The Recovery Benefit on Skin Blood Flow Using Vibrating Foam Rollers for Postexercise Muscle Fatigue in Runners
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
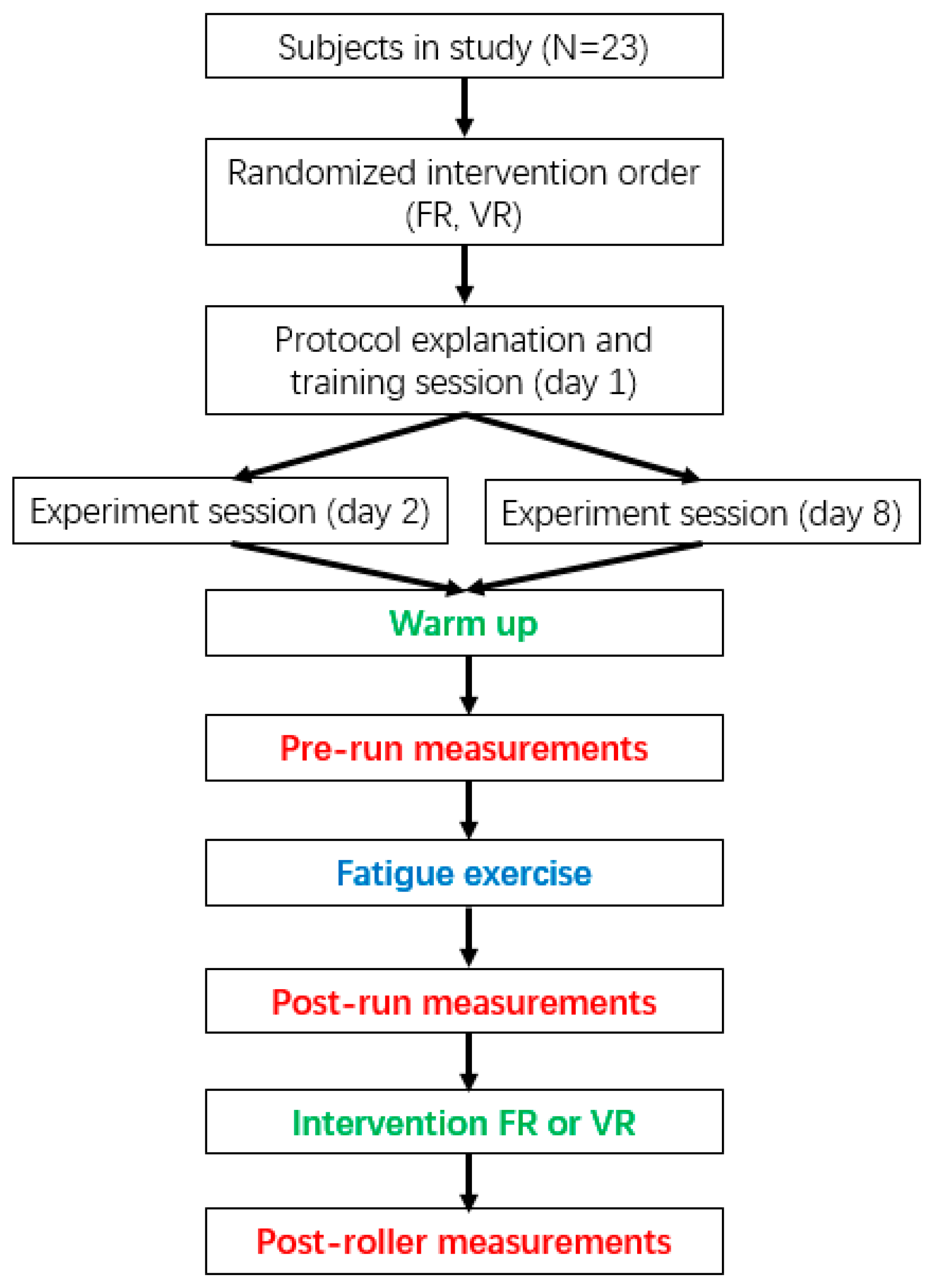
2.2. Examination Protocol
2.3. Examination Instrument and Outcome
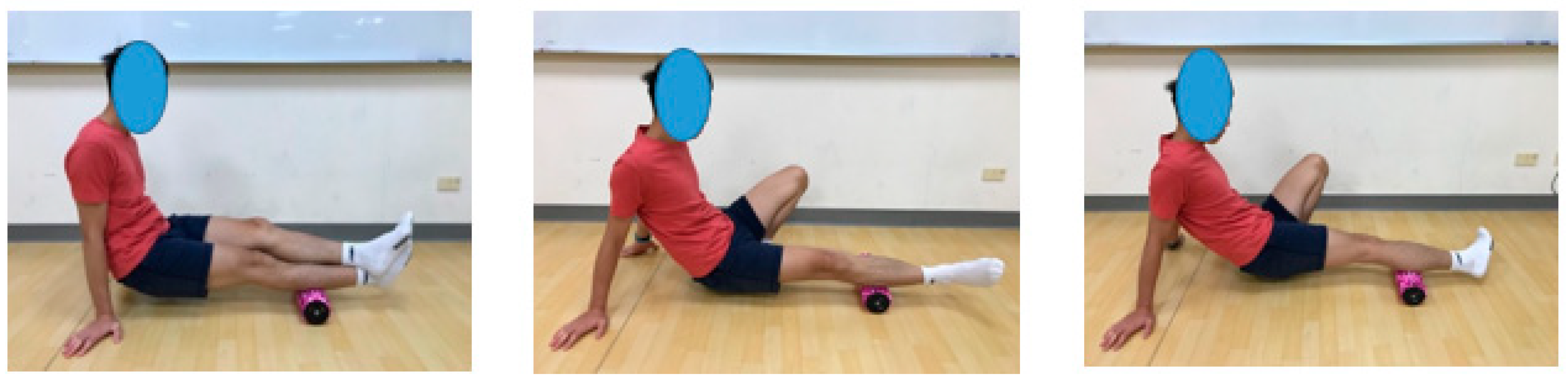
2.3.1. Vibrating Roller Technique
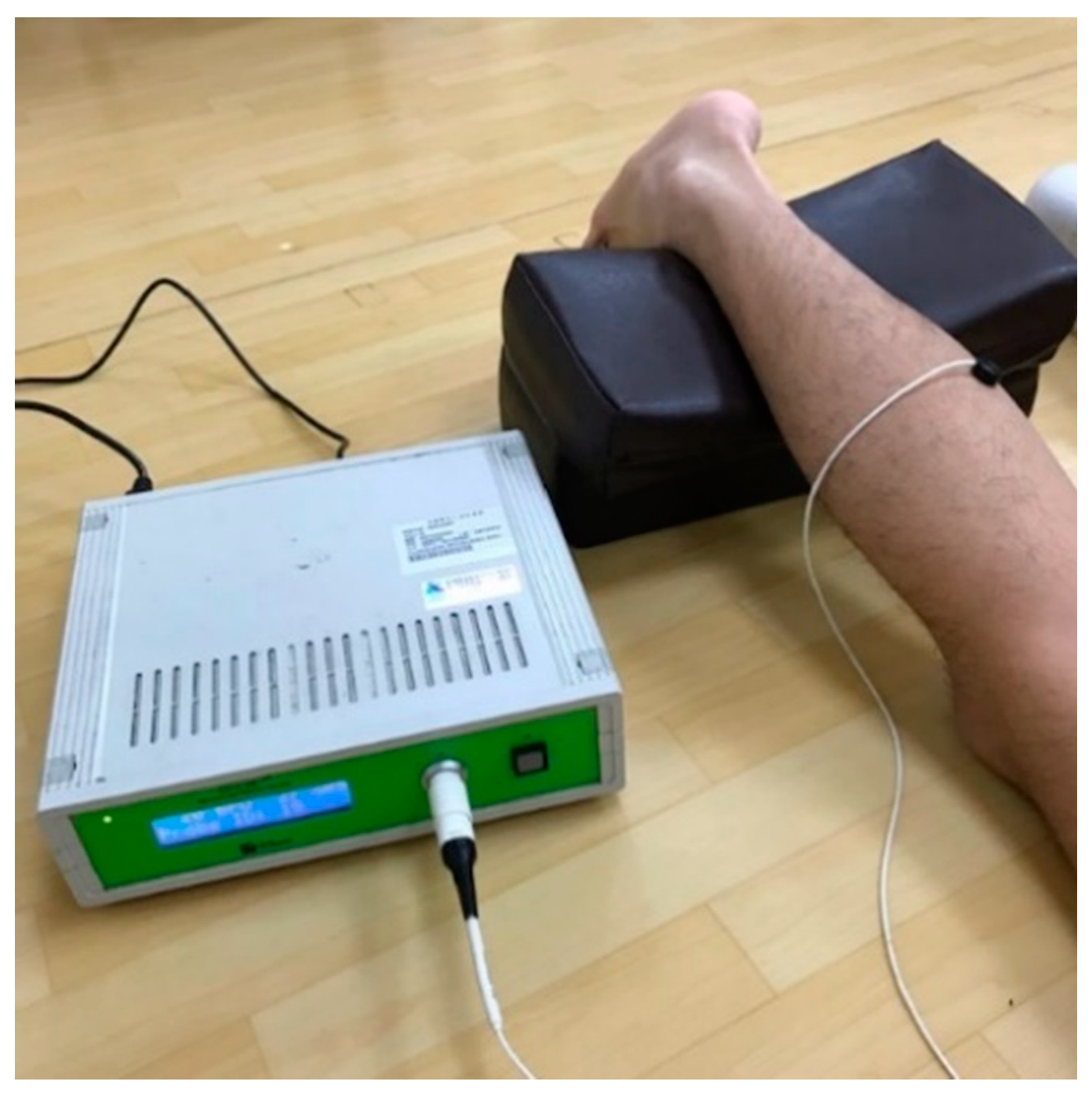
2.3.2. Laser Doppler Flowmetry
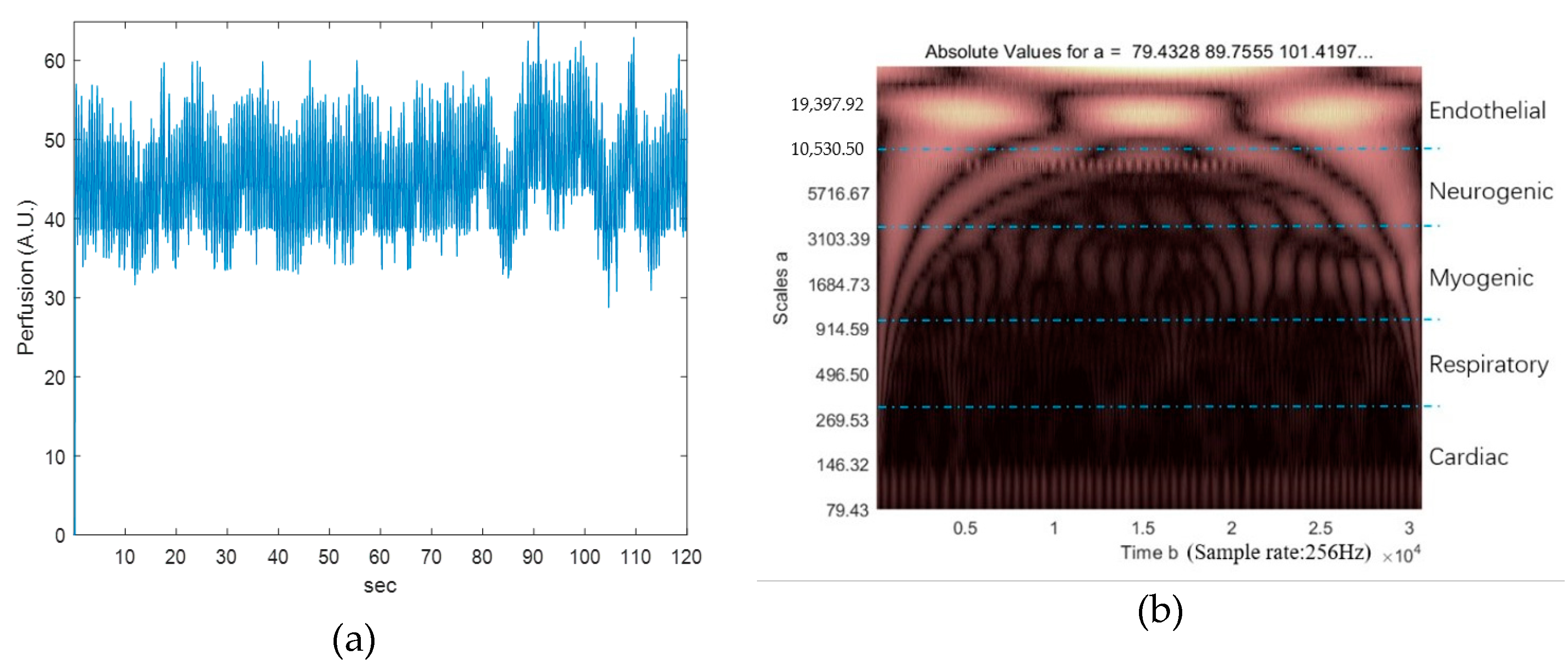
2.3.3. Blood Flow Perfusion and Oscillation Analysis
2.4. Statistical Analysis
3. Results
3.1. Skin Blood Flow Perfusion
3.1.1. Two-Way Repeated-Measures ANOVA and Posthoc Analysis in Skin Blood Flow Perfusion
3.1.2. Analysis of Relative Changes in Normalized Skin Blood Flow Perfusion
3.2. Blood Flow Oscillation
3.2.1. Two-Way Repeated-Measures ANOVA and Posthoc Analysis in Blood Flow Oscillation
3.2.2. The Analysis of Relative Changes in Normalized Blood Flow Oscillation
3.3. Visual Analog Scale (VAS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Allen, D.G.; Lamb, G.D.; Westerblad, H. Skeletal muscle fatigue: Cellular mechanisms. Physiol. Rev. 2008, 88, 287–332. [Google Scholar] [CrossRef]
- Koblbauer, I.F.; Schooten, K.S.V.; Verhagen, E.A.; Dien, J.H.V. Kinematic changes during running-induced fatigue and relations with core endurance in novice runners. J. Sci. Med. Sport 2014, 17, 419–424. [Google Scholar] [CrossRef]
- Gandevia, S.C. Spinal and supraspinal factors in human muscle fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef]
- Portillo-Soto, A.; Eberman, L.E.; Demchak, T.J.; Peebles, C. Comparison of blood flow changes with soft tissue mobilization and massage therapy. J. Altern. Complement. Med. 2014, 20, 932–936. [Google Scholar] [CrossRef] [PubMed]
- Albin, S.R.; Koppenhaver, S.; Bailey, B.; Blommel, H.; Fenter, B.; Lowrimore, C.; Smith, A.C.; McPoil, T.G. The effect of manual therapy on gastrocnemius muscle stiffness in healthy individuals. Foot 2019, 38, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Nunes, G.S.; Bender, P.U.; De Menezes, F.S.; Yamashitafuji, I.; Vargas, V.Z.; Wageck, B.B. Massage therapy decreases pain and perceived fatigue after long-distance Ironman triathlon: A randomised trial. J. Physiother. 2016, 62, 83–87. [Google Scholar] [CrossRef]
- Baumgart, C.; Freiwald, J.; Kühnemann, M.; Hotfiel, T.; Hüttel, M.; Hoppe, M.W. Foam rolling of the calf and anterior thigh: Biomechanical loads and acute effects on vertical jump height and muscle stiffness. Sports 2019, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Behm, D.G.; Wilke, J. Do self-myofascial release devices release myofascia? Rolling mechanisms: A narrative review. Sports Med. 2019, 49, 1173–1181. [Google Scholar] [CrossRef]
- Freiwald, J.; Baumgart, C.; Kühnemann, M.; Hoppe, M.W. Foam-rolling in sport and therapy—Potential benefits and risks: Part 2—Positive and adverse effects on athletic performance. Sports Orthop. Traumatol. 2016, 32, 267–275. [Google Scholar] [CrossRef]
- Hendricks, S.; Hill, H.; Hollander, S.D.; Lombard, W.; Parker, R. Effects of foam rolling on performance and recovery: A systematic review of the literature to guide practitioners on the use of foam rolling. J. Bodyw. Mov. Ther. 2020, 24, 151–174. [Google Scholar] [CrossRef]
- Schroder, J.F.; Lueders, L.; Schmidt, M.; Braumann, K.-M.; Hollander, K. Foam rolling effects on soft tissue tone, elasticity and stiffness in the time course of recovery after weight training. Sports Orthop. Traumatol. 2018, 35, 171–177. [Google Scholar] [CrossRef]
- Poppendieck, W.; Wegmann, M.; Ferrauti, A.; Kellmann, M.; Pfeiffer, M.; Meyer, T. Massage and performance recovery: A meta-analytical review. Sports Med. 2016, 46, 183–204. [Google Scholar] [CrossRef] [PubMed]
- Beardsley, C.; Škarabot, J. Effects of self-myofascial release: A systematic review. J. Bodyw. Mov. Ther. 2015, 19, 747–758. [Google Scholar] [CrossRef] [PubMed]
- Torres, R.; Ribeiro, F.; Duarte, J.A.; Cabri, J.M. Evidence of the physiotherapeutic interventions used currently after exercise-induced muscle damage: Systematic review and meta-analysis. Phys. Ther. Sport 2012, 13, 101–114. [Google Scholar] [CrossRef] [PubMed]
- Fagnani, F.; Giombini, A.; Di Cesare, A.; Pigozzi, F.; Di Salvo, V. The effects of a whole-body vibration program on muscle performance and flexibility in female athletes. Am. J. Phys. Med. Rehabil. 2006, 85, 956–962. [Google Scholar] [CrossRef]
- Imtiyaz, S.; Veqar, Z.; Shareef, M.Y. To compare the effect of vibration therapy and massage in prevention of Delayed Onset Muscle Soreness (DOMS). J. Clin. Diagn. Res. 2014, 8, 133–136. [Google Scholar] [CrossRef]
- Maloney-Hinds, C.; Petrofsky, J.S.; Zimmerman, G. The effect of 30 Hz vs. 50 Hz passive vibration and duration of vibration on skin blood flow in the arm. Med. Sci. Monit. 2008, 14, 112–116. [Google Scholar]
- Kurt, C. Alternative to traditional stretching methods for flexibility enhancement in well-trained combat athletes: Local vibration versus whole-body vibration. Biol. Sport 2015, 32, 225–233. [Google Scholar] [CrossRef]
- García-Gutiérrez, M.T.; Guillén-Rogel, P.; Cochrane, D.J.; Marín, P.J. Cross transfer acute effects of foam rolling with vibration on ankle dorsiflexion range of motion. J. Musculoskelet. Neuronal Interact. 2018, 18, 262–267. [Google Scholar]
- Cheatham, S.W.; Stull, K.R.; Kolber, M.J. Comparison of a vibration roller and a nonvibration roller intervention on knee range of motion and pressure pain threshold: A randomized controlled trial. J. Sport Rehabil. 2019, 28, 39–45. [Google Scholar] [CrossRef]
- Han, S.-W.; Lee, Y.-S.; Lee, N.-J. The influence of the vibration form roller exercise on the pains in the muscles around the hip joint and the joint performance. J. Phys. Ther. Sci. 2017, 29, 1844–1847. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-J.; Chu, I.-H.; Lyu, B.-J.; Chang, W.-D.; Chang, N.-J. Comparison of vibration rolling, nonvibration rolling, and static stretching as a warm-up exercise on flexibility, joint proprioception, muscle strength, and balance in young adults. J. Sports Sci. 2018, 36, 2575–2582. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-H.; Park, C.-B. The immediate effects of foam roller with vibration on hamstring flexibility and jump performance in healthy adults. J. Exerc. Rehabil. 2019, 15, 50–54. [Google Scholar] [CrossRef]
- Lim, J.-H.; Park, C.-B.; Kim, B.-G. The effects of vibration foam roller applied to hamstring on the quadriceps electromyography activity and hamstring flexibility. J. Exerc. Rehabil. 2019, 15, 560–565. [Google Scholar] [CrossRef]
- Lin, W.-C.; Lee, C.-L.; Chang, N.-J. Acute effects of dynamic stretching followed by vibration foam rolling on sports performance of badminton athletes. J. Sports Sci. Med. 2020, 19, 420–428. [Google Scholar] [PubMed]
- Romero-Moraleda, B.; González-García, J.; Cuéllar-Rayo, Á.; Balsalobre-Fernández, C.; Muñoz-García, D.; Morencos, E. Effects of vibration and non-vibration foam rolling on recovery after exercise with induced muscle damage. J. Sports Sci. Med. 2019, 18, 172–180. [Google Scholar] [PubMed]
- De Benito, A.M.; Valldecabres, R.; Ceca, D.; Richards, J.D.; Barrachina-Igual, J.; Pablos, A. Effect of vibration vs non-vibration foam rolling techniques on flexibility, dynamic balance and perceived joint stability after fatigue. PeerJ 2019, 7, e8000. [Google Scholar] [CrossRef] [PubMed]
- Fuller, J.T.; Thomson, R.L.; Howe, P.R.C.; Buckley, J.D. Effect of vibration on muscle perfusion: A systematic review. Clin. Physiol. Funct. Imaging 2012, 33, 1–10. [Google Scholar] [CrossRef]
- Menéndez, H.; Martín-Hernández, J.; Ferrero, C.; Figueroa, A.; Herrero, A.J.; Marín, P.J. Influence of isolated or simultaneous application of electromyostimulation and vibration on leg blood flow. Eur. J. Appl. Physiol. 2015, 115, 1747–1755. [Google Scholar] [CrossRef]
- Lohman, E.B.; Bains, G.S.; Lohman, T.; DeLeon, M.; Petrofsky, J.S. A comparison of the effect of a variety of thermal and vibratory modalities on skin temperature and blood flow in healthy volunteers. Med. Sci. Monit. 2011, 17, 72–81. [Google Scholar] [CrossRef]
- Lohman, E.; Sackiriyas, K.S.B.; Bains, G.S.; Calandra, G.; Lobo, C.; Nakhro, D.; Malthankar, G.; Paul, S. A comparison of whole body vibration and moist heat on lower extremity skin temperature and skin blood flow in healthy older individuals. Med. Sci. Monit. 2012, 18, 415–424. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tzen, Y.-T.; Weinheimer-Haus, E.M.; Corbiere, T.F.; Koh, T.J. Increased skin blood flow during low intensity vibration in human participants: Analysis of control mechanisms using short-time Fourier transform. PLoS ONE 2018, 13, e0200247. [Google Scholar] [CrossRef] [PubMed]
- Zange, J.; Molitor, S.; Illbruck, A.; Müller, K.; Schönau, E.; Kohl-Bareis, M.; Rittweger, J. In the unloaded lower leg, vibration extrudes venous blood out of the calf muscles probably by direct acceleration and without arterial vasodilation. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 114, 1005–1012. [Google Scholar] [CrossRef] [PubMed]
- Cui, R.F.; Luo, S.T.; Lu, L.Q.; Zhou, W.W.; Li, Z.Y. A method for extracting characteristic frequency components of blood flow signals based on wavelet transform. Appl. Mech. Mater. 2013, 313, 1221–1224. [Google Scholar] [CrossRef]
- Hodges, G.J.; Mallette, M.M.; Martin, Z.T.; Del Pozzi, A.T. Effect of sympathetic nerve blockade on low-frequency oscillations of forearm and leg skin blood flow in healthy humans. Microcirculation 2017. [Google Scholar] [CrossRef]
- Grinevich, A.A.; Tankanag, A.; Tikhonova, I.; Chemeris, N. A new approach to the analysis of skin blood flow oscillations in human. Microvasc. Res. 2019, 126, 103889–103896. [Google Scholar] [CrossRef]
- Mizeva, I.A.; Vetrova, D.V. Pulsations of cutaneous blood flow during local heating. Russ. J. Biomech. 2014, 18, 447–454. [Google Scholar]
- Jan, Y.-K.; Liao, F.; Rice, L.A.; Woods, J.A. Using reactive hyperemia to assess the efficacy of local cooling on reducing sacral skin ischemia under surface pressure in people with spinal cord injury: A preliminary report. Arch. Phys. Med. Rehabil. 2013, 94, 1982–1989. [Google Scholar] [CrossRef]
- Harkikh, E.; Mizeva, I.; Makovik, I.; Dremin, V.; Zherebtsov, E.; Potapova, E.; Dunaev, A. Blood flow oscillations as a signature of microvascular abnormalities. Proc. SPIE 2018, 10685, 1–7. [Google Scholar]
- Lohman, E.; Petrofsky, J.S.; Maloney-Hinds, C.; Betts-Schwab, H.; Thorpe, D. The effect of whole body vibration on lower extremity skin blood flow in normal subjects. Med. Sci. Monit. 2007, 13, 71–76. [Google Scholar]
- Mitchell, U.H.; Johnson, P.K. Vibration and skin blood flow changes in subjects with restless legs syndrome. J. Parkinsonism Restless Legs Syndr. 2014, 4, 9–16. [Google Scholar] [CrossRef][Green Version]
- Jan, Y.-K.; Struck, B.D.; Foreman, R.D.; Robinson, C. Wavelet analysis of sacral skin blood flow oscillations to assess soft tissue viability in older adults. Microvasc. Res. 2009, 78, 162–168. [Google Scholar] [CrossRef] [PubMed]


| Title 1 | Male | Female |
|---|---|---|
| Age (years) | 26.2 ± 5.2 | 26.6 ± 7.8 |
| Height (m) | 169.5 ± 3.9 | 156.8 ± 5.1 |
| Prerun | Postrun | Postroller | ||
|---|---|---|---|---|
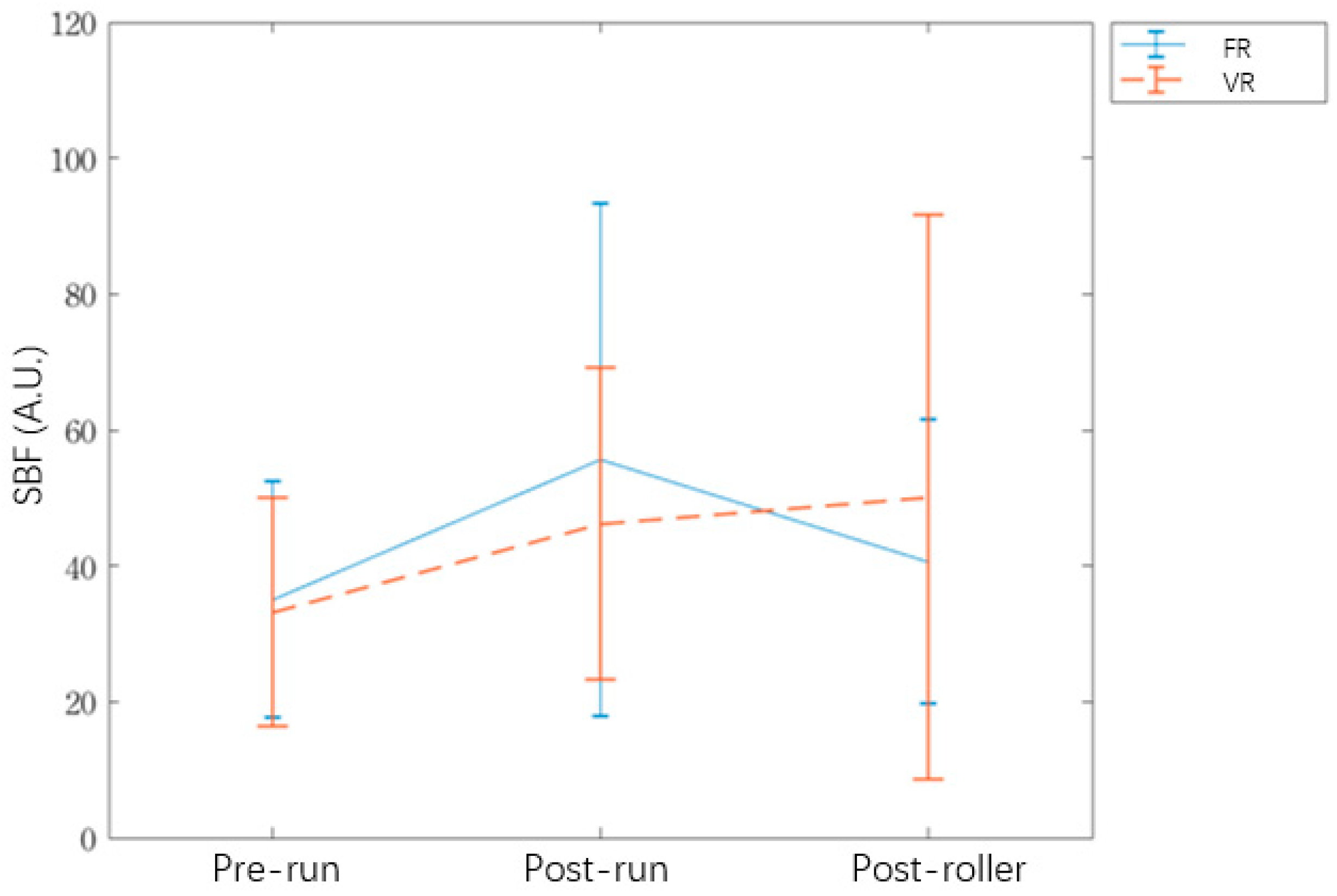
| SBF | Foam roller | 35.1 (17.4) | 55.6 (37.8) | 40.7 (20.8) |
| Vibrating roller | 33.3 (16.8) | 46.2 (23.0) | 50.1 (41.6) | |
| BFO endothelial | Foam roller | 11.1 (6.0) | 11.0 (5.3) | 11.4 (5.4) |
| Vibrating roller | 10.5 (6.1) | 10.6 (4.2) | 12.5 (7.9) | |
| BFO neurogenic | Foam roller | 7.6 (3.0) | 6.5 (4.1) | 7.0 (4.0) |
| Vibrating roller | 7.0 (4.3) | 5.6 (2.4) | 6.3 (2.9) | |
| BFO myogenic | Foam roller | 15.9 (5.0) | 16.0 (6.0) | 18.0 (6.8) |
| Vibrating roller | 13.6 (5.8) | 16.4 (5.1) | 17.8 (6.9) | |
| F Value | df | p | |||
|---|---|---|---|---|---|
| SBF | Roller | 0.018 | 1 | 0.894 | 0.0001 |
| Time | 9.810 | 2 | 0.001 * | 0.1294 | |
| Roller × Time | 1.128 | 2 | 0.343 | 0.0168 | |
| BFO endothelial | Roller | 0.163 | 1 | 0.690 | 0.0012 |
| Time | 0.891 | 2 | 0.425 | 0.0133 | |
| Roller × Time | 0.283 | 2 | 0.756 | 0.0043 | |
| BFO neurogenic | Roller | 2.931 | 1 | 0.101 | 0.0217 |
| Time | 1.338 | 2 | 0.284 | 0.0199 | |
| Roller × Time | 0.031 | 2 | 0.970 | 0.0005 | |
| BFO myogenic | Roller | 0.733 | 1 | 0.401 | 0.0055 |
| Time | 4.439 | 2 | 0.025 * | 0.0630 | |
| Roller × Time | 1.298 | 2 | 0.294 | 0.0193 |
| Roller | Section (I) | Section (J) | Difference (J-I) | p |
|---|---|---|---|---|
| Foam roller | Prerun | Postrun | 20.536 (7.130) | 0.026 * |
| Prerun | Postroller | 5.579 (3.762) | 0.457 | |
| Postrun | Postroller | −14.957 (7.981) | 0.223 | |
| Vibrating roller | Prerun | Postrun | 12.988 (5.306) | 0.068 |
| Prerun | Postroller | 16.903 (7.890) | 0.130 | |
| Postrun | Postroller | 3.915 (8.680) | 1 |
| Intervention | Pair Difference | df | p | ||
|---|---|---|---|---|---|
| SBF | Prerun vs. | Foam roller | 27.90% (78.44) | 22 | 0.04 * |
| Postroller | Vibrating roller | 79.23%(137.33) | |||
| Postrun vs. | Foam roller | −2.21% (97.52) | 22 | 0.24 | |
| Postroller | Vibrating roller | 19.00%(91.59) | |||
| BFO endothelial | Prerun vs. | Foam roller | 33.10% (79.17) | 22 | 0.32 |
| Postroller | Vibrating roller | 46.47% (102.10) | |||
| Postrun vs. | Foam roller | 19.38% (60.35) | 22 | 0.12 | |
| Postroller | Vibrating roller | 53.08% (138.63) | |||
| BFO neurogenic | Prerun vs. | Foam roller | −4.11% (58.59) | 22 | 0.42 |
| Postroller | Vibrating roller | −7.16% (50.73) | |||
| Postrun vs. | Foam roller | 12.77% (55.25) | 22 | 0.27 | |
| Postroller | Vibrating roller | 23.61% (67.43) | |||
| BFO myogenic | Prerun vs. | Foam roller | 13.52% (34.34) | 22 | 0.03 * |
| Postroller | Vibrating roller | 55.19% (99.48) | |||
| Postrun vs. | Foam roller | 21.16% (72.93) | 22 | 0.43 | |
| Postroller | Vibrating roller | 17.65% (45.58) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, Y.-H.; Wang, A.-Y.; Yang, C.-C.; Guo, L.-Y. The Recovery Benefit on Skin Blood Flow Using Vibrating Foam Rollers for Postexercise Muscle Fatigue in Runners. Int. J. Environ. Res. Public Health 2020, 17, 9118. https://doi.org/10.3390/ijerph17239118
Lai Y-H, Wang A-Y, Yang C-C, Guo L-Y. The Recovery Benefit on Skin Blood Flow Using Vibrating Foam Rollers for Postexercise Muscle Fatigue in Runners. International Journal of Environmental Research and Public Health. 2020; 17(23):9118. https://doi.org/10.3390/ijerph17239118
Chicago/Turabian StyleLai, Yi-Horng, Ai-Yi Wang, Chia-Chi Yang, and Lan-Yuen Guo. 2020. "The Recovery Benefit on Skin Blood Flow Using Vibrating Foam Rollers for Postexercise Muscle Fatigue in Runners" International Journal of Environmental Research and Public Health 17, no. 23: 9118. https://doi.org/10.3390/ijerph17239118
APA StyleLai, Y.-H., Wang, A.-Y., Yang, C.-C., & Guo, L.-Y. (2020). The Recovery Benefit on Skin Blood Flow Using Vibrating Foam Rollers for Postexercise Muscle Fatigue in Runners. International Journal of Environmental Research and Public Health, 17(23), 9118. https://doi.org/10.3390/ijerph17239118






