Parental Attitudes to Childhood Overweight: The Multiple Paths through Healthy Eating, Screen Use, and Sleeping Time
Abstract
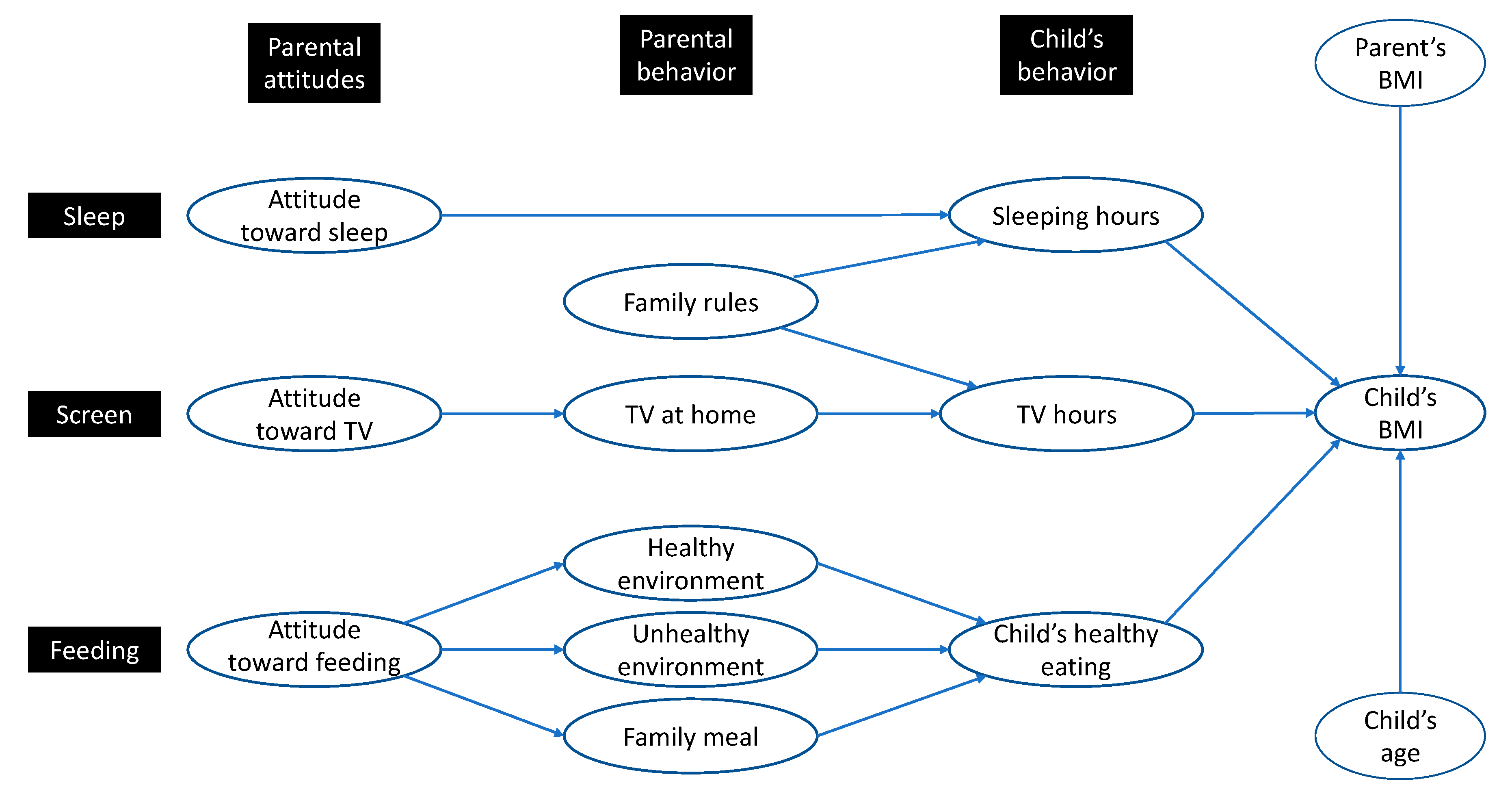
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Sample Description
3.2. Descriptives, Reliability and Validity
3.3. Model Estimation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (2020). Report 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 26 October 2020).
- De Onis, M.; Blössner, M.; Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 2010, 92, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Potter, L.; Wallston, K.; Trief, P.; Ulbrecht, J. Attributing discrimination to weight: Associations with well-being, self-care, and disease status in patients with type 2 diabetes mellitus. J. Behav. Med. 2015, 38, 863–875. [Google Scholar] [CrossRef] [PubMed]
- De Costa, P.; Moller, P.; Frost, M.B.; Olsen, A. Changing children’s eating behaviour—A review of experimental research. Appetite 2017, 113, 327–357. [Google Scholar] [CrossRef]
- Romanos-Nanclares, A.; Zazpe, I.; Santiago, S.; Marín, L.; Rico-Campà, A.; Martín-Calvo, N. Influence of Parental Healthy-Eating Attitudes and Nutritional Knowledge on Nutritional Adequacy and Diet Quality among Preschoolers: The SENDO Project. Nutrients 2018, 10, 1875. [Google Scholar] [CrossRef]
- Lydecker, J.A.; Grilo, C.M. The apple of their eye: Attitudinal and behavioral correlates of parents’ perceptions of child obesity. Obesity 2016, 24, 1124–1131. [Google Scholar] [CrossRef]
- Michie, S.; Abraham, C. Interventions to change health behaviours: Evidence-based or evidence-inspired? Psychol. Health 2004, 19, 29–49. [Google Scholar] [CrossRef]
- Sleddens, E.F.C.; Gerards, S.M.; Thijs, C.; de Vries, N.K.; Kremers, S.P.J. General parenting, childhood overweight and obesity-inducing behaviors: A review. Int. J. Pediatric Obes. 2011, 6, 12–27. [Google Scholar] [CrossRef]
- Rhee, K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. Ann. Am. Acad. Political Soc. Sci. 2008, 615, 11–37. [Google Scholar] [CrossRef]
- Koplan, J.P.; Liverman, C.T.; Kraak, V.I. Preventing Childhood Obesity (National A); National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Birch, L.; Fisher, J. Development of Eating Behaviors among Children and Adolescents. Pediatrics 1998, 101 (Suppl. 2), 539–549. [Google Scholar]
- Trost, S.G.; Sallis, J.F.; Pate, R.R.; Freedson, P.S.; Taylor, W.C.; Dowda, M. Evaluating a model of parental influence on youth physical activity. Am. J. Prev. Med. 2003, 25, 277–282. [Google Scholar] [CrossRef]
- Barradas, D.T.; Fulton, J.E.; Blanck, H.M.; Huhman, M. Parental influences on youth television viewing. J. Pediatrics 2007, 151, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Maher, C.A.; Matricciani, L.; Olds, T.S. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int. J. Obes. 2013, 37, 546–551. [Google Scholar] [CrossRef]
- Taheri, S. The link between short sleep duration and obesity: We should recommend more sleep to prevent obesity. Arch. Dis. Child. 2006, 91, 881–884. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Beydoun, M.A.; Wang, Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity 2008, 16, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Buxton, O.M.; Chang, A.M.; Spilsbury, J.C.; Bos, T.; Emsellem, H.; Knutson, K.L. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health 2015, 1, 15–27. [Google Scholar] [CrossRef]
- Gibson, S.; Lambert, J.; Neate, D. Associations between weight status, physical activity, and consumption of biscuits, cakes and confectionery among young people in Britain. Nutr. Bull. 2004, 29, 301–309. [Google Scholar] [CrossRef]
- Riddoch, C.J.; Andersen, L.B.; Wedderkopp, N.; Harro, M.; Klasson-Heggebø, L.; Sardinha, L.B.; Cooper, A.R.; Ekelund, U. Physical activity levels and patterns of 9- and 15-yr-old European children. Med. Sci. Sports Exerc. 2004, 36, 86–92. [Google Scholar] [CrossRef]
- Biddle, S.J.; Gorely, T.; Marshall, S.J. Is television viewing a suitable marker of sedentary behavior in young people? Ann. Behav. Med. 2009, 38, 147–153. [Google Scholar] [CrossRef]
- Danner, F.W. A national longitudinal study of the association between hours of TV viewing and the trajectory of BMI growth among US children. J. Pediatric Psychol. 2008, 33, 1100–1107. [Google Scholar] [CrossRef]
- Dennison, B.A.; Erb, T.A.; Jenkins, P.L. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics 2002, 109, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Francis, L.; Lee, Y.; Birch, L. Parental weight status and girls’ television viewing, snacking, and body mass indexes. Obes. Res. 2003, 11, 143–151. [Google Scholar] [CrossRef]
- Jago, R.; Baranowski, T.; Baranowski, J.C.; Thompson, D.; Greaves, K.A. BMI from 3–6 y of age is predicted by TV viewing and physical activity, not diet. Int. J. Obes. 2005, 29, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Van Zutphen, M.; Bell, A.C.; Kremer, P.J.; Swinburn, B.A. Association between the family environment and television viewing in Australian children. J. Paediatr. Child Health 2007, 43, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Mazur, A.; Caroli, M.; Radziewicz-Winnicki, I.; Nowicka, P.; Weghuber, D.; Neubauer, D.; Dembiński, Ł.; Crawley, F.P.; White, M.; Hadjipanayis, A. Reviewing and addressing the link between mass media and the increase in obesity among European children: The European Academy of Paediatrics and The European Childhood Obesity Group consensus statement. Acta Paediatr. 2018, 107, 568–576. [Google Scholar] [CrossRef]
- Lobstein, T.; Davies, S. Defining and labelling healthy and unhealthy food. Public Health Nutr. 2008, 12, 331–340. [Google Scholar] [CrossRef]
- Hammons, A.J.; Fiese, B.H. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics 2011, 127, 1565–1574. [Google Scholar] [CrossRef]
- Maccoby, E.E. The Role of Parents in the Socialization of Children. Dev. Psychol. 1992, 28, 1006–1017. [Google Scholar] [CrossRef]
- Hutchinson, S.L.; Baldwin, C.K. The power of parents: Positive parenting to maximize youth’s potential. In Recreation and Youth Development; Witt, P.A., Caldwell, L.L., Eds.; Venture Publishing: State College, PA, USA, 2005; pp. 243–264. [Google Scholar]
- Scaglioni, S.; Salvioni, M.; Galimberti, C. Influence of parental attitudes in the development of children eating behaviour. Br. J. Nutr. 2008, 99, S22–S25. [Google Scholar] [CrossRef]
- Glasman, L.R.; Albarracín, D. Forming attitudes that predict future behavior: A meta-analysis of the attitude-behavior relation. Psychol. Bull. 2006, 132, 778–822. [Google Scholar] [CrossRef]
- Baranowski, T.; O’Connor, T.; Hughes, S.; Sleddens, E.; Beltran, A.; Frankel, L.; Mendoza, J.A.; Baranowski, J. We have a problem! Measurement of parenting. Child. Obes. 2013, 9, 1–4. [Google Scholar] [CrossRef] [PubMed]
- LeCroy, M.N.; Siega-Riz, A.M.; Albrecht, S.S.; Ward, D.S.; Cai, J.; Perreira, K.M.; Isasi, C.R.; Mossavar-Rahmani, Y.; Gallo, L.C.; Castañeda, S.F.; et al. Association of food parenting practice patterns with obesogenic dietary intake in Hispanic/Latino youth: Results from the Hispanic Community Children’s Health Study/Study of Latino Youth (SOL Youth). Appetite 2019, 140, 277–287. [Google Scholar] [CrossRef]
- Adam, E.K.; Snell, E.K.; Pendry, P. Sleep timing and quantity in ecological and family context: A nationally representative time-diary study. J. Fam. Psychol. 2007, 21, 4–19. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.; Ogden, J. Children’s eating attitudes and behaviour: A study of the modelling and control theories of parental influence. Health Educ. Res. 2004, 19, 261–271. [Google Scholar] [CrossRef]
- Hearn, M.D.; Baranowski, T.; Baranowski, J.; Doyle, C.; Smith, M.; Lin, L.S.; Resnicow, K. Environmental Influences on Dietary Behavior among Children: Availability and Accessibility of Fruits and Vegetables Enable Consumption. J. Health Educ. 1998, 29, 26–32. [Google Scholar] [CrossRef]
- Hendy, H.M.; Williams, K.E.; Camise, T.S. Kid’s Choice Program improves weight management behaviors and weight status in school children. Appetite 2011, 56, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Birch, L.L.; Johnson, S.L.; Grimm-Thomas, K.; Fisher, J.O. The child feeding questionnaire (CFQ) an instrument for assessing parental control in child feeding. Appetite 2001, 36, 201–210. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019; Available online: https://www.R-project.org/ (accessed on 25 October 2020).
- Revelle, W. Psych: Procedures for Personality and Psychological Research; Northwestern University: Evanston, IL, USA, 2018; Available online: https://CRAN.R-project.org/package=psych (accessed on 25 October 2020).
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Tatham, R.L. Multivariate Data Analysis, 7th ed.; Prentice-Hall: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Lindell, M.; Whitney, D. Accounting for common method variance in cross-sectional research designs. J. Appl. Psychol. 2001, 86, 114–120. [Google Scholar] [CrossRef]
- Matricciani, L.; Paquet, C.; Galland, B.; Short, M.; Olds, T. Children’s sleep and health: A metareview. Sleep Med. Rev. 2019, 46, 136–150. [Google Scholar] [CrossRef] [PubMed]
- Kelman, S. Unleashing Change: A Study of Organizational Renewal in Government; Technical Notes; Brookings Institution Press: Washington, DC, USA, 2005; Available online: https://scholar.harvard.edu/files/skelman/files/technicalfootnotes.pdf (accessed on 25 October 2020).
- Draxten, M.; Fulkerson, J.A.; Friend, S.; Flattum, C.F.; Schow, R. Parental role modeling of fruits and vegetables at meals and snacks is associated with children’s adequate consumption. Appetite 2014, 78, 1–7. [Google Scholar] [CrossRef] [PubMed]
- De Bourdeaudhuij, I.; Velde, S.; Brug, J.; Due, P.; Wind, M.; Sandvik, C.; Klepp, K.-I. Personal, social and environmental predictors of daily fruit and vegetable intake in 11-year-old children in nine European countries. Eur. J. Clin. Nutr. 2008, 62, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Moksony, F. Small Is Beautiful: The Use and Interpretation of R2 in Social Research. Szociologiai Szemle 1990, 130–138, (Special Issue). [Google Scholar]
| Variables and Items | Mean | Standard Deviation | ||
|---|---|---|---|---|
| Parental Attitudes | ||||
| Attitude toward sleep (Likert 1–5) | ||||
| Is healthy for my child to sleep a lot | 3.53 | 1.22 | ||
| I like my child to sleep for a long time | 3.25 | 1.19 | ||
| Attitude toward TV/screen (Likert 1–5) | ||||
| It is harmful that my child watches TV/screen (reversed) | 1.91 | 1.02 | ||
| Watching TV/screen is healthy entertainment for my child | 1.98 | 0.90 | ||
| Attitude toward feeding (Likert 1–5) | ||||
| I like to be responsible in feeding my child | 4.61 | 0.72 | ||
| I like to decide if my child has taken the right foods | 4.55 | 0.71 | ||
| I like to decide the size of the portions my child takes | 2.56 | 1.25 | ||
| Parental Behavior | ||||
| Family rules (1 = never, 5 = always) | ||||
| You require your child to keep his room clean and tidy | 4.43 | 0.81 | ||
| You require your child put aside dirty clothes | 4.56 | 0.80 | ||
| You set certain limits on TV/screen watching and time to be home | 4.24 | 0.95 | ||
| You enforce the rules you establish | 4.28 | 0.80 | ||
| Availability of TV at home | ||||
| Days your child has dinner while watching TV/screen | 4.13 | 2.78 | ||
| Number of TVs/screens you have at home | 2.28 | 1.01 | ||
| Healthy environment (0–7 days in the week) | ||||
| Days you have fruit available at home | 6.43 | 1.27 | ||
| Days you serve peeled fruit for dinner | 3.36 | 2.55 | ||
| Days you eat fruit | 5.40 | 1.96 | ||
| Days you eat vegetables | 5.38 | 1.73 | ||
| Unhealthy environment (0–7 days in the week) | ||||
| Days you drink sugared sodas | 2.23 | 2.28 | ||
| Days you eat candy, chocolate, or sweets | 1.81 | 1.65 | ||
| Days you eat salty snacks: chips, peanuts, etc. | 1.72 | 1.47 | ||
| Family meal (0–7 days in the week) | ||||
| Days you have dinner with your child | 5.01 | 2.47 | ||
| Days you prepare your child a dinner specially for him/her (reversed) | 6.10 | 1.70 | ||
| Days you serve your child a little of each of the meals on the table | 4.68 | 2.60 | ||
| Child’s Behavior | ||||
| Sleeping hours | ||||
| Number of hours per day that the child sleeps | 9.70 | 0.61 | ||
| TV/screen hours | ||||
| Number of hours per day the child watches TV/screen | 2.02 | 1.03 | ||
| Child’s healthy eating (0–7 days) | ||||
| Days a week your child eats fruit at home | 5.01 | 2.04 | ||
| Days a week your child eats dinner with vegetables | 3.26 | 2.10 | ||
| Days a week your child drinks sugared soda (reversed) | 5.71 | 1.67 | ||
| Dependent Variable | ||||
| Child’s BMI | 17.89 | 3.18 | ||
| Control Variables | ||||
| Parent’s BMI | 24.38 | 4.16 | ||
| Child’s age | 8.93 | 1.75 | ||
| Gender Distribution | ||||
| Parents (% female) | 83.37 | |||
| Children (% female) | 51.28 | |||
| Variables/Constructs and Items | λ 1 | ρ | AVE | Cronbach’s Alpha |
|---|---|---|---|---|
| Attitude toward sleep (Likert 1–5) | 0.88 | 0.79 | 0.88 | |
| Is healthy for my child to sleep a lot | 0.94 | |||
| I like my child to sleep for a long time | 0.84 | |||
| Attitude toward feeding (Likert 1–5) | 0.69 | 0.53 | 0.69 | |
| I like to be responsible in feeding my child | 0.73 | |||
| I like to decide if my child has taken the right foods | 0.72 | |||
| Family rules (Likert 1–5) | 0.69 | 0.43 | 0.68 | |
| You require your child to keep his room clean and tidy | 0.76 | |||
| You require your child put aside dirty clothes | 0.63 | |||
| You enforce the rules you establish | 0.54 |
| Constructs | Attitude toward Sleep | Attitude toward Feeding | Family Rules |
|---|---|---|---|
| Attitude toward sleep | 1 | ||
| Attitude toward feeding | 0.04 | 1 | |
| Family rules | −0.10 | 0.35 | 1 |
| Path | Model 1 | Model 2 |
|---|---|---|
| Parental Attitude toward TV → Availability of TV at home | 0.16 (4.99) *** | 0.16 (4.99) *** |
| Parental Attitude toward feeding → Healthy environment | 0.24 (5.23) *** | 0.24 (5.23) *** |
| Parental Attitude toward feeding → Unhealthy environment | −0.20 (−4.25) *** | −0.20 (−4.25) *** |
| Parental Attitude toward feeding → Family meal | 0.26 (5.98) *** | 0.26 (5.98) *** |
| Parental Attitude toward sleep → Child’s Sleeping hours | 0.07 (1.98) * | 0.07 (1.98) * |
| Family rules → Child´s Sleeping hours | 0.20 (4.89) *** | 0.20 (4.89) *** |
| Family rules → Child´s TV hours | −0.10 (−2.68) ** | −0.10 (−2.68) ** |
| Availability of TV at home → Child´s TV hours | 0.21 (6.49) *** | 0.21 (6.49) *** |
| Availability of TV at home → Child´s Healthy eating | −0.06 (−2.02) * | |
| Healthy environment → Child´s Healthy eating | 0.44 (16.04) *** | 0.44 (15.99) *** |
| Unhealthy environment → Child´s Healthy eating | −0.15 (−5.05) *** | −0.15 (−4.80) *** |
| Family meal → Child´s Healthy eating | 0.16 (5.26) *** | 0.16 (5.13) *** |
| Child´s Sleeping hours → Child´s BMI | −0.08 (−2.46) * | −0.08 (−2.46) * |
| Child´s TV hours → Child´s BMI | 0.13 (4.53) *** | 0.13 (4.50) *** |
| Child´s Healthy eating → Child’s BMI | 0.00 (0.14) ns | |
| Child’s age → Child’s BMI | 0.17 (4.12) *** | 0.17 (4.11) *** |
| Parent’s BMI → Child’s BMI | 0.26 (8.14) *** | 0.26 (8.14) *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giménez Garcia-Conde, M.; Marin, L.; Ruiz de Maya, S.; Cuestas, P.J. Parental Attitudes to Childhood Overweight: The Multiple Paths through Healthy Eating, Screen Use, and Sleeping Time. Int. J. Environ. Res. Public Health 2020, 17, 7885. https://doi.org/10.3390/ijerph17217885
Giménez Garcia-Conde M, Marin L, Ruiz de Maya S, Cuestas PJ. Parental Attitudes to Childhood Overweight: The Multiple Paths through Healthy Eating, Screen Use, and Sleeping Time. International Journal of Environmental Research and Public Health. 2020; 17(21):7885. https://doi.org/10.3390/ijerph17217885
Chicago/Turabian StyleGiménez Garcia-Conde, Miguel, Longinos Marin, Salvador Ruiz de Maya, and Pedro J. Cuestas. 2020. "Parental Attitudes to Childhood Overweight: The Multiple Paths through Healthy Eating, Screen Use, and Sleeping Time" International Journal of Environmental Research and Public Health 17, no. 21: 7885. https://doi.org/10.3390/ijerph17217885
APA StyleGiménez Garcia-Conde, M., Marin, L., Ruiz de Maya, S., & Cuestas, P. J. (2020). Parental Attitudes to Childhood Overweight: The Multiple Paths through Healthy Eating, Screen Use, and Sleeping Time. International Journal of Environmental Research and Public Health, 17(21), 7885. https://doi.org/10.3390/ijerph17217885






