
- Bartram, T.; Karimi, L.; Leggat, S.G.; Stanton, P. Social identification: Linking high performance work systems, psychological empowerment and patient care. Int. J. Hum. Resour. Manag. 2014, 25, 2401–2419. [Google Scholar] [CrossRef]
- Karatepe, O.M.; Olugbade, O.A. The mediating role of work engagement in the relationship between high-performance work practices and job outcomes of employees in Nigeria. Int. J. Contemp. Hosp. Manag. 2016, 28, 2350–2371. [Google Scholar] [CrossRef]
- Smith-Miller, C.A.; Shaw-Kokot, J.; Curro, B.; Jones, C.B. An integrative review: Fatigue among nurses in acute care settings. JONA: J. Nurs. Adm. 2014, 44, 487–494. [Google Scholar] [CrossRef]
- Han, K.; Trinkoff, A.M.; Geiger-Brown, J. Factors associated with work-related fatigue and recovery in hospital nurses working 12-hour shifts. Workplace Health Saf. 2014, 62, 409–414. [Google Scholar] [CrossRef]
- Hinshaw, A.S. Keeping patients safe: A collaboration among nurse administrators and researchers. Nurs. Adm. Q. 2006, 30, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.S.; Chee, C.Y.; Ho, R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 2020, 49, 1–3. [Google Scholar]
- Epp, K. Burnout in critical care nurses: A literature review. Dynamics (Pemb. Ont.) 2012, 23, 25–31. [Google Scholar]
- World Health Organization. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020 (No. WHO/2019-nCoV/IPC PPE_use/2020.2); WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Radic, A.; Lück, M.; Ariza-Montes, A.; Han, H. Fear and Trembling of Cruise Ship Employees: Psychological Effects of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6741. [Google Scholar] [CrossRef] [PubMed]

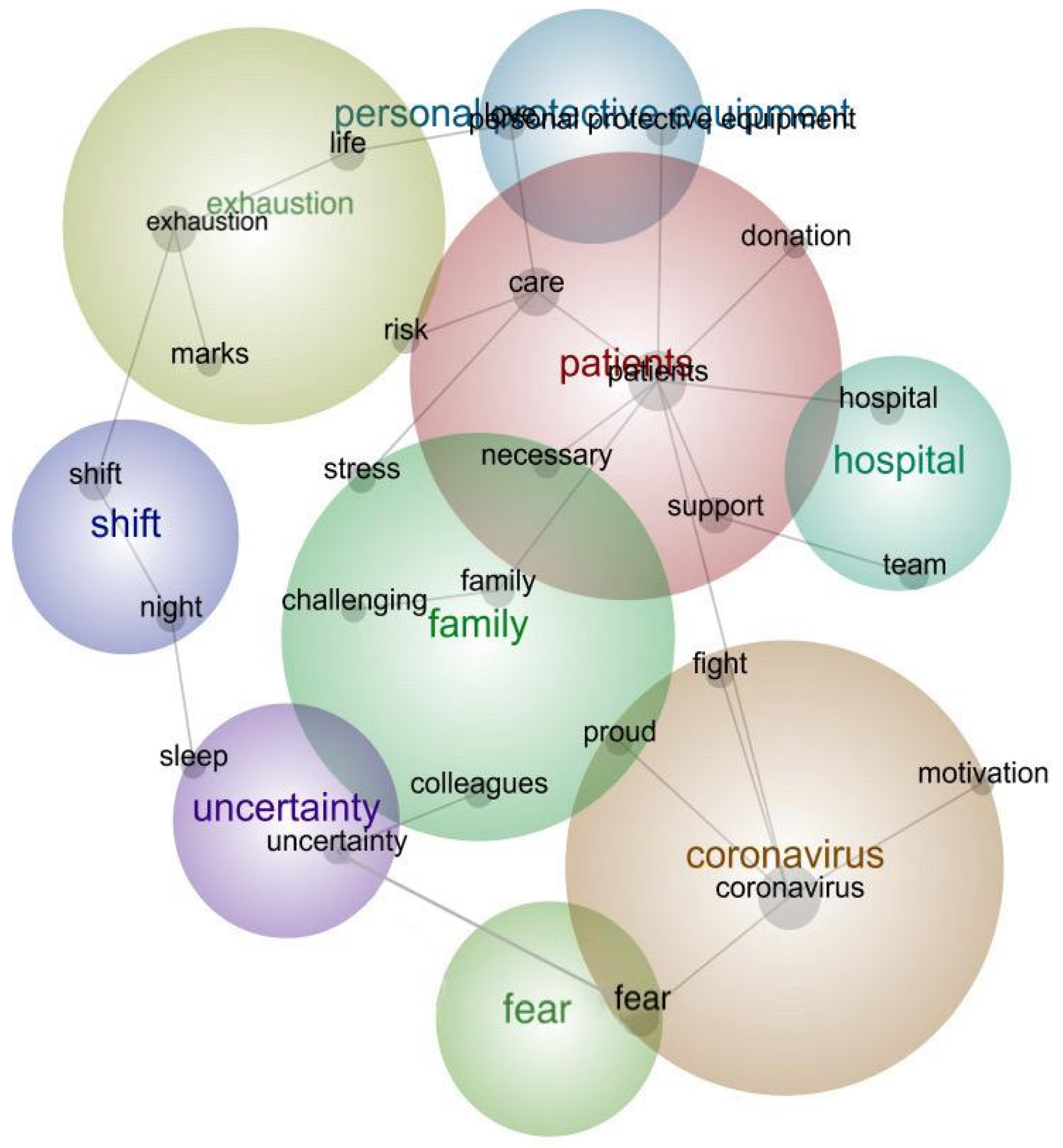
| Themes | Concepts | Relevancy |
|---|---|---|
| Patients | patient | 100% |
| care | 44% | |
| risk | 41% | |
| support | 33% | |
| donation | 27% | |
| necessary | 38% | |
| Coronavirus | coronavirus | 37% |
| motivation | 31% | |
| proud | 28% | |
| fight | 19% | |
| Exhaustion | exhaustion | 39% |
| marks | 30% | |
| life | 21% | |
| Family | family | 20% |
| patients | 18% | |
| challenging | 18% | |
| risk | 14% | |
| Hospital | hospital | 18% |
| team | 11% | |
| Shift | shift | 15% |
| night | 9% | |
| Uncertainty | uncertainty | 11% |
| sleep | 9% | |
| Fear | fear | 12% |
| Personal protective equipment | Personal protective equipment | 12% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arasli, H.; Furunes, T.; Jafari, K.; Saydam, M.B.; Degirmencioglu, Z. Hearing the Voices of Wingless Angels: A Critical Content Analysis of Nurses’ COVID-19 Experiences. Int. J. Environ. Res. Public Health 2020, 17, 8484. https://doi.org/10.3390/ijerph17228484
Arasli H, Furunes T, Jafari K, Saydam MB, Degirmencioglu Z. Hearing the Voices of Wingless Angels: A Critical Content Analysis of Nurses’ COVID-19 Experiences. International Journal of Environmental Research and Public Health. 2020; 17(22):8484. https://doi.org/10.3390/ijerph17228484
Chicago/Turabian StyleArasli, Huseyin, Trude Furunes, Kaveh Jafari, Mehmet Bahri Saydam, and Zehra Degirmencioglu. 2020. "Hearing the Voices of Wingless Angels: A Critical Content Analysis of Nurses’ COVID-19 Experiences" International Journal of Environmental Research and Public Health 17, no. 22: 8484. https://doi.org/10.3390/ijerph17228484
APA StyleArasli, H., Furunes, T., Jafari, K., Saydam, M. B., & Degirmencioglu, Z. (2020). Hearing the Voices of Wingless Angels: A Critical Content Analysis of Nurses’ COVID-19 Experiences. International Journal of Environmental Research and Public Health, 17(22), 8484. https://doi.org/10.3390/ijerph17228484









