Use of Acupuncture for the Treatment of Sports-Related Injuries in Athletes: A Systematic Review of Case Reports
Abstract
1. Introduction
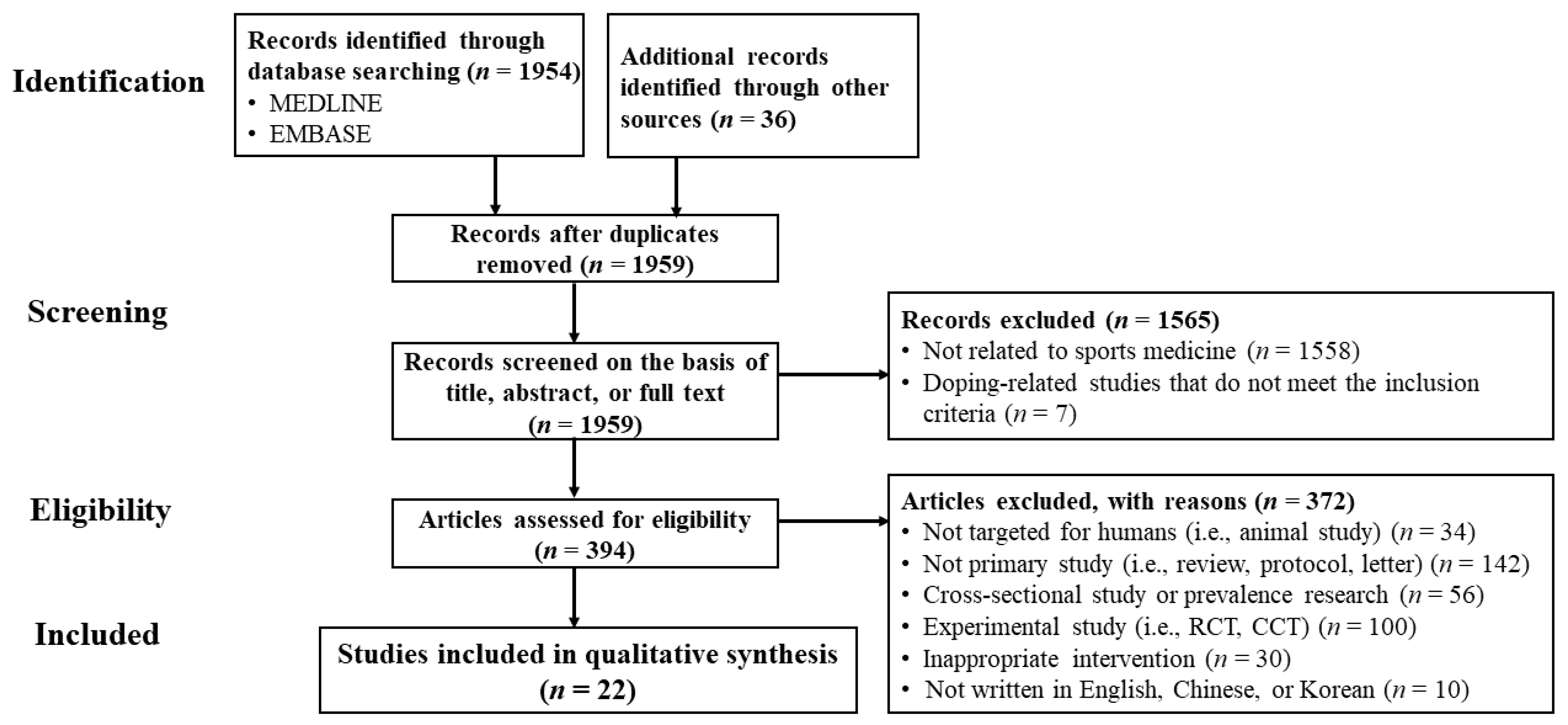
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection, Data Extraction, and Data Analysis
2.3. Data Extraction and Data Analysis
3. Results
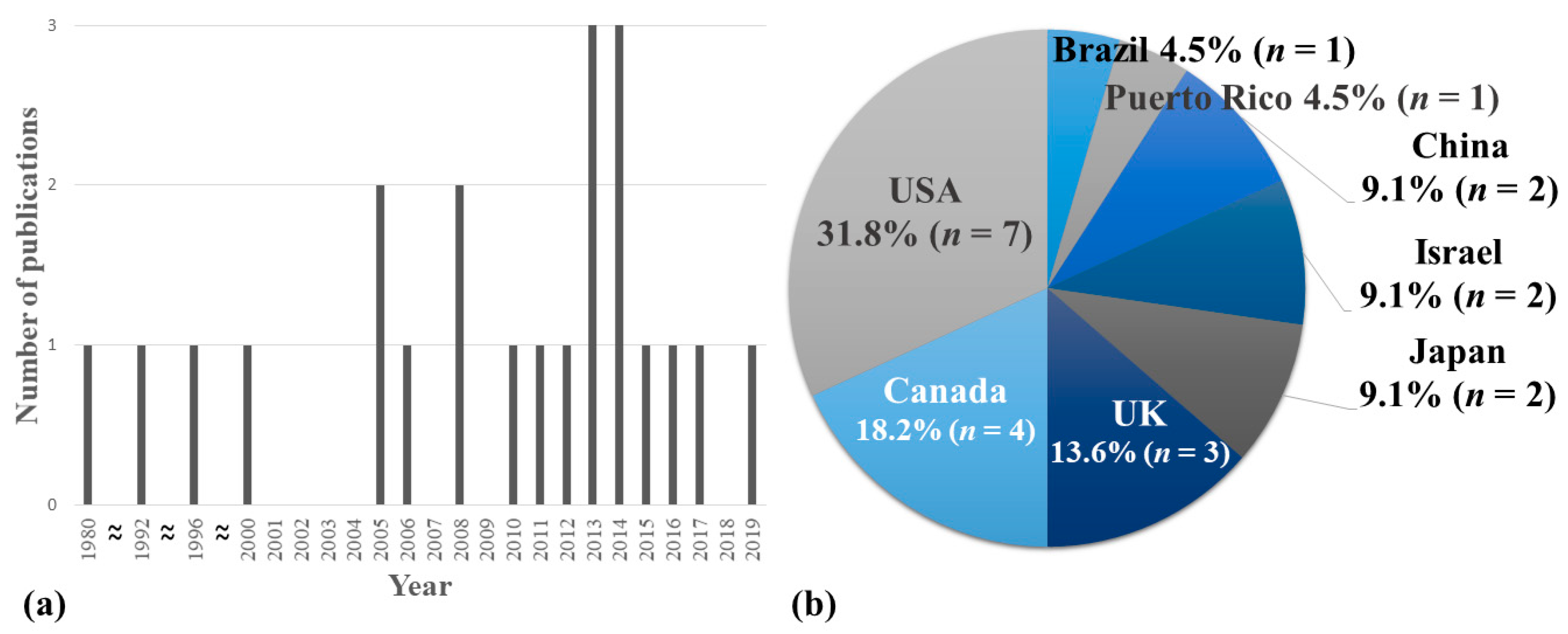
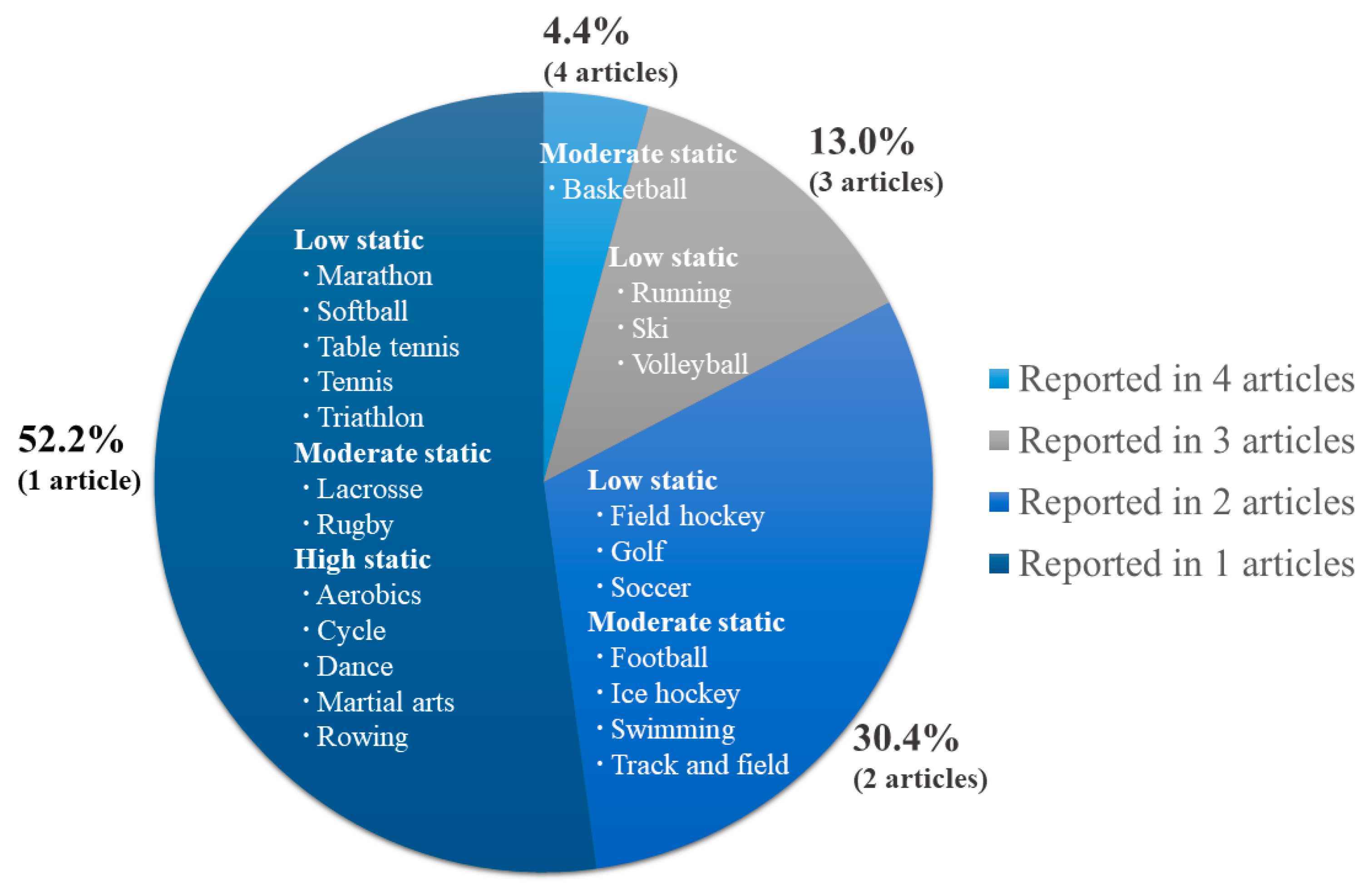
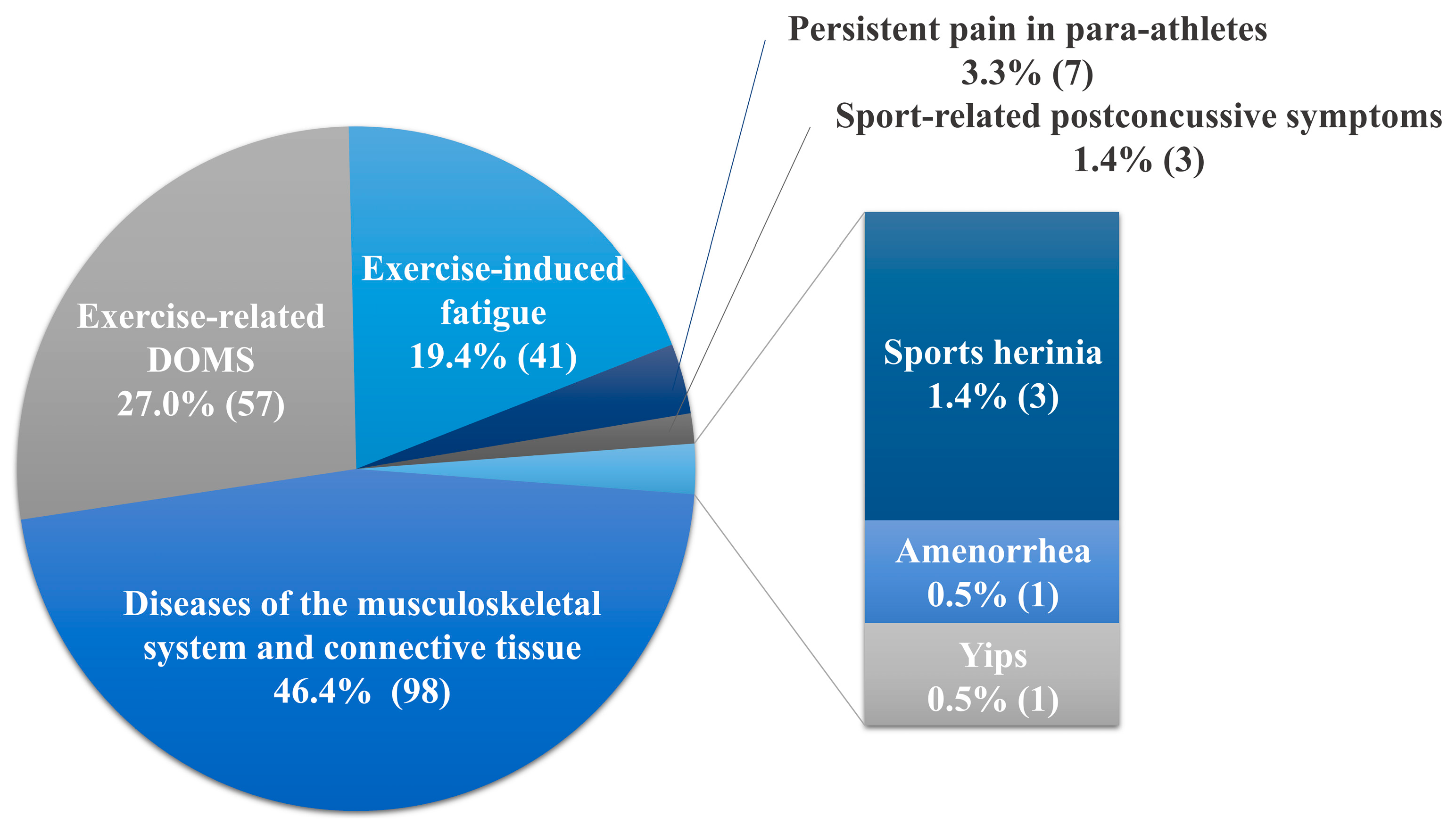
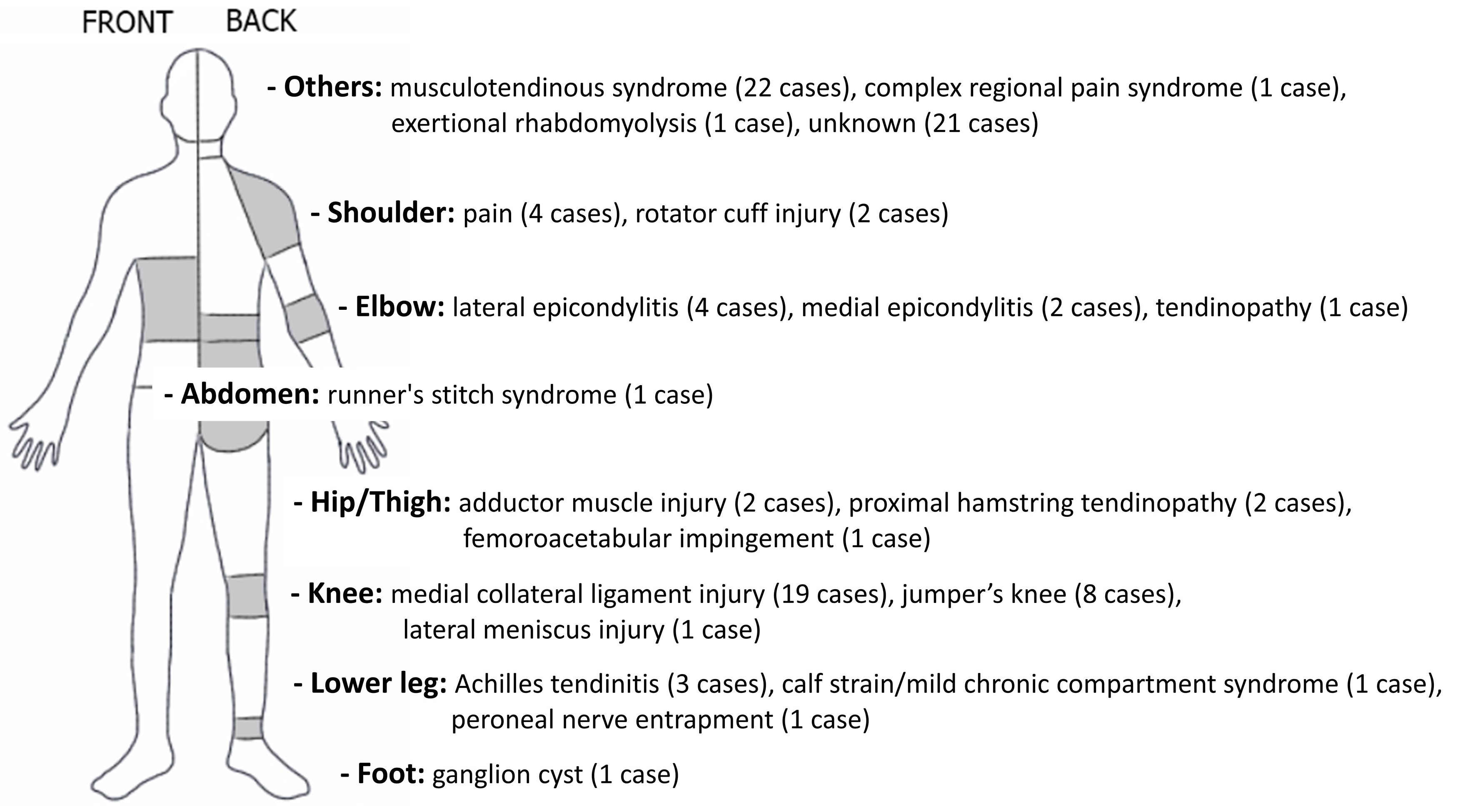
3.1. Demographic Information, Main Concerns, and Symptoms of the Patient
3.2. Therapeutic Intervention
3.2.1. Acupuncture
3.2.2. Other Intervention (Co-Intervention)
3.2.3. Treatment Duration and Session
3.3. Follow-Up and Outcomes
3.3.1. Outcome Measures
3.3.2. Results
3.3.3. Adverse Events
3.3.4. Return to Play and Recurrence
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef] [PubMed]
- Petridou, A.; Siopi, A.; Mougios, V. Exercise in the management of obesity. Metabolism 2019, 92, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Parkkari, J.; Kujala, U.M.; Kannus, P. Is it possible to prevent sports injuries? Review of controlled clinical trials and recommendations for future work. Sports Med. 2001, 31, 985–995. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.R.; Baker, R.J. Musculoskeletal injuries in sports. Prim. Care Clin. Off Pract. 2006, 33, 545–579. [Google Scholar] [CrossRef] [PubMed]
- Alessandrino, F.; Balconi, G. Complications of muscle injuries. J. Ultrasound 2013, 16, 215–222. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khan, K.; Brukner, P. Brukner & Khan’s Clinical Sports Medicine; McGraw-Hill Education: New York, NY, USA, 2011. [Google Scholar]
- Šmela, P.; Pačesová, P.; Kraček, S.; Hájovský, D. Performance Motivation of Elite Athletes, Recreational Athletes and Non-Athletes. Acta Fac. Educ. Phys. Univ. Comen. 2017, 57, 125–133. [Google Scholar] [CrossRef]
- Zippelius, K.; Schwarzinger, A. Sports injuries-improved healing processes due to integrative TCM therapy. Eur. J. Orient. Med. 2017, 8, 28–33. [Google Scholar]
- Herring, S.A.; Kibler, W.B.; Putukian, M. The team physician and the return-to-play decision: A consensus statement-2012 update. Med. Sci. Sports Exerc. 2012, 44, 2446–2448. [Google Scholar] [CrossRef]
- Ting, J.H.; Wallis, D.H. Medical management of the athlete: Evaluation and treatment of important issues in sports medicine. Clin. Podiatr. Med. Surg. 2007, 24, 127–158. [Google Scholar] [CrossRef]
- Doyscher, R.; Kraus, K.; Finke, B.; Scheibel, M. Acute and overuse injuries of the shoulder in sports. Orthopade 2014, 43, 202–208. [Google Scholar] [CrossRef]
- Krauss, A. Why all randomised controlled trials produce biased results. Ann. Med. 2018, 50, 312–322. [Google Scholar] [CrossRef]
- Dainesi, S.M.; Goldbaum, M. Reasons behind the participation in biomedical research: A brief review. Rev. Bras. Epidemiol. 2014, 17, 842–851. [Google Scholar] [CrossRef]
- Grimes, D.A.; Schulz, K.F. Descriptive studies: What they can and cannot do. Lancet 2002, 359, 145–149. [Google Scholar] [CrossRef]
- Kuchar, E. The importance of case reports in current pediatric endocrinology and metabolism literature—The analysis of publications indexed in Medline in the years 2004–2009. Pediatr. Endocrinol. Diabetes Metab. 2010, 16, 119–122. [Google Scholar]
- Gopikrishna, V. A report on case reports. J. Conserv. Dent. 2010, 13, 265–271. [Google Scholar] [CrossRef]
- Yuan, Q.-L.; Wang, P.; Liu, L.; Sun, F.; Cai, Y.-S.; Wu, W.-T.; Ye, M.-L.; Ma, J.-T.; Xu, B.-B.; Zhang, Y.-G. Acupuncture for musculoskeletal pain: A meta-analysis and meta-regression of sham-controlled randomized clinical trials. Sci. Rep. 2016, 6, 30675. [Google Scholar] [CrossRef]
- Filshie, J.; White, A.; Cummings, M. Medical Acupuncture: A Western Scientific Approach, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Han, J.-S. Acupuncture and endorphins. Neurosci. Lett. 2004, 361, 258–261. [Google Scholar] [CrossRef]
- Cheng, K.J. Neurobiological Mechanisms of Acupuncture for Some Common Illnesses: A Clinician’s Perspective. J. Acupunct. Meridian Stud. 2014, 7, 105–114. [Google Scholar] [CrossRef]
- Pirnia, B.; Bazargan, N.M.; Hamdieh, M.; Pirnia, K.; Malekanmehr, P.; Maleki, F.; Zahiroddin, A. The Effectiveness of Auricular Acupuncture on the Levels of Cortisol in a Depressed Patient. Iran. J. Public Health 2019, 48, 1748–1750. [Google Scholar] [PubMed]
- Hui, K.K.; Marina, O.; Liu, J.; Rosen, B.R.; Kwong, K.K. Acupuncture, the limbic system, and the anticorrelated networks of the brain. Auton. Neurosci. 2010, 157, 81–90. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Vickers, A.; Bland, M.; Torgerson, D.; Corbett, M.S.; Spackman, E.; Saramago, P.; Woods, B.; Weatherly, H.; Sculpher, M.; et al. Acupuncture for chronic pain and depression in primary care: A programme of research. Program. Grants Appl. Res. 2017, 5, 1–316. [Google Scholar] [CrossRef]
- Cui, C.-L.; Wu, L.-Z.; Luo, F. Acupuncture for the Treatment of Drug Addiction. Neurochem. Res. 2008, 33, 2013–2022. [Google Scholar] [CrossRef]
- Huang, Q.; Luo, D.; Chen, L.; Liang, F.X.; Chen, R. Effectiveness of Acupuncture for Alzheimer’s Disease: An Updated Systematic Review and Meta-analysis. Curr. Med Sci. 2019, 39, 500–511. [Google Scholar] [CrossRef] [PubMed]
- MacIntyre, K.; Gomes, B.; MacKenzie, S.; D’Angelo, K. Conservative management of an elite ice hockey goaltender with femoroacetabular impingement (FAI): A case report. J. Can. Chiropr. Assoc. 2015, 59, 398–409. [Google Scholar]
- Lin, K.; Tung, C. Acupuncture for Recovery from Pediatric Sport-Related Concussion. Med Acupunct. 2016, 28, 217–222. [Google Scholar] [CrossRef]
- Garlanger, K.L.; Fredericks, W.H.; Do, A.; Bauer, B.A.; Laskowski, E.R. The Feasibility and Effects of Acupuncture in an Adolescent Nordic Ski Population. PM R 2017, 9, 795–803. [Google Scholar] [CrossRef]
- Luetmer, M.T.; Do, A.; Canzanello, N.C.; Bauer, B.A.; Laskowski, E.R. The Feasibility and Effects of Acupuncture on Muscle Soreness and Sense of Well-being in an Adolescent Football Population. Am. J. Phys. Med. Rehabil. 2019, 98, 964–970. [Google Scholar] [CrossRef]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef]
- Mitchell, J.H.; Haskell, W.L.; Raven, P.B. Classification of sports. J.Am. Coll. Cardiol. 1994, 24, 864–866. [Google Scholar] [CrossRef]
- Dlin, R.A.; Benmair, J.; Hanne, N. Pain Relief in Sports Injuries—Application of TENS to Acupuncture Points. Int. J. Sports Med. 1980, 1, 203–206. [Google Scholar] [CrossRef]
- Sternfeld, M.; Finkelstein, Y.; Eliraz, A.; Hod, I. Runner’s stitch syndrome successfully treated by acupuncture. Am. J. Acupunct. 1992, 20, 213–215. [Google Scholar]
- Seplow, W. Management of Lateral Meniscus Injury. Sports Chiropr. Rehabil. 1996, 10, 86–88. [Google Scholar]
- Hoven, J.; Snyder, R.; Andrew, T. Management of peroneal nerve entrapment in an elite skier: A case report. J. Sports Chiropr. Rehabil. 2000, 14, 70–74. [Google Scholar]
- Rosted, P. Acupuncture for treatment of the yips?—A case report. Acupunct. Med. 2005, 23, 188–189. [Google Scholar] [CrossRef]
- Young, K. Sports Injuries and TCM. J. Chin. Med. 2005, 78, 1–10. [Google Scholar]
- Martinez-Silvestrini, J.A.; Micheo, W.F. Complex regional pain syndrome in pediatric sports: A case series of three young athletes. Boletín la Asoc Médica Puerto Rico 2006, 98, 31–37. [Google Scholar]
- Chen, Y.Z.; Xu, Y.; Yang, W.B.; Lu, Y.H.; Fang, H.B. Observation on therapeutic effect of catgut implantation at acupoints on exercise fatigue and study on the mechanism. Zhongguo Zhen Jiu 2008, 28, 656–658. [Google Scholar]
- Yan, X.N.; Ren, C.X. Cause and treatment of sports injury in knee joint medial collateral ligament. Zhongguo Zuzhi Gongcheng Yanjiuyu Linchuang Kangfu 2008, 12, 5567–5570. [Google Scholar]
- Osborne, N.J.; Gatt, I.T. Management of Shoulder Injuries Using Dry Needling in Elite Volleyball Players. Acupunct. Med. 2010, 28, 42–45. [Google Scholar] [CrossRef]
- Donoyama, N.; Hotoge, S.; Ohkoshi, N. Acupuncture Might Have Contributed to Improving Amenorrhoea in a Top Athlete. Acupunct. Med. 2011, 29, 304–306. [Google Scholar] [CrossRef] [PubMed]
- Yuill, E.A.; Pajaczkowski, J.A.; Howitt, S.D. Conservative care of sports hernias within soccer players: A case series. J. Bodyw. Mov. Ther. 2012, 16, 540–548. [Google Scholar] [CrossRef]
- Morimoto, Y.; Saito, A.; Tokuhashi, Y. Low level laser therapy for sports injuries. Laser Ther. 2013, 22, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Pearcey, G.E.P.; Bradbury-Squires, D.J.; Power, K.E.; Behm, D.G.; Button, D.C. Exertional Rhabdomyolysis in an Acutely Detrained Athlete/Exercise Physiology Professor. Clin. J. Sport Med. 2013, 23, 496–498. [Google Scholar] [CrossRef]
- Woitzik, E.; Kissel, J. Ganglion cyst of the foot treated with electroacupuncture: A case report. J. Can. Chiropr. Assoc. 2013, 57, 310–315. [Google Scholar]
- Abe, G.C.; Yonamine, B.T.S.; Mello, C.A.D.S.; Ramos, P.E.; Conde, M.S.; Oliveira, A.S.B. Acupuncture for Treating Persistent Pain in Brazilian Para-Athletes. Med Acupunct. 2014, 26, 50–56. [Google Scholar] [CrossRef]
- Gliedt, J.A.; Daniels, C.J. Chiropractic management of elbow tendinopathy following a sports related trauma. J. Can. Chiropr. Assoc. 2014, 58, 52–57. [Google Scholar]
- Jayaseelan, D.J.; Moats, N.; Ricardo, C.R. Rehabilitation of Proximal Hamstring Tendinopathy Utilizing Eccentric Training, Lumbopelvic Stabilization, and Trigger Point Dry Needling: 2 Case Reports. J. Orthop. Sports Phys. Ther. 2014, 44, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Kleinhenz, J.; Streitberger, K.; Windeler, J.; Güssbacher, A.; Mavridis, G.; Martin, E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain 1999, 83, 235–241. [Google Scholar] [CrossRef]
- Kamali, F.; Sinaei, E.; Morovati, M. Comparison of Upper Trapezius and Infraspinatus Myofascial Trigger Point Therapy by Dry Needling in Overhead Athletes With Unilateral Shoulder Impingement Syndrome. J. Sport Rehabil. 2019, 28, 243–249. [Google Scholar] [CrossRef]
- Callison, M. Clinical study: Acupuncture & tibial stress syndrome (Shin splints). J. Chin. Med. 2002, 70, 24–28. [Google Scholar]
- Karagounis, P.; Tsironi, M.; Prionas, G.; Tsiganos, G.; Baltopoulos, P. Treatment of plantar fasciitis in recreational athletes: Two different therapeutic protocols. Foot Ankle Spec. 2011, 4, 226–234. [Google Scholar] [CrossRef]
- Timpka, T.; Jacobsson, J.; Bickenbach, J.; Finch, C.F.; Ekberg, J.; Nordenfelt, L. What is a sports injury? Sports Med. 2014, 44, 423–428. [Google Scholar] [CrossRef]
- Joseph, C.W.; Finch, C.F. Sports Injuries. International Encyclopedia of Public Health, 2nd ed.; Quah, S.R., Cockerham, W.C., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 79–86. [Google Scholar]
- Renström, P.; Johnson, R.J. Overuse injuries in sports. A review. Sports Med. 1985, 2, 316–333. [Google Scholar] [CrossRef]
- Crockett, B. Rehabilitation of the athlete. Mo. Med. 2011, 108, 173–175. [Google Scholar]
- Babatunde, O.O.; Jordan, J.L.; Van der Windt, D.A.; Hill, J.C.; Foster, N.E.; Protheroe, J. Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PLoS ONE 2017, 12, e0178621. [Google Scholar] [CrossRef]
- Mehallo, C.J.; Drezner, J.A.; Bytomski, J.R. Practical management: Nonsteroidal antiinflammatory drug (NSAID) use in athletic injuries. Clin. J. Sport Med. 2006, 16, 170–174. [Google Scholar] [CrossRef]
- Jeon, M.S.; Bae, S.Y. The Study of Athlete Patients Visited Korean Medical Clinic in CheongJu-Gym at the 2016 CheongJu World Martial Arts. J. Sports Korean Med. 2016, 16, 51–56. [Google Scholar]
- Oh, M.J.; Son, I.M.; Shin, J.M.; Cho, J.H. The Study of Patients Visited Korean Medical Clinic in Athletes’ Village Hospital at The 28th Univesiade Gwanju Korea. J. Sports Korean Med. 2016, 16, 1–7. [Google Scholar]
- Yang, C.; Lee, E.; Hwang, E.H.; Kwon, O.; Lee, J.H. Management of Sport Injuries with Korean Medicine: A Survey of Korean National Volleyball Team. Evid. Based Complement. Alternat. Med. 2016, 2016, 1–7. [Google Scholar] [CrossRef]
- Kim, D.S.; Lee, Y.H.; Bae, K.S.; Baek, G.H.; Lee, S.Y.; Shim, H.; On, M.G.; Rhie, S.J.Y. PyeongChang 2018 Winter Olympic Games and athletes’ usage of ‘polyclinic’ medical services. BMJ Open Sport Exerc. Med. 2019, 5, e000548. [Google Scholar] [CrossRef]
- Araujo, C.G.; Scharhag, J. Athlete: A working definition for medical and health sciences research. Scand. J. Med. Sci. Sports 2016, 26, 4–7. [Google Scholar] [CrossRef]
- Chang, W.D.; Chang, N.J.; Lin, H.Y.; Wu, J.H. Effects of Acupuncture on Delayed-Onset Muscle Soreness: A Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2020, 2020, 5864057. [Google Scholar] [CrossRef]
| Study | Demographic Information | Main Concerns and Symptoms of the Patient | Medical History | Administration of Intervention | Follow-up and Outcomes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Study ID | Coun. (Lang) | Sports type | Age (yr) | No. of Cases | Disorders | Duration | Previous Interventions | ① Interventions ② Duration ③ No. of sessions | Outcome measures | Results | Adverse events | ① Return to play ② Recurrence (f/u) | Authors’ comments for acupuncture treatments |
| Diseases of the musculoskeletal system and connective tissue | ||||||||||||||
| 1 | Dlin, 1980 [33] | Israel (Eng.) | ND | 12–44 (mean = 2(5) | 22 | Musculotendinous syndromes of the chronic exertion type (shoulder, knee, anterior tibia, back pain) | Few wks-several mon | At least a 2 to 3 wk period: [all patients] heat application, rest; [as needed] oral anti-inflammatory medication (indomethacin), physiotherapy (ultrasound, or local steroid injections) | ① TENS ② ND ③ 2–6 | (1) Pain questionnaire (2) Pain grade | (1) Complete pain relief (n = 1(5), good (>50% reduction) (n = (4), fair (30–50% reduction) (n = (1), poor (<30% reduction) (n = (2) (2) Grade 0 (n = 17), 2 grades reduction (good result) (n = (2), 1 grade reduction (fair result) (n = (1), No changes (n = (2) | None | ① 18 of 22 subjects returned to full sports activity ② 10-day-2-mon after return to full sports activity (n = 6) | TENS stimulation of acupuncture points may be effective in the therapy of painful sports injuries of the athletic exertion type. |
| 2 | Sternfeld, 1992 [34] | Israel (Eng.) | Long-distance running | 16 | 1 | Runner’s stitch syndrome | Several mon | Analgesics and NSAIDs | ① MA ② 31-day [1/day (3-day)+1/wk (4-wk)] ③ 7 | Symptoms | Complete and permanent recovery | ND | ① Resuming all activities and achievements in competitive sports ② None (several wks) | We suggest acupuncture as a preferred therapy for cases involving runner’s stitch syndrome. |
| 3 | Seplow, 1996 [35] | USA (Eng.) | Basketball | 17 | 1 | Lateral meniscus injury (a tear of the posterior horn of the lateral meniscus) | 3-day | Ice, rest, NSAIDs (2-day) | ① EA + others ② Initial 2-wk ③ ND | Symptoms | Walk without limp or pain and range of knee flexion returned to 130° | ND | ① Return to training in 5-wks, full participation in 8-wks ② ND | When tears are diagnosed, conservative methods may be effective in treating these athletes and may in fact be more effective in many cases. |
| 4 | Hoven, 2000 [36] | USA (Eng.) | Ski | 19 | 1 | Peroneal nerve entrapment and ankle sprain | ND | Pelvic/lower extremity chiropractic manipulation, interferential current, cryotherapy (3-day) | ① MA + others ② 5-day ③ 5 | Symptoms | Pain and weakness alleviated after 3-day of care | ND | ①, ② ND | It appears that chiropractic manipulation of the lumbar, pelvis and lower extremity, combined with interferential current, cryotherapy, acupuncture and trigger point therapy played a significant role in alleviating the peroneal neuropathy experienced by this elite junior national skier. |
| 5 | Young, 2005 [38] | UK (Eng.) | Rugby | #1: 19; #2: 32 | 2 | #1: Calf strain/mild chronic compartment syndrome; #2: Tennis elbow/muscle tightness | #1: 6-mon; #2: ND | ND | ① EA + MA + others ② #1: 6-wk #2: 4-wk (2/wk) ③ #1: 12; #2: 8 | Symptoms | #1: Completion of the full training without pain #2: Training at ease | ND | ① #1: Playing games without pain; #2: Playing at ease ② ND | Even though using acupuncture is very effective in treatment, there comes a time in the treatment of an injury when you will need to open the channels physically to allow qi and blood to flow smoothly and to return the shortened muscle back to its normal length. |
| 6 | Martínez-Silvestrini, 2006 [39] | Puerto Rico (Eng.) | ND | 11 | 1 * | CRPS after lower extremity trauma and clinical depression | Few wks | (For CRPS treatment) Hydrotherapy, electrical stimulation, ultrasound to the Achilles tendon, stretching, active assisted range of motion, weight bearing, opioid analgesics, corticosteroids | ① MA + others ② 3-mon ③ ND | Symptoms | The clinics discharge without any deficits | ND | ①, ② ND | ND |
| 7 | Yan, 2008 [41] | China (Chin.) | Football | Mean = 21 | 19 ** | Sports injury in knee joint medial collateral ligament | ND | ND | ① EA + others ② ND (one course comprised 7-day) ③ ND | (1) Recovery time (2) Therapeutic effect (3) The overall efficiency | (1) Rapid (23%); moderate (50%) (2) Recovered (40%); partly recovered (53%) (3) 93% | ND | ①, ② ND | ND |
| 8 | Osborne, 2010 [42] | UK (Eng.) | Volleyball | 23–27 (mean = 2(5) | 4 | Anterior/anterolateral shoulder pain (1) | #1: 2 mon.; #2: 6 yr.; #3: 18 mon.; #4: 6-mon | Conservative treatment (#1: Thera band, stretching; #2, #3: ND; #4: exercises, stretching) | ① MA + others ② 1-mon-long intense competitive phase ③ #1, #3, #4: 1; #2: 2 | (1) Functional assessment (MPQ) (2) ROM (3) Verbal pain scores (4) Muscle strength | (1)-(4) All scores improved | ND | ① Continuing overhead activities ② ND | These cases support the use of dry needling in elite athletes during a competitive phase with short-term pain relief and improved function in shoulder injuries. |
| 9 | Pearcey, 2013 [46] | Canada (Eng.) | ND | 31 | 1 | Exertional rhabdomyolysis | Few days | Intravenous hydration with sodium bicarbonate and blood work [3 days] | ① MA + others ② 2 day ③ ND | CK levels | Declined by 45% | ND | ① 1 mon. after the diagnosis, the subject slowly returned to high-intensity resistance training (>2/wk.) without any complications ② ND | ND |
| 10 | Woitzik, 2013 [47] | Canada (Eng.) | Cycle | 45 | 1 | Ganglion cyst of the foot | 10-day | ND | ① EA ② 4-wk (1/wk) ③ 4 | Symptoms | Resolution of the cyst (11 day after final treatment) | ND | ①, ② ND | EA may be a novel and non-invasive conservative approach for the treatment of ganglion cysts. |
| 11 | Morimoto, 2013 [45] | Japan (Eng.) | Various sports (2) | 17–77 (mean = 39) | 41 | Jumper’s knee, lateral/medial epicondylitis, Achilles tendinitis, adductor muscle injury, rotator cuff injuries, etc.(3) | ND | ND | ① LA + others ② ND ③ 2–10 (mean = 4.(1) | Pain Relief Score | 5 or less (n = 27,66%) | ND | ①, ② ND | Low-level LA is an effective treatment for sports injuries, particularly jumper’s knee, tennis elbow and Achilles tendinitis. |
| 12 | Gliedt, 2014 [49] | USA (Eng.) | Basketball | 41 | 1 | Sub-acute left elbow tendinopathy | 5 wk | Self-massage, OTC NSAIDs | ① MA + others ② ND (1/wk) ③ 2 | Symptoms | Reduced left elbow swelling and left wrist extensor muscle hypertonicity, and no pain | ND | ① A return to normal recreational athletic activities including basketball ② None (6-wk) | The patient’s outcomes indicated a quick resolution of subjective complaints and objective findings with the chosen treatment. |
| 13 | Jayaseelan, 2014 [50] | USA (Eng.) | Running | #1: 70; #2: 69 | 2 | Proximal hamstring tendinopathy | #1: 7 mon; #2: 5 mon | Eccentric training of hamstrings, lumbopelvic stabilization exercises, patient education (2-wk: “Phase 1” treatment) | ① MA + others ② #1: 3 wk; #2: 4 wk (“Phase 2” treatment) (1/wk) ③ 3 | (1) Pain (NRS) (2) Global rating of change (3) Lower Extremity Functional Scale (4) Tenderness (5) Strength | (1)–(5) All score improvement, significant function improvement | ND | ① Each patient returned to running and sitting without symptoms ② None (6 mon) | In these 2 runners, eccentric loading of the hamstrings, lumbopelvic stabilization exercises, and trigger point dry needling provided short- and long-term pain reduction and functional benefits. |
| 14 | MacIntyre, 2015 [27] | Canada (Eng.) | Ice hockey | 22 | 1 | FAI | 4 yr | None | ① EA + others ② 6-wk (1–2/wk) ③ 8 | Symptoms | No pain [at rest, daily activities (including exercise), all stress tests used for initial physical examination]; despite having less pain, the hip scour and FADIR tests still provided a hard end-feel and palpable click at extreme ROM | ND | ① At 8 wk ② None (6 mon) | Conservative management utilizing a multimodal approach, as described in the case, should be first line treatment. |
| Exercise-induced fatigue | ||||||||||||||
| 15 | Chen, 2008 [40] | China (Chin.) | Rowing, track and field, swimming, table tennis (4) | 15–26 (mean = 20) | 41 | Exercise-induced fatigue | N/A | N/A | ① Catgut embedding ② 90–120 day ③ 6 | (1) Training-related condition (2) Changes level of blood testosterone and hemoglobin | (1) Significantly improved (2) Significantly increased | ND | ①, ② N/A | Catgut implantation at acupoints can significantly improve exercise fatigue in the player and the mechanism is possibly related with increase of testosterone and hemoglobin levels. |
| 16 | Garlanger, 2017 [29] | USA (Eng.) | Nordic ski | 14–17 | 15 | Exercise-related DOMS and sense of well-being | N/A | N/A | ① MA + others ② 2 wk ③ 1–5 | (1) Time required by research staff on treatment days (2) Cost (3) AEs (4) Participant/provider ratio (5) Effect on DOMS 6) Effect on sense of well-being | (1) 90 min (2) 1500 USD (3) (See next column) (4) 7:1 (5) significantly improved (p < 0.05) 6) NS | No severe AEs; Minor AEs (73%, site pain, etc.) | ①, ② N/A | Providing acupuncture to adolescent Nordic ski athletes in the practice field under extreme temperature is feasible with the appropriate resources. |
| 17 | Luetmer, 2019 [30] | USA (Eng.) | Football | 13–18 (mean = 16) | 42 | Exercise-related DOMS and sense of well-being | N/A | N/A | ① MA + others ② 5-day ③ 5 (n = 1(1); 4 (n = 1(3); 3 (n = 8); 2 (n = 6); 1 (n = (4) | Same as above | (1) 75 min (2) 700 USD (3) (See next column) (4) 7–10:1 (5) significantly improved (p < 0.001) (6) NS | No severe AEs; Minor AEs (55%, mild focal numbness or tingling) | ①, ② N/A | Effectively providing acupuncture to multiple adolescent football players in their training environment is feasible with appropriate staff and resources. |
| Others | ||||||||||||||
| 18 | Abe, 2014 [48] | Brazil (Eng.) | Various sports (Paralympic athletes) (5) | Mean = 35 | 7 | Persistent pain (shoulder, elbow, spine, or knee) (6) | #1: 4-wk; #2-#4, #6: chronic, intermittent; #5: 2-wk; #7: 8-wk | Oral/topical NSAIDs, muscle relaxant, physiotherapy, immobilization (7) | ① MA + others ② 6 wk (2/wk) ③ 12 | (1) Pain (VAS) (2) Pain (MPQ) | (1), (2) Significant pain reduction | No severe AEs; Minor AEs (episodic local bleeding); One athlete died of liver cancer after this study | ①, ② ND | Pain symptoms were reduced with acupuncture. The mean duration required for improvement was eight acupuncture sessions. |
| 19 | Lin, 2016 [28] | USA (Eng.) | #1: Ice hockey #2: Field hockey and lacrosse #3: Soccer | #1: 8; #2: 15; #3: 18 | 3 | Sport-related postconcussive symptoms | #1,#2: 1 mon; #3: 1.5 mon | Physical therapy, medications (8) | ① MA + EA + others ② #1, #2, 6-wk; #3, 14-wk (1/wk) ③ #1, #2, 6; #3, 14 | (1) Pain (VAS) (2) Pain (BPI) (3) Postconcussive symptoms questionnaire | (1)-(3) Satisfactory symptomatic reduction in all patients | None | ① #1, #2: ND; #3: Return to all sports activities (All patients returned to their physical, social, and school activities) ② ND | Acupuncture with conventional medication appeared to reduce the postconcussive symptoms in the 3 patients. |
| 20 | Yuill, 2012 [44] | Canada (Eng.) | #1: Soccer #2, #3: Soccer and hockey | #1: 23; #2: 18; #3: 29 | 3 | Sports hernia (chronic groin pain) | #1: 5 wk; #2: 3-mon; #3: 5-wk | #1: None; #2: Ice, interferential current, ultrasound (2 mon); #3: Physiotherapy, adductor stretching/strengthening, interferential current, ultrasound | ① MA + EA + others ② 6–8-wk (1–2/wk) ③ 6–16 | (1) Pain (VAS) (2) Resisted muscle testing | (1) 0/10 in all cases at the time of patient discharge (2) All positive tests changed to negative | ND | ① Within 3–4 days of last therapy ② None (2 yr) | Three soccer players, of varying levels of ability, presenting with a suspected sports hernia were relieved of their pain after 8 weeks of conservative care. |
| 21 | Donoyama, 2011 [43] | Japan (Eng.) | Middle- and long- distance running | 26 | 1 | Amenorrhoea | Several mon | A norgestrel-ethinyl estradiol combination (2-wk] | ① MA + others ② 13 mon ③ 46 | (1) Menstrual blood flow (2) Basal Body Temperature (3) Body Weight (4) Body Fat Rate (5) BMI | (1) Amount and duration of menstrual flow increased at regular intervals (2) Moved close to the biphasic pattern (3)-(5) NS | ND | ①, ② ND | Acupuncture treatment may be a feasible treatment option in the field of sports medicine to help competitive athletes with amenorrhoea. |
| 22 | Rosted, 2005 [37] | UK (Eng.) | Golf | 65 | 1 | Yips | 2 yr | None | ① MA ② Few weeks (1/wk+1/2-wk) ③ 8 | Symptoms | Symptoms disappeared after 1 treatment | ND | ① Playing golf using his right hand without symptoms ② None (2 yr) | Acupuncture may be worth trying in patients with the yips since this condition is otherwise difficult to treat. |
| No. | Study ID | Sports Type | Disorders | Details of Acupuncture (Acupuncture Sites) | Co-Intervention |
|---|---|---|---|---|---|
| Diseases of the musculoskeletal system and connective tissue | |||||
| 1 | Dlin, 1980 [33] | ND | Musculotendinous syndromes of the chronic exertion type (shoulder, knee, anterior tibia, and back pain) | TENS (MTrPs or acupoints) | None |
| 2 | Sternfeld, 1992 [34] | Long-distance running | Runner’s stitch syndrome | MA (PC3, LR14, ST36, SP9, LR2, SP3) | None |
| 3 | Seplow, 1996 [35] | Basketball | Lateral meniscus injury (a tear of the posterior horn of the lateral meniscus) | EA (ST41, GB43, BL54, BL60) | Ice, kinesiology, resistance bands |
| 4 | Hoven, 2000 [36] | Ski | Peroneal nerve entrapment and ankle sprain | MA (ST40, GB34, GB35, GB36) | Chiropractic manipulation (lumbar spine, pelvis, lower extremity), interferential current, cryotherapy, soft tissue mobilization |
| 5 | Young, 2005 [38] | Rugby | #1: Calf strain and mild chronic compartment syndrome #2: Tennis elbow and muscle tightness | #1: - EA (BL55-BL57, BL57-GB35) - MA (BL40, BL57, BL58, BL60, BL65, GB34, GB41, LI4) #2: - EA (ashi points, EX-B2 from C3 to L5) - MA (ashi points, GB21, LI15, TE14, TE5, LI10, LI11, LI12, LI5, LI4, LI3, TE3) | #1: Tuina (gun-fa, rolling technique; rou-fa, kneading; plucking (frictions)), stretching, patient education #2: Tuina (gun-fa), cupping (epicondyle) |
| 6 | Martínez-Silvestrini, 2006 [39] | ND | CRPS after lower extremity trauma and clinical depression | (for clinical depression and pain disorder treatment) MA (ND) | (for clinical depression and pain disorder treatment) Fluoxetine (SSRIs) |
| 7 | Yan, 2008 [41] | Football | Sports injury in knee joint medial collateral ligament | EA (EX-LE2, EX-LE5, GB34) | Massage, physiotherapy, cold pack, electric stimulation, external preparation, surgery, splint, rehabilitation training (as needed) |
| 8 | Osborne, 2010 [42] | Volleyball | Anterior/anterolateral shoulder pain | MA (MTrPs: scapulohumeral muscles) | Soft tissue therapy around the shoulder, post-training icing strategies, exercises and stretching |
| 9 | Pearcey, 2013 [46] | ND | Exertional rhabdomyolysis | MA (from shoulder to hand) | Intravenous hydration with sodium bicarbonate and blood work |
| 10 | Woitzik, 2013 [47] | Cycle | Ganglion cyst of the foot | EA (ST36, LR3, 2 needles inserted into the cyst on opposite sides stimulated at 5 Hz) | None |
| 11 | Morimoto, 2013 [45] | Various sports | Jumper’s knee, lateral epicondylitis of humerus, Achilles tendinitis, adductor muscle injury, medial epicondylitis of humerus, rotator cuff injuries, etc | LA (low level laser therapy at points of pain/or acupuncture points) | Medication (NSAIDs) or a poultice (as needed) |
| 12 | Gliedt, 2014 [49] | Basketball | Sub-acute left elbow tendinopathy | MA (palpated areas of tenderness, just distal to the insertion site of the common wrist extensor muscles) | HVLA spinal manipulation (thoracic spine), ART (elbow), home exercise program (Brugger’s exercises for postural dysfunction) |
| 13 | Jayaseelan, 2014 [50] | Running | Proximal hamstring tendinopathy | MA (MTrPs: medial/lateral hamstrings, adductor magnus muscle) | Eccentric training of hamstrings, lumbopelvic stabilization exercises, patient education |
| 14 | MacIntyre, 2015 [27] | Ice hockey | FAI | EA (2 Hz, L2-L5 bilaterally, and hip muscles and nerves, SP12, LR10, GB29, BL53, BL54) | Soft tissue therapy, spinal manipulative therapy, MWM and rehabilitation exercises |
| Exercise-induced fatigue | |||||
| 15 | Chen, 2008 [40] | Rowing, track and field, swimming, table tennis | Exercise-induced fatigue | Catgut embedding (CV4, BL23, GV4, ST36, SP6 and etc.) | None |
| 16 | Garlanger, 2017 [29] | Nordic ski | Exercise-related DOMS and sense of well-being | MA (when underlying muscle soreness occurred: SP10, ST34, SP9, ST36, GB34, BL56; if no specific muscle soreness: ST36, GB34, ST34) | NSAIDs (24–48 h prior to the study, n = 6; between treatment days 2 and 3, n = 3; between treatment days 4 and 5, n = 1) |
| 17 | Luetmer, 2019 [30] | Football | Exercise-related DOMS and sense of well-being | MA (when underlying muscle soreness occurred: SP10, ST34, SP9, ST36, GB34, BL56; if no specific muscle soreness: ST36, GB34, ST34) | NSAIDs or acetaminophen (before day 1, n = 7; between day 1 and 2, n = 7; between days 2 and 3, n = 10; between days 3 and 4, n = 8; between days 4 and 5, n = 9) |
| Others | |||||
| 18 | Abe, 2014 [48] | Various sports (Paralympic athletes) | Persistent pain (shoulder, elbow, spine, or knee) | MA (CV12, CV3, LI4, LU7, HT7, SP10, ST36, LR2, KI3) | The training schedule and the usual treatment regimens maintained |
| 19 | Lin, 2016 [28] | Ice hockey, field hockey, lacrosse, soccer | Sport-related postconcussive symptoms | - MA (#1: LI4, ST36, LR3, TE5, Ashi points; #2: LI4, ST36, LR3, TE5, SP6, Yin-Tang, Ashi points; #3: LI4, ST36, SP6, LR3, TE23, GV20, Yin-Tang, TE5, LI11, ST7, BL4, BL6, TE9, GB21, GB20, Ashi points) - EA(2-Hz, ST 36) | Cupping (Back Shu points), Gua sha (Back Shu points, treatment involving repeated pressured strokes over body surface with a smooth edged tool), conventional medical therapies maintained |
| 20 | Yuill, 2012 [44] | Soccer, hockey | Sports hernia (chronic groin pain) | - EA (2 Hz, L2-L4, T10-T12 bilaterally) - MA (#1: SP 13, ST 29, ST30, KI11, GB28 #2: ST29, ST30, LR9, LR10 #3: ST30, LR10) | Soft tissue therapy, laser therapy and microcurrent (site of the chief complaint), stretching, Wobenzyme (2400mg tabs, 2/day, 2 weeks), rehabilitation therapy, plyometric training (3/week, 8 weeks) |
| 21 | Donoyama, 2011 [43] | Middle- and long- distance running | Amenorrhoea | MA (CV6, CV12, LR3, LR14, BL17, BL18, BL23, SP6, SP10) | A norgestrel-ethinyl estradiol combination (as needed) |
| 22 | Rosted, 2005 [37] | Golf | Yips | MA (GV20, EX-HN-1, TE5) | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-W.; Lee, J.-H.; Kim, S.-Y. Use of Acupuncture for the Treatment of Sports-Related Injuries in Athletes: A Systematic Review of Case Reports. Int. J. Environ. Res. Public Health 2020, 17, 8226. https://doi.org/10.3390/ijerph17218226
Lee J-W, Lee J-H, Kim S-Y. Use of Acupuncture for the Treatment of Sports-Related Injuries in Athletes: A Systematic Review of Case Reports. International Journal of Environmental Research and Public Health. 2020; 17(21):8226. https://doi.org/10.3390/ijerph17218226
Chicago/Turabian StyleLee, Ji-Won, Jun-Hwan Lee, and Song-Yi Kim. 2020. "Use of Acupuncture for the Treatment of Sports-Related Injuries in Athletes: A Systematic Review of Case Reports" International Journal of Environmental Research and Public Health 17, no. 21: 8226. https://doi.org/10.3390/ijerph17218226
APA StyleLee, J.-W., Lee, J.-H., & Kim, S.-Y. (2020). Use of Acupuncture for the Treatment of Sports-Related Injuries in Athletes: A Systematic Review of Case Reports. International Journal of Environmental Research and Public Health, 17(21), 8226. https://doi.org/10.3390/ijerph17218226





