Prevalence of Alpha(α)-Thalassemia in Southeast Asia (2010–2020): A Meta-Analysis Involving 83,674 Subjects
Abstract
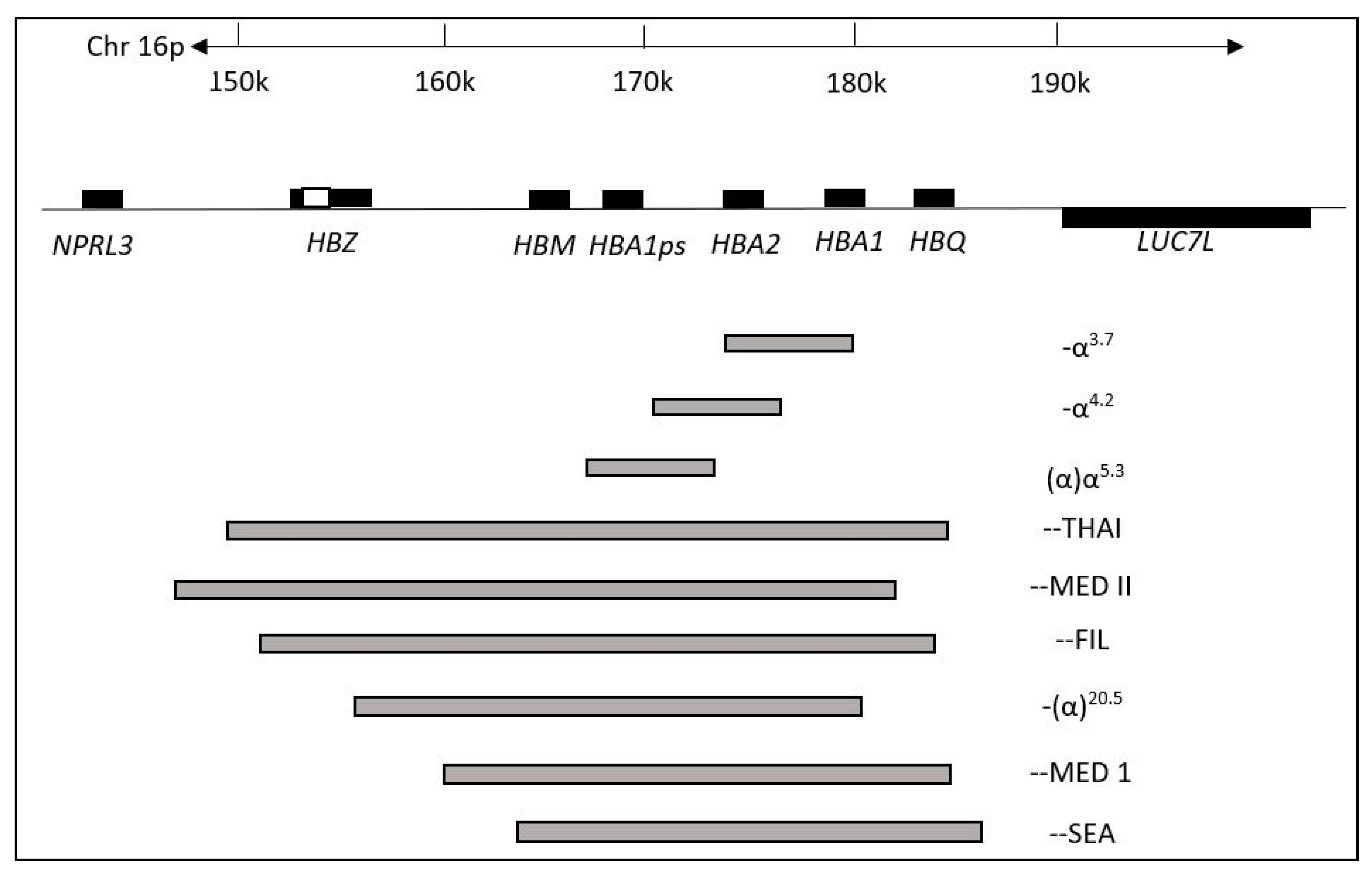
1. Introduction
2. Materials and Methods
2.1. Study Guidelines and Literature Search
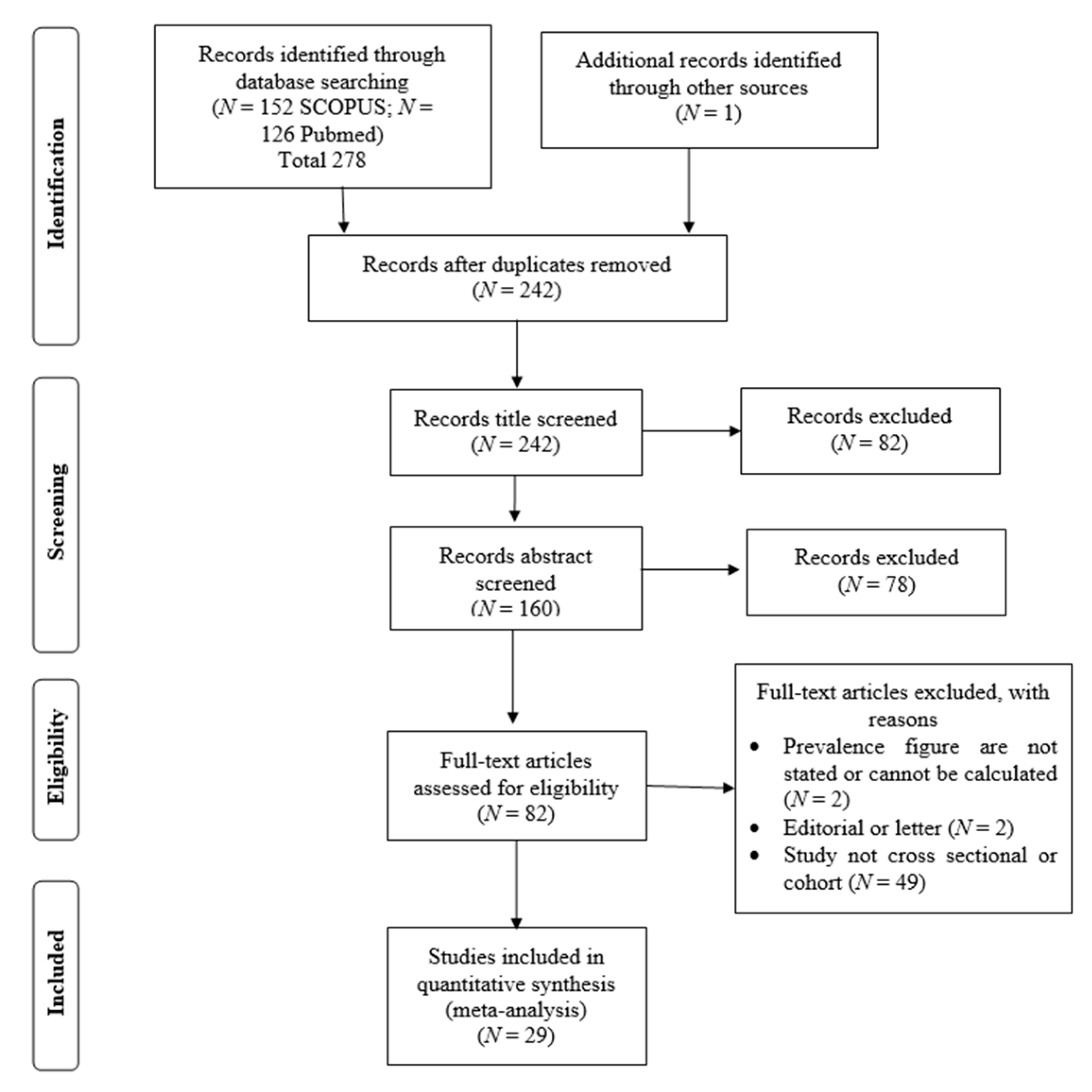
2.2. Selection of Studies and Data Extraction
2.3. Statistical Analyses
3. Results
3.1. Study Characteristics
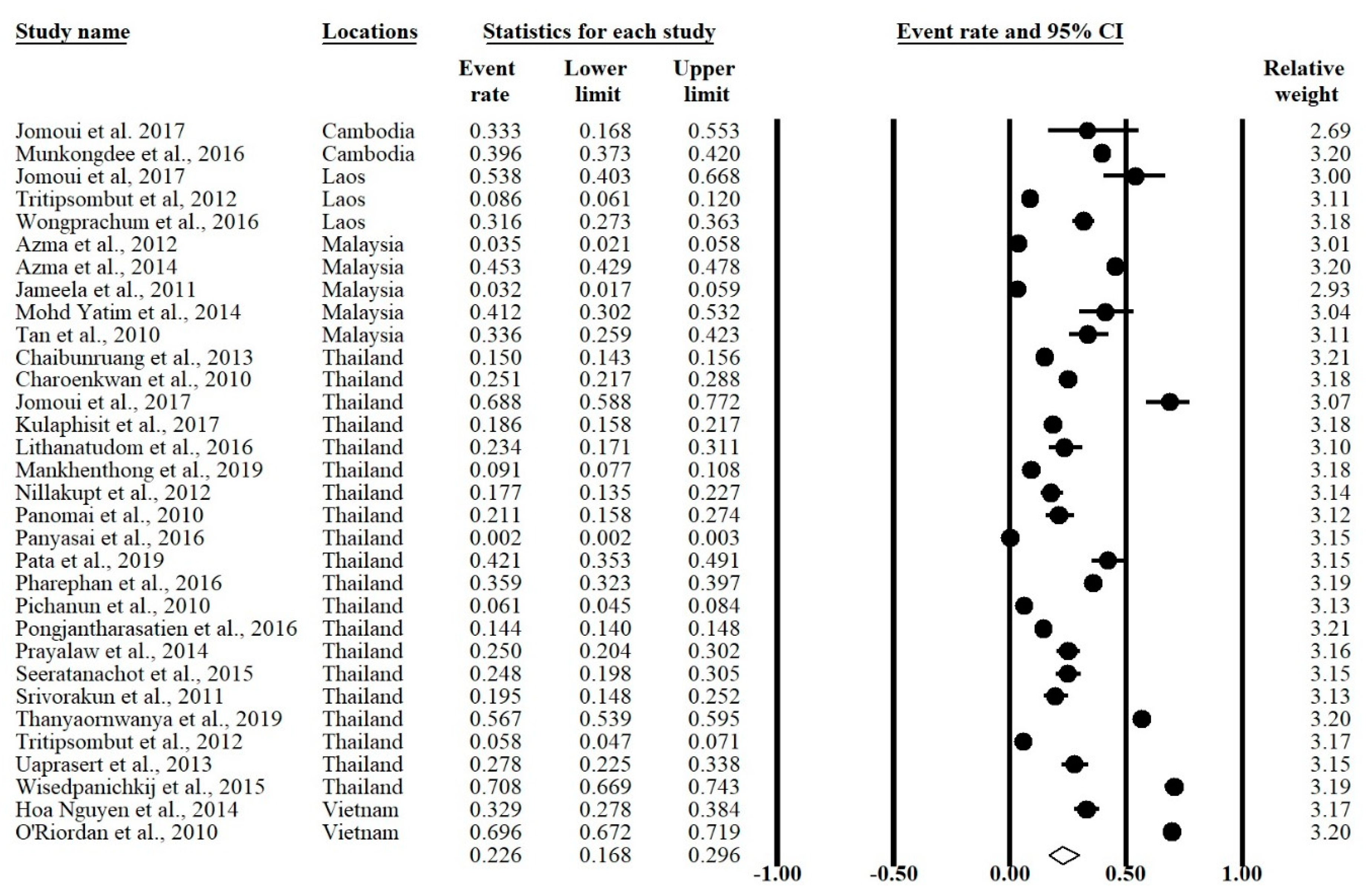
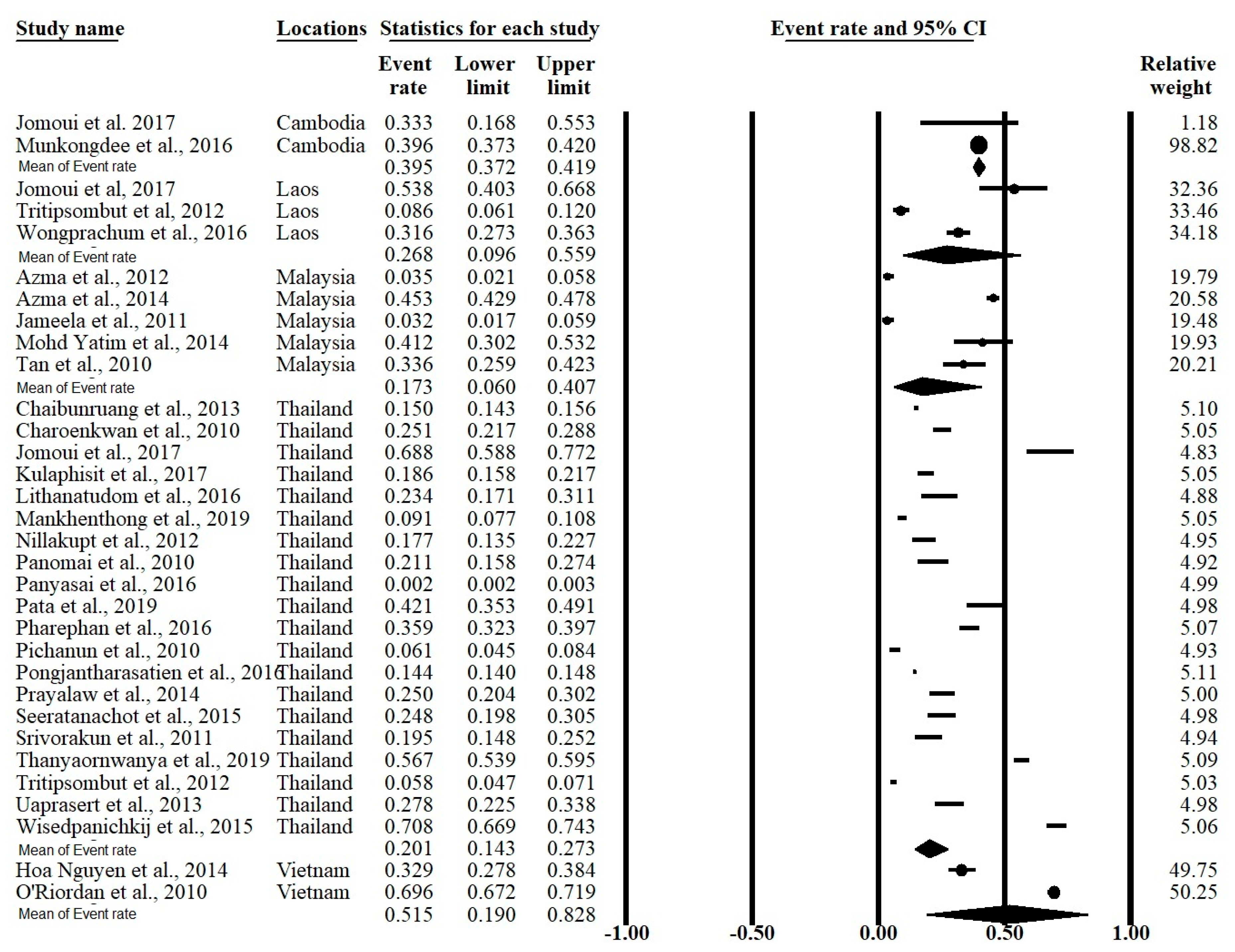
3.2. Meta-Analysis Outcomes
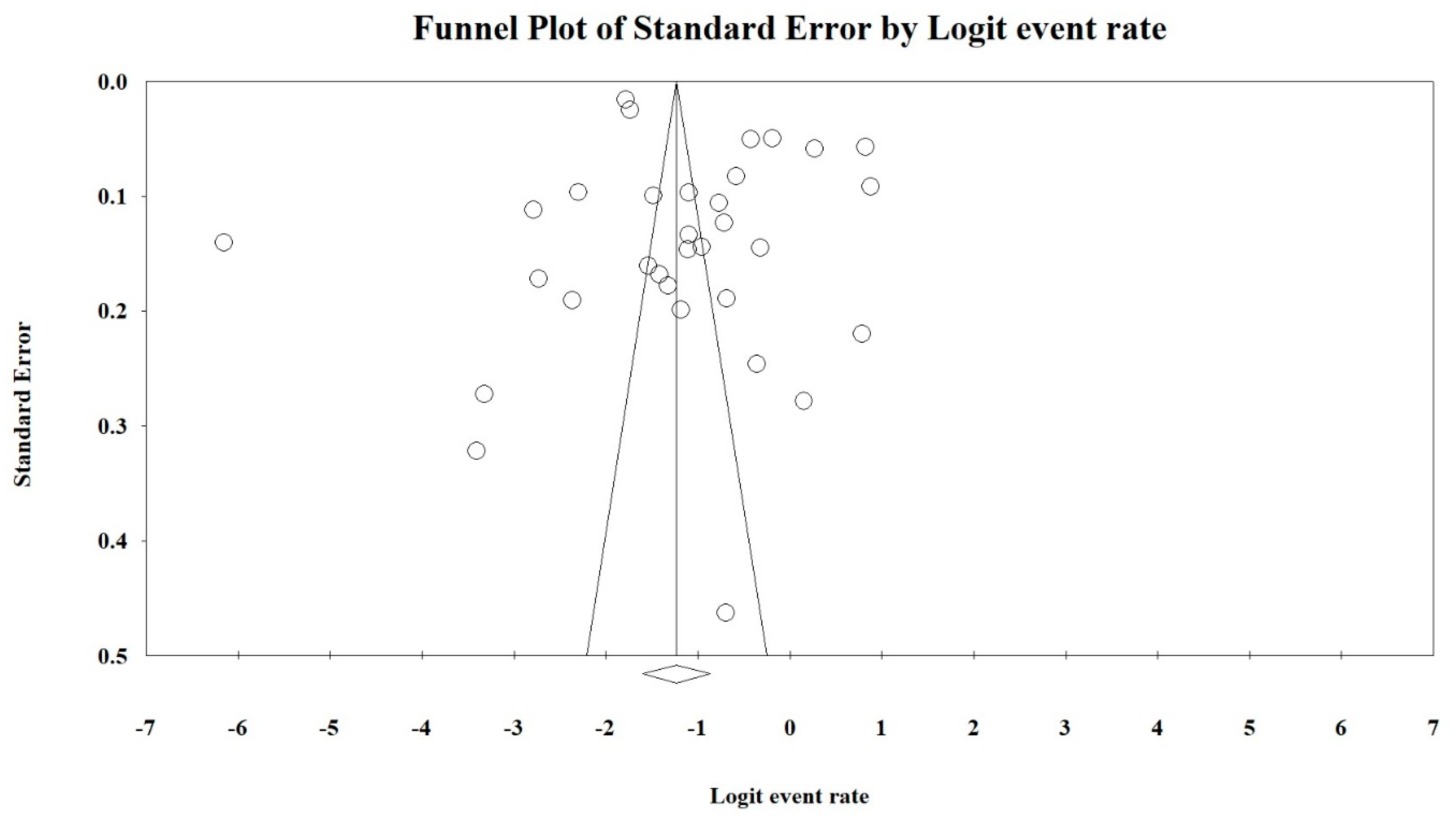
3.3. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Higgs, D.R.; Engel, J.D.; Stamatoyannopoulos, G. Thalassemia. Lancet 2012, 379, 73–383. [Google Scholar] [CrossRef]
- Rosnah, B.; Rosline, H.; Zaidah, A.W.; Noor Haslina, M.N.; Marini, R.; Shafini, M.Y.; Nurul Ain, F.A. Detection of common deletional alpha-thalassemia spectrum by molecular technique in Kelantan, Northeastern Malaysia. ISRN Hematol. 2010, 2012, 462969. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.I.M.A.; Lee, P.C.; Wee, Y.C.; Tan, K.L.; Mahali, N.F.; George, E.; Chua, K.H. High prevalence of alpha- and beta-thalassemia in the Kadazadusuns in East Malaysia: Challenges in providing effective health care for an indigenous group. J. Biomed. Biotechnol. 2010, 2010, 706872. [Google Scholar] [CrossRef] [PubMed]
- Azma, R.Z.; Ainoon, O.; Hafiza, A.; Azlin, I.; Noor Farisah, A.R.; Nor Hidayati, S.; Noor Hamidah, H. Molecular characteristic of alpha thalassemia among patients diagnosed in UKM medical centre. Malays. J. Pathol. 2014, 36, 27–32. [Google Scholar]
- Kulaphisit, M.; Kampuansai, J.; Leecharoenkiat, K.; Wathikthinnakon, M.; Kangwanpong, D.; Munkongdee, T.; Svasti, S.; Fucharoen, S.; Smith, D.R.; Lithanatudom, P. A comprehensive ethnic-based analysis of alpha thalassemia allele frequency in northern Thailand. Sci. Rep. 2017, 7, 4690. [Google Scholar] [CrossRef]
- Farashi, S.; Harteveld, C.L. Molecular basis of α-thalassemia. Blood Cells Mol. Dis. 2018, 70, 43–53. [Google Scholar] [CrossRef]
- Chui, D.H.K. Alpha-Thalassemia: Hb H disease and Hb Bart’s hydrops fetalis. Ann. N. Y. Acad. Sci. 2005, 1054, 25–32. [Google Scholar] [CrossRef]
- Weatherall, D.J.; Clegg, J.B. The Thalassemia Syndrome, 4th ed.; Blackwell Scientific Publication: Oxford, UK, 2011. [Google Scholar]
- Casale, M.; Meloni, A.; Filosa, A.; Cuccia, L.; Caruso, V.; Palazzi, G.; Rita Gamberini, M.; Pitrolo, L.; Caterina Putti, M.; Giuseppe D’Ascola, D.; et al. Multiparametric Cardiac Magnetic Resonance Survey in Children with Thalassemia Major. Circ. Cardiovasc. Imaging 2015, 8, e003230. [Google Scholar] [CrossRef]
- Kurtoglu, A.U.; Kurtoglu, E.; Temizkan, A.K. Effect of iron overload on endocrinopathies in patients with beta-thalassaemia major and intermedia. Endokrynol. Pol. 2012, 63, 260–263. [Google Scholar]
- Suthat, F.; Pranee, W. Haemoglobinopathies in Southeast Asian. Indian J. Med. Res. 2011, 134, 498–506. [Google Scholar]
- Galanello, R.; Cao, A. Alpha-thalassemia. Gen. Med. 2011, 13, 83–88. [Google Scholar] [CrossRef]
- Kuesap, J.; Chaijaroenkul, W.; Rungsihirunrat, K.; Pongjantharasatien, K.; Na-Bangchang, K. Coexistance of Malaria and Thalassemia in malaria endemic areas of Thailand. Korean J. Parasitol. 2015, 53, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Rosanas-Uegell, A.; Senn, N.; Raru, P.; Aponte, J.J.; Reeder, J.C.; Siba, P.M.; Michon, P.; Mueller, I. Lack of associations of α(+)-thalassemia with the risk of Plasmodium falciparum and Plasmodium vivax infection and disease in a cohort of children aged 3-21 months from Papua New Guinea. Int. J. Parasitol. 2012, 42, e1000097. [Google Scholar] [CrossRef]
- Vento, S.; Cainelli, F.; Cesario, F. Infections and thalassemia. Lancet Infect. Dis. 2006, 6, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Ryan, K.; Bain, B.J.; Worthington, D.; James, J.; Plews, D.; Mason, A.; Roper, D.; Rees, D.C.; de la Salle, B.; Streetly, A.; et al. Significant haemoglobinopathies: Guidelines for screening and diagnosis. Br. J. Haematol. 2010, 149, 35–49. [Google Scholar] [CrossRef]
- Lithanatudom, P.; Khampan, P.; Smith, D.R.; Svasti, S.; Fucharoen, S.; Kangwanpong, D.; Kampuansai, J. The prevalence of alpha-thalssemia amongst Tai and Mon-Khmer ethnic groups residing in northern Thailand: A population-based study. Hematology 2016, 21, 480–485. [Google Scholar] [CrossRef]
- O’Riordan, S.; Hien, T.T.; Miles, K.; Allen, A.; Quyen, N.N.; Hung, N.Q.; Anh, D.Q.; Tuyen, L.N.; Khia, D.B.; Thai, C.Q.; et al. Large scale screening for haemoglobin disorders in southern Vietnam: Implications for avoidance and management. Br. J. Haematol. 2010, 150, 359–364. [Google Scholar] [CrossRef]
- Moher, D.; Loberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Dersimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Light, R.J.; Pillemer, D.B. Summing up: The Science of Reviewing Research; Harvard University Press: Cambridge, MA, USA, 1984. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H.R. Comprehensive meta-analysis version 2. Englewood 2005, 104, 188–191. [Google Scholar]
- Munkongdee, T.; Tanakulmas, J.; Butthep, P.; Winichagoon, P.; Main, B.; Yiannakis, M.; George, J.; Devenish, R.; Fucharoen, S.; Svasti, S. Molecular epidemiology of hemoglobinpathies in Cambodia. Hemoglobin 2016, 40, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Jomoui, W.; Fucharoen, G.; Sanchaisuriya, K.; Charoenwijitkul, P.; Maneesarn, J.; Xu, X.; Fucharoen, S. Genetic origin of α0-thalassemia (SEA deletion) in Southeast Asian populations and application to accurate prenatal diagnosis of Hb Bart’s hydrops fetalis syndrome. J. Hum. Gen. 2017, 62, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Wongprachum, K.; Sanchaisuriya, K.; Dethvongphanh, M.; Norcharoen, B.; Vidamaly, V.; Sanchaisuriya, P.; Fucharoen, S.; Fucharoen, G.; Schelp, F.P. Molecular heterogeneity of thalassemia among pregnant Laotian women. Acta Hematol. 2016, 135, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Tritipsombut, J.; Sanchaisuriya, K.; Phollarp, P.; Bouakhasith, D.; Sanchaisuriya, P.; Fucharoen, G.; Fucharoen, S.; Schelp, F.P. Micromapping of thalassemia and hemoglobinopathies in different regions of northeast Thailand and Vientaine, Laos people’s democratic republic. Hemoglobin 2012, 36, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Azma, R.Z.; Ainoon, O.; Azlin, I.; Hamenuddin, H.; Hadi, N.A.; Tatt, W.K.; Syazana, I.N.; Asmaliza, A.M.; Das, S.; Hamidah, N.H. Prevalence of iron deficiency anaemia and thalassemia trait among undergraduate medical students. Clin. Ter. 2012, 163, 287–291. [Google Scholar]
- Jameela, S.; Sharifah Sabirah, S.O.; Babam, J.; Phan, C.L.; Visalachy, P.; Chang, K.M.; Salwana, M.A.; Zuridah, A.; Subramanian, Y.; Rahimah, A. Thalassemia screening among students in a secondary school in Ampang, Malaysia. Med. J. Malays. 2011, 66, 522–524. [Google Scholar]
- Mohd Yatim, N.F.; Abd Rahim, M.; Menon, K.; Al-Hassan, F.M.; Ahmad, R.; Manocha, A.B.; Saleem, M.; Yahaya, B.H. Molecular characterization of α and β-thalassaemia among malay patients. Int. J. Mol. Sci. 2014, 15, 8835–8845. [Google Scholar] [CrossRef]
- Charoenkwan, P.; Taweephol, R.; Sirichotiyakul, S.; Tantiprabha, W.; Sae-Tung, R.; Suanta, S.; Sakdasirisathaporn, P.; Sanguansermsri, T. Cord blood screening for α-thalassemia and hemoglobin variants by isoelectric focusing in northern Thai neonates: Correlation with genotypes and hematologic parameters. Blood Cells Mol. Dis. 2010, 45, 53–57. [Google Scholar] [CrossRef]
- Nillakupt, K.; Nathalang, O.; Arnutti, P.; Jindadamrongwech, S.; Boonsiri, T.; Panichkul, S.; Areekul, W. Prevalence and hematological parameters of thalassemia in the Kradarn subdistrict Chachoengsao province, Thailand. J. Med. Assoc. Thai. 2011, 95, S124–S132. [Google Scholar]
- Pongjantharasatien, K.; Banyatsuppasin, W.; Pounsawat, S.; Jindadamrongwech, S. Occurrence of the --SEA, --THAI, and --FIL α-thalassemia-1 carriers from a 7-year study at Ramathibodi hospital, Bangkok, Thailand. Hemoglobin 2016, 40, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Pichanun, D.; Munkongdee, T.; Klamchuen, S.; Butthep, P.; Winichagoon, P.; Fucharoen, S.; Svasti, S. Molecular screening of the Hbs constant spring (codon 142, TAA>CAA, α2) and paksé (codon 142, TAA>TAT, α2) mutations in Thailand. Hemoglobin 2010, 34, 582–586. [Google Scholar] [CrossRef] [PubMed]
- Pharephan, S.; Sirivatanapa, P.; Makonkawkeyoon, S.; Tuntiwechapikul, W.; Makonkawkeyoon, L. Prevalence of α-thalassemia genotypes in pregnant women in northern Thailand. Indian J. Med. Res. 2016, 143, 315–322. [Google Scholar] [CrossRef]
- Panyasai, S.; Fucharoen, G.; Fucharoen, S. Hemoglobin variants in Northern Thailand: Prevalence, heterogeneity and molecular characteristics. Genet. Test Mol. Biomark. 2016, 20, 37–43. [Google Scholar] [CrossRef]
- Panomai, N.; Sanchaisuriya, K.; Yamsri, S.; Sanchaisuriya, P.; Fucharoen, S.; Schelp, F.P. Thalassemia and iron deficiency in a group of northeast Thai school children: Relationship to the occurrence of anaemia. Eur. J. Pediatr. 2010, 169, 1317–1322. [Google Scholar] [CrossRef]
- Prayalaw, P.; Fuchafoen, G.; Fucharoen, S. Routine screening for α-thalassemia using an immunochromatographic strip assay for haemoglobin Bart’s. J. Med. Screen. 2014, 21, 120–125. [Google Scholar] [CrossRef]
- Seeratanachot, T.; Shimbhu, D.; Charoenkwan, P.; Sanguansermsri, T. Detection of deletion α+-thalassemia mutation [-α (3.7), -α (4.2)] by quantitative PCR assay. Southeast Asian J. Trop. Med. Public Health 2015, 46, 110–115. [Google Scholar]
- Wisedpanichkij, R.; Jindadamrongwech, S.; Butthep, P. Identification of Hb constant spring (HBA2: c.427T>C) by an automated high performance liquid chromatography method. Hemoglobin 2015, 39, 190–195. [Google Scholar] [CrossRef]
- Uaprasert, N.; Settapiboon, R.; Amomsiriwat, S.; Sarnthammakul, P.; Thanapat, T.; Rojnuckarin, P.; Sutcharitchan, P. Diagnostic utility of isoelectric focusing and high performance liquid chromatography in neonatal cord blood screening for thalassemia and non-sickling hemoglobinopathies. Clin. Chim. Acta. 2013, 427, 23–26. [Google Scholar] [CrossRef]
- Srivorakun, H.; Fucharoen, G.; Changtrakul, Y.; Komwilaisak, P.; Fucharoen, S. Thalassemia and hemoglobinopathies in South East Asia newborns: Diagnostic assessment using capillary electrophoresis system. Clin. Biochem. 2011, 44, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Chaibunruang, A.; Prommetta, S.; Yamsri, S.; Fucharoen, G.; Sae-Ung, N.; Sanchaisuriya, K.; Fucharoen, S. Molecular and hematological studies in a large cohort of α0-thalassemia in northeast Thailand: Data from a single referral centre. Blood Cells Mol. Dis. 2013, 51, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Thanyaornwanya, C.; Singha, K.; Fucharoen, G.; Sanchaisuriya, K.; Thepphitak, P.; Wintachai, P.; Karnpean, R.; Fucharoen, S. Molecular characteristics of α+-thalassemia (3.7 kb deletion) in Southeast Asia: Molecular subtypes, haplotypic heterogeneity, multiple founder effects and laboratory diagnosis. Clin. Biochem. 2019, 71, 31–37. [Google Scholar] [CrossRef]
- Mankhenthong, K.; Phusua, A.; Suantan, S.; Srisittipoj, P.; Charoenkwan, P.; Sanguansermsri, T. Molecular characteristics of thalassemia and haemoglobin variants in prenatal diagnosis program in northern Thailand. Int. J. Hematol. 2019, 110, 474–481. [Google Scholar] [CrossRef]
- Pata, S.; Laopajon, W.; Pongpaiboon, M.; Thongkum, W.; Polpong, N.; Munkongdee, T.; Paiboonsukwong, K.; Fucharoen, S.; Tayapiwatana, C.; Kasinrerk, W. Impact of the detection of ζ-globin chains and haemoglobin Bart’s using immunochromatographic strip test for α0-thalassemia (--SEA) differential diagnosis. PLoS ONE 2019, 14, e0223996. [Google Scholar] [CrossRef]
- Hoa Nguyen, V.; Sanchaisuriya, K.; Wongprachum, K.; Nguyen, M.D.; Phan, T.T.; Vo, V.T.; Sanchaisuriya, P.; Fucharoen, S.; Schelp, F.P. Hemoglobin constant spring is markedly high in women of an ethnic minority group in Vietnam: A community-based survey and hematologic features. Blood Cell Mol. Dis. 2014, 52, 161–165. [Google Scholar] [CrossRef]
- Modell, B.; Darlison, M. Global epidemiology in haemoglobin disorders and derived service indicators. Bull. World Health Organ. 2008, 86, 480–487. [Google Scholar] [CrossRef]
- Nadkarni, A.; Phanasgaonkar, S.; Colah, R.; Mohanty, D.; Ghosh, K. Prevalence and Molecular Characterization of α-Thalassemia Syndromes among Indians. Genet. Test. 2008, 12, 177–180. [Google Scholar] [CrossRef]
- Souza, A.E.S.; Cardoso, G.L.; Takanashi, S.Y.L.; Guerreiro, J.F. α-Thalassemia (3.7 kb deletion) in a population from the Brazilian Amazon region: Santarém, Pará State. Genet. Mol. Res. 2009, 8, 477–481. [Google Scholar] [CrossRef]
- AL-Awamy, B.H. Thalassemia syndromes in Saudi Arabia. Meta-analysis of local studies. Saudi Med. J. 2000, 21, 8–17. [Google Scholar]
- Kee, B.P.; Lian, L.H.; Lee, P.C.; Lai, T.X.; Chua, K.H. Genetic data for 15 STR loci in a Kadazan-Dusun population from East Malaysia. Genet. Mol. Res. 2011, 10, 739–743. [Google Scholar] [CrossRef] [PubMed]
- Forget, B.G.; Bunn, H.F. Classification of the disorders of haemoglobin. Cold Spring Harb. Perspect. Med. 2013, 3, a011684. [Google Scholar] [CrossRef]
- Krause, M.A.; Diakite, S.A.S.; Lopera-Mesa, T.M.; Amaratunga, C.; Arie, T.; Traore, K.; Doumbia, S.; Konate, D.; Keefer, J.R.; Diakite, M.; et al. α-thalassemia impairs the cytoadherence of Plasmodium falciparum-infected erythrocytes. PLoS ONE 2012, e37214. [Google Scholar] [CrossRef] [PubMed]
- Gundula, M.-O.; Gros, P. Erthrocyte variants and the nature of their malaria protective effect. Cell. Microbiol. 2005, 7, 753–763. [Google Scholar] [CrossRef]
- World Health Organization. World Malaria Report 2019; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
| Author [Reference] | α-Thalassemia Genotyping Method | Genotypes Found in the Study | Country | Specific Ethnic 1 | Events 2 | Total 3 |
|---|---|---|---|---|---|---|
| Munkongdee et al., 2016 [25] | Polymerase chain reaction (PCR) | -α3.7, -α4.2, --SEA, αCS, αPs | Cambodia | N/A | 646 | 1631 |
| Jomoui et al., 2017 [26] | PCR | --SEA | Cambodia | N/A | 7 | 21 |
| Wongprachum et al., 2012 [27] | PCR | -α3.7, -α4.2, --SEA, --THAI, αCS, αPs, αQ-Thailand | Laos | N/A | 130 | 411 |
| Jomoui et al., 2017 [26] | PCR | --SEA | Laos | N/A | 28 | 52 |
| Tritipsombut et al., 2012 [28] | PCR | -α3.7, -α4.2, --SEA, αCS, αPs | Laos | N/A | 30 | 349 |
| Azma et al., 2012 [29] | PCR | Malaysia | N/A | 14 | 400 | |
| Azma et al., 2014 [4] | PCR | -α3.7, -α4.2, --SEA, αCS, αCD59, αIVS I-1 | Malaysia | Malay, Chinese, Indian, Other | 736 | 1623 |
| Jameela et al., 2011 [30] | PCR | -α3.7, -α4.2, --SEA, --FIL, α125 | Malaysia | Malay, Chinese, Indian, Sikh, Iban | 10 | 310 |
| Mohd Yatim et al., 2014 [31] | PCR | -α3.7, --SEA, αCS, αCD59, | Malaysia | Malay | 28 | 68 |
| Tan et al., 2010 [3] | PCR | -α3.7, -α4.2, --SEA, --THAI, --FIL, αCS, α125, | Malaysia | Kadazandusun | 42 | 125 |
| Charoenkwan et al., 2010 [32] | PCR | -α3.7, -α4.2, --SEA, -αQ-Thailand, αCS | Thailand | N/A | 142 | 566 |
| Lithanatudom et al., 2016 [17] | PCR | -α3.7, -α4.2, --SEA, --THAI, αCS, αPs | Thailand | Yong, Yuan, Lue, Khuen, Blang, Mon, Paluang, Lawa | 33 | 141 |
| Nillakupt et al., 2012 [33] | PCR | -α3.7, --SEA, αCS, αPs | Thailand | N/A | 47 | 266 |
| Pongjantharasatien et al., 2016 [34] | PCR | --SEA, --THAI, --FIL, -αthal-1 | Thailand | N/A | 4555 | 31,632 |
| Pichanun et al., 2010 [35] | PCR | -α3.7, αCS, αPs | Thailand | N/A | 36 | 587 |
| Pharephan et al., 2016 [36] | PCR | -α3.7, -α4.2, --SEA, αCS | Thailand | N/A | 229 | 638 |
| Panyasai et al., 2016 [37] | PCR | -α3.7, -αQT, --SEA, | Thailand | N/A | 51 | 23,914 |
| Panomai et al., 2010 [38] | PCR | -α3.7, -α4.2, --SEA, --THAI, αCS, αPs | Thailand | N/A | 40 | 190 |
| Prayalaw et al., 2014 [39] | PCR | -α3.7, -α4.2, --SEA, αCS, -αQ-Thailand | Thailand | N/A | 75 | 300 |
| Seeratanachot et al., 2015 [40] | Realtime-PCR | -α3.7, -α4.2, --SEA | Thailand | N/A | 62 | 250 |
| Wisedpanichkij et al., 2015 [41] | PCR | -α3.7, -α4.2, --SEA, αCS | Thailand | N/A | 409 | 578 |
| Uaprasert et al., 2013 [42] | PCR | -α3.7, -α4.2, αCS | Thailand | N/A | 67 | 241 |
| Srivorakun et al., 2011 [43] | PCR | -α3.7, --SEA, αCS | Thailand | N/A | 44 | 226 |
| Tritipsombut et al., 2012 [28] | PCR | -α3.7, -α4.2, --SEA, αCS, αPs | Thailand | N/A | 85 | 1460 |
| Chaibunruang et al., 2013 [44] | PCR | --SEA, --THAI | Thailand | N/A | 1874 | 12,525 |
| Kulaphisit et al., 2017 [5] | PCR | -α3.7, -α4.2, --SEA, --THAI, αCS, αPs | Thailand | Yong, Lue, Yuan, Shan, Khuen, Htin, Paluang, Blang, Lawa, Mon, Skaw Karen, Pwo Karen, Padong Karen | 124 | 668 |
| Thanyaornwanya et al., 2019 [45] | PCR | -α3.7, -α4.2, αCS, αPs | Thailand | N/A | 676 | 1192 |
| Jomoui et al., 2017 [26] | PCR | --SEA | Thailand | N/A | 66 | 96 |
| Mankhenthong et al., 2019 [46] | PCR | -α3.7, -α4.2, --SEA, --THAI, αCS | Thailand | N/A | 118 | 1290 |
| Pata et al., 2019 [47] | PCR | -α3.7, -α4.2, --SEA, --THAI, αCS | Thailand | N/A | 82 | 195 |
| O’Riordan et al., 2010 [18] | PCR | -α3.7, -α4.2, --SEA, --THAI, --FIL, αCS | Vietnam | Kinh, Dao, Tay, Nung, S’Tieng, M’Nong, Rac Iay, E De | 996 | 1431 |
| Hoa Nguyen et al., 2014 [48] | PCR | -α3.7, -α4.2, --SEA, --THAI, --SEA, αCS, αPs | Vietnam | Cό-Tu | 98 | 298 |
| Total | 11,580 | 83,674 | ||||
| Heterogeneity | Prevalence Rate (95% CI) | Sample Size (N) | No. of Studies (N) | Subgroups | |
|---|---|---|---|---|---|
| I2 (%) | p-Value | ||||
| 99.53 | <0.001 | 0.226 (0.168–0.296) | 83,674 | 32 | Overall |
| 0 | 0.560 | 0.395 (0.372–0.419) | 1652 | 2 | Cambodia |
| 97.26 | <0.001 | 0.268 (0.096–0.559) | 812 | 3 | Laos |
| 98.20 | <0.001 | 0.173 (0.060–0.407) | 2526 | 5 | Malaysia |
| 99.47 | <0.001 | 0.201 (0.143–0.273) | 76,955 | 20 | Thailand |
| 99.22 | <0.001 | 0.515 (0.190–0.828) | 1729 | 2 | Vietnam |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goh, L.P.W.; Chong, E.T.J.; Lee, P.-C. Prevalence of Alpha(α)-Thalassemia in Southeast Asia (2010–2020): A Meta-Analysis Involving 83,674 Subjects. Int. J. Environ. Res. Public Health 2020, 17, 7354. https://doi.org/10.3390/ijerph17207354
Goh LPW, Chong ETJ, Lee P-C. Prevalence of Alpha(α)-Thalassemia in Southeast Asia (2010–2020): A Meta-Analysis Involving 83,674 Subjects. International Journal of Environmental Research and Public Health. 2020; 17(20):7354. https://doi.org/10.3390/ijerph17207354
Chicago/Turabian StyleGoh, Lucky Poh Wah, Eric Tzyy Jiann Chong, and Ping-Chin Lee. 2020. "Prevalence of Alpha(α)-Thalassemia in Southeast Asia (2010–2020): A Meta-Analysis Involving 83,674 Subjects" International Journal of Environmental Research and Public Health 17, no. 20: 7354. https://doi.org/10.3390/ijerph17207354
APA StyleGoh, L. P. W., Chong, E. T. J., & Lee, P.-C. (2020). Prevalence of Alpha(α)-Thalassemia in Southeast Asia (2010–2020): A Meta-Analysis Involving 83,674 Subjects. International Journal of Environmental Research and Public Health, 17(20), 7354. https://doi.org/10.3390/ijerph17207354





