The Relationship of Urbanization and Performance of Activity and Participation Functioning among Adults with Developmental Disabilities in Taiwan
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.2.1. Functioning Score of WHODAS 2.0-36-Item
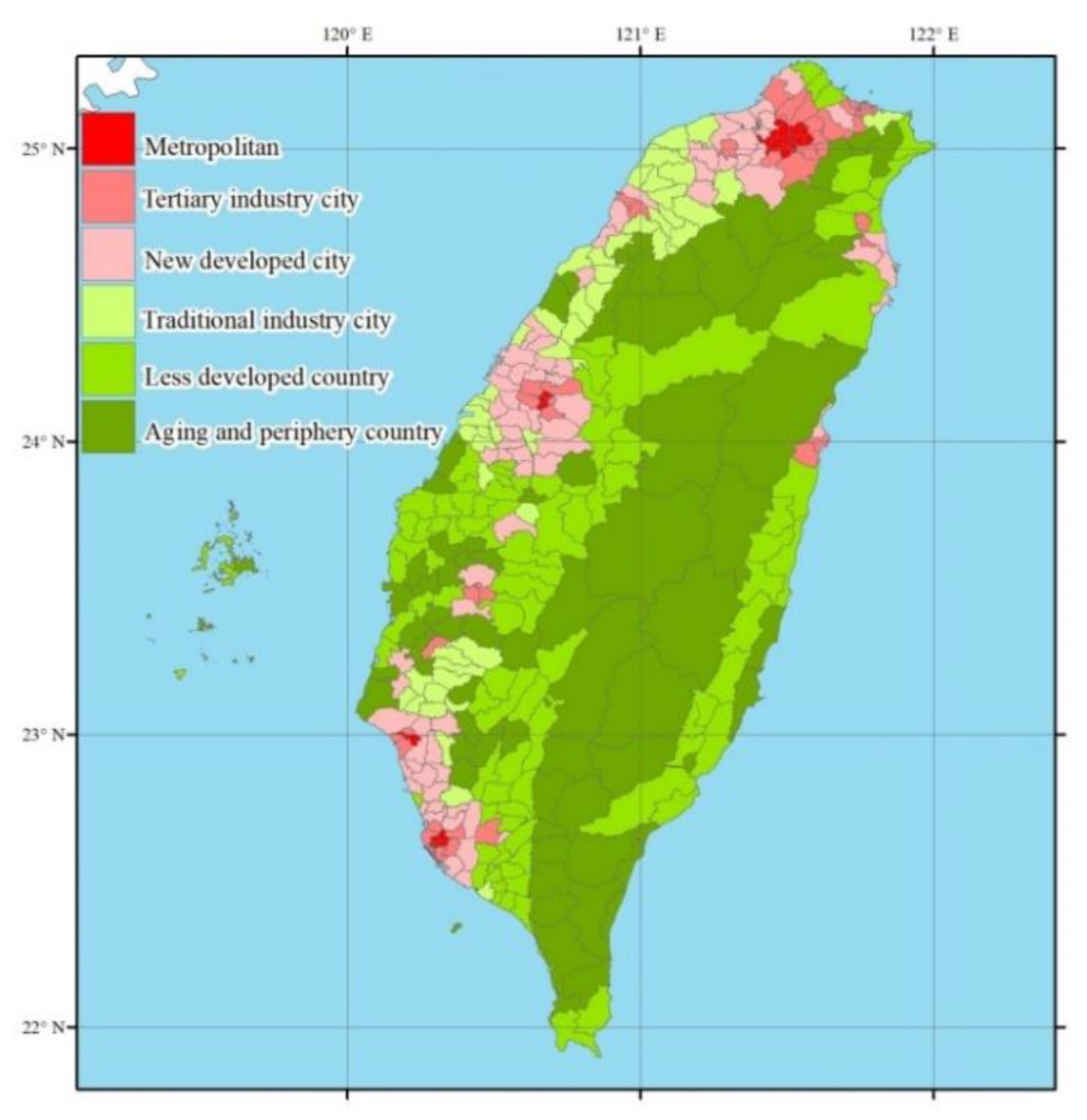
2.2.2. The Definition of the Urbanization
2.3. Data Analysis
3. Results
3.1. The Characters of Our Participators
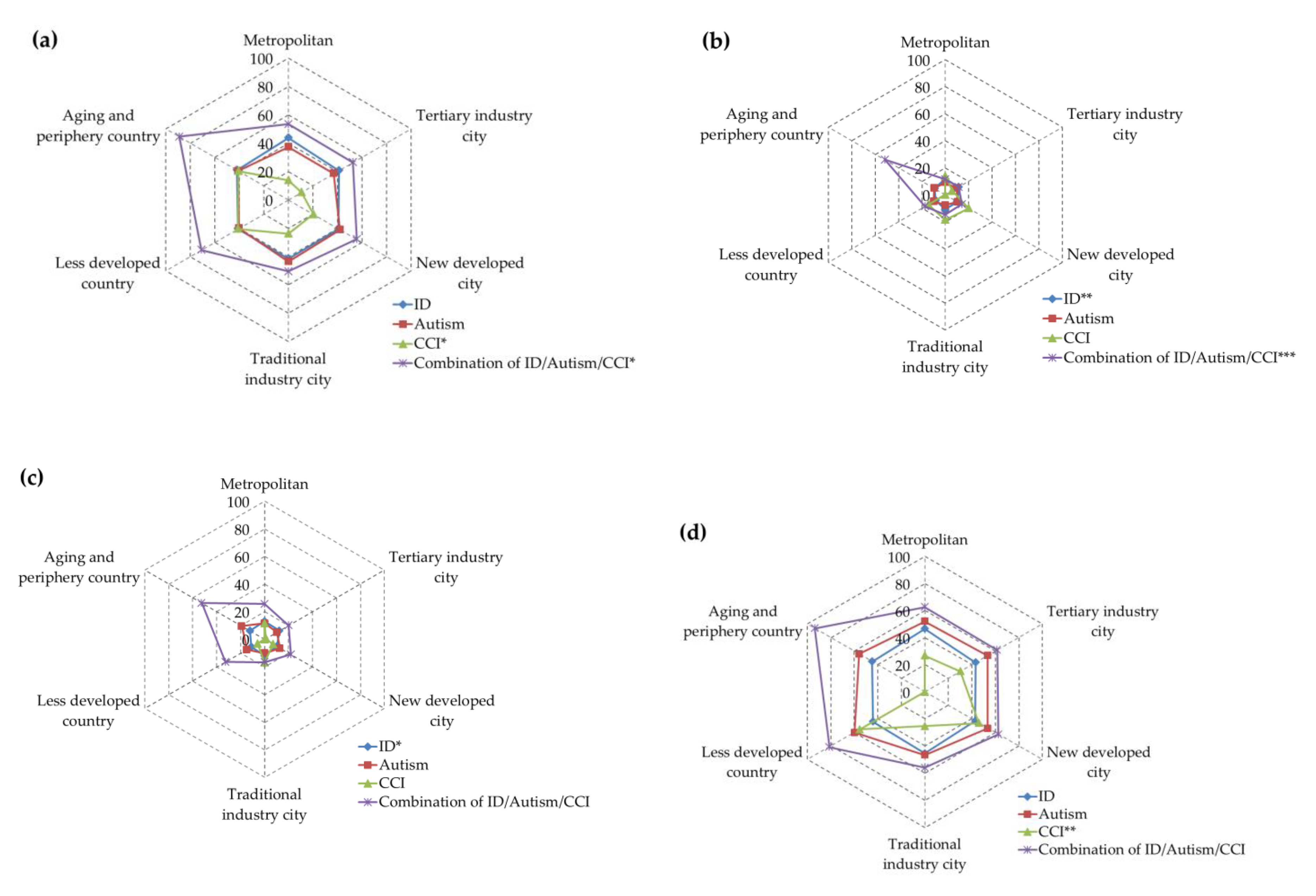
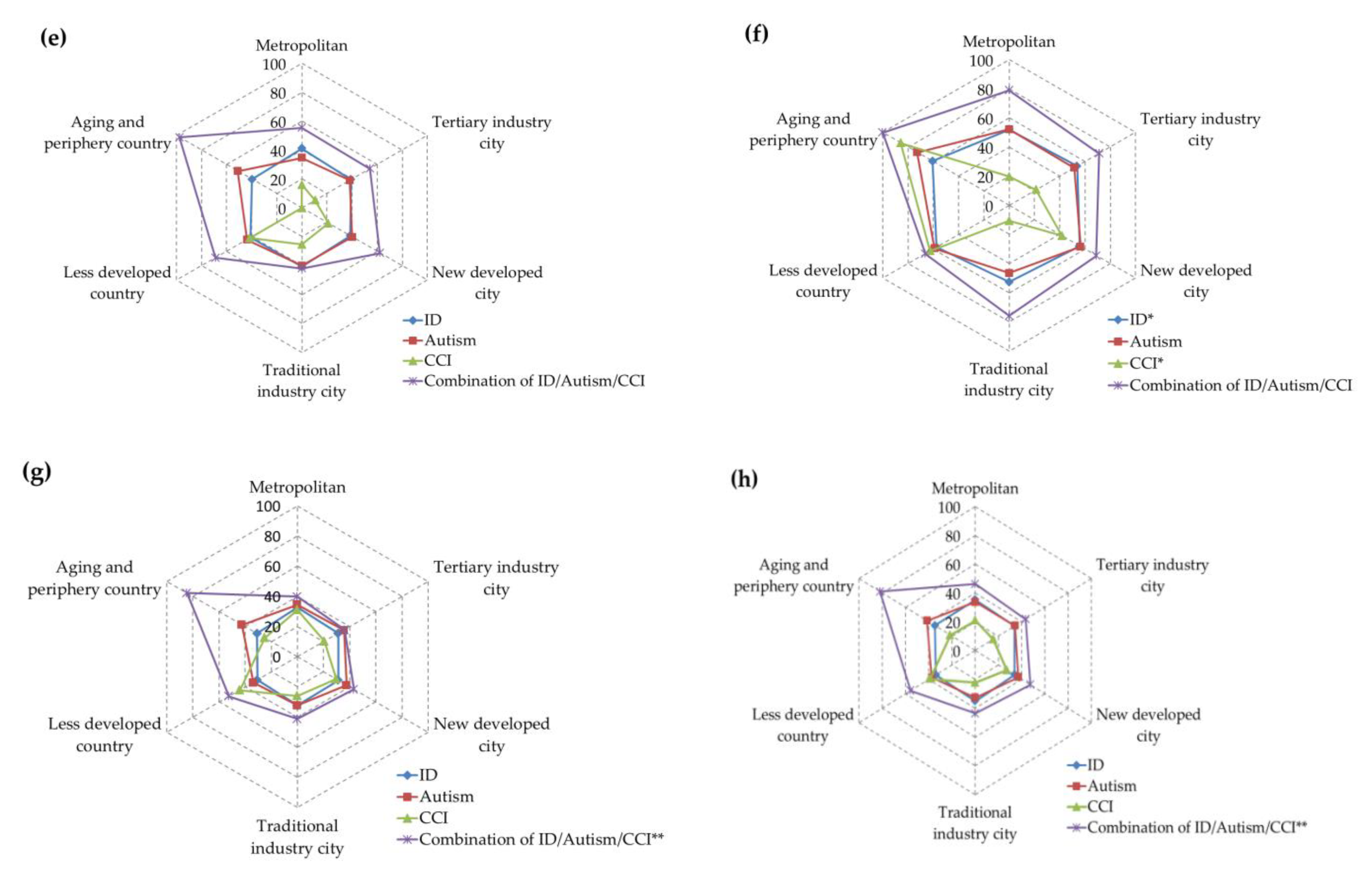
3.2. The Relationship between Urbanization, Impairments, and Performance of Functioning
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ID | Intellectual Disability |
| CCI | Concomitant Communicative Impairment |
| DEDS | Disability Eligibility Determination System |
| FUNDES- Adult | Functioning Scale of the Disability Evaluation System- Adult version |
| ICF | International Classification of Health, Functioning, and Disability |
| WHODAS 2.0 | World Health Organization Disability Assessment Schedule 2.0 |
| ASD | Autism Spectrum Disorders |
References
- Van Naarden Braun, K.; Yeargin-Allsopp, M.; Lollar, D. Activity limitations among young adults with developmental disabilities: A population-based follow-up study. Res. Dev. Disabil. 2009, 30, 179–191. [Google Scholar] [CrossRef]
- Okoro, C.A.; Hollis, N.D.; Cyrus, A.C.; Griffin-Blake, S. Prevalence of Disabilities and Health Care Access by Disability Status and Type Among Adults-United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 882–887. [Google Scholar] [CrossRef]
- Sage, R.; Ward, B.; Myers, A.; Ravesloot, C. Transitory and Enduring Disability among Urban and Rural People. J. Rural Health 2019, 35, 460–470. [Google Scholar] [CrossRef]
- Zhao, G.; Okoro, C.A.; Hsia, J.; Garvin, S.W.; Town, M. Prevalence of Disability and Disability Types by Urban–Rural County Classification-US, 2016. Am. J. Prev. Med. 2019, 57, 749–756. [Google Scholar] [CrossRef]
- von Reichert, C.; Cromartie, J.B.; Arthun, R.O. Impacts of Return Migration on Rural US Communities. Rural Sociol. 2014, 79, 200–226. [Google Scholar] [CrossRef]
- Von Reichert, C.; Greiman, L.; Myers, A.; Rural Institute, University of Montana. The Geography of Disability in America: On Rural-Urban Differences in Impairment Rates. In Independent Living and Community Participation; University of Montana Rural Institute: Missoula, MT, USA, 2014; Volume 7, Available online: https://scholarworks.umt.edu/ruralinst_independent_living_community_participation/7 (accessed on 1 June 2020).
- Jones, J. The geography of mental health. Epidemiol. Psychiatr. Sci. 2001, 10, 219–224. [Google Scholar] [CrossRef][Green Version]
- Ngui, E.M.; Khasakhala, L.; Ndetei, D.; Roberts, L.W. Mental disorders, health inequalities and ethics: A global perspective. Int. Rev. Psychiatry 2010, 22, 235–244. [Google Scholar] [CrossRef]
- Chow, W.S.; Priebe, S. Understanding psychiatric institutionalization: A conceptual review. BMC Psychiatry 2013, 13, 169. Available online: http://www.biomedcentral.com/1471-244X/13/169 (accessed on 20 March 2020). [CrossRef]
- Cummings, J.R.; Allen, L.; Clennon, J.; Ji, X.; Druss, B.G. Geographic access to specialty mental health care across high- and low-income U.S. communities. JAMA Psychiatry 2017, 74, 476–484. [Google Scholar] [CrossRef]
- Jacob, K.S. Community care for people with mental disorders in developing countries: Problems and possible solutions. Br. J. Psychiatry 2001, 178, 296–298. [Google Scholar] [CrossRef]
- Patel, V. Health systems research: A pragmatic model for meeting mental health needs in low-income countries. In Unmet Need in Psychiatry; Andrews, G., Henderson, S., Eds.; Cambridge University Press: Cambridge, UK, 2000; pp. 363–377. [Google Scholar] [CrossRef]
- Haas, K.; Wilson, N.J.; Cordier, R.; Vaz, S.; Chung-yeung Lee, H. The Experiences of Young Autistic Adults in Using Metropolitan Public Transport; Cooperative Research Centre for Living with Autism: Brisbane, Australia, 2020; Available online: https://www.autismcrc.com.au/sites/default/files/reports/3-041_Young-autistic-adults-on-public-transport_Report_2020.pdf (accessed on 1 June 2020).
- Chiu, T.-Y.; Yen, C.-F.; Chou, C.-H.; Lin, J.-D.; Hwang, A.-W.; Liao, H.-F.; Chi, W.-C. Development of traditional Chinese version of World Health Organization Disability Assessment Schedule 2.0 36–item (WHODAS 2.0) in Taiwan: Validity and reliability analyses. Res. Dev. Disabil. 2014, 35, 2812–2820. [Google Scholar] [CrossRef] [PubMed]
- Yen, C.-F.; Hwang, A.-W.; Liou, T.-H.; Chiu, T.-Y.; Hsu, H.-Y.; Chi, W.-C.; Wu, T.-F.; Chang, B.-S.; Lu, S.-J.; Liao, H.-F.; et al. Validity and reliability of the Functioning Disability Evaluation Scale-Adult Version based on the WHODAS 2.0–36 items. J. Formos. Med. Assoc. 2014, 113, 839–849. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Organization Disability Assessment Schedule, 2nd Version (WHODAS 2.0); World Health Organization: Geneva, Switzerland, 2010; Available online: https://www.who.int/classifications/icf/whodasii/en/ (accessed on 1 June 2020).
- Chia-Feng, Y.; Shyang-Woei, L. Justice in Dementia Care Resource Allocation: How Should We Plan for Dementia Services? Int. J. Environ. Res. Public Health 2019, 16, 1754. [Google Scholar] [CrossRef]
- Ruey, C.; Tsan-Hon, L.; Nae-Fang, M.; Kwang-Hwa, C.; Chia-Feng, Y.; Hua-Fang, L.; Wen-Chou, C.; Kuei-Ru, C. Using World Health Organization Disability Assessment Schedule 2.0 in People with Schizophrenia: A 4-Year Follow-Up. Eur. Arch. Psychiatry Clin. Neurosci. 2019, 270, 301–310. [Google Scholar]
- Tzu-Herng, H.; Tsan-Hon, L.; Kuei-Ru, C.; Wen-Chou, C.; Chia-Feng, Y.; Hua-Fang, L.; Ing-Jy, T. Large-Scale Assessment of Function and Disability in Patients with Parkinson’s Disease Using the Functioning Disability Evaluation Scale-Adult Version. Int. J. Environ. Res. Public Health 2018, 15, 2788. [Google Scholar]
- Lee, Y.-H.; Chang, K.-H.; Escorpizo, R.; Chi, W.-C.; Yen, C.-F.; Liao, H.-F.; Huang, S.-W.; Liou, T.-H. Accuracy of the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) score as an objective assessment tool for predicting return-to-work status after head and neck cancer in male survivors. Support. Care Cancer 2018, 27, 433–441. [Google Scholar] [CrossRef]
- Lu, S.-J.; Liou, T.-H.; Yen, C.-F.; Chang, F.-H.; Chen, Y.-L.; Escorpizo, R.; Strauser, D.R.; Pan, A.-W. Determinants of Employment Outcome for the People with Schizophrenia Using the WHODAS 2.0. J. Occup. Rehabil. 2019, 29, 375–383. [Google Scholar] [CrossRef]
- Chang, K.-F.; Chang, K.-H.; Chi, W.-C.; Huang, S.-W.; Yen, C.-F.; Liao, H.-F.; Liou, T.-H.; Chao, P.-Z.; Lin, I.-C. Influence of visual impairment and hearing impairment on functional dependence status among people in Taiwan—An evaluation using the WHODAS 2.0 score. J. Chin. Med Assoc. 2018, 81, 376–382. [Google Scholar] [CrossRef]
- Chen, R.; Liou, T.-H.; Chang, K.-H.; Yen, C.-F.; Liao, H.-F.; Chi, W.-C.; Chou, K.-R. Assessment of functioning and disability in patients with schizophrenia using the WHO Disability Assessment Schedule 2.0 in a large-scale database. Eur. Arch. Psychiatry Clin. Neurosci. 2018, 268, 65–75. [Google Scholar] [CrossRef]
- Tzeng, G.-H.; Wu, T.-Y. Characteristics of Urbanization Levels in Taiwan Districts. Geogr. Res. 1986, 12, 287–323. Available online: http://rportal.lib.ntnu.edu.tw:80/handle/20.500.12235/23622 (accessed on 2 June 2020).
- Hsu, S.-M.; Hung, Y.-T. Stratification, Sampling Error, and the Design Effect of the 2001 TEDS Sampling Design. J. Elect. Stud. 2003, 10, 59–91. [Google Scholar] [CrossRef]
- Li, L.-A. A Study on the Order of the Degree of Urbanization among the Lo Chi-Hon Strata of Taiwan Counties. Surv. Res. Method Appl. 2004, 15, 5–30. [Google Scholar] [CrossRef]
- Liu, C.-Y.; Hung, Y.-T.; Chuang, Y.-L.; Chen, Y.-J.; Weng, W.-S.; Liu, J.-S.; Liang, K.-Y. Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large Scale Health Interview Survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar] [CrossRef]
- Hou, P.-C.; Tu, S.-H.; Liao, P.-S.; Hung, Y.-T.; Chang, Y.-H. The Typology of Townships in Taiwan: The Analysis of Sampling Stratification of the 2005–2006 “Taiwan Social Change Survey”. Surv. Res. Method Appl. 2008, 23, 7–32. [Google Scholar] [CrossRef]
- Lauritsen, M.B.; Astrup, A.; Pedersen, C.B.; Obel, C.; Schendel, D.E.; Schieve, L.; Yeargin-Allsopp, M.; Parner, E.T. Urbanicity and autism spectrum disorders. J. Autism Dev. Disord. 2014, 44, 394–404. [Google Scholar] [CrossRef]
- Baio, J.; Wiggins, L.; Christensen, D.L.; Maenner, M.J.; Daniels, J.; Warren, Z.; Kurzius-Spencer, M.; Zahorodny, W.; Robinson Rosenberg, C.; White, T.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years-Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill. Summ. 2018, 67, 1–23. [Google Scholar] [CrossRef]
- Rzhetsky, A.; Bagley, S.C.; Wang, K.; Lyttle, C.S.; Cook, E.H., Jr.; Altman, R.B.; Gibbons, R.D. Environmental and State-Level Regulatory Factors Affect the Incidence of Autism and Intellectual Disability. PLoS Comput. Biol. 2014, 10, e1003518. [Google Scholar] [CrossRef]
- Raina, S.K.; Chander, V.; Bhardwaj, A.K.; Kumar, D.; Sharma, S.; Kashyap, V.; Singh, M.; Bhardwaj, A. Prevalence of Autism Spectrum Disorder among Rural, Urban, and Tribal Children (1–10 Years of Age). J. Neurosci. Rural Pract. 2017, 8, 368–374. [Google Scholar] [CrossRef]
- Fillary, R.; Pernice, R. Social inclusion in workplaces where people with intellectual disabilities are employed: Implications for supported employment professionals. Int. J. Rehabil. Res. 2006, 29, 31–36. [Google Scholar] [CrossRef]
- Hansen, R.H.; Hinojosa, J.; Commission on Practice. Occupational therapy’s commitment to non-discrimination and inclusion. Am. J. Occup. Ther. 2009, 63, 819–820. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Variables | Content | The Data Sources |
|---|---|---|
| 1. Demography characters | Gender, birthday, the date of test, work status, living status, address of living, etc. | Self-report |
| 2. Disease and Disability | ICD code, the type of disability, the severity of disability, etc. | To be diagnosed by the physicians |
| 3. The activity and participation functioning | (1) Cognition (6 items), by assessing communication and thinking activities such as concentrating, remembering, problem-solving, learning and communicating; (2) Mobility (5 items), by assessing activities such as standing, moving around inside the home, getting out of the home and walking a long distance; (3) Self-care (4 items), assessing activities such as hygiene, dressing, eating and staying alone; (4) Getting along (5 items), by assessing interactions with other people and any difficulty experienced due to health conditions; (5) life activities (8 items-pertaining to the household, school, or work), by assessing any difficulty experienced with day-to-day activities (activities that people perform on most days) which are associated with domestic responsibilities, leisure, work and school; and (6) Participation (8 items), | The evaluations were carried out by physicians and other professionals such as occupational therapists (OTs), physical therapists (PTs), speech therapists (STs), social workers, psychologists, and nurses. |
| Variables | ID n = 4455 | Autism n = 670 | Concomitant Communicative Impairment (CCI) n = 110 | Combination of ID/Autism/CCI n = 139 |
|---|---|---|---|---|
| Age (Mean ± SD) *** | 30.67 ± 13.27 | 23.19 ± 7.73 | 47.56 ± 16.32 | 22.66 ± 7.31 |
| Gender *** | ||||
| Male | 2459 (55.2) | 590 (88.1) | 74 (67.3) | 110 (79.1) |
| Female | 1996 (44.8) | 80 (11.9) | 36 (32.7) | 29 (20.9) |
| Work status *** | ||||
| No | 2640 (59.4) | 262 (39.5) | 49 (44.5) | 82 (59.0) |
| Yes | 965 (21.7) | 99 (14.9) | 37 (33.6) | 18 (12.9) |
| Retire/students/house wife | 836 (18.8) | 302 (45.6) | 24 (21.8) | 39 (28.1) |
| The severity of disability *** | ||||
| Mile | 1281 (40.9) | 423 (63.1) | 60 (54.5) | 17 (12.2) |
| Moderate | 1853 (41.6) | 159 (23.7) | 22 (20.0) | 55 (39.6) |
| Severe | 592 (13.3) | 66 (9.9) | 9 (8.2) | 40 (28.8) |
| Profound | 189 (4.2) | 22 (3.3) | 19 (17.3) | 27 (19.4) |
| Urban Type of Living City (Urbanization) *** | ||||
| Metropolitan | 724 (16.3) | 199 (29.7) | 32 (29.1) | 33 (23.7) |
| Tertiary industry city | 929 (20.9) | 256 (38.2) | 19 (17.3) | 39 (28.1) |
| New developed city | 1333 (29.9) | 143 (21.3) | 24 (21.8) | 33 (23.7) |
| Traditional industry city | 513 (11.5) | 24 (3.6) | 17 (15.5) | 13 (9.4) |
| Less developed country | 701 (15.7) | 34 (5.1) | 17 (15.5) | 17 (12.2) |
| Aging country | 182 (4.1) | 9 (1.3) | 0 (−) | 4 (2.9) |
| periphery country | 73 (1.6) | 5 (0.7) | 1 (0.9) | 0 (−) |
| Living status *** | ||||
| Living in community $ | 4172 (94.4) | 624 (94.3) | 107 (97.3) | 120 (86.3) |
| Living in an institution | 249 (5.6) | 38 (5.7) | 3 (2.7) | 19 (13.7) |
| Income Status of Households *** (n = 1657) | ||||
| Low income households | 176 (12.3) | 5 (3.4) | 2 (7.4) | 11 (22.9) |
| Middle-income households | 97 (6.8) | 4 (2.7) | 0 (−) | 1 (2.6) |
| General households | 116 (85.5) | 140 (94.0) | 25 (92.6) | 36 (75.0) |
| Domain | ID n = 4455 | Autism n = 670 | CCI n = 110 | Combination of ID/Autism/CCI n = 139 |
|---|---|---|---|---|
| Do1 Cognition *** | 42.02 ± 25.39 | 34.96 ± 23.87 | 30.45 ± 29.89 | 52.63 ± 29.42 |
| Do2 Mobility *** | 10.84 ± 19.60 | 6.70 ± 14.43 | 22.27 ± 28.54 | 11.06 ± 18.57 |
| Do3 Self-care *** | 11.85 ± 19.23 | 9.69 ± 17.06 | 13.73 ± 25.80 | 21.94 ± 26.26 |
| Do4 Get along *** | 44.62 ± 29.67 | 49.56 ± 28.11 | 45.53 ± 33.42 | 60.91 ± 30.53 |
| Do5-1 Life activities: Work and school task *** | 40.32 ± 31.55 | 34.10 ± 31.37 | 32.09 ± 38.72 | 54.03 ± 35.50 |
| Do5-2 Life activities: Household *** | 56.31 ± 44.41 | 48.07 ± 41.16 | 45.13 ± 46.87 | 67.37 ± 39.91 |
| Do6 Participation *** | 31.84 ± 23.32 | 32.41 ± 23.06 | 38.41 ± 27.85 | 39.06 ± 26.60 |
| Summary Scores *** | 34.76 ± 20.54 | 31.28 ± 19.08 | 34.12 ± 25.70 | 43.75 ± 22.68 |
| Variables: Age, Domain and Urbanization | ID n = 4455 | Autism n = 670 | CCI n = 110 | Combination of ID/Autism/CCI n = 139 |
|---|---|---|---|---|
| After adjust age | 29.88 | |||
| Domain 1 | ¥ F = 1.38 p = 0.228 | F = 1.345 p = 0.243 | F = 2.814 * p = 0.020 | F = 2.391 * p = 0.041 |
| Metropolitan | 43.65 ± 0.91 | 37.17 ± 1.74 | 13.68 ± 4.33 | 53.30 ± 4.25 |
| Tertiary industry city | 41.32 ± 0.80 | 37.02 ± 1.54 | 10.70 ± 5.62 | 52.76 ± 3.91 |
| New developed city | 40.93 ± 0.67 | 42.17 ± 2.05 | 20.39 ± 5.00 | 55.62 ± 4.25 |
| Traditional industry city | 41.63 ± 1.07 | 43.58 ± 4.98 | 23.98 ± 5.94 | 50.55 ± 6.77 |
| Less developed country | 40.89 ± 0.92 | 40.31 ± 4.18 | 41.16 ± 5.93 | 70.78 ± 14.08 |
| Aging and periphery country | 41.94 ± 1.53 | 40.85 ± 6.52 | 40.50 ± 24.39 | 88.94 ± 12.19 |
| Domain 2 | F = 3.028N ** p = 0.010 | F = 0.259 p = 0.935 | F = 0.843 p = 0.522 | F = 4.420 *** p < 0.001 |
| Metropolitan | 11.71 ± 0.68 | 9.01 ± 1.31 | 13.85 ± 3.27 | 11.36 ± 3.20 |
| Tertiary industry city | 11.36 ± 0.60 | 9.76 ± 1.16 | 5.80 ± 4.23 | 11.34 ± 2.95 |
| New developed city | 10.36 ± 0.50 | 10.55 ± 1.54 | 20.01 ± 3.77 | 14.21 ± 3.20 |
| Traditional industry city | 11.02 ± 0.81 | 7.76 ± 3.76 | 18.65 ± 4.48 | 14.70 ± 5.10 |
| Less developed country | 8.41 ± 0.70 | 9.90 ± 3.15 | 14.48 ± 4.47 | 17.33 ± 4.46 |
| Aging and periphery country | 9.21 ± 1.15 | 9.40 ± 4.91 | −1.32 ± 18.38 § | 51.71 ± 9.19 |
| Domain 3 | F = 2.514 * p = 0.028 | F = 1.158 p = 0.329 | F = 0.883 p = 0.495 | F = 2.089 p = 0.071 |
| Metropolitan | 13.00 ± 0.70 | 11.54 ± 1.35 | 11.55 ± 3.37 | 25.72 ± 3.30 |
| Tertiary industry city | 12.48 ± 0.62 | 10.35 ± 1.19 | 1.09 ± 4.37 | 20.15 ± 3.04 |
| New developed city | 10.42 ± 0.52 | 12.85 ± 1.59 | 7.22 ± 3.88 | 22.01 ± 3.30 |
| Traditional industry city | 11.98 ± 0.84 | 10.05 ± 3.87 | 16.68 ± 4.61 | 16.58 ± 5.26 |
| Less developed country | 10.93 ± 0.72 | 14.80 ± 3.25 | 5.95 ± 4.60 | 32.68 ± 4.60 |
| Aging and periphery country | 12.09 ± 1.19 | 19.06 ± 5.01 | −5.02 ± 18.95 § | 52.60 ± 9.47 |
| Domain 4 | F = 1.968 p = 0.08 | F = 0.735 p = 0.597 | F = 3.353 ** p = 0.008 | F = 2.28 p = 0.05 |
| Metropolitan | 46.61 ± 1.07 | 52.07 ± 2.04 | 26.91 ± 5.09 | 62.71 ± 4.99 |
| Tertiary industry city | 43.30 ± 0.94 | 53.69 ± 1.80 | 30.51 ± 6.60 | 61.75 ± 4.59 |
| New developed city | 42.88 ± 0.79 | 53.80 ± 2.40 | 46.12 ± 5.87 | 62.74 ± 4.99 |
| Traditional industry city | 45.40 ± 1.27 | 46.62 ± 5.85 | 25.27 ± 7.00 | 55.94 ± 7.95 |
| Less developed country | 44.16 ± 1.08 | 60.00 ± 4.92 | 55.37 ± 6.96 | 81.34 ± 6.95 |
| Aging and periphery country | 44.80 ± 1.79 | 55.91 ± 7.66 | −9.74 ± 28.65 § | 93.94 ± 14.32 |
| Domain 5-1 | F = 0.934 p = 0.458 | F = 1.287 p = 0.268 | F = 1.882 p = 0.104 | F = 2.079 p = 0.072 |
| Metropolitan | 41.18 ± 1.15 | 34.65 ± 2.20 | 16.13 ± 5.48 | 55.57 ± 5.37 |
| Tertiary industry city | 39.28 ± 1.01 | 38.35 ± 1.94 | 10.68 ± 7.10 | 54.32 ± 4.94 |
| New developed city | 38.70 ± 0.85 | 40.24 ± 2.59 | 21.15 ± 6.31 | 62.36 ± 5.37 |
| Traditional industry city | 40.64 ± 1.36 | 39.97 ± 6.24 | 25.28 ± 7.50 | 41.83 ± 8.55 |
| Less developed country | 40.82 ± 1.16 | 43.84 ± 5.29 | 41.58 ± 7.49 | 69.00 ± 7.42 |
| Aging and periphery country | 39.75 ± 1.93 | 51.07 ± 8.23 | −10.43 ± 30.81 § | 97.71 ± 15.40 |
| Domain 5-2 | F = 2.751 * p = 0.017 | F = 1.135 p = 0.340 | F = 3.085 * p = 0.012 | F = 0.719 p = 0.610 |
| Metropolitan | 52.07 ± 1.59 | 52.30 ± 3.04 | 19.88 ± 7.29 | 78.99 ± 7.43 |
| Tertiary industry city | 53.87 ± 1.40 | 51.68 ± 2.68 | 21.44 ± 9.83 | 71.39 ± 6.84 |
| New developed city | 55.84 ± 1.17 | 56.59 ± 3.58 | 41.71 ± 8.74 | 69.07 ± 7.43 |
| Traditional industry city | 52.53 ± 1.88 | 46.46 ± 8.71 | 10.55 ± 10.38 | 75.80 ± 11.84 |
| Less developed country | 57.41 ± 1.61 | 59.02 ± 7.32 | 62.57 ± 10.36 | 66.39 ± 10.35 |
| Aging and periphery country | 60.80 ± 2.67 | 72.77 ± 11.40 | 85.91 ± 42.65 | 100.28 ± 21.32 |
| Domain 6 | F = 0.839 p = 0.522 | F = 0.607 p = 0.694 | F = 1.412 p = 0.226 | F = 3.749 ** p = 0.003 |
| Metropolitan | 32.78 ± 0.84 | 34.59 ± 1.62 | 31.12 ± 4.03 | 39.83 ± 3.95 |
| Tertiary industry city | 31.18 ± 0.74 | 35.39 ± 1.43 | 20.54 ± 5.22 | 35.93 ± 3.64 |
| New developed city | 31.19 ± 0.62 | 37.45 ± 1.90 | 29.48 ± 4.65 | 43.02 ± 3.95 |
| Traditional industry city | 32.11 ± 1.00 | 32.25 ± 4.63 | 25.90 ± 5.52 | 41.27 ± 6.29 |
| Less developed country | 30.73 ± 0.86 | 34.02 ± 3.89 | 44.19 ± 5.51 | 52.42 ± 5.50 |
| Aging and periphery country | 30.88 ± 1.42 | 42.42 ± 6.06 | 25.23 ± 22.68 | 84.53 ± 11.34 |
| Summary Scores | F = 0.961 p = 0.441 | F = 1.018 p = 0.406 | F = 2.086 p = 0.073 | F = 3.228 ** p = 0.009 |
| Metropolitan | 35.29 ± 0.72 | 33.69 ± 1.37 | 20.91 ± 3.43 | 46.14 ± 3.36 |
| Tertiary industry city | 33.991 ± 0.63 | 34.34 ± 1.21 | 15.54 ± 4.44 | 43.39 ± 3.09 |
| New developed city | 33.77 ± 0.53 | 37.07 ± 1.62 | 27.00 ± 3.95 | 47.34 ± 3.36 |
| Traditional industry city | 35.25 ± 0.85 | 32.81 ± 3.94 | 22.20 ± 4.69 | 43.70 ± 5.35 |
| Less developed country | 33.96 ± 0.73 | 37.30 ± 3.31 | 39.23 ± 4.68 | 55.62 ± 4.67 |
| Aging and periphery country | 34.76 ± 1.21 | 41.37 ± 5.15 | 21.61 ± 19.27 | 81.79 ± 9.63 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, S.-W.; Chiu, T.-Y.; Liou, T.-H.; Yen, C.-F.; Chen, H.-G. The Relationship of Urbanization and Performance of Activity and Participation Functioning among Adults with Developmental Disabilities in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 7553. https://doi.org/10.3390/ijerph17207553
Lin S-W, Chiu T-Y, Liou T-H, Yen C-F, Chen H-G. The Relationship of Urbanization and Performance of Activity and Participation Functioning among Adults with Developmental Disabilities in Taiwan. International Journal of Environmental Research and Public Health. 2020; 17(20):7553. https://doi.org/10.3390/ijerph17207553
Chicago/Turabian StyleLin, Shyang-Woei, Tzu-Ying Chiu, Tsan-Hon Liou, Chia-Feng Yen, and Hui-Guan Chen. 2020. "The Relationship of Urbanization and Performance of Activity and Participation Functioning among Adults with Developmental Disabilities in Taiwan" International Journal of Environmental Research and Public Health 17, no. 20: 7553. https://doi.org/10.3390/ijerph17207553
APA StyleLin, S.-W., Chiu, T.-Y., Liou, T.-H., Yen, C.-F., & Chen, H.-G. (2020). The Relationship of Urbanization and Performance of Activity and Participation Functioning among Adults with Developmental Disabilities in Taiwan. International Journal of Environmental Research and Public Health, 17(20), 7553. https://doi.org/10.3390/ijerph17207553








