A Feasibility Study for Implementation “Health Arcade”: A Study Protocol for Prototype of Multidomain Intervention Based on Gamification Technologies in Acutely Hospitalized Older Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Participants and Eligibility Criteria
2.3. Participant-Selection and Consent Process
2.4. Ethics and Dissemination
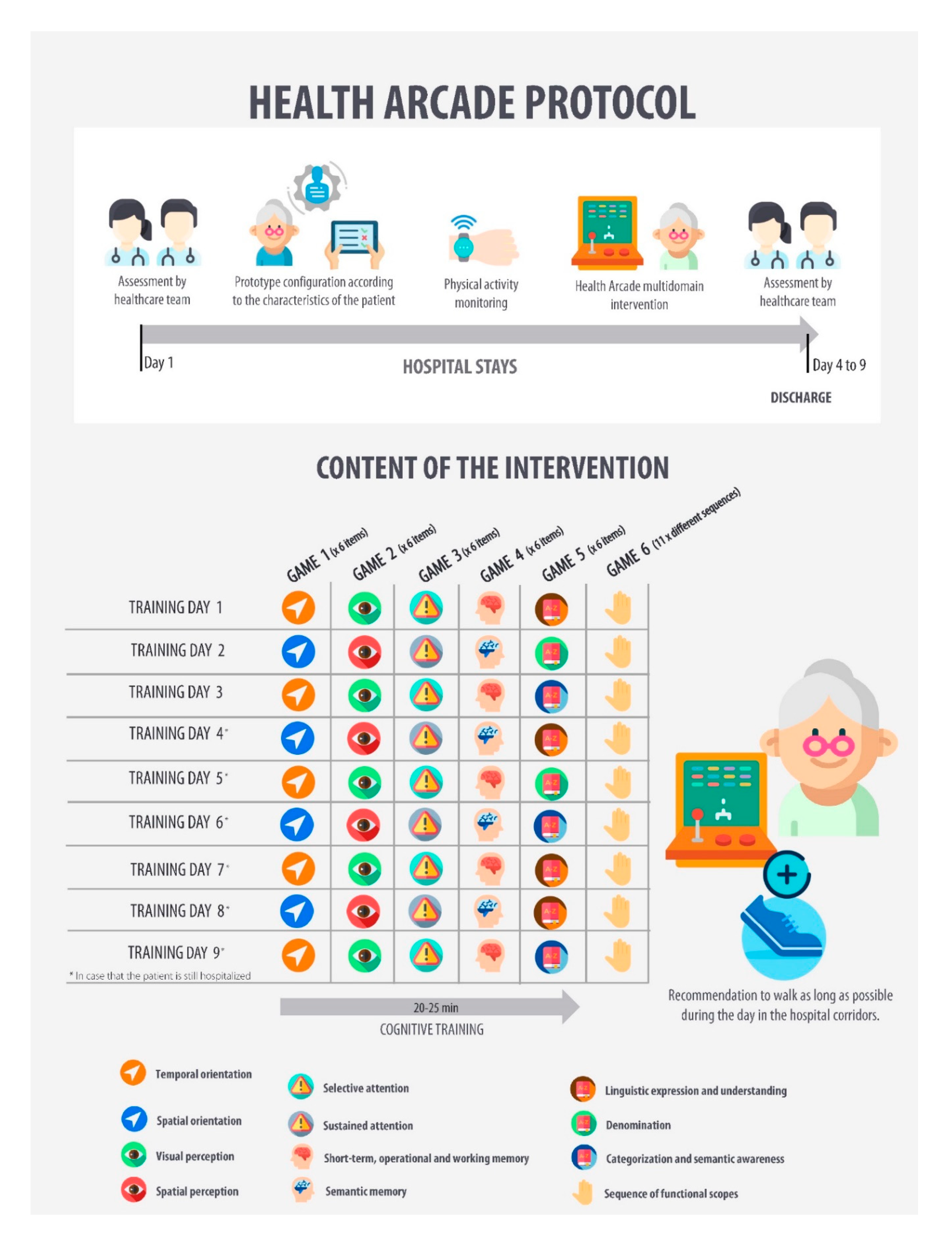
2.5. Interventions
2.6. Outcomes Assessment
2.7. Planned Statistical Analysis
3. Expected Results/Discussion
4. Conclusions
5. Trial Status
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wolinsky, F.D.; Callahan, C.M.; Fitzgerald, J.F.; Johnson, R.J. Changes in Functional Status and the Risks of Subsequent Nursing Home Placement and Death. J. Gerontol. 1993, 48, S94–S101. [Google Scholar] [PubMed]
- Goodwin, J.S.; Howrey, B.; Zhang, D.D.; Kuo, Y.-F. Risk of Continued Institutionalization After Hospitalization in Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66A, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Ageing and Health. 2015. Available online: https://www.who.int/ageing/events/world-report-2015-launch/en/ (accessed on 21 July 2020).
- Villumsen, M.; Jorgensen, M.G.; Andreasen, J.; Rathleff, M.S.; Mølgaard, C.M. Very Low Levels of Physical Activity in Older Patients During Hospitalization at an Acute Geriatric Ward: A Prospective Cohort Study. J. Aging Phys. Act. 2015, 23, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Boyd, C.M.; Landefeld, C.S.; Counsell, S.R.; Palmer, R.M.; Fortinsky, R.H.; Rn, D.K.; Ma, C.B.; Covinsky, K.E. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J. Am. Geriatr. Soc. 2008, 56, e2179. [Google Scholar] [CrossRef] [PubMed]
- Hoogerduijn, J.G.; Buurman, B.M.; Korevaar, J.C.; Grobbee, D.E.; De Rooij, S.E.; Schuurmans, M.J. The prediction of functional decline in older hospitalised patients. Age Ageing 2012, 41, e387. [Google Scholar] [CrossRef]
- Brown, C.J.; Redden, D.T.; Flood, K.L.; Allman, R.M. The Underrecognized Epidemic of Low Mobility During Hospitalization of Older Adults. J. Am. Geriatr. Soc. 2009, 57, 1660–1665. [Google Scholar] [CrossRef]
- Surkan, M.J.; Gibson, W. Interventions to Mobilize Elderly Patients and Reduce Length of Hospital Stay. Can. J. Cardiol. 2018, 34, 881–888. [Google Scholar] [CrossRef]
- Gill, T.M.; Allore, H.G.; Gahbauer, E.A.; Murphy, T.E. Change in Disability After Hospitalization or Restricted Activity in Older Persons. JAMA 2010, 304, 1919. [Google Scholar] [CrossRef]
- Cuevas-Lara, C.; Izquierdo, M.; Gutiérrez-Valencia, M.; Marín-Epelde, I.; Zambom-Ferraresi, F.; Contreras-Escámez, B.; Martínez-Velilla, N.; Zambom-Ferrasi, F. Effectiveness of Occupational Therapy Interventions in Acute Geriatric Wards: A Systematic Review. Maturitas 2019, 127, 43–50. [Google Scholar] [CrossRef]
- Ali, Z.; Usman, M. A Framework for Game Engine Selection for Gamification and Serious Games. In FTC 2016 Proceedings of Future Technologies Conference; Institute of Electrical and Electronics Engineers Inc.: San Francisco, CA, USA, 2017; pp. 1199–1207. [Google Scholar] [CrossRef]
- Bonnechère, B.; Bonnechère, B. Serious Games in Rehabilitation. In Serious Games in Physical Rehabilitation; Springer International Publishing: Leuven, Belgium, 2018; pp. 41–109. [Google Scholar] [CrossRef]
- Groh, F. Gamification: State of the Art Definition and Utilization. In Proceedings of the 4th Seminar on Research Trends in Media Informatics; Institute of Media Informatics of the Ulm University: Ulm, Germany, 2012; pp. 39–46. [Google Scholar]
- Kapp, K. The Gamification of Learning and Instruction: Game-Based Methods and Strategies for Training and Education; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Gupta, A.; Gomathi, S. A Review on Gamification and Its Potential to Motivate and Engage Employees and Customers: Employee Engagement through Gamification. Int. J. Sociotechnology Knowl. Dev. 2017, 42–52. [Google Scholar] [CrossRef]
- Pereira, P.; Duarte, E.; Rebelo, F.; Noriega, P. A Review of Gamification for Health-Related Contexts. In Design, User Experience, and Usability. User Experience Design for Diverse Interaction Platforms and Environments; (DUXU 2014); Marcus, A., Ed.; Springer: Cham, Switzerland, 2014; Volume 8518 LNCS, pp. 742–753. [Google Scholar] [CrossRef]
- Gentry, S.V.; Gauthier, A.; L’Estrade Ehrstrom, B.; Wortley, D.; Lilienthal, A.; Tudor Car, L.; Dauwels-Okutsu, S.; Nikolaou, C.K.; Zary, N.; Campbell, J.; et al. Serious Gaming and Gamification Education in Health Professions: Systematic Review. J. Med. Internet Res. 2019, 21, e12994. [Google Scholar] [CrossRef] [PubMed]
- Kolb, N.A.; Smith, A.G.; Singleton, J.R.; Beck, S.L.; Howard, D.; Dittus, K.; Karafiath, S.; Mooney, K. Chemotherapy-Related Neuropathic Symptom Management: A Randomized Trial of an Automated Symptom-Monitoring System Paired with Nurse Practitioner Follow-Up. Support. Care Cancer 2018, 26, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Theng, Y.-L.; Lee, J.W.Y.; Patinadan, P.V.; Foo, S.S.B. The Use of Videogames, Gamification, and Virtual Environments in the Self-Management of Diabetes: A Systematic Review of Evidence. Games Health J. 2015, 4, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Klompstra, L.V.; Jaarsma, T.; Strömberg, A. Exergaming in Older Adults: A Scoping Review and Implementation Potential for Patients with Heart Failure. Eur. J. Cardiovasc. Nurs. 2014, 13, 388–398. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Lara, C.; Izquierdo, M.; De Asteasu, M.L.S.; Ramírez-Vélez, R.; Zambom-Ferraresi, F.; Zambom-Ferraresi, F.; Martínez-Velilla, N. Impact of Game-Based Interventions on Health-Related Outcomes in Hospitalized Older Patients: A Systematic Review. J. Am. Med. Dir. Assoc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Velilla, N.; Herrero, A.C.; Cadore, E.L.; Sáez de Asteasu, M.L.; Izquierdo, M. Iatrogenic Nosocomial Disability Diagnosis and Prevention. J. Am. Med. Dir. Assoc. 2016, 17, 762–764. [Google Scholar] [CrossRef] [PubMed]
- Richter, G.; Raban, D.R.; Rafaeli, S. Studying Gamification: The Effect of Rewards and Incentives on Motivation. In Gamification in Education and Business; Springer International Publishing: Cham, Switzerland, 2015; pp. 21–46. [Google Scholar] [CrossRef]
- Edwards, E.A.; Lumsden, J.; Rivas, C.; Steed, L.; Edwards, L.A.; Thiyagarajan, A.; Sohanpal, R.; Caton, H.; Griffiths, C.J.; Munafò, M.R.; et al. Gamification for Health Promotion: Systematic Review of Behaviour Change Techniques in Smartphone Apps. BMJ Open 2016, e012447. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 2191–2194. [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association with Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Simonsick, E.M.; Salive, M.E.; Wallace, R.B. Lower-Extremity Function in Persons over the Age of 70 Years as a Predictor of Subsequent Disability. N. Engl. J. Med. 1995, 332, 556–562. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared With the Short Physical Performance Battery. Journals Gerontol. Ser. A 2000, 55, M221–M231. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Pi, J.; Olivé, J.M.; Esteban, M. Mini Mental State Examination: Asociación de la puntuación obtenida con la edad y grado de alfabetización en una población anciana. Med. Clin. 1994, 103, 641–644. [Google Scholar]
- Brodaty, H.; Connors, M.H.; Loy, C.; Teixeira-Pinto, A.; Stocks, N.; Gunn, J.; Mate, K.E.; Pond, C.D. Screening for Dementia in Primary Care: A Comparison of the GPCOG and the MMSE. Dement. Geriatr. Cogn. Disord. 2016, 42, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Roth, M.; Tym, E.; Mountjoy, C.; Huppert, F.; Hendrie, H.; Vema, S.; Goddard, R. CAMDEX: A standardized instrument for the diagnosis of mental disorders in teh Elderly with the Special referente to the early detection of dementia. Br. J. Psychiatry 1986, 149, 698–709. [Google Scholar] [CrossRef] [PubMed]
- Vilalta, J.; Llinà, J.; López-Pousa, S.; Amiel, J.; Vidal, C. CAMDEX, validación de la adaptación española. Neurologia 1990, 5, 117–120. [Google Scholar]
- Van Bennekom, C.A.M.; Jelles, F.; Lankhorst, G.J.; Bouter, L.M. Responsiveness of the Rehabilitation Activities Profile and the Barthel Index. J. Clin. Epidemiol. 1996, 49, 39–44. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Martínez de la Iglesia, J.; Onís Vilches, M.C.; Dueñas Herrero, R.; Albert Colomer, C.; Aguado Taberné, C.; Luque Luque, R. Versión Española Del Cuestionario de Yesavage Abreviado (GDS) Para El Despistaje de Depresión En Mayores de 65 Años: Adaptación y Validación. MEDIFAM Rev. Med. Fam. y Comunitaria 2002, 12, 620–630. [Google Scholar] [CrossRef]
- García-Gordillo, M.Á.; del Pozo-Cruz, B.; Adsuar, J.C.; Cordero-Ferrera, J.M.; Abellán-Perpiñán, J.M.; Sánchez-Martínez, F.I. Validation and Comparison of EQ-5D-3L and SF-6D Instruments in a Spanish Parkinson’s Disease Population Sample. Nutr. Hosp. 2015, 2808–2821. [Google Scholar]
- Badia, X.; Roset, M.; Montserrat, S.; Herdman, M.; Segura, A. The Spanish version of EuroQol: A description and its applications. European Quality of Life scale. Med. Clin. (Barc). 1999, 112, 79–85. [Google Scholar] [PubMed]
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying Confusion: The Confusion Assessment Method. A New Method for Detection of Delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nyström, C.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Medicine 2017, 1821–1845. [Google Scholar] [CrossRef] [PubMed]
- Rantanen, T.; Guralnik, J.M.; Foley, D.; Masaki, K.; Leveille, S.; Curb, J.D.; White, L. Midlife Hand Grip Strength as a Predictor of Old Age Disability. J. Am. Med. Assoc. 1999, 281, 558–560. [Google Scholar] [CrossRef]
- Laukkanen, P.; Heikkinen, E.; Kauppinen, M. Muscle Strength and Mobility as Predictors of Survival in 75-84-Year-Old People. Age Ageing 1995, 24, 468–473. [Google Scholar] [CrossRef]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A Review of the Measurement of Grip Strength in Clinical and Epidemiological Studies: Towards a Standardised Approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and Analysis of Pilot Studies: Recommendations for Good Practice. J. Eval. Clin. Pract. 2004, 307–312. [Google Scholar] [CrossRef]
- Sim, J.; Lewis, M. The Size of a Pilot Study for a Clinical Trial Should Be Calculated in Relation to Considerations of Precision and Efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef]
- Hertzog, M.A. Considerations in Determining Sample Size for Pilot Studies. Res. Nurs. Heal. 2008, 31, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Sáez de Asteasu, M.L.; Martínez-Velilla, N.; Zambom-Ferraresi, F.; Casas-Herrero, Á.; Cadore, E.L.; Galbete, A.; Izquierdo, M. Assessing the Impact of Physical Exercise on Cognitive Function in Older Medical Patients during Acute Hospitalization: Secondary Analysis of a Randomized Trial. PLOS Med. 2019, 16, e1002852. [Google Scholar] [CrossRef]
- Martínez-Velilla, N.; Casas-Herrero, A.; Zambom-Ferraresi, F.; Sáez De Asteasu, M.L.; Lucia, A.; Galbete, A.; García-Baztán, A.; Alonso-Renedo, J.; González-Glaría, B.; Gonzalo-Lázaro, M.; et al. Effect of Exercise Intervention on Functional Decline in Very Elderly Patients During Acute Hospitalization: A Randomized Clinical Trial. JAMA Intern. Med. 2019, 179, 28–36. [Google Scholar] [CrossRef] [PubMed]

| Inclusion | Exclusion |
|---|---|
| Barthel Index score ≥60 points. | Expected length of stay <6 days. |
| Without major cognitive disorder or with mild cognitive impairment (Mini Mental State Examination ≥19; Global Deterioration Scale score = 1–3). | Uncontrolled arrhythmias, acute pulmonary embolism and myocardial infarction, or extremity bone fracture in the past 3 months. |
| Able to ambulate (with/without assistance). | Terminal illness. |
| The participant must be able to communicate and collaborate with the researchers. |
| Cognitive Area | Name of Game | Description | Sequences | Goals | Total Score | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Day 1 | 41 | |||||||||
 | Clock needles | Select the option that corresponds to the time shown on the clock. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Which figure is it? | Select the option that corresponds to the figure shown on the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Word soup | Select the option that corresponds to the word hidden in word soup. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Memorize the picture | Remember and select the option that corresponds to the image shown in the previous image. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Synonyms | Select the option that corresponds to the synonym of the word that appears on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 2 | 41 | |||||||||
 | Near or far | Select the option that corresponds to the nearest or farthest object in the picture on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Count the figures | Select the option that corresponds to the total number of figures displayed on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Follow the runner! | Select the option that corresponds to the position that a certain runner has reached. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | The proverb | Select the option that correctly completes the proverb. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | What is it called? | Select the option that corresponds to the utility of the object displayed on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 3 | 41 | |||||||||
 | Calendar | Select the option that corresponds to the date shown on the calendar. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Which figure is it? | Select the option that corresponds to the figure shown on the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | The highest number | Select the option that corresponds to the highest number displayed on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Count the boxes | Remember and select the option that corresponds to the numbers of boxes shown in the previous screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Categories | Select the option that corresponds to the word that is not related to that category of words. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 4 | 41 | |||||||||
 | Supermarket shelves | Select the option that corresponds to the position of the food of the picture that appears on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | The architect | Select the option that corresponds to the figure shown on the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Soup of Symbols | Select the option that corresponds to the number of a certain symbol indicated in each sequence. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Fruit basket | Select the option that corresponds to the fruits of the picture that appears on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Complete the sentence | Select the option that correctly completes the sentence. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 5 | 41 | |||||||||
 | Clock needles | Select the option that corresponds to the time shown on the clock. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Which figure is it? | Select the option that corresponds to the figure shown on the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Word soup | Select the option that corresponds to the word hidden in word soup. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Memorize the picture | Remember and select the option that corresponds to the image shown in the photo previous. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | The lost word | Select the option that contains the word that correctly completes the sentence. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 6 | 41 | |||||||||
 | Near or far | Select the option that corresponds to the nearest or farthest object in the picture on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Count the figures | Select the option that corresponds to the total number of figures displayed on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Follow the runner! | Select the option that corresponds to the position that a certain runner has reached. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | The proverb | Select the option that correctly completes the proverb. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | What would you take with you? | Select the option that contains the most appropriate object for the proposed scenario or situation. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 7 | 41 | |||||||||
 | Calendar | Select the option that corresponds to the date shown on the calendar. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Which figure is it? | Select the option that corresponds to the figure shown on the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | The highest number | Select the option that corresponds to the highest number displayed on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Count the boxes | Remember and select the option that corresponds to the numbers of boxes shown in the previous screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Situations | Select the option that corresponds to the action or activity shown in the image. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 8 | 41 | |||||||||
 | Supermarket shelves | Select the option that corresponds to the position of the food of the picture that appears on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | The architect | Select the option that corresponds to the figure shown in the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Soup of Symbols | Select the option that corresponds to the number of a certain symbol indicated in each sequence. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Fruit basket | Select the option that corresponds to the fruits of the picture that appears on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Categories | Select the option that corresponds to the word that does not correspond to that category of words. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
| Day 9 | 41 | |||||||||
 | Clock needles | Select the option that corresponds to the time shown in the clock. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Which figure is it? | Select the option that corresponds to the figure shown in the picture. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Word soup | Select the option that corresponds to the word hidden in word soup. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Memorize the picture | Remember and select the option that corresponds to the image shown in the previous image. | 6 | Select the correct option in less than 15 s. | 6 | |||||
 | Ferris wheel of letters | Select the word that can be formed from the letters that appear on the screen. | 6 | Select the correct option in less than 20 s. | 6 | |||||
 | Sequence of functional scopes | Press the button with the number that appears on the screen. | 11 | Select the correct option in less than 15 s. | 11 | |||||
 | Temporal orientation |  | Visual perception |  | Selective attention | |||||
 | Short-term, operational and working memory |  | Linguistic expression and understanding |  | Categorization and semantic awareness | |||||
 | Spatial orientation |  | Spatial perception |  | Sustained attention | |||||
 | Semantic memory |  | Denomination |  | Oculo-manual coordination control | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuevas-Lara, C.; Izquierdo, M.; Zambom-Ferraresi, F.; Sáez de Asteasu, M.L.; Marín-Epelde, I.; Chenhuichen, C.; Zambom-Ferraresi, F.; Ramírez-Vélez, R.; García-Hermoso, A.; Casas-Herrero, Á.; et al. A Feasibility Study for Implementation “Health Arcade”: A Study Protocol for Prototype of Multidomain Intervention Based on Gamification Technologies in Acutely Hospitalized Older Patients. Int. J. Environ. Res. Public Health 2020, 17, 8058. https://doi.org/10.3390/ijerph17218058
Cuevas-Lara C, Izquierdo M, Zambom-Ferraresi F, Sáez de Asteasu ML, Marín-Epelde I, Chenhuichen C, Zambom-Ferraresi F, Ramírez-Vélez R, García-Hermoso A, Casas-Herrero Á, et al. A Feasibility Study for Implementation “Health Arcade”: A Study Protocol for Prototype of Multidomain Intervention Based on Gamification Technologies in Acutely Hospitalized Older Patients. International Journal of Environmental Research and Public Health. 2020; 17(21):8058. https://doi.org/10.3390/ijerph17218058
Chicago/Turabian StyleCuevas-Lara, César, Mikel Izquierdo, Fabiola Zambom-Ferraresi, Mikel L. Sáez de Asteasu, Itxaso Marín-Epelde, Chenhui Chenhuichen, Fabricio Zambom-Ferraresi, Robinson Ramírez-Vélez, Antonio García-Hermoso, Álvaro Casas-Herrero, and et al. 2020. "A Feasibility Study for Implementation “Health Arcade”: A Study Protocol for Prototype of Multidomain Intervention Based on Gamification Technologies in Acutely Hospitalized Older Patients" International Journal of Environmental Research and Public Health 17, no. 21: 8058. https://doi.org/10.3390/ijerph17218058
APA StyleCuevas-Lara, C., Izquierdo, M., Zambom-Ferraresi, F., Sáez de Asteasu, M. L., Marín-Epelde, I., Chenhuichen, C., Zambom-Ferraresi, F., Ramírez-Vélez, R., García-Hermoso, A., Casas-Herrero, Á., Capón-Sáez, A., Lozano-Vicario, L., Criado-Martín, I., Sánchez-Latorre, M., Antoñanzas-Valencia, C., & Martínez-Velilla, N. (2020). A Feasibility Study for Implementation “Health Arcade”: A Study Protocol for Prototype of Multidomain Intervention Based on Gamification Technologies in Acutely Hospitalized Older Patients. International Journal of Environmental Research and Public Health, 17(21), 8058. https://doi.org/10.3390/ijerph17218058










