Area-Level Associations between Built Environment Characteristics and Disability Prevalence in Australia: An Ecological Analysis
Abstract
1. Introduction
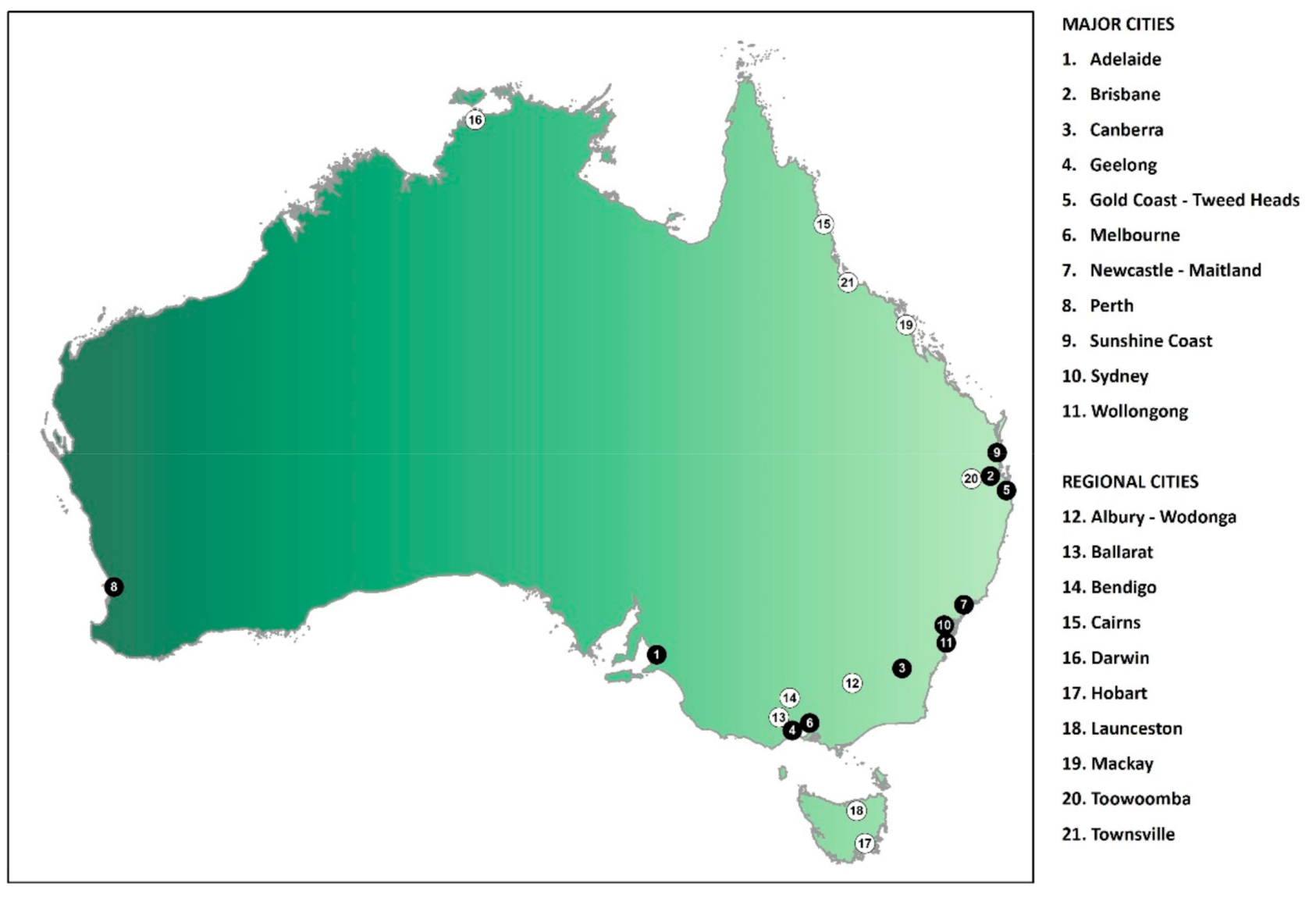
- Is area-level disability prevalence associated with area-level built environment characteristics such as walkability, healthy food environment, distance to social infrastructure services, proximity to public open space and availability of public transport?
- Do associations between area-level disability prevalence and area-level built environment characteristics differ for major cities versus regional cities?
2. Materials and Methods
2.1. Data Sources
2.2. Outcome
2.3. Exposures
2.4. Covariates
2.5. Level of Geographic Aggregation
2.6. Statistical Analysis
2.7. Ethics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Definition |
|---|---|
| Number of healthier food options (count) | Count of ‘healthier’ food options (supermarkets or fruit and vegetable grocers) within 3200 meters of dwelling via pedestrian road network |
| Healthier food proportion (%) | Healthy food choices percentage—‘healthier’ food options (supermarkets or fruit and vegetable grocers) as percentage of ‘healthier’ and fast-food options combined, within 3200 meters of a dwelling via a pedestrian road network |
| Physical activity and recreation destination | Average distance to closest physical activity and recreation destination (meters) |
| Distance to library | Average distance to closest library (meters) |
| Distance to CentreLink | Average distance to closest CentreLink office (meters). CentreLink is Australia’s national social security provider. |
| Distance to Disability Employment Service | Average distance to closest Disability Employment Service provider (meters). Disability Employment Services (DES) are an Australian government program that provides assistance with preparing for, finding and keeping employment for people with disability, injuries or health conditions. |
| Distance to general practitioner | Average distance to closest general practitioner (meters) |
| Distance to pharmacy | Average distance to closest pharmacy (meters) |
| Distance to generalist counselling | Average distance to closest generalist counselling service (meters) |
| Distance to dentist | Average distance to closest dentist (meters) |
| Distance to adult mental health | Average distance to closest adult mental health services (meters) |
| Distance to family counselling | Average distance to closest family counselling and/or family therapy service (meters) |
| Distance to psychology | Average distance to closest psychology service (meters) |
| Distance to hospital | Average distance to closest hospital (meters) |
| Distance to activity center | Average distance to closest activity center (meters) |
| Walkability | Average walkability index for local 1600 meters walkable neighborhoods, relative to study region. The index is calculated as the sum of standardized scores of street connectivity, dwelling density and a daily living score reflecting access to three kinds of basic amenities (a public transport stop, a supermarket and a convenience location). A higher walkability index means better walkability. |
| Public open space proximity | Percentage of dwellings within 400 meters of public open space |
| Public transport availability | Percentage of dwellings within 400 meters of public transport stop with a frequent weekday service (at least once every 30 min, 7am–7pm) |
References
- World Health Organization. Shanghai Declaration on Promoting Health in the 2030 Agenda for Sustainable Development. Available online: https://www.who.int/healthpromotion/conferences/9gchp/shanghai-declaration/en/ (accessed on 3 August 2020).
- World Health Organization. Shanghai Consensus on Healthy Cities 2016. Mayors forum. In Proceedings of the 9th Global Conference on Health Promotion, Shanghai, China, 21–24 November 2016; Available online: https://www.who.int/healthpromotion/conferences/9gchp/healthy-city-pledge/en/ (accessed on 3 August 2020).
- Arundel, J.; Lowe, M.; Hooper, P.; Roberts, R.; Rozek, J.; Higgs, C.; Giles-Corti, B. Creating Liveable Cities in Australia: Mapping Urban Policy Implementation and Evidence-Based National Liveability Indicators; Centre for Urban Research, RMIT University: Melbourne, VIC, Australia, 2017. [Google Scholar]
- Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Davern, M.; Gunn, L.; Whitzman, C.; Higgs, C.; Giles-Corti, B.; Simons, K.; Villanueva, K.; Mavoa, S.; Roberts, R.; Badland, H. Using spatial measures to test a conceptual model of social infrastructure that supports health and wellbeing. Cities Health 2018, 1, 194–209. [Google Scholar] [CrossRef]
- Pearce, J.R.; Richardson, E.A.; Mitchell, R.J.; Shortt, N.K. Environmental justice and health: A study of multiple environmental deprivation and geographical inequalities in health in New Zealand. Soc. Sci. Med. 2011, 73, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.R.; Richardson, E.A.; Mitchell, R.J.; Shortt, N.K. Environmental justice and health: The implications of the socio-spatial distribution of multiple environmental deprivation for health inequalities in the United Kingdom. Trans. Inst. Br. Geogr. 2010, 35, 522–539. [Google Scholar] [CrossRef]
- Badland, H.; Whitzman, C.; Lowe, M.; Davern, M.; Aye, L.; Butterworth, I.; Hes, D.; Giles-Corti, B. Urban liveability: Emerging lessons from Australia for exploring the potential for indicators to measure the social determinants of health. Soc. Sci. Med. 2014, 111, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Foster, S.; Lowe, M.; Sallis, J.F.; Stevenson, M.; et al. City planning and population health: A global challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef]
- Garin, N.; Olaya, B.; Miret, M.; Ayuso-Mateos, J.L.; Power, M.; Bucciarelli, P.; Haro, J.M. Built environment and elderly population health: A comprehensive literature review. Clin. Pr. Epidemiol. Ment. Health 2014, 10, 103–115. [Google Scholar] [CrossRef]
- Sallis, J.F.; Bowles, H.R.; Bauman, A.; Ainsworth, B.E.; Bull, F.C.; Craig, C.L.; Sjostrom, M.; De Bourdeaudhuij, I.; Lefevre, J.; Mastudo, V.; et al. Neighborhood environments and physical activity among adults in 11 countries. Am. J. Prev. Med. 2009, 36, 484–490. [Google Scholar] [CrossRef]
- Faerstein, E.; da Silveira, I.H.; Boclin, K.D.S.; Curioni, C.C.; de Castro, I.R.R.; Junger, W.L. Associations of neighborhood socioeconomic, natural and built environmental characteristics with a 13-year trajectory of non-work physical activity among civil servants in Rio de Janeiro, Brazil: The Pro-Saude Study. Health Place 2018, 53, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V.; Roux, A.V.D.; Nettleton, J.A.; Jacobs, D.R. Associations of the local food environment with diet quality—A comparison of assessments based on surveys and geographic information systems. Am. J. Epidemiol. 2008, 167, 917–924. [Google Scholar] [CrossRef]
- Bernsdorf, K.A.; Lau, C.J.; Andreasen, A.H.; Toft, U.; Lykke, M.; Glumer, C. Accessibility of fast food outlets is associated with fast food intake. A study in the Capital Region of Denmark. Health Place 2017, 48, 102–110. [Google Scholar] [CrossRef]
- Emerson, E.; Honey, H.; Llewellyn, G. Left Behind: 2013. Monitoring the Social Inclusion of Young Australians With Self-Reported Long Term Health Conditions, Impairments or Disabilities 2001–2011; Technical Report 1, February 2013; Centre for Disability Research and Policy, University of Sydney: Sydney, Australia, 2013. [Google Scholar]
- Banks, L.M.; Kuper, H.; Polack, S. Poverty and disability in low- and middle-income countries: A systematic review. PLoS ONE 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Brucker, D.L.; Mitra, S.; Chaitoo, N.; Mauro, J. More likely to be poor whatever the measure: Working-age persons with disabilities in the united states. Soc. Sci. Q. 2015, 96, 273–296. [Google Scholar] [CrossRef]
- Kavanagh, A.M.; Krnjacki, L.; Aitken, Z.; LaMontagne, A.D.; Beer, A.; Baker, E.; Bentley, R. Intersections between disability, type of impairment, gender and socio-economic disadvantage in a nationally representative sample of 33,101 working-aged Australians. Disabil. Health J. 2015, 8, 191–199. [Google Scholar] [CrossRef]
- Kavanagh, A.M.; Krnjacki, L.; Beer, A.; Lamontagne, A.D.; Bentley, R. Time trends in socio-economic inequalities for women and men with disabilities in Australia: Evidence of persisting inequalities. Int. J. Equity Health 2013, 12. [Google Scholar] [CrossRef]
- Krnjacki, L.; Emerson, E.; Llewellyn, G.; Kavanagh, A.M. Prevalence and risk of violence against people with and without disabilities: Findings from an Australian population-based study. Aust. N. Z. J. Public Health 2016, 40, 16–21. [Google Scholar] [CrossRef]
- Hughes, K.; Bellis, M.A.; Jones, L.; Wood, S.; Bates, G.; Eckley, L.; McCoy, E.; Mikton, C.; Shakespeare, T.; Officer, A. Prevalence and risk of violence against adults with disabilities: A systematic review and meta-analysis of observational studies. Lancet 2012, 379, 1621–1629. [Google Scholar] [CrossRef]
- Milner, A.; LaMontagne, A.; Aitken, Z.; Bentley, R.; Kavanagh, A. Employment status and mental health among persons with and without a disability: Evidence from an Australian cohort study. J. Epidemiol. Community Health 2014, 68, 1064–1071. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, A.M.; Aitken, Z.; Emerson, E.; Sahabandu, S.; Milner, A.; Bentley, R.; LaMontagne, A.D.; Pirkis, J.; Studdert, D. Inequalities in socio-economic characteristics and health and wellbeing of men with and without disabilities: A cross-sectional analysis of the baseline wave of the Australian Longitudinal Study on Male Health. BMC Public Health 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.L.; Ahmed, Z.; Kerr, M.P. Health care provision for people with a learning disability—Record-linkage study of epidemiology and factors contributing to hospital care uptake. Br. J. Psychiatry 2000, 176, 37–41. [Google Scholar] [CrossRef]
- Emerson, E. Deprivation, ethnicity and the prevalence of intellectual and developmental disabilities. J. Epidemiol. Community Health 2012, 66, 218–224. [Google Scholar] [CrossRef]
- Liu, N.; Kruger, E.; Tennant, M. Prevalence of disability among the major cities in Australia 2012 with geographical representation of distribution in Western Australia. Health Promot. J. Austral. 2020, 31, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. The Geography of Disability and Economic Disadvantage in Australian Capital Cities; Cat. no. DIS 54; Australian Institute of Health and Welfare: Canberra, Australia, 2009. [Google Scholar]
- Lowe, M.; Whitzman, C.; Badland, H.; Davern, M.; Aye, L.; Hes, D.; Butterworth, I.; Giles-Corti, B. Planning Healthy, Liveable and Sustainable Cities: How Can Indicators Inform Policy? Urban. Policy Res. 2015, 33, 131–144. [Google Scholar] [CrossRef]
- Higgs, C.; Badland, H.; Simons, K.; Knibbs, L.D.; Giles-Corti, B. The Urban Liveability Index: Developing a policy-relevant urban liveability composite measure and evaluating associations with transport mode choice. Int. J. Health Geogr. 2019, 18. [Google Scholar] [CrossRef] [PubMed]
- Badland, H.; Pearce, J. Liveable for whom? Prospects of urban liveability to address health inequities. Soc. Sci. Med. 2019, 232, 94–105. [Google Scholar] [CrossRef]
- United Nations. Convention on the Rights of Persons with Disabilities. Available online: www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities.html (accessed on 3 August 2020).
- World Health Organization. International Classification of Functioning, Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Commonwealth of Australia. 2010–2020 National Disability Strategy. An Initiative of the Council of Australian Governments; Commonwealth of Australia: Canberra, Australia, 2011. [Google Scholar]
- World Health Organization; World Bank. World Report on Disability; World Health Organization World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Rosenberg, D.E.; Huang, D.L.; Simonovich, S.D.; Belza, B. Outdoor built environment barriers and facilitators to activity among midlife and older adults with mobility disabilities. Gerontologist 2013, 53, 268–279. [Google Scholar] [CrossRef]
- Clarke, P.; Ailshire, J.A.; Bader, M.; Morenoff, J.D.; House, J.S. Mobility disability and the urban built environment. Am. J. Epidemiol. 2008, 168, 506–513. [Google Scholar] [CrossRef]
- Huang, D.; Rosenberg, D.; Simonovich, S.; Belza, B. Food Access Patterns and Barriers among Midlife and Older Adults with Mobility Disabilities. J. Aging Res. 2012, 2012, 1–8. [Google Scholar] [CrossRef]
- Clarke, P.J.; Ailshire, J.A.; Nieuwenhuijsen, E.R.; de Kleijn-de Vrankrijker, M.W. Participation among adults with disability: The role of the urban environment. Soc. Sci. Med. 2011, 72, 1674–1684. [Google Scholar] [CrossRef]
- Levasseur, M.; Genereux, M.; Bruneau, J.F.; Vanasse, A.; Chabot, E.; Beaulac, C.; Bedard, M.M. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: Results from a scoping study. BMC Public Health 2015, 15. [Google Scholar] [CrossRef]
- Schur, L.; Ameri, M.; Adya, M. Disability, voter turnout, and polling place accessibility. Soc. Sci. Q. 2017, 98, 1374–1390. [Google Scholar] [CrossRef]
- McDonald, K.E.; Williamson, P.; Weiss, S.; Adya, M.; Blanck, P.; DBTAC: Southeast ADA Center PAR Research Consortium. The march goes on: Community access for people with disabilities. J. Community Psychol. 2015, 43, 348–363. [Google Scholar] [CrossRef]
- Botticello, A.L.; Rohrbach, T.; Cobbold, N. Differences in the community built environment influence poor perceived health among persons with spinal cord injury. Arch. Phys. Med. Rehabil. 2015, 96, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Bigonnesse, C.; Mahmood, A.; Chaudhury, H.; Mortenson, W.B.; Miller, W.C.; Ginis, K.A.M. The role of neighborhood physical environment on mobility and social participation among people using mobility assistive technology. Disabil. Soc. 2018, 33, 866–893. [Google Scholar] [CrossRef]
- Botticello, A.L.; Rohrbach, T.; Cobbold, N. Disability and the built environment: An investigation of community and neighborhood land uses and participation for physically impaired adults. Ann. Epidemiol. 2014, 24, 545–550. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Australia’s Health 2018; Australian Institute of Health and Welfare: Canberra, Australia, 2018. [Google Scholar]
- Australian Institute of Health and Welfare. Access to Health Services by Australians with Disability; Cat. no. DIS 70; Australian Institute of Health and Welfare: Canberra, Australia, 2017. [Google Scholar]
- Productivity Commission. Report on Government Services 2018. Available online: https://www.pc.gov.au/research/ongoing/report-on-government-services/2018 (accessed on 3 August 2020).
- National Disability Insurance Scheme. COAG Disability Reform Council Quarterly Report; National Disability Insurance Scheme: Canberra, Australia, 31 March 2019. [Google Scholar]
- Morgenstern, H. Ecologic studies. In Modern Epidemiology; Rothman, K.J., Greenland, S., Lash, T.L., Eds.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2008; pp. 511–531. [Google Scholar]
- Macintyre, S.; Ellaway, A. Ecological approaches: Rediscovering the role of the physical and social environment. In Social Epidemiology; Berkman, L.F., Kawachi, I., Eds.; Oxford University Press: Oxford, UK, 2000; pp. 332–348. [Google Scholar]
- Schwartz, S. The fallacy of the ecological fallacy: The potential misuse of a concept and the consequences. Am. J. Public Health 1994, 84, 819–824. [Google Scholar] [CrossRef]
- Lakhani, A.; Parekh, S.; Gudes, O.; Grimbeek, P.; Harre, P.; Stocker, J.; Kendall, E. Disability support services in Queensland, Australia: Identifying service gaps through spatial analysis. Appl. Geogr. 2019, 110, 102045. [Google Scholar] [CrossRef]
- Gao, F.; Foster, M.; Liu, Y. Disability concentration and access to rehabilitation services: A pilot spatial assessment applying geographic information system analysis. Disabil. Rehabil. 2019, 41, 2468–2476. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 4431.0.55.002—ABS Sources of Disability Information, 2012—2016; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Australian Bureau of Statistics. 2079.0—Census of Population and Housing: Community Profile, DataPack and TableBuilder Templates, Australia, 2016; Australian Bureau of Statistics: Canberra, Australia, 2019.
- Australian Bureau of Statistics. 2016 Census—Counting persons, Place of Usual Residence (MB) [TableBuilder Pro]. Available online: https://www.abs.gov.au/websitedbs/censushome.nsf/home/tablebuilder (accessed on 29 July 2020).
- Australian Bureau of Statistics. 4430.0—Disability, Ageing and Carers, Australia: Summary of Findings, 2018; Australian Bureau of Statistics: Canberra, Australia, 2019.
- Australian Urban Observatory. Metadata. Available online: https://auo.org.au/portal/metadata/ (accessed on 3 August 2020).
- Australian Bureau of Statistics. 1270.0.55.005—Australian Statistical Geography Standard (ASGS): Volume 5—Remoteness Structure, July 2016; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Australian Bureau of Statistics. 1270.0.55.001—Australian Statistical Geography Standard (ASGS): Volume 1—Main Structure and Greater Capital City Statistical Areas, July 2016; Australian Bureau of Statistics: Canberra, Australia, 2016.
- Metzel, D.S.; Giordano, A. Locations of employment services and people with disabilities. J. Disabil. Policy Stud. 2007, 18, 88–97. [Google Scholar] [CrossRef]
- Loh, V.H.Y.; Rachele, J.N.; Brown, W.J.; Ghani, F.; Washington, S.; Turrell, G. The potential for walkability to narrow neighbourhood socioeconomic inequalities in physical function: A case study of middle-aged to older adults in Brisbane, Australia. Health Place 2019, 56, 99–105. [Google Scholar] [CrossRef]
- Baker, E.; Lester, L.; Beer, A.; Bentley, R. An Australian geography of unhealthy housing. Geogr. Res. 2019, 57, 40–51. [Google Scholar] [CrossRef]
- Baker, E.; Bentley, R.; Lester, L.; Beer, A. Housing affordability and residential mobility as drivers of locational inequality. Appl. Geogr. 2016, 72, 65–75. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Richardson, E.A.; Shortt, N.K.; Pearce, J.R. Neighborhood environments and socioeconomic inequalities in mental well-being. Am. J. Prev. Med. 2015, 49, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Baum, F.; Palmer, C. ‘Opportunity structures’: Urban landscape, social capital and health promotion in Australia. Health Promot. Int. 2002, 17, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Carey, G.; Crammond, B.; De Leeuw, E. Towards health equity: A framework for the application of proportionate universalism. Int. J. Equity Health 2015, 14. [Google Scholar] [CrossRef] [PubMed]
- Benach, J.; Malmusi, D.; Yasui, Y.; Miguel Martinez, J. A new typology of policies to tackle health inequalities and scenarios of impact based on Rose’s population approach. J. Epidemiol. Community Health 2013, 67, 286–291. [Google Scholar] [CrossRef]
- Jackson, M.A. Models of disability and human rights: Informing the improvement of built environment accessibility for people with disability at neighborhood scale? Laws 2018, 7, 10. [Google Scholar] [CrossRef]
- Imrie, R. Responding to the design needs of disabled people. J. Urban. Des. 2000, 5, 199–219. [Google Scholar] [CrossRef]
- Lau, W.K.; Ho, D.C.W.; Yau, Y. Assessing the disability inclusiveness of university buildings in Hong Kong. Int. J. Strat. Prop. Manag. 2016, 20, 184–197. [Google Scholar] [CrossRef]
- Macintyre, S. Deprivation amplification revisited; or, is it always true that poorer places have poorer access to resources for healthy diets and physical activity? Int. J. Behav. Nutr. Phys. Act. 2007, 4. [Google Scholar] [CrossRef]
- Zhou, Q.; Llewellyn, G.; Emerson, E.; Stancliffe, R.; Badland, H. Spatial Distribution of Working Age Adults with Disabilities Across Australia: A Small Area Analysis of the 2016 Census; Centre of Research Excellence in Disability and Health: Melbourne, Australia, 2017. [Google Scholar]
- Australian Institute of Health and Welfare. People with disability in Australia 2020; Australian Institute of Health and Welfare AIHW: Canberra, ACT, Australia, 2020. [Google Scholar]
- Fortune, N.; Badland, H.; Clifton, S.; Emerson, E.; Rachele, J.; Stancliffe, R.J.; Zhou, Q.; Llewellyn, G. The Disability and Wellbeing Monitoring Framework: Data, data gaps, and policy implications. Aust. New Zealand J. Public Health 2020, 44, 227–232. [Google Scholar] [CrossRef]
| Variables | Range | Median | Mean | Standard Deviation |
|---|---|---|---|---|
| Outcome variable1 | ||||
| Disability prevalence (15–64 years)—all SA2s (Statistical Area Level 2s) (%) | 0–11.9 | 2.7 | 3.0 | 1.5 |
| Major city SA2s (%) | 11.9 | 2.6 | 2.9 | 1.5 |
| Regional city SA2s (%) | 9.8 | 3.2 | 3.5 | 1.6 |
| Exposure variables2 | ||||
| Number of healthier food options (count) | 0–60 | 5 | 7 | 7 |
| Healthier food proportion (%) | 0–100 | 41 | 43 | 15 |
| Physical activity and recreation (meters) | 265–78,546 | 4934 | 2828 | 6442 |
| Library (meters) | 576–22,912 | 2490 | 3200 | 2503 |
| Centrelink (meters) | 556–49,384 | 4361 | 5364 | 4127 |
| Disability employment service (meters) | 399–26,996 | 2817 | 3677 | 2993 |
| General practitioner (meters) | 202–9165 | 1026 | 1241 | 880 |
| Pharmacy (meters) | 240–9863 | 1122 | 1373 | 979 |
| Generalist counselling (meters) | 289–61,553 | 2249 | 3339 | 3916 |
| Dentist (meters) | 241–22,975 | 1240 | 1753 | 1861 |
| Adult mental health (meters) | 600–78,935 | 6419 | 8891 | 8602 |
| Family counselling (meters) | 475–79,383 | 4374 | 6874 | 8162 |
| Psychology (meters) | 242–55,769 | 1530 | 2318 | 3145 |
| Hospital (meters) | 294–39,903 | 3627 | 5100 | 4730 |
| Activity center (meters) | 236–61,127 | 1770 | 2522 | 3029 |
| Walkability (index) | −7.2–11 | 0.2 | 0.3 | 2.1 |
| Public open space (% dwellings) | 0–100 | 78 | 74 | 19 |
| Public transport availability (% dwellings) | 0–100 | 52 | 52 | 20 |
| Variable 1 | Beta Coefficients | CI low | CI high |
|---|---|---|---|
| Physical activity and recreation | 0.29 | 0.22 | 0.37 |
| Family counselling | 0.28 | 0.20 | 0.35 |
| Psychology | 0.27 | 0.20 | 0.35 |
| Adult mental health | 0.24 | 0.17 | 0.32 |
| Dentist | 0.23 | 0.15 | 0.30 |
| Generalist counselling | 0.20 | 0.13 | 0.28 |
| Activity center | 0.18 | 0.10 | 0.25 |
| Hospital | 0.10 | 0.03 | 0.18 |
| General practitioner | 0.10 | 0.02 | 0.17 |
| Pharmacy | 0.10 | 0.02 | 0.17 |
| Library | 0.06 | −0.02 | 0.14 |
| Healthier food proportion | −0.03 | −0.10 | 0.05 |
| Centrelink | −0.04 | −0.12 | 0.03 |
| Disability Employment Service | −0.09 | −0.16 | −0.01 |
| Public open space proximity | −0.22 | −0.29 | −0.14 |
| Walkability | −0.31 | −0.39 | −0.24 |
| Number of healthier food options | −0.35 | −0.42 | −0.27 |
| Public transport availability | −0.36 | −0.43 | −0.29 |
| Variable 1 | Major Cities Beta Coef. (95% CI) | Regional Cities Beta Coef. (95% CI) | ||
|---|---|---|---|---|
| Physical activity and recreation | 0.33 | (0.26, 0.41) | −0.20 | (−0.48, 0.07) |
| Adult mental health | 0.27 | (0.20, 0.35) | −0.09 | (−0.43, 0.25) |
| Dentist | 0.29 | (0.20, 0.37) | −0.07 | (−0.24, 0.09) |
| Hospital | 0.15 | (0.06, 0.23) | −0.18 | (−0.36, 0.00) |
| General practitioner | 0.14 | (0.05, 0.23) | −0.10 | (−0.24, 0.05) |
| Pharmacy | 0.12 | (0.03, 0.20) | −0.08 | (−0.24, 0.08) |
| Walkability | −0.35 | (−0.43, −0.28) | 0.14 | (−0.16, 0.44) |
| Number of healthier food options | −0.35 | (−0.42, −0.27) | 0.50 | (−0.03, 1.04) |
| Public transport availability | −0.36 | (−0.44, −0.29) | 0.38 | (−0.06, 0.82) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fortune, N.; Singh, A.; Badland, H.; Stancliffe, R.J.; Llewellyn, G. Area-Level Associations between Built Environment Characteristics and Disability Prevalence in Australia: An Ecological Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7844. https://doi.org/10.3390/ijerph17217844
Fortune N, Singh A, Badland H, Stancliffe RJ, Llewellyn G. Area-Level Associations between Built Environment Characteristics and Disability Prevalence in Australia: An Ecological Analysis. International Journal of Environmental Research and Public Health. 2020; 17(21):7844. https://doi.org/10.3390/ijerph17217844
Chicago/Turabian StyleFortune, Nicola, Ankur Singh, Hannah Badland, Roger J. Stancliffe, and Gwynnyth Llewellyn. 2020. "Area-Level Associations between Built Environment Characteristics and Disability Prevalence in Australia: An Ecological Analysis" International Journal of Environmental Research and Public Health 17, no. 21: 7844. https://doi.org/10.3390/ijerph17217844
APA StyleFortune, N., Singh, A., Badland, H., Stancliffe, R. J., & Llewellyn, G. (2020). Area-Level Associations between Built Environment Characteristics and Disability Prevalence in Australia: An Ecological Analysis. International Journal of Environmental Research and Public Health, 17(21), 7844. https://doi.org/10.3390/ijerph17217844






