INFERENCE: An Evidence-Based Approach for Medicolegal Causal Analyses
Abstract
1. Introduction
2. Current Methods of Medicolegal Causal Analysis
3. The INtegration of Forensic Epidemiology and the Rigorous EvaluatioN of Causation Elements (INFERENCE) Approach and the Approach Selection Procedure
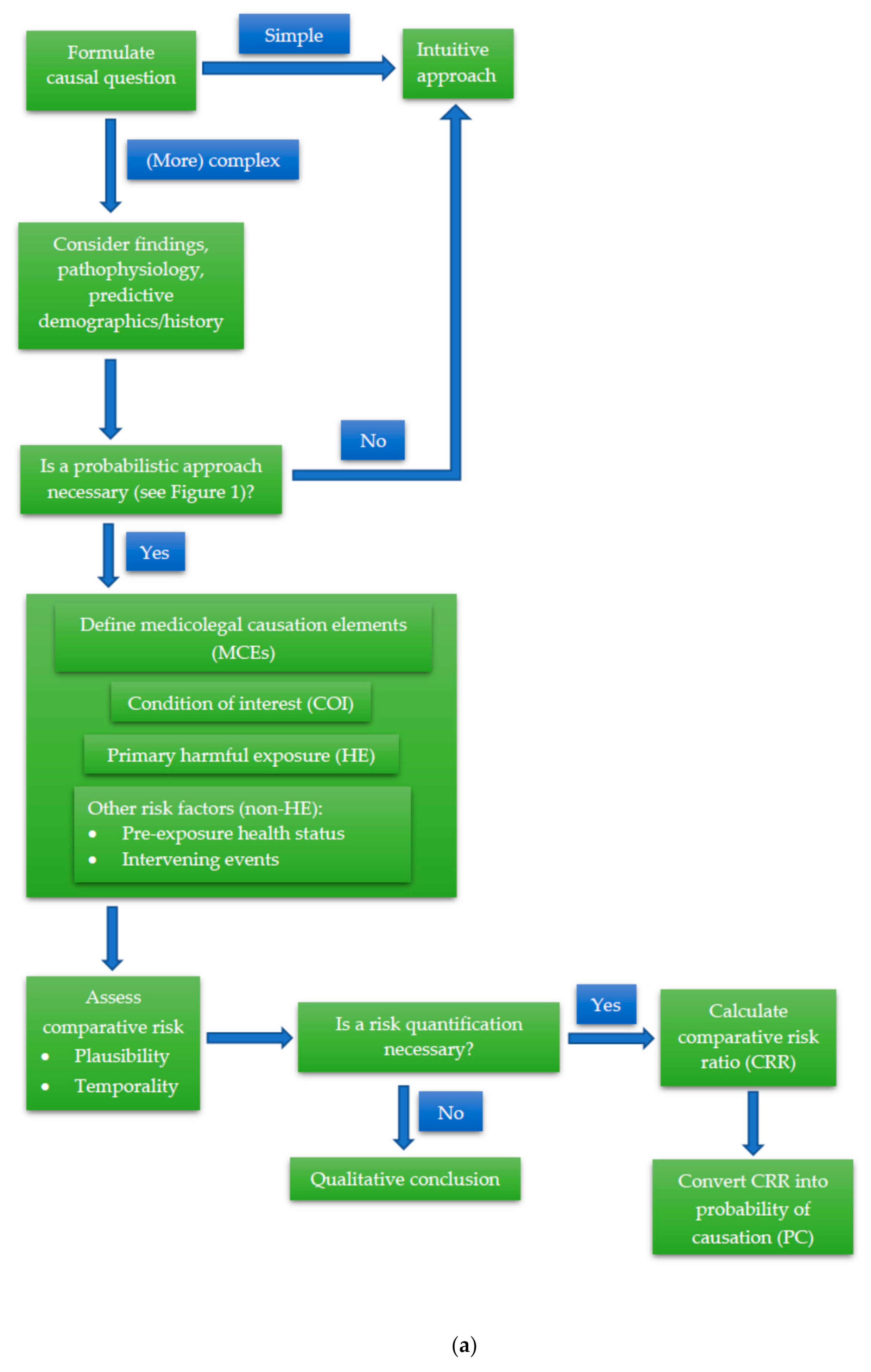
3.1. Formulation of the Causal Question to be Investigated
3.2. Consideration of Examination Findings, Injury/Pathophysiologic Mechanism, and Predictive Demographics and History
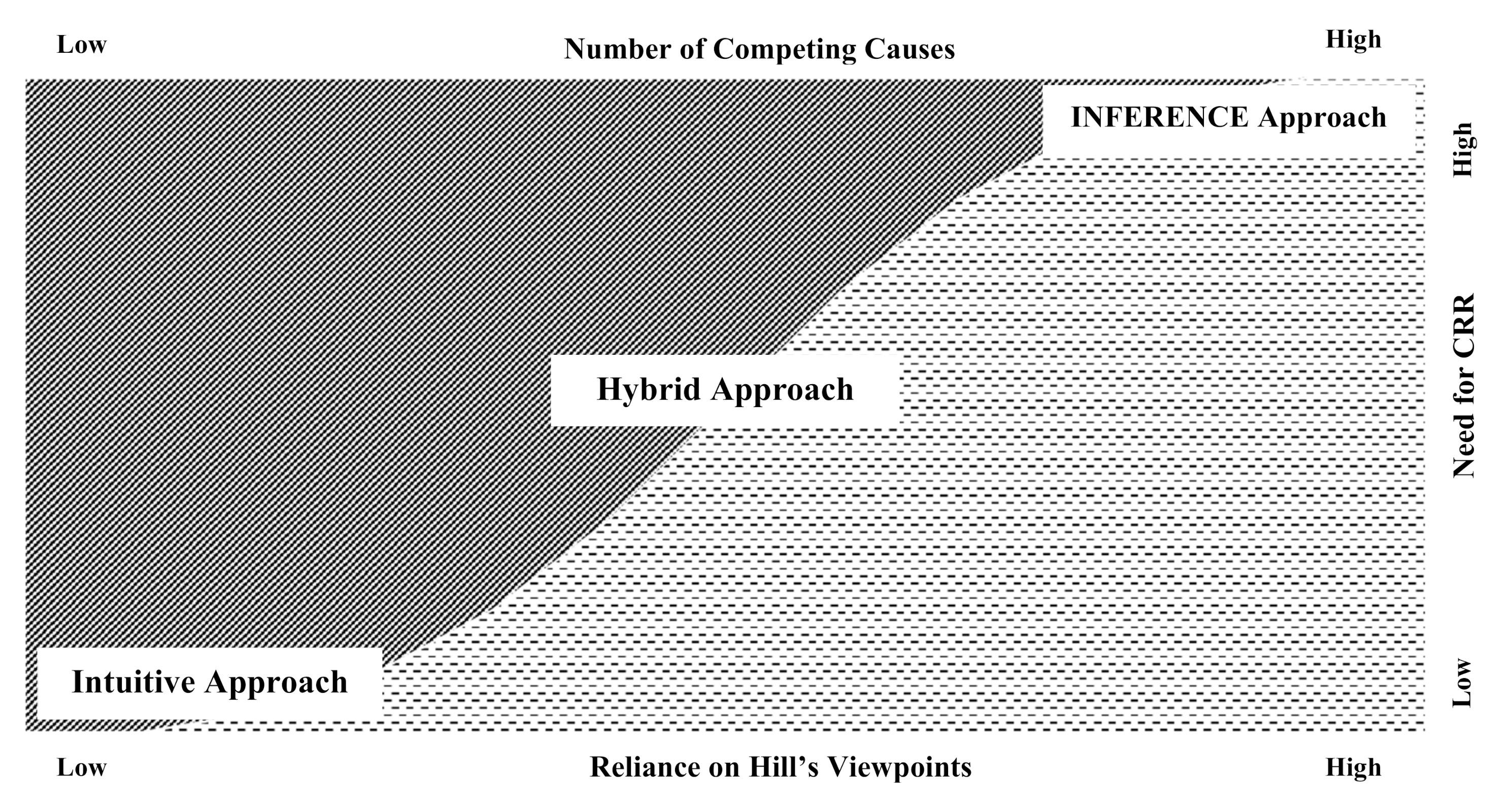
- The number of competing causes
- The need for an inventory of the Hill causal viewpoints. For a novel or otherwise previously unestablished causal relationship, an analysis of the relevant Hill viewpoints may be required to establish whether the relationship is plausible (please refer to Appendix B for an overview of the Hill viewpoints)
- The need to quantify and compare risks via a CRR approach.
3.3. Definition of the Medicolegal Causation Elements (MCE)
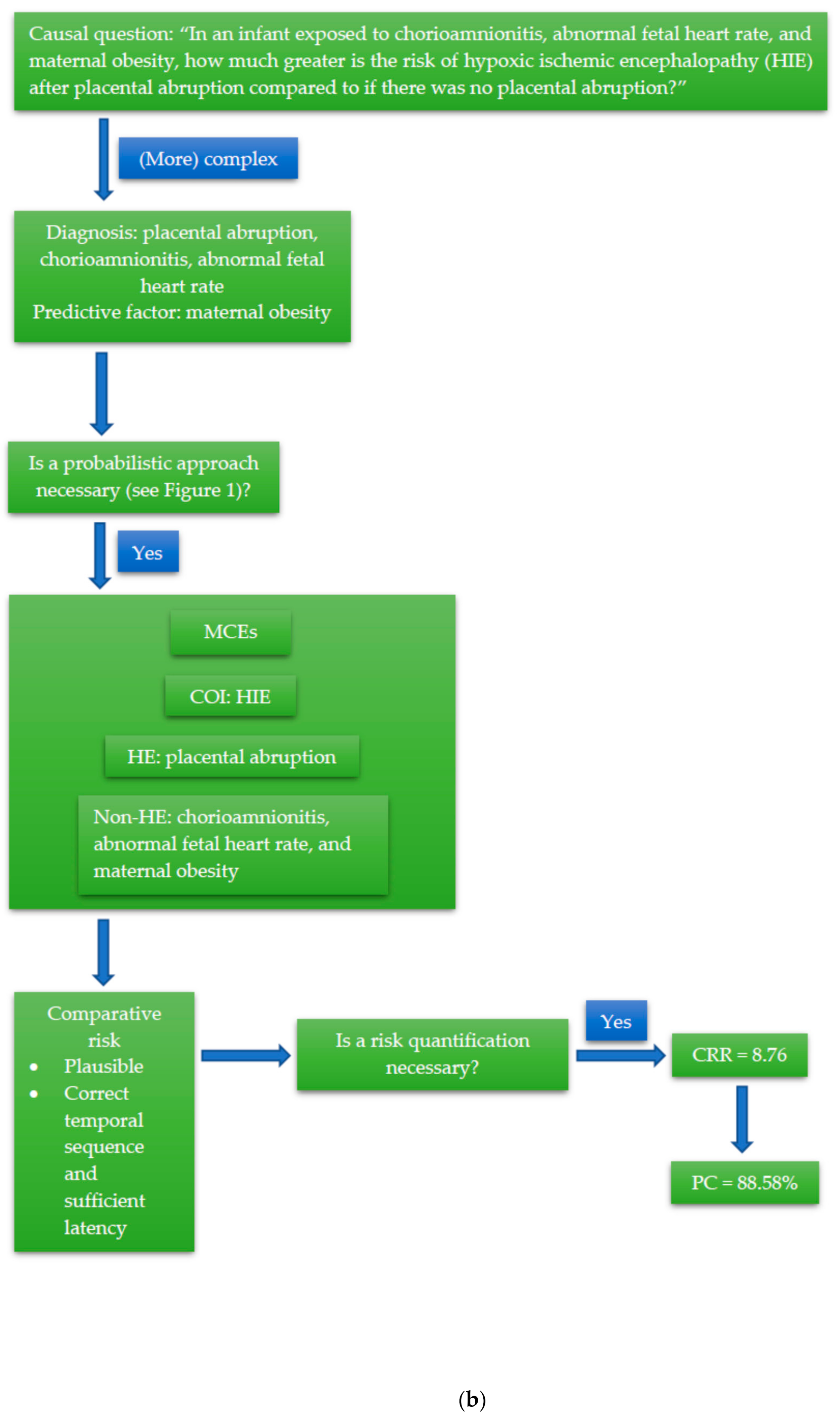
- Definition of the condition of interest (COI):The exact nature of the COI at the time it is being assessed should be described. This description includes the anatomical location, pathological features (i.e., fracture, laceration), level of severity, and natural history and sequelae (i.e., spinal cord injury, sudden cardiac death), based on the review of available medical evidence. If an examination of the harmed party is also performed as a part of the analysis, the current condition and functional impairments, therapeutic options, and prognosis may also be described in some cases. The opposing parties should generally agree on this definition of the COI before it can be used in the next steps, although this may not always be possible. The COI might not be the most current condition of the harmed party, but it is the condition that is thought to be caused by the alleged harmful exposure. In the example, the COI is fetal HIE as diagnosed using the appropriate medical criteria.
- Definition of the alleged primary harmful exposure (HE):The HE is a description of the alleged cause of the COI by the claiming party, including, when relevant, the nature, level of severity, and timing or temporal association of the defendant’s actions of interest, as well as the mechanism by which the actions caused the alleged harm/injury. This description, too, should be sufficiently well defined and agreed upon by the opposing parties. The HE in the example is placental abruption.
- Definition of potential competing causes (non-HE):
- ○
- The pre-exposure health status: as the harmed party’s current health status, relevant to the COI, will be compared to their health status prior to the HE, their pre-existing health status must be described in sufficient detail to allow for a pre-HE/post-HE comparison of the health status. This description should include any pre-existing diseases/impairments/conditions that could have caused or contributed to the COI in the absence of the HE, or which could have interacted with the HE to a substantial degree. Chorioamnionitis, abnormal fetal heart rate, and maternal obesity can all be classified as factors of the pre-exposure health status (pre-existing conditions) in the example case.
- ○
- Intervening events: any events that could have contributed to or interacted with the COI, occurring either after the HE and before the first indication of the COI, or after the COI but potentially acting as a modifier of the condition, should be listed. In the example, this could be in the form of a delay in properly treating the placental abruption.
3.4. Comparative Risk Assessment of Competing Causes
- Plausibility assessment: after the primary HE and all other potential non-HE causes of the COI have been identified, a plausibility assessment must first be performed on the relationship between the COI and the HE, and then on each discrete non-HE cause in order to evaluate the evidence for general causation [19,24,25]. The goal of this part of the analysis is to assess the pathophysiological plausibility of the injury mechanism based on available scientific literature as well as clinical expertise [24] and to avoid a post hoc ergo propter hoc fallacy (in which a biologically implausible causal relationship is erroneously deemed to be causal, solely because the effect followed the event in time) [25]. Obviously implausible, trivial, or temporally remote proposed non-HE causes can be eliminated from consideration in this step as well [24]. In the HIE case, all risk factors that were present (i.e., placental abruption, chorioamnionitis, abnormal fetal heart rate, and maternal obesity) can plausibly cause HIE through known pathophysiologic principles, whether individually or in various combinations [26,27,28,29,30,31].
- Temporality assessment: it is essential to establish the timing of the alleged harmful exposure and the first symptom/sign of the injury, for several reasons [24,25]. First, the temporal sequence of the injury following the harm must be correct. Second, the evidence of injury must occur within the effect range of the harmful exposure (“sufficiency”), and the latency between exposure and the first indication of injury must be quantified. The latency is then used to estimate the “hazard-period” between the HE and the first manifestation of the COI [22,25]. From a temporal point-of-view, the risk factors present in the HIE case all precede the occurrence of HIE within a sufficient range of time, as based on medical record data, so temporality can also be established.
- Determination of the CRR numerator value: the numerator is obtained from the risk of the COI given the HE, which is quantified from available epidemiologic data. For the HIE case, epidemiologic data show that the risk of HIE in a neonate exposed to placental abruption in addition to chorioamnionitis, abnormal fetal heart rate, and maternal obesity is 14.9% (1 in 6.7).
- Determination of the CRR denominator value: the denominator represents either the risk of the condition due to a risk that is attributable to a discrete event (a non-HE) or the pre-COI health status and natural history of the individual (the “base risk”). The latter is estimated from epidemiologic data of the cumulative risk of the COI occurring in the hazard period in association with all other potential causes but in the absence of the HE. The estimation of base risk from epidemiologic data is typically based on the assumption that the base risk is relatively uniform over time, allowing for the calculation of cumulative risk during the hazard period based on an established annual risk. In the example, the CRR denominator consists of the risk of HIE in a neonate exposed to chorioamnionitis, abnormal fetal heart rate, and maternal obesity, in the absence of placental abruption. Epidemiologic data shows this value to be 1.7% (1 in 59).
- Calculation of the CRR: the numerator is divided by the denominator to arrive at the CRR. In this case, the CRR is thus:
- The CRR can be converted into a probability of causation (PC) [15], as follows:
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| No. | Approach | Category | Application | Example | Strengths | Weaknesses |
|---|---|---|---|---|---|---|
| 1. | Intuitive approach (i.e., scientific common-sense) | Intuitive | Simple cases where the causal relationship “makes sense” based on fundamental scientific principles | Death following a gunshot wound to the head | Practical, does not need exceptional/additional resources | Not suitable for more complex cases where the causal relationship is not as readily apparent |
| 2. | Categorical intuitive deduction (i.e., the Sherlock Holmes style or educated guess) | Intuitive | Cases where there is only one plausible cause at the same time | Death following ingestion of insecticides in a previously healthy person with no signs of trauma | Impressive expert witness testimony | Not suitable for more complex cases where there is more than one plausible cause, requires a lot of professional experience, potentially misleading |
| 3. | Hill’s viewpoints | Intuitive-probabilistic | Cases with sufficient epidemiologic evidence and literature to assess competing causal hypotheses | Post-traumatic headache in a sexual-assault victim | Check-list-like criteria to guide causal inference | Temporal sequence is the only real “causal criterion”, the meaning or value of the other criteria can be unclear |
| 4. | The American Medical Association (AMA) Guides to the Evaluation of Disease and Injury Causation | Intuitive-probabilistic | Primarily cases of injury with multiple plausible causes and work-related conditions | Lower back-pain in a factory worker who stands all-day | Provide elements that may be used for a systematic step-by-step causal analysis, primarily to assess work-relatedness | Lengthy and complicated process, does not produce a PC/quantification of the level of certainty |
| 5. | Forcier-Lacerte medicolegal causal analysis model | Intuitive-probabilistic | Primarily cases of injury with multiple plausible causes and cases related to insurance claims | An elderly woman with severe osteoporosis who sustains a slip-and-fall resulting in several fractured ribs | Provide elements that may be used for a systematic step-by-step causal analysis, categorizes possible causes into (1) the accident, (2) preexisting health status, and (3) intervening event. | Lengthy and complicated process, does not produce a PC/quantification of the level of certainty |
| 6. | The epidemiology-based approach by Siegerink et al. | Probabilistic | Civil litigations or cases of tort, where the issue is primarily about the proportional liability of multiple plausible causes | The risk of lung cancer in a factory worker exposed to asbestos, who is also a heavy smoker with a family history of lung cancer | Fits both the sufficient cause model and the counterfactual model, offers proportional liability for each component cause (i.e., the unlawful act plus other possible factors) | Could overestimate the number of components of the sufficient cause, leading to an underestimation of liability, all components are considered as of equal importance, while from a legal perspective some causes may be more important than others (e.g., unlawful act vs genetics) |
| 7. | The 3-step medicolegal causation approach by Freeman | Probabilistic | Cases of injuries with multiple plausible causes that do not require a high degree of energy, preexisting conditions symptomatic after relatively minor trauma, or conditions with an insidious symptom onset | An elderly woman with shoulder pain after a minimal-damage rear-impact collision | Practicable, systematic, fits the standards of both medical and legal practice by establishing (1) plausibility, (2) temporality, and (3) the absence of a more probable alternative explanation (differential etiology) | Requires sufficient epidemiologic data and comprehension of epidemiologic methods to compare risks of differential etiologies |
| 8. | The forensic epidemiology approach | Probabilistic | Highly complex cases with multiple plausible causes | Peripartum cardiomyopathy in a young woman following exposure to doxorubicin | Systematic, provides a scientifically valid and verifiable quantification of probability in the form of a comparative risk ratio (CRR) and a probability of causation (PC), results are suitable for presentation in a court of law | Uses epidemiologic principles, methods, and data to formulate a probability, the analyses and calculations can be quite complicated, might not be suitable for day-to-day forensic medical practice |
Appendix B
| Viewpoint | Definition [18,35] | Forensic Example |
|---|---|---|
| Strength of association | A strong association, which is typically indicated by a high relative risk (RR), is more probably to be causal. | The association between a GSW to the head and death is generally speaking very strong because the risk of dying from a GSW to the head is extremely high. On the other hand, not all patients with septic shock die, and neither do all patients receiving opiate injections. Thus, the risk of dying from either cause is not as high as from a GSW to the head. |
| Consistency | If an association is observed in different settings or circumstances, it is probably causal. | That a person who has been shot in the head dies because of it has been observed repeatedly in various settings. Meanwhile, the death of a patient with septic shock is subject to a variation of circumstances, with or without opiate injections. |
| Specificity | If an effect is significantly associated with a certain cause or vice versa, then their relationship is probably causal. | A GSW to the head very specifically leads to death (although miraculous recoveries do occur very rarely). The relationship between septic shock and death, and between opiate injections and death, is, however, not as specific. |
| Temporality | The suspected cause must precede its effect, with a (biologically) appropriate sufficiency and latency (window period). | In cases of deaths, the temporal sequence is rarely an issue. What must be considered are two other aspects of temporality, i.e., temporal plausibility and temporal latency. In a GSW to the head, death often occurs instantaneously. Therefore, the causal relationship is usually plausible timewise, and the existence of competing causes occurring in the temporal window between the GSW and death (e.g., myocardial infarction) is highly unlikely. In contrast, a patient with septic shock dying, say, 6 h after injection of a short-acting opiate is less plausibly related to the injection than if death occurred in 30 min. Additionally, more competing causes could have occurred in the temporal window, which must be considered. |
| (Biological) plausibility | The degree to which the association is explainable by (currently known) scientific principles. | That a GSW to the head is (almost certainly) incompatible with life is consistent with known biological and scientific principles. The relationship between septic shock, opiate injections, and death is, however, subject to closer scrutiny as there are various biologic factors that could influence the outcome. |
| Coherence | The causal relationship may not seriously conflict present fundamental scientific facts. | In the simplest of words, it “makes sense” that a person who has been shot to the head subsequently dies. On the other hand, we would possibly be more surprised to find a patient dying after receiving an opiate injection that has been given appropriately. |
| Analogy | Known causal relationships between similar causes and effects may be translatable to unknown causal investigations. | A GSW to the head using a shotgun and a small-caliber bullet can be considered analogous in that it usually results in the same outcome, i.e., death. Thus, the exposure is translatable from one GSW case to the other. In the opiate-case, however, what can be considered as analogous is harder to define. More factors (e.g., from the patient, the injection, even the person giving the injection) need to be comparable be able to translate the exposure between cases. |
| Experiment | In some cases, experimental studies can provide evidence of causality. | It might be quite impossible to find experimental evidence for the GSW to the head (as with many exposures to trauma in forensic medical cases). For the opiate injection, however, randomized-controlled experiments are available and should be considered. |
| Dose-response relationship | A bigger “dose” (e.g., greater exposure) usually leads to a greater effect. | This viewpoint is more appropriate in the opiate injection case as the relationship between the dose of the opiate preparation and death is directly proportional. Nevertheless, it could also apply to the GSW if we consider the bullet caliber, shooting distance, etc. as the “dose”. |
References
- Madea, B. History of forensic medicine—A brief introduction. In History of Forensic Medicine; Madea, B., Ed.; Lehmanns Media: Berlin, Germany, 2017; pp. 3–27. [Google Scholar]
- Pinheiro, J. Introduction to forensic medicine and pathology. In Forensic Anthropology and Medicine: Complementary Sciences from Recovery to Cause of Death; Schmitt, A., Cunha, E., Pinheiro, J., Eds.; Humana Press Inc.: Totowa, NJ. USA, 2006; pp. 13–38. [Google Scholar]
- Meilia, P.D.I.; Freeman, M.D.; Zeegers, M.P. A review of the diversity in taxonomy, definitions, scope, and roles in forensic medicine: Implications for evidence-based practice. Forensic Sci. Med. Pathol. 2018, 14, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Honore, A. Principles and values underlying the concept of causation in law. In Causation in Law and Medicine; Mendelson, D., Freckelton, I.R., Eds.; Routledge: New York, NY, USA, 2016; pp. 3–13. [Google Scholar]
- Maldonado, G. The role of counterfactual theory in causal reasoning. Ann. Epidemiol. 2016, 26, 681–682. [Google Scholar] [CrossRef] [PubMed]
- Höfler, M. The Bradford Hill considerations on causality: A counterfactual perspective. Emerg. Themes Epidemiol. 2005, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Höfler, M. Causal inference based on counterfactuals. BMC Med. Res. Methodol. 2005, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D. Counterfactuals and comparative possibility. J. Philos. Logic 1973, 2, 418–446. [Google Scholar] [CrossRef]
- Meilia, P.D.I.; Freeman, M.D.; Zeegers, M.P. A review of causal inference in forensic medicine. Forensic Sci. Med. Pathol. 2020, 16, 313–320. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress; A Report of the Surgeon General; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2014.
- Green, M.; Freedman, D.; Gordis, L. Reference guide on epidemiology. In Reference Manual on Scientific Evidence, 3rd ed.; The National Academies Press: Washington, DC, USA, 2011; pp. 551–632. [Google Scholar]
- Freeman, M.D.; Zeegers, M.P. Introduction. In Forensic Epidemiology: Principles and Practice; Freeman, M.D., Zeegers, M.P., Eds.; Academic Press: Cambridge, MA, USA, 2016; pp. xv–xvii. [Google Scholar]
- Freeman, M.; Rossignol, A.M.; Hand, M.L. Forensic Epidemiology: A systematic approach to probabilistic determinations in disputed matters. J. Forensic Leg. Med. 2008, 15, 281–290. [Google Scholar] [CrossRef]
- Freeman, M.; Rossignol, A.M.; Hand, M.L. Applied forensic epidemiology: The Bayesian evaluation of forensic evidence in vehicular homicide investigation. J. Forensic Leg. Med. 2009, 16, 83–92. [Google Scholar] [CrossRef]
- Freeman, M.; Zeegers, M. Principles and applications of forensic epidemiology in the medicolegal setting. Law Probab. Risk 2015, 14, 269–278. [Google Scholar] [CrossRef]
- Koehler, S.A.; Freeman, M. Forensic epidemiology: A method for investigating and quantifying specific causation. Forensic Sci. Med. Pathol. 2014, 10, 217–222. [Google Scholar] [CrossRef]
- Freeman, M.D. The Role of Forensic Epidemiology in Evidence-Based Forensic Medical Practice. Ph.D. Thesis, Umeå Universitet, Umeå, Sweden, 2013. [Google Scholar]
- Hill, A.B. The Environment and Disease: Association or Causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef] [PubMed]
- LaCerte, M.; Forcier, P. Medicolegal causal analysis. Phys. Med. Rehabil. Clin. N. Am. 2002, 13, 371–408. [Google Scholar] [CrossRef]
- Worrall, J. Causality in medicine: Getting back to the Hill top. Prev. Med. 2011, 53, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Zeegers, M.; Bours, M.; Freeman, M. Methods Used in Forensic Epidemiologic Analysis. In Forensic Epidemiology: Principles and Practice; Freeman, M.D., Zeegers, M.P., Eds.; Elsevier: London, UK, 2016; pp. 71–110. [Google Scholar]
- Freeman, M.; Cahn, P.; Franklin, F. Applied forensic epidemiology, part 1: Medical negligence. Epidemiology 2014, 2, 1–11. [Google Scholar]
- Robertson, B.; Vignaux, G.A.; Berger, C.E.H. Interpreting Evidence: Evaluating Forensic Science in the Courtroom, 2nd ed.; John Wiley & Sons Ltd.: West Sussex, UK, 2016. [Google Scholar]
- Freeman, M.D. A Practicable and Systematic Approach to Medicolegal Causation. Orthopedics 2018, 41, 70–72. [Google Scholar] [CrossRef]
- Freeman, M.D.; Franklin, F. Medical negligence investigation. In Forensic Epidemiology: Principles and Practice; Freeman, M.D., Zeegers, M.P., Eds.; Academic Press: London, UK, 2016; pp. 351–370. [Google Scholar]
- Torbenson, V.E.; Tolcher, M.C.; Nesbitt, K.M.; Colby, C.E.; El-Nashar, S.A.; Gostout, B.S.; Weaver, A.L.; Mc Gree, M.E.; Famuyide, A.O. Intrapartum factors associated with neonatal hypoxic ischemic encephalopathy: A case-controlled study. BMC Pregnancy Childbirth 2017, 17, 1–7. [Google Scholar] [CrossRef]
- Parker, S.-J.; Kuzniewicz, M.; Niki, H.; Wu, Y.W. Antenatal and Intrapartum Risk Factors for Hypoxic-Ischemic Encephalopathy in a US Birth Cohort. J. Pediatr. 2018, 203, 163–169. [Google Scholar] [CrossRef]
- Peebles, P.J.; Duello, T.M.; Eickhoff, J.C.; McAdams, R.M. Antenatal and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy. J. Perinatol. 2019, 40, 63–69. [Google Scholar] [CrossRef]
- Michaeli, J.; Srebnik, N.; Zilberstein, Z.; Rotem, R.; Bin-Nun, A.; Grisaru-Granovsky, S. Intrapartum fetal monitoring and perinatal risk factors of neonatal hypoxic–ischemic encephalopathy. Arch. Gynecol. Obstet. 2020, 1–9. [Google Scholar] [CrossRef]
- Lundgren, C.; Brudin, L.; Wanby, A.-S.; Blomberg, M. Ante- and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy. J. Matern. Neonatal Med. 2018, 31, 1595–1601. [Google Scholar] [CrossRef]
- Liljestrom, L.; Wikstrom, A.-K.; Agren, J.; Jonsson, M. Antepartum risk factors for moderate to severe neonatal hypoxic ischemic encephalopathy: A Swedish national cohort study. Acta Obstet. Gynecol. Scand. 2018, 97, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. For and Against Methodologies: Some Perspectives on Recent Causal and Statistical Inference Debates. Eur. J. Epidemiol. 2017, 32, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.V.; Goodman, K.J. Causal criteria and counterfactuals; nothing more (or less) than scientific common sense. Emerg. Themes Epidemiol. 2006, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Dror, I. A Hierarchy of Expert Performance. J. Appl. Res. Mem. Cogn. 2016, 5, 121–127. [Google Scholar] [CrossRef]
- Freeman, M.; Kohles, S.S. Application of the Hill criteria to the causal association between post-traumatic headache and assault. Egypt. J. Forensic Sci. 2011, 1, 35–40. [Google Scholar] [CrossRef][Green Version]
| Category of Causal Analysis Methods | Intuitive | Probabilistic | |
|---|---|---|---|
| Hybrid | INFERENCE | ||
| Formulation of a causal question | (+) | (+) | (+) |
| Consideration of examination findings, injury/pathophysiologic mechanism, and predictive demographics and history | (±) | (+) | (+) |
| Definition of the medicolegal causation elements (MCE) | (+) | (+) | |
| Comparative risk assessment of competing causes (plausibility, temporality) | (+) | (+) | |
| Quantification of comparative risk | (+) | ||
| Case type examples | High risk, single suspect cause, e.g.,: Gunshot wound to the head/decapitation injury | Multiple suspect cause (requiring comparison of risk), but without need to quantify risks precisely, e.g.,: Risk of intracranial bleeding due to suspected (unproven) shaken-baby syndrome versus spontaneous bleeding due to known factor VII deficiency | Multiple suspect causes and the need for quantitative comparisons via comparative risk ratio (CRR) analysis, e.g.,: Increase in risk of hypoxic-ischemic encephalopathy due to placental abruption versus due to other known risk factors without placental abruption |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meilia, P.D.I.; Zeegers, M.P.; Herkutanto; Freeman, M. INFERENCE: An Evidence-Based Approach for Medicolegal Causal Analyses. Int. J. Environ. Res. Public Health 2020, 17, 8353. https://doi.org/10.3390/ijerph17228353
Meilia PDI, Zeegers MP, Herkutanto, Freeman M. INFERENCE: An Evidence-Based Approach for Medicolegal Causal Analyses. International Journal of Environmental Research and Public Health. 2020; 17(22):8353. https://doi.org/10.3390/ijerph17228353
Chicago/Turabian StyleMeilia, Putri Dianita Ika, Maurice P. Zeegers, Herkutanto, and Michael Freeman. 2020. "INFERENCE: An Evidence-Based Approach for Medicolegal Causal Analyses" International Journal of Environmental Research and Public Health 17, no. 22: 8353. https://doi.org/10.3390/ijerph17228353
APA StyleMeilia, P. D. I., Zeegers, M. P., Herkutanto, & Freeman, M. (2020). INFERENCE: An Evidence-Based Approach for Medicolegal Causal Analyses. International Journal of Environmental Research and Public Health, 17(22), 8353. https://doi.org/10.3390/ijerph17228353








