Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review
Abstract
1. Introduction
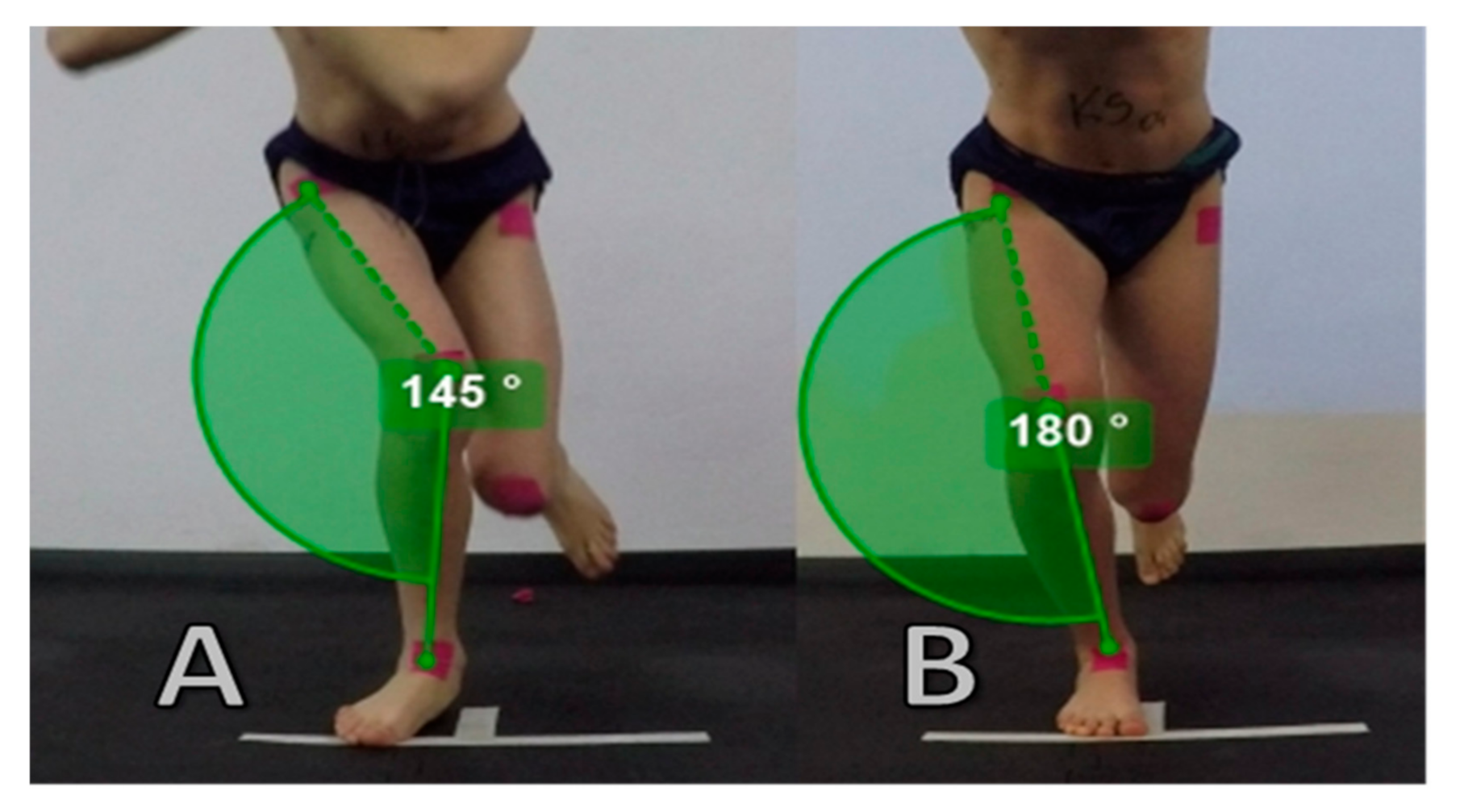
Dynamic Knee Valgus
2. Relationship between Squat and Landing on a Single-Leg and Double-Leg in Terms of Knee Valgus
3. Selected Modifiable Factors of Dynamic Knee Valgus
3.1. Impact of the Neuromuscular Trunk Control on Knee Kinetics
3.2. Hip Strength and Muscle Activation as Causes of the Incorrect Movement Pattern of the Knee
Activation and Coactivation of the Gluteus Muscles for Knee Control
3.3. The Role of Strength and Muscle Activation Quadriceps and Hamstring in Stabilizing the Knee
3.4. The Possible Impact of the Ankle Range of Motion and Foot Aspect
3.5. Fatigue as a Factor in the Context of Dynamic Knee Valgus
4. Exercise Training to Reduce Dynamic Knee Valgus
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- van Mechelen, W.; Hlobil, H.; Kemper, H.C.G. Incidence, Severity, Aetiology and Prevention of Sports Injuries. Sports Med. 1992, 14, 82–99. [Google Scholar] [CrossRef]
- Van Tiggelen, D.; Wickes, S.; Stevens, V.; Roosen, P.; Witvrouw, E. Effective prevention of sports injuries: A model integrating efficacy, efficiency, compliance and risk-taking behaviour. Br. J. Sports Med. 2008, 42, 648–652. [Google Scholar] [CrossRef]
- Ellenberger, L.; Oberle, F.; Lorenzetti, S.; Frey, W.O.; Snedeker, J.G.; Spörri, J. Dynamic knee valgus in competitive alpine skiers: Observation from youth to elite and influence of biological maturation. Scand. J. Med. Sci. Sports 2020, 30, 1212–1220. [Google Scholar] [CrossRef]
- Agel, J.; Rockwood, T.; Klossner, D. Collegiate ACL Injury Rates Across 15 Sports: National Collegiate Athletic Association Injury Surveillance System Data Update (2004–2005 Through 2012–2013). Clin. J. Sport Med. 2016, 26, 518–523. [Google Scholar] [CrossRef]
- Neal, B.S.; Barton, C.J.; Gallie, R.; O’Halloran, P.; Morrissey, D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: A systematic review and meta-analysis. Gait Posture. 2016, 45, 69–82. [Google Scholar] [CrossRef]
- Benjaminse, A.; Webster, K.E.; Kimp, A.; Meijer, M.; Gokeler, A. Revised Approach to the Role of Fatigue in Anterior Cruciate Ligament Injury Prevention: A Systematic Review with Meta-Analyses. Sports Med. 2019, 49, 565–586. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex systems approach for sports injuries: Moving from risk factor identification to injury pattern recognition-narrative review and new concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed]
- Radzimiński, Ł.; Szwarc, A.; Padrón-Cabo, A.; Jastrzębski, Z. Correlations between body composition, aerobic capacity, speed and distance covered among professional soccer players during official matches. J. Sports Med. Phys. Fit. 2020, 60, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Mauntel, T.C.; Frank, B.S.; Begalle, R.L.; Blackburn, J.T.; Padua, D.A. Kinematic differences between those with and without medial knee displacement during a single-leg squat. J. Appl. Biomech. 2014, 30, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am. J. Sports Med. 2006, 34, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Holden, S.; Boreham, C.; Delahunt, E. Sex Differences in Landing Biomechanics and Postural Stability During Adolescence: A Systematic Review with Meta-Analyses. Sports Med. 2016, 46, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Waldén, M.; Krosshaug, T.; Bjørneboe, J.; Andersen, T.E.; Faul, O.; Hägglund, M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: A systematic video analysis of 39 cases. Br. J. Sports Med. 2015, 49, 1452–1460. [Google Scholar] [CrossRef] [PubMed]
- Grassi, A.; Smiley, S.P.; Di Roberti Sarsina, T.; Signorelli, C.; Marcheggiani Muccioli, G.M.; Bondi, A.; Romagnoli, M.; Agostini, A.; Zaffagnini, S. Mechanisms and situations of anterior cruciate ligament injuries in professional male soccer players: A YouTube-based video analysis. Eur. J Orthop. Surg. Traumatol. 2017, 27, 967–981. [Google Scholar] [CrossRef]
- Kanamori, A.; Woo, S.L.; Ma, C.B.; Zeminski, J.; Rudy, T.W.; Li, G.; Livesay, G.A. The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: A human cadaveric study using robotic technology. Arthroscopy 2000, 16, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, Y.; Woo, S.L.-Y.; Loh, J.C.; Tsuda, E.; Tang, P.; McMahon, P.J.; Debski, R.E. A quantitative analysis of valgus torque on the ACL: A human cadaveric study. J. Orthop. Res. 2003, 21, 1107–1112. [Google Scholar] [CrossRef]
- Winby, C.R.; Lloyd, D.G.; Besier, T.F.; Kirk, T.B. Muscle and external load contribution to knee joint contact loads during normal gait. J. Biomech. 2009, 42, 2294–2300. [Google Scholar] [CrossRef] [PubMed]
- Gadikota, H.R.; Kikuta, S.; Qi, W.; Nolan, D.; Gill, T.J.; Li, G. Effect of increased iliotibial band load on tibiofemoral kinematics and force distributions: A direct measurement in cadaveric knees. J. Orthop. Sports Phys. Ther. 2013, 43, 478–485. [Google Scholar] [CrossRef]
- Lephart, S.M.; Pincivero, D.M.; Giraldo, J.L.; Fu, F.H. The role of proprioception in the management and rehabilitation of athletic injuries. Am. J. Sports Med. 1997, 25, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Cerulli, G.; Benoit, D.L.; Caraffa, A.; Ponteggia, F. Proprioceptive training and prevention of anterior cruciate ligament injuries in soccer. J. Orthop. Sports Phys. Ther. 2001, 31, 655–660, discussion 661. [Google Scholar] [CrossRef]
- Acevedo, R.J.; Rivera-Vega, A.; Miranda, G.; Micheo, W. Anterior Cruciate Ligament Injury. Curr. Sports Med. Rep. 2014, 13, 186–191. [Google Scholar] [CrossRef]
- Gokeler, A.; Neuhaus, D.; Benjaminse, A.; Grooms, D.R.; Baumeister, J. Principles of Motor Learning to Support Neuroplasticity After ACL Injury: Implications for Optimizing Performance and Reducing Risk of Second ACL Injury. Sports Med. 2019, 49, 853–865, Correction in 2019, 49, 979. [Google Scholar] [CrossRef]
- Petersen, W.; Rembitzki, I.; Liebau, C. Patellofemoral pain in athletes. Open Access J. Sports Med. 2017, 8, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Carson, D.W.; Ford, K.R. Sex differences in knee abduction during landing: A systematic review. Sports Health. 2011, 3, 373–382. [Google Scholar] [CrossRef]
- Schurr, S.A.; Marshall, A.N.; Resch, J.E.; Saliba, S.A. Two-dimensional video analysis is comparable to 3d motion capture in lower extremity movement assessment. Int. J. Sports Phys. Ther. 2017, 12, 163–172. [Google Scholar]
- Werner, D.M.; Di Stasi, S.; Lewis, C.L.; Barrios, J.A. Test-retest reliability and minimum detectable change for various frontal plane projection angles during dynamic tasks. Phys. Ther. Sport. 2019, 40, 169–176. [Google Scholar] [CrossRef]
- Prins, M.R.; van der Wurff, P. Females with patellofemoral pain syndrome have weak hip muscles: A systematic review. Aust. J. Physiother. 2009, 55, 9–15. [Google Scholar] [CrossRef]
- Herrington, L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee 2014, 21, 514–517. [Google Scholar] [CrossRef]
- Yamazaki, J.; Muneta, T.; Ju, Y.J.; Sekiya, I. Differences in kinematics of single leg squatting between anterior cruciate ligament-injured patients and healthy controls. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 56–63. [Google Scholar] [CrossRef]
- DiCesare, C.A.; Montalvo, A.; Barber Foss, K.D.; Thomas, S.M.; Ford, K.R.; Hewett, T.E.; Jayanthi, N.A.; Stracciolini, A.; Bell, D.R.; Myer, G.D. Lower Extremity Biomechanics Are Altered Across Maturation in Sport-Specialized Female Adolescent Athletes. Front. Pediatr. 2019, 7, 268. [Google Scholar] [CrossRef]
- Munro, A.; Herrington, L.; Comfort, P. The Relationship Between 2-Dimensional Knee-Valgus Angles During Single-Leg Squat, Single-Leg-Land, and Drop-Jump Screening Tests. J. Sport Rehabil. 2017, 26, 72–77. [Google Scholar] [CrossRef][Green Version]
- Padua, D.A.; Bell, D.R.; Clark, M.A. Neuromuscular characteristics of individuals displaying excessive medial knee displacement. J. Athl. Train. 2012, 47, 525–536. [Google Scholar] [CrossRef]
- Ali, N.; Rouhi, G.; Robertson, G. Gender, Vertical Height and Horizontal Distance Effects on Single-Leg Landing Kinematics: Implications for Risk of non-contact ACL Injury. J. Hum. Kinet. 2013, 37, 27–38. [Google Scholar] [CrossRef]
- Lyle, M.A.; Valero-Cuevas, F.J.; Gregor, R.J.; Powers, C.M. Control of dynamic foot-ground interactions in male and female soccer athletes: Females exhibit reduced dexterity and higher limb stiffness during landing. J. Biomech. 2014, 47, 512–517. [Google Scholar] [CrossRef]
- Donohue, M.R.; Ellis, S.M.; Heinbaugh, E.M.; Stephenson, M.L.; Qin, Z.; Boyi, D. Differences and correlations in knee and hip mechanics during single-leg landing, single-leg squat, double-leg landing, and double-leg squat tasks. Res. Sports Med. 2015, 23, 394–411. [Google Scholar] [CrossRef]
- Harty, C.M.; DuPont, C.E.; Chmielewski, T.L.; Mizner, R.L. Intertask comparison of frontal plane knee position and moment in female athletes during three distinct movement tasks. Scand. J. Med. Sci. Sports. 2011, 21, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.B.; Ford, K.R.; Nguyen, A.D. Shultz SJ. Biomechanical Comparison of Single- and Double-Leg Jump Landings in the Sagittal and Frontal Plane. Orthop. J. Sports Med. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Santamaria, L.J.; Webster, K.E. The Effect of Fatigue on Lower-Limb Biomechanics During Single-Limb Landings: A Systematic Review. J. Orthop. Sports Phys. Ther. 2010, 40, 464–473. [Google Scholar] [CrossRef]
- Koga, H.; Nakamae, A.; Shima, Y.; Iwasa, J.; Myklebust, G.; Engebretsen, L.; Bahr, R.; Krosshaug, T. Mechanisms for noncontact anterior cruciate ligament injuries: Knee joint kinematics in 10 injury situations from female team handball and basketball. Am. J. Sports Med. 2010, 38, 2218–2225. [Google Scholar] [CrossRef]
- Krosshaug, T.; Nakamae, A.; Boden, B.P.; Engebretsen, L.; Smith, G.; Slauterbeck, J.R.; Hewett, T.E.; Bahr, R. Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases. Am. J. Sports Med. 2007, 35, 359–367. [Google Scholar] [CrossRef]
- Hewett, T.E.; Torg, J.S.; Boden, B.P. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: Lateral trunk and knee abduction motion are combined components of the injury mechanism. Br. J. Sports Med. 2009, 43, 417–422. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Hoogenboom, B.J.; Myer, G.D. Understanding and preventing acl injuries: Current biomechanical and epidemiologic considerations—Update 2010. N. Am. J. Sports Phys. Ther. 2010, 5, 234–251. [Google Scholar]
- Nakagawa, T.H.; Maciel, C.D.; Serrão, F.V. Trunk biomechanics and its association with hip and knee kinematics in patients with and without patellofemoral pain. Man. Ther. 2015, 20, 189–193. [Google Scholar] [CrossRef]
- Chuter, V.H.; Janse de Jonge, X.A.K. Proximal and distal contributions to lower extremity injury: A review of the literature. Gait Posture 2012, 36, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.D.; Ireland, M.L.; Davis, I. Core Strength and Lower Extremity Alignment during Single Leg Squats. Med. Sci. Sports Exerc. 2006, 38, 5. [Google Scholar] [CrossRef]
- Stickler, L.; Finley, M.; Gulgin, H. Relationship between hip and core strength and frontal plane alignment during a single leg squat. Phys. Ther. Sport 2015, 16, 66–71. [Google Scholar] [CrossRef]
- Cronström, A.; Creaby, M.W.; Nae, J.; Ageberg, E. Gender differences in knee abduction during weight-bearing activities: A systematic review and meta-analysis. Gait Posture 2016, 49, 315–328. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.R.; Nguyen, A.-D.; Dischiavi, S.L.; Hegedus, E.J.; Zuk, E.F.; Taylor, J.B. An evidence-based review of hip-focused neuromuscular exercise interventions to address dynamic lower extremity valgus. Open Access J. Sports Med. 2015, 6, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Hollman, J.H.; Ginos, B.E.; Kozuchowski, J.; Vaughn, A.S.; Krause, D.A.; Youdas, J.W. Relationships between Knee Valgus, Hip-Muscle Strength, and Hip-Muscle Recruitment during a Single-Limb Step-Down. J. Sport Rehabil. 2009, 18, 104–117. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the hip: A focus on muscular actions. J. Orthop. Sports Phys. Ther. 2010, 40, 82–94. [Google Scholar] [CrossRef]
- Claiborne, T.L.; Armstrong, C.W.; Gandhi, V.; Pincivero, D.M. Relationship between Hip and Knee Strength and Knee Valgus during a Single Leg Squat. J. Appl. Biomech. 2006, 22, 41–50. [Google Scholar] [CrossRef]
- Suzuki, H.; Omori, G.; Uematsu, D.; Nishino, K.; Endo, N. The influence of hip strength on knee kinematics during a single-legged medial drop landing among competitive collegiate basketball players. Int. J. Sports Phys. Ther. 2015, 10, 592–601. [Google Scholar]
- Neamatallah, Z.; Herrington, L.; Jones, R. An investigation into the role of gluteal muscle strength and EMG activity in controlling HIP and knee motion during landing tasks. Phys. Ther. Sport 2020, 43. [Google Scholar] [CrossRef]
- Kagaya, Y.; Fujii, Y.; Nishizono, H. Association between hip abductor function, rear-foot dynamic alignment, and dynamic knee valgus during single-leg squats and drop landings. J. Sport Health Sci. 2015, 4, 182–187. [Google Scholar] [CrossRef]
- Jacobs, C.A.; Uhl, T.L.; Mattacola, C.G.; Shapiro, R.; Rayens, W.S. Hip abductor function and lower extremity landing kinematics: Sex differences. J. Athl. Train. 2007, 42, 76–83. [Google Scholar]
- Malloy, P.J.; Morgan, A.M.; Meinerz, C.M.; Geiser, C.F.; Kipp, K. Hip External Rotator Strength Is Associated With Better Dynamic Control of the Lower Extremity During Landing Tasks. J. Strength Cond. Res. 2016, 30, 282–291. [Google Scholar] [CrossRef]
- Dix, J.; Marsh, S.; Dingenen, B.; Malliaras, P. The relationship between hip muscle strength and dynamic knee valgus in asymptomatic females: A systematic review. Phys. Ther. Sport. 2019, 37, 197–209. [Google Scholar] [CrossRef]
- Cashman, G.E. The effect of weak hip abductors or external rotators on knee valgus kinematics in healthy subjects: A systematic review. J. Sport Rehabil. 2012, 21, 273–284. [Google Scholar] [CrossRef]
- Hollman, J.H.; Hohl, J.M.; Kraft, J.L.; Strauss, J.D.; Traver, K.J. Modulation of Frontal-Plane Knee Kinematics by Hip-Extensor Strength and Gluteus Maximus Recruitment During a Jump-Landing Task in Healthy Women. J. Sport Rehabil. 2013, 22, 184–190. [Google Scholar] [CrossRef]
- Latash, M.L. Muscle coactivation: Definitions, mechanisms, and functions. J. Neurophysiol. 2018, 120, 88–104. [Google Scholar] [CrossRef]
- Wild, C.Y.; Steele, J.R.; Munro, B.J. Insufficient hamstring strength compromises landing technique in adolescent girls. Med. Sci. Sports Exerc. 2013, 45, 497–505. [Google Scholar] [CrossRef]
- Lloyd, D.G.; Buchanan, T.S. Strategies of muscular support of varus and valgus isometric loads at the human knee. J. Biomech. 2001, 34, 1257–1267. [Google Scholar] [CrossRef]
- Dhaher, Y.Y.; Tsoumanis, A.D.; Rymer, W.Z. Reflex muscle contractions can be elicited by valgus positional perturbations of the human knee. J. Biomech. 2003, 36, 199–209. [Google Scholar] [CrossRef]
- Palmieri-Smith, R.M.; Wojtys, E.M.; Ashton-Miller, J.A. Association between preparatory muscle activation and peak valgus knee angle. J. Electromyogr Kinesiol. 2008, 18, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.N.; McLean, S.G.; Palmieri-Smith, R.M. Associations between lower limb muscle activation strategies and resultant multi-planar knee kinetics during single leg landings. J. Sci. Med. Sport 2014, 17, 408–413. [Google Scholar] [CrossRef]
- Dill, K.E.; Begalle, R.L.; Frank, B.S.; Zinder, S.M.; Padua, D.A. Altered knee and ankle kinematics during squatting in those with limited weight-bearing-lunge ankle-dorsiflexion range of motion. J. Athl. Train. 2014, 49, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Wyndow, N.; de Jong, A.; Rial, K.; Tucker, K.; Collins, N.; Vicenzino, B.; Russel, T.; Crossley, K. The relationship of foot and ankle mobility to the frontal plane projection angle in asymptomatic adults. J. Foot Ankle Res. 2016, 9, 3. [Google Scholar] [CrossRef]
- Lima, Y.L.; Ferreira, V.M.L.M.; de Paula Lima, P.O.; Bezerra, M.A.; de Oliveira, R.R.; Almeida, G.P.L. The association of ankle dorsiflexion and dynamic knee valgus: A systematic review and meta-analysis. Phys. Ther. Sport 2018, 29, 61–69. [Google Scholar] [CrossRef]
- Mason-Mackay, A.R.; Whatman, C.; Reid, D. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: A systematic review. J. Sci Med. Sport. 2017, 20, 451–458. [Google Scholar] [CrossRef]
- Pohl, M.B.; Messenger, N.; Buckley, J.G. Changes in foot and lower limb coupling due to systematic variations in step width. Clin. Biomech. 2006, 21, 175–183. [Google Scholar] [CrossRef]
- Benjaminse, A.; Habu, A.; Sell, T.C.; Abt, J.P.; Fu, F.H.; Myers, J.B.; Lephart, S.M. Fatigue alters lower extremity kinematics during a single- leg stop-jump task. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 400–407. [Google Scholar] [CrossRef]
- Kellis, E.; Kouvelioti, V. Agonist versus antagonist muscle fatigue effects on thigh muscle activity and vertical ground reaction during drop landing. J. Elect. Kinesiol. 2009, 19, 55–64. [Google Scholar] [CrossRef]
- Gandevia, S.C. Spinal and supraspinal factors in human muscle fatigue. Physiol. Rev. 2001, 81, 1725–1789. [Google Scholar] [CrossRef]
- Tamura, A.; Akasaka, K.; Otsudo, T.; Sawada, Y.; Okubo, Y.; Shiozawa, J.; Toda, Y.; Yamada, K. Fatigue alters landing shock attenuation duringa single-leg vertical drop jump. Orthop. J. Sports Med. 2016, 4. [Google Scholar] [CrossRef]
- Lessi, G.; dos Santos, A.; Batista, L.; de Oliveira, G.; Serrăo, F. Effects of fatigue on lower limb, pelvis and trunk kinematics and muscle activation: Gender differences. J. Elect. Kinesiol. 2017, 32, 9–14. [Google Scholar] [CrossRef]
- Barber-Westin, S.D.; Noyes, F.R. Effect of fatigue protocols on lower limb neuromuscular function and implications for anterior cruciate ligament injury prevention training: A systematic review. Am. J. Sports Med. 2017, 45, 3388–3396. [Google Scholar] [CrossRef]
- Hiemstra, L.A.; Lo, I.K.; Fowler, P.J. Effect of fatigue on knee proprioception: Implications for dynamic stabilization. J. Orthop. Sports Phys. Ther. 2001, 31, 598–605. [Google Scholar] [CrossRef]
- Abd-Elfattah, H.M.; Abdelazeim, F.H.; Elshennawy, S. Physical and cognitive consequences of fatigue: A review. J. Adv. Res. 2015, 6, 351–358. [Google Scholar] [CrossRef]
- Kernozek, T.W.; Torry, M.R.; Iwasaki, M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am. J. Sports Med. 2008, 36, 554–565. [Google Scholar] [CrossRef]
- Pol, R.; Hristovski, R.; Medina, D.; Balague, N. From microscopic to macroscopic sports injuries. Applying the complex dynamic systems approach to sports medicine: A narrative review. Br. J. Sports Med. 2008, 53. [Google Scholar] [CrossRef]
- Bourne, M.N.; Webster, K.E.; Hewett, T.E. Is Fatigue a Risk Factor for Anterior Cruciate Ligament Rupture? Sports Med. 2019, 49, 1629–1635. [Google Scholar] [CrossRef]
- Marshall, A.N.; Hertel, J.; Hart, J.M.; Russell, S.; Saliba, S.A. Visual Biofeedback and Changes in Lower Extremity Kinematics in Individuals With Medial Knee Displacement. J. Athl. Train. 2020, 55, 255–264. [Google Scholar] [CrossRef]
- Palmer, K.; Hebron, C.; Williams, J.M. A randomised trial into the effect of an isolated hip abductor strengthening programme and a functional motor control programme on knee kinematics and hip muscle strength. BMC Musculoskelet. Disord. 2015, 16, 105. [Google Scholar] [CrossRef]
- Hopper, A.J.; Haff, E.E.; Joyce, C.; Lloyd, R.S.; Haff, G.G. Neuromuscular Training Improves Lower Extremity Biomechanics Associated with Knee Injury during Landing in 11–13 Year Old Female Netball Athletes: A Randomized Control Study. Front. Physiol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Dawson, S.J.; Herrington, L. Improving Single-Legged–Squat Performance: Comparing 2 Training Methods with Potential Implications for Injury Prevention. J. Athl. Train. 2015, 50, 921–929. [Google Scholar] [CrossRef]
- Sasaki, S.; Tsuda, E.; Yamamoto, Y.; Maeda, S.; Kimura, Y.; Fujita, Y.; Ishibashi, Y. Core-Muscle Training and Neuromuscular Control of the Lower Limb and Trunk. J. Athl. Train. 2019, 54, 959–969. [Google Scholar] [CrossRef]
- Attwood, M.J.; Roberts, S.P.; Trewartha, G.; England, M.E.; Stokes, K.A. Efficacy of a movement control injury prevention programme in adult men’s community rugby union: A cluster randomised controlled trial. Br. J. Sports Med. 2018, 52, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Barengo, N.C.; Meneses-Echávez, J.F.; Ramírez-Vélez, R.; Cohen, D.D.; Tovar, G.; Bautista, J.E. The impact of the FIFA 11+ training program on injury prevention in football players: A systematic review. Int. J. Environ. Res. Public Health 2014, 11, 11986–12000. [Google Scholar] [CrossRef]
| TRUNK | |||
| Study | Participants | Outcome parameters | Results |
| Wilson et al. 2006 | F = 22 (19.4 ± 0.7y) M = 24 (19.9 ± 2.3y) Division 1A or 1AA basketball, soccer, or volleyball players. | Peak isometric torque: trunk flexion, lateral flexion and extension Knee valgus: FPPA (2-D) during SLS | BOTH: SLS Greater trunk lateral flexion strength among participant with lower knee valgus angles (FPPA) |
| Stickler et al. 2015 | F = 40 (22.88 ± 0.32y) | Handheld dynamometer isometric: side lying plank test (trunk lateral flexion) Knee valgus: FPPA (2-D) during SLS | FEMALE: SLS Greater trunk lateral flexion strength among female with lower knee valgus angles (FPPA) |
| Nakagawa et al. 2015 | F = 20 M = 10 (both: 22.3 ± 3.0y) Control group (healthy without PFP) | Handheld dynamometer isometric: trunk extension, flexion with rotation and side bridge Knee valgus: Electromagnetic tracking system (3-D) during SLS | BOTH: SLS Greater strength of trunk lateral flexion (side bridge test) among healthy participant with lower knee valgus angles. |
| KNEE | |||
| Study | Participants | Outcome parameters | Results |
| Wilson et al. 2006 | F = 22 (19.4 ± 0.7y) M = 24 (19.9 ± 2.3y) Division 1A or 1AA basketball, soccer, or volleyball players. | Peak isometric torque: Knee flexion and extension Knee valgus: FPPA (2-D) during SLS | BOTH: SLS Greater strength of knee flexor among participant with higher knee valgus angles (positive correlation) |
| Claiborne et al. 2006 | F = 15 (23.5 ± 3.7y) M = 15 (26.4 ± 5.2y) | Isokinetic eccentric/concentric strength: knee extension and flexion Knee valgus: FPKM (Frontal plane knee motion) in 3-D during SLS | Both: SLS Participants with greater knee strength exhibited less valgus motion |
| Wild et al. 2013 | F = 33 (10–13y, Tanner stage II) | Isokinetic eccentric/concentric strength: knee extension and flexion Knee valgus: 3-D motion analyses system during SLL | Female: SLL Females with lower flexor (hamstring) strength displayed significantly greater knee valgus angles. |
| ACTIVATION | |||
| Palmieri-Smith et al. 2008 | F = 18 (24.0 ± 5.2y) M = 10 (23.6 ± 3.8y) recreationally active (Tegner score 5 or 6). | EMG: Dynamic and MVIC rectus femoris, vastus lateralis, vastus medialis, medial hamstring, lateral hamstring Knee valgus: 3-D motion capture kinematic during SLL | Female: SLL A greater muscle pre-activity of vastus lateralis and lateral hamstring was associated with greater peak knee valgus angle. A smaller peak valgus angle was associated with increased pre-activity of the vastus medialis muscle Both or males: SLL Muscle activation was not associated with the peak knee valgus angle |
| Brown et al. 2013 | F = 35 (15.1 ± 1.2y) basketball, field hockey, and soccer players | EMG: Dynamic and MVIC vastus lateralis (VL), rectus femoris, lateral hamstring (LH) Knee valgus: 3-D motion analyses system during SLL | Female: SLL Muscle pre-activity of vastus lateralis, rectus femoris, lateral hamstring, and VL: LH ratio was not a significant predictive. |
| HIP | |||
| Study | Participants | Outcome parameters | Results |
| Neamatallah 2020 | F = 17 (25.7 ± 4.5y) M = 17 (26.9 ± 3.8y) physically active (participating in least 3 h of exercise per week) | Isokinetic muscle strength concentric/eccentric: hip abduction and hip extension Knee valgus: 3D motion analysis during SLS/SLL (Forward Landing - FL, Single Medial Landing -SML, Single Lateral Landing - SLL) | FEMALE: SLS Female with greater hip abduction concentric and hip extension eccentric strength had lower knee valgus angles SLL (FL, SML, SLL) Female with greater hip abduction concentric strength (very strong negative correlation) and hip abduction eccentric strength (strong negative correlation) had lower knee valgus angles. |
| Claiborne et al. 2006 | F = 15 (23.5 ± 3.7y) M = 15 (26.4 ± 5.2y) | Isokinetic eccentric/concentric strength: Hip (abduction/adduction, flexion/extension, and internal/external rotation Knee valgus: FPKM (Frontal plane knee motion) in 3-D during SLS | BOTH: SLS Greater strength of concentric hip abduction among participant with lower knee valgus angles. (Weak to moderate negative correlation) |
| Suzuki 2015 | F = 23 (19.96 ± 0.77y) M = 20 (20.20 ± 1.54y) intercollegiate basketball players | Hand-held dynamometer – hip extensor, abductor and external rotator Knee valgus 3-D analysis system during SLL (SML) | FEMALE: SLL Greater knee valgus angle at IC among participant with lower strength of hip extension, hip abduction and external rotation. |
| Stickler et al. 2015 | F = 40 (22.88 ± 0.32y) | Handheld dynamometer isometric: hip abduction, extension, external rotation Knee valgus: FPPA (2-D) during SLS | FEMALE: SLS Female with greater hip abduction, hip extension and external rotation strength had lower knee peak valgus angles (FPPA) |
| Wilson et al. 2006 | F = 22 (19.4 ± 0.7y) M = 24 (19.9 ± 2.3y) Division 1A or 1AA basketball, soccer, or volleyball players. | Peak isometric torque: Hip abduction and external rotation Knee valgus: FPPA (2-D) during SLS | BOTH: SLS Greater hip external rotation strength among participant with greater knee valgus angles (positive correlation) |
| Jacobs & Matacola 2005 | F = 10 (22.1 ± 2.3y) M = 8 (24.1 ± 2.2y) Recreationally active adults. | Isokinetic peak eccentric torque: Hip abductor Knee valgus: 3-D analysis system during SLL | FEMALE: SLL Female with larger eccentric peak torque had lower peak knee valgus angles MALE: SLL No significant correlations between eccentric peak torque and knee valgus |
| ACTIVATION/COACTIVATION | |||
| Mauntel et al. 2013 | MKD group (20.2 ± 1.8y) F = 10 M = 10 Control group (20.2 ± 1.5y) F = 10 M = 10 physically active, defined as participation in at least 30 min. of physical activity, 3 times per week for at least 6 months | EMG Dynamic (descent phase of SLS) and MVIC Gluteus maximus and medius, hip adductors (hip coactivation ratios) Knee valgus: 3-D motion analysis during SLS | BOTH: SLS Hip coactivation ratios shows smaller gluteus medius to hip adductor (GMed:Hip Add) and gluteus maximus to hip adductor (GMax:Hip Add) coactivation ratios in valgus group than in the control group |
| Neamatallah 2020 | F = 17 (25.7 ± 4.5y) M = 17 (26.9 ± 3.8y) physically active (participating in least 3 h of exercise per week) | EMG Dynamic and MVIC Gluteus maximus and medius Knee valgus: 3D motion analysis during SLS/SLL (Forward Landing, Single Medial Landing, Single Lateral Landing) | FEMALE: SLL (FL) Higher G Max EMG activity was associated with higher knee valgus angles among female (positive correlation). MALE: SLS: Higher G Med. EMG activity was associated with higher knee valgus angles among male (positive correlation). |
| ANKLE AND FOOT | |||
| Study | Participants | Outcome parameters | Results |
| Wyndow et al. 2016 | Both = 30 (22 ± 3y) | Ankle dorsiflexion Range: knee-to-wall lunge test Foot mobility was quantified as the difference in dorsal midfoot height or midfoot width, between non-weight bearing and bilateral weight bearing positions Knee valgus: 2-D FPPA during SLS | BOTH: SLS higher midfoot width mobility, or lower ankle joint dorsiflexion range and midfoot height mobility, were associated with a greater knee valgus angles (FPPA) |
| Mauntel et al. 2013 | Valgus group (20.2 ± 1.8y) F = 10 M = 10 Control group (20.2 ± 1.5y) F = 10 M = 10 physically active, defined as participation in at least 30 min. of physical activity, 3 times per week for at least 6 months | Ankle dorsiflexion range (in extended position) Supine Leg straight – goniometer measurement (in flexed) Supine Knee flexed – goniometer measurement Knee valgus: 3-D motion analysis during SLS | BOTH: SLS Valgus group displayed significantly less passive ankle dorsiflexion with the knee extended and flexed |
| Kagaya et al. 2015 | F = 130 (16.9 ± 0.6y) high-school basketball players, basketball experience, 6.7 ± 2.0 y. | Rear-foot eversion alignment – dynamic heel-floor test (HFT) Knee valgus: 2D video images (Knee-in distance) during SLS and SLL | FEMALE: SLS and SLL The KID were greater in the HFT-positive (≥5˚ angle) than in the HFT-negative group (<5˚ angle) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilczyński, B.; Zorena, K.; Ślęzak, D. Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 8208. https://doi.org/10.3390/ijerph17218208
Wilczyński B, Zorena K, Ślęzak D. Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review. International Journal of Environmental Research and Public Health. 2020; 17(21):8208. https://doi.org/10.3390/ijerph17218208
Chicago/Turabian StyleWilczyński, Bartosz, Katarzyna Zorena, and Daniel Ślęzak. 2020. "Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review" International Journal of Environmental Research and Public Health 17, no. 21: 8208. https://doi.org/10.3390/ijerph17218208
APA StyleWilczyński, B., Zorena, K., & Ślęzak, D. (2020). Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review. International Journal of Environmental Research and Public Health, 17(21), 8208. https://doi.org/10.3390/ijerph17218208






