Voluntary Reduction of Social Interaction during the COVID-19 Pandemic in Taiwan: Related Factors and Association with Perceived Social Support
Abstract
1. Introduction
1.1. Reduction of Social Interaction and Social Support during the Coronavirus Disease 2019 Pandemic
1.2. Factors Related to the Reduction of Social Interaction
1.3. COVID-19 Pandemic in Taiwan
1.4. Aims of This Study
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Voluntary Reduction of Social Interaction
2.2.2. Perceived Social Support
2.2.3. Worry about Contracting COVID-19
2.2.4. General Anxiety
2.2.5. Demographic Variables
2.3. Statistical Analysis
3. Results
3.1. Proportion of Respondents Who Voluntarily Reduced Their Social Interaction
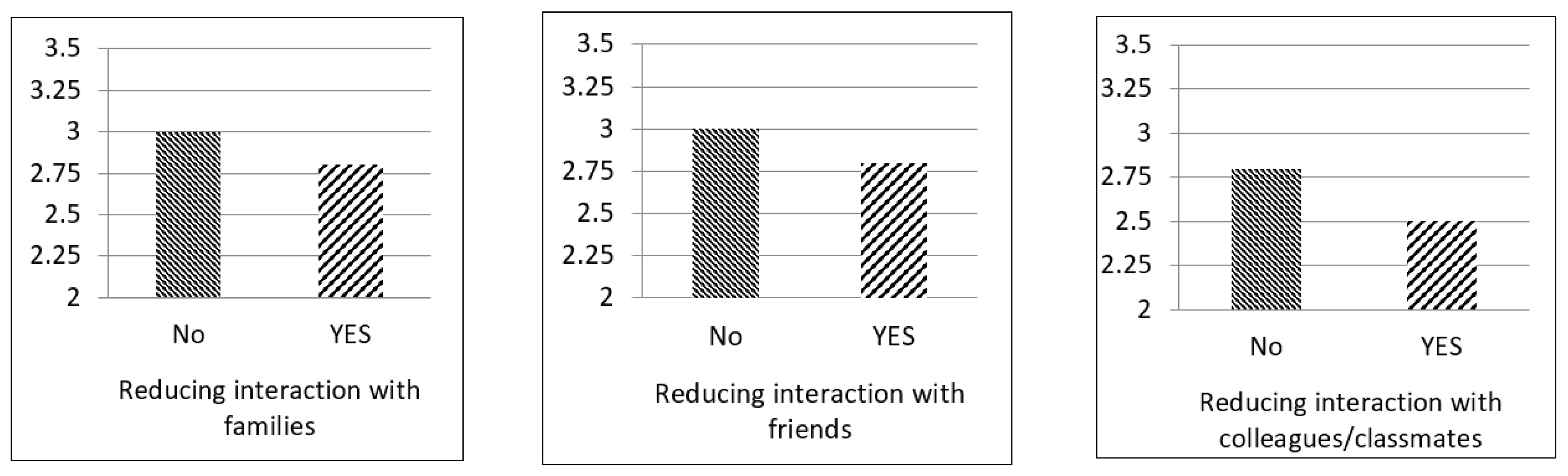
3.2. Association between the Voluntary Reduction of Social Interaction and Perceived Social Support
3.3. Factors Related to the Voluntary Reduction of Social Interaction
4. Discussion
4.1. Voluntary Reduction of Social Interaction and Its Association with Perceived Social Support
4.2. Factors Related to Voluntary Reduction of Social Interaction
4.3. Future Research
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Science and Engineering at Johns Hopkins. Modeling 2019-nCoV. Available online: https://systems.jhu.edu/research/public-health/ncov-model (accessed on 18 July 2020).
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Lee, Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry 2020, 19, 250. [Google Scholar] [CrossRef]
- Crayne, M.P. The traumatic impact of job loss and job search in the aftermath of COVID-19. Psychol. Trauma 2020, 12, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19-related school closings and risk of weight gain among children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef]
- Moore, S.A.; Faulkner, G.; Rhodes, R.E.; Brussoni, M.; Chulak-Bozzer, T.; Ferguson, L.J.; Mitra, R.; O’Reilly, N.; Spence, J.C.; Vanderloo, L.M.; et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: A national survey. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 85. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus and COVID-19 pandemic: A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Oksanen, A.; Kaakinen, M.; Latikka, R.; Savolainen, I.; Savela, N.; Koivula, A. Regulation and trust: 3-month follow-up study on COVID-19 mortality in 25 European countries. JMIR Public Health Surveill. 2020, 6, e19218. [Google Scholar] [CrossRef]
- Pollitt, K.J.G.; Peccia, J.; Ko, A.I.; Kaminski, N.; Dela Cruz, C.S.; Nebert, D.W.; Reichardt, J.K.V.; Thompson, D.C.; Vasiliou, V. COVID-19 vulnerability: The potential impact of genetic susceptibility and airborne transmission. Hum. Genom. 2020, 14, 17. [Google Scholar] [CrossRef]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Glass, R.J.; Glass, L.M.; Beyeler, W.E.; Min, H.J. Targeted social distancing design for pandemic influenza. Emerg. Infect. Dis. 2006, 12, 1671–1681. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Bavel, J.J.V.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef] [PubMed]
- Cooke, B.; Rossmann, M.; McCubbin, H.; Patterson, J. Examining the definition and assessment of social support: A resource for individuals and families. Fam. Relat. 1988, 37, 211–216. [Google Scholar] [CrossRef]
- Zysberg, L.; Zisberg, A. Days of worry: Emotional intelligence and social support mediate worry in the COVID-19 pandemic. J. Health Psychol. 2020, 1–10. [Google Scholar] [CrossRef]
- Ye, Z.; Yang, X.; Zeng, C.; Wang, Y.; Shen, Z.; Li, X.; Lin, D. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl. Psychol. Health Well Being 2020. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef]
- Labrague, L.J.; De Los Santos, J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020. [Google Scholar] [CrossRef]
- Rozanova, J.; Shenoi, S.; Zaviryukha, I.; Zeziulin, O.; Kiriazova, T.; Rich, K.; Mamedova, E.; Yariy, V. Social support is key to retention in care during COCID-19 pandemic among older people with HIV and substance use disorders in Ukraine. Subst. Use Misuse 2020, 55, 1902–1904. [Google Scholar] [CrossRef]
- Pantell, M.S.; Shields-Zeeman, L. Maintaining social connections in the setting of COVID-19 social distancing: A call to action. Am. J. Public Health 2020, 110, 1367–1368. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior: Theory, Research, and Practice; Jossey-Bass: San Francisco, CA, USA, 2015. [Google Scholar]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the health belief model. Health Educ. Behav. 1988, 15, 175–183. [Google Scholar] [CrossRef]
- Xie, K.; Liang, B.; Dulebenets, M.A.; Mei, Y. The impact of risk perception on social distancing during the COVID-19 pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 6256. [Google Scholar] [CrossRef] [PubMed]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef]
- Vytal, K.E.; Arkin, N.E.; Overstreet, C.; Lieberman, L.; Grillon, C. Induced-anxiety differentially disrupts working memory in generalized anxiety disorder. BMC Psychiatry 2016, 16, 62. [Google Scholar] [CrossRef]
- Xie, W.; Campbell, S.; Zhang, W. Working memory capacity predicts individual differences in social-distancing compliance during the COVID-19 pandemic in the United States. Proc. Natl. Acad. Sci. USA 2020, 117, 17667–17674. [Google Scholar] [CrossRef] [PubMed]
- Przeworski, A.; Newman, M.G.; Pincus, A.L.; Kasoff, M.B.; Yamasaki, A.S.; Castonguay, L.G.; Berlin, K.S. Interpersonal pathoplasticity in individuals with generalized anxiety disorder. J. Abnorm. Psychol. 2011, 120, 286–298. [Google Scholar] [CrossRef]
- Zhang, J.; Litvinova, M.; Liang, Y.; Wang, Y.; Wang, W.; Zhao, S.; Wu, Q.; Merler, S.; Viboud, C.; Vespignani, A.; et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 2020, 368, 1481–1486. [Google Scholar] [CrossRef]
- Alsan, M.; Stantcheva, S.; Yang, D.; Cutler, D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw. Open 2020, 3, e2012403. [Google Scholar] [CrossRef]
- Cheng, H.-Y.; Li, S.-Y.; Yang, C.-H. Initial rapid and proactive response for the COVID-19 outbreak—Taiwan’s experience. J. Formos. Med. Assoc. 2020, 119, 771–773. [Google Scholar] [CrossRef]
- Taiwan Centers for Disease Control. COVID-19. Available online: https://www.cdc.gov.tw/ (accessed on 18 July 2020).
- World Health Organization. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. 2004. Available online: https://www.who.int/csr/sars/country/table2004_04_21/en/ (accessed on 6 September 2020).
- Wang, P.W.; Lu, W.H.; Ko, N.Y.; Chen, Y.L.; Li, D.J.; Chang, Y.P.; Yen, C.F. COVID-19-related information sources and the relationship with confidence in people coping with COVID-19: Facebook survey study in Taiwan. J. Med. Internet Res. 2020, 22, e20021. [Google Scholar] [CrossRef]
- Ramo, D.E.; Rodriguez, T.M.; Chavez, K.; Sommer Prochaska, J.J. Facebook recruitment of young adult smokers for a cessation trial: Methods, metrics, and lessons learned. Internet Interv. 2014, 1, 58–64. [Google Scholar] [CrossRef]
- Liao, Q.; Cowling, B.J.; Lam, W.W.; Ng, D.M.; Fielding, R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 in Hong Kong: Ten cross-sectional surveys. BMC Infect. Dis. 2014, 14, 169. [Google Scholar] [CrossRef]
- Leung, G.M.; Ho, L.M.; Chan, S.K.; Ho, S.Y.; Bacon-Shone, J.; Choy, R.Y.; Hedley, A.J.; Lam, T.H.; Fielding, R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005, 40, 1713–1720. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.; Gorusch, R.; Luschene, R. State Trait Anxiety Inventory: A Test Manual/Test Form; Consulting Psychologists Press: Palo Alto, CA, USA, 1970. [Google Scholar]
- Bolger, N.; Eckenrode, J. Social relationships, personality, and anxiety during a major stressful event. J. Pers. Soc. Psychol. 1991, 61, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.N.; Armitage, C.J.; Tampe, T.; Dienes, K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: A UK-based focus group study. BMJ Open 2020, 10, e039334. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Xia, G.; Pang, P.; Wu, B.; Wei, J.; Li, Y.T.; Wang, M.; Ling, Q.; Chang, X.; Wang, J.; et al. COVID-19 epidemic peer support and crisis intervention via social media. Community Ment. Health J. 2020, 56, 786–792. [Google Scholar] [CrossRef]
- Nouri, S.; Khoong, E.C.; Lyles, C.R.; Karliner, L. Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic. NEJM Catal. Innov. Care Deliv. 2020. [Google Scholar] [CrossRef]
- Dionne, G.; Desjardins, D.; Lebeau, M.; Messier, S.; Dascal, A. Health care workers’ risk perceptions and willingness to report for work during an influenza pandemic. Risks 2018, 6, 8. [Google Scholar] [CrossRef]
- Hua, J.; Shaw, R. Corona virus (COVID-19) “infodemic” and emerging issues through a data lens: The case of China. Int. J. Environ. Res. Public Health 2020, 17, 2309. [Google Scholar] [CrossRef]
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—An update on the status. Mil. Med. Res. 2020, 7, 11. [Google Scholar] [CrossRef]
- Plagg, B.; Engl, A.; Piccoliori, G.; Eisendle, K. Prolonged social isolation of the elderly during COVID-19: Between benefit and damage. Arch. Gerontol. Geriatr. 2020, 89, 104086. [Google Scholar] [CrossRef]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- Bobkowski, P.; Smith, J. Social media divide: Characteristics of emerging adults who do not use social network websites. Media Cult. Soc. 2013, 35, 771–781. [Google Scholar] [CrossRef]
| Variables | n (%) | Mean (SD) | Range |
|---|---|---|---|
| Sex | |||
| Women | 1305 (66.8) | ||
| Men | 649 (33.2) | ||
| Age | |||
| Younger | 1000 (51.2) | ||
| Older | 954 (48.8) | ||
| Education level | |||
| High (university or above) | 1736 (88.8) | ||
| Low (high school or below) | 218 (11.2) | ||
| Reduction of social interaction with others | |||
| Family members | 217 (11.1) | ||
| Friends | 744 (38.1) | ||
| Colleagues or classmates | 706 (36.1) | ||
| One form | 213 (10.9) | ||
| Two forms | 454 (23.2) | ||
| Three forms | 182 (9.3) | ||
| Perceived social support | |||
| Family members | 3.0 (0.8) | 0–4 | |
| Friends | 2.9 (0.7) | 0–4 | |
| Colleagues or classmates | 2.7 (0.8) | 0–4 | |
| Worry about contracting COVID-19 | |||
| Low | 998 (51.1) | ||
| High | 956 (48.9) | ||
| General anxiety | |||
| Low | 1011 (51.7) | ||
| High | 943 (48.3) |
| Variables | Perceived Support from Family Members | Perceived Support from Friends | Perceived Support from Colleagues/Classmates | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI of B | p | B | 95% CI of B | p | B | 95% CI of B | p | |
| Reduction of interactions with a | |||||||||
| Family members | −0.075 | −0.300, −0.078 | 0.001 | ||||||
| Friends | −0.105 | −0.220, −0.088 | <0.001 | ||||||
| Colleagues/classmates | −0.112 | −0.268, −0.115 | <0.001 | ||||||
| Men b | 0.044 | 0.000, 0.148 | 0.052 | −0.026 | −0.107, 0.028 | 0.243 | 0.016 | −0.049, 0.107 | 0.479 |
| Older age c | 0.074 | 0.049, 0.191 | 0.001 | −0.002 | −0.076, 0.054 | 0.945 | 0.076 | 0.044, 0.194 | 0.001 |
| Low education level d | −0.050 | −0.244, −0.018 | 0.027 | −0.061 | −0.240, −0.035 | 0.007 | −0.018 | −0.166, 0.070 | 0.442 |
| Variables | Reduction of Interactions with Family Members | Reduction of Interactions with Friends | Reduction of Interactions with Colleagues/Classmates | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI of OR | p | OR | 95% CI of OR | p | OR | 95% CI of OR | p | |
| Men a | 1.025 | 0.749, 1.401 | 0.879 | 0.993 | 0.810, 1.219 | 0.949 | 1.270 | 1.036, 1.557 | 0.022 |
| Older age b | 1.388 | 1.034, 1.863 | 0.029 | 1.796 | 1.477, 2.183 | <0.001 | 1.587 | 1.305, 1.931 | <0.001 |
| Low education level c | 0.882 | 0.543, 1.435 | 0.614 | 0.705 | 0.513, 0.969 | 0.031 | 0.749 | 0.544, 1.030 | 0.076 |
| High worry about contracting COVID-19 d | 2.103 | 1.536, 2.879 | <0.001 | 2.508 | 2.051, 3.067 | <0.001 | 2.305 | 1.884, 2.821 | <0.001 |
| High general anxiety e | 1.851 | 1.346, 2.546 | <0.001 | 1.206 | 0.984, 1.480 | 0.072 | 1.210 | 0.986, 1.485 | 0.068 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chou, W.-P.; Wang, P.-W.; Chen, S.-L.; Chang, Y.-P.; Wu, C.-F.; Lu, W.-H.; Yen, C.-F. Voluntary Reduction of Social Interaction during the COVID-19 Pandemic in Taiwan: Related Factors and Association with Perceived Social Support. Int. J. Environ. Res. Public Health 2020, 17, 8039. https://doi.org/10.3390/ijerph17218039
Chou W-P, Wang P-W, Chen S-L, Chang Y-P, Wu C-F, Lu W-H, Yen C-F. Voluntary Reduction of Social Interaction during the COVID-19 Pandemic in Taiwan: Related Factors and Association with Perceived Social Support. International Journal of Environmental Research and Public Health. 2020; 17(21):8039. https://doi.org/10.3390/ijerph17218039
Chicago/Turabian StyleChou, Wei-Po, Peng-Wei Wang, Shiou-Lan Chen, Yu-Ping Chang, Chia-Fen Wu, Wei-Hsin Lu, and Cheng-Fang Yen. 2020. "Voluntary Reduction of Social Interaction during the COVID-19 Pandemic in Taiwan: Related Factors and Association with Perceived Social Support" International Journal of Environmental Research and Public Health 17, no. 21: 8039. https://doi.org/10.3390/ijerph17218039
APA StyleChou, W.-P., Wang, P.-W., Chen, S.-L., Chang, Y.-P., Wu, C.-F., Lu, W.-H., & Yen, C.-F. (2020). Voluntary Reduction of Social Interaction during the COVID-19 Pandemic in Taiwan: Related Factors and Association with Perceived Social Support. International Journal of Environmental Research and Public Health, 17(21), 8039. https://doi.org/10.3390/ijerph17218039






