Effect of Electronic Activity Monitors and Pedometers on Health: Results from the TAME Health Pilot Randomized Pragmatic Trial
Abstract
1. Introduction
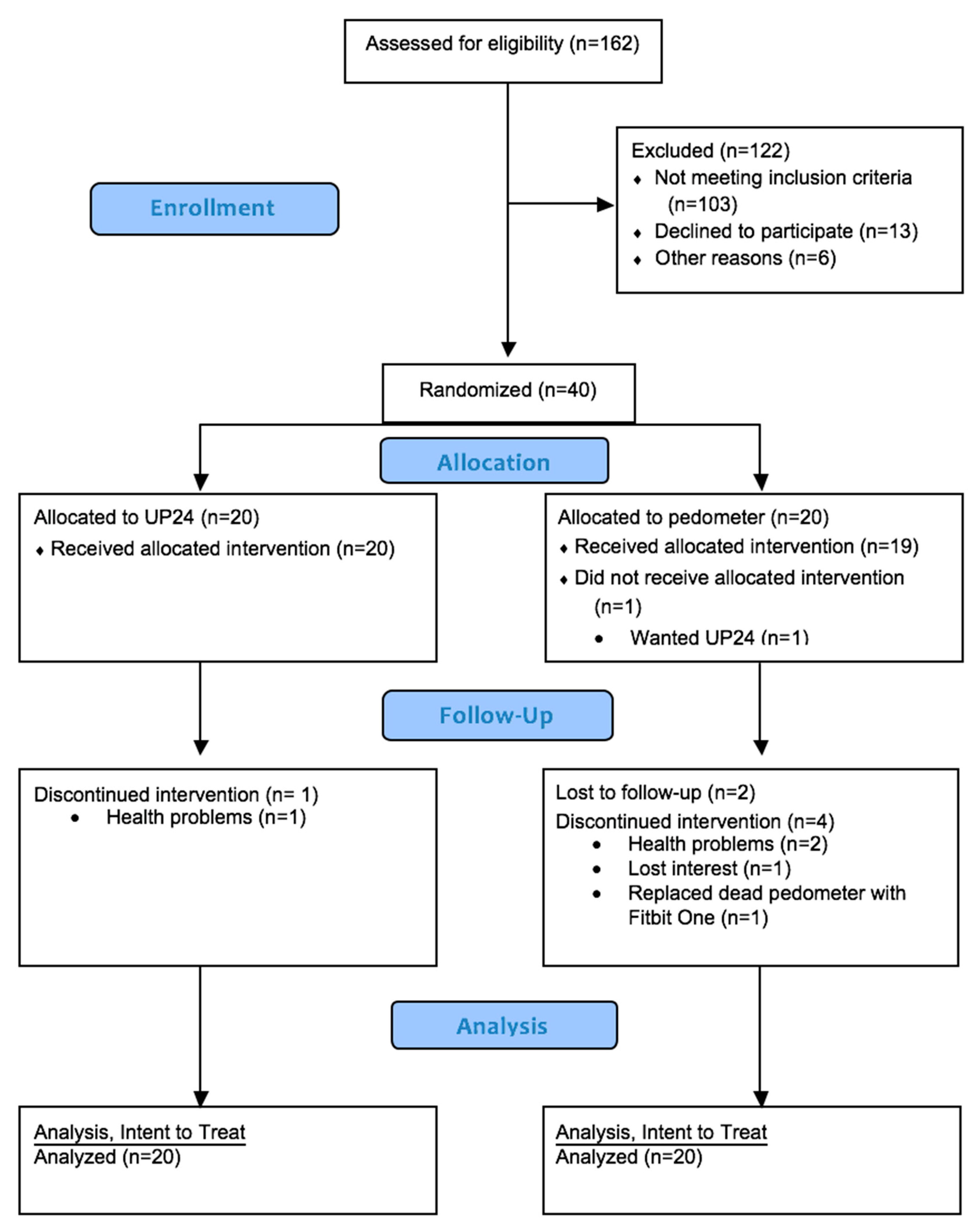
2. Materials and Methods
2.1. Sample
2.2. Intervention
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Primary Outcomes
3.2. Secondary Outcomes
4. Discussion
4.1. Limitations and Strengths
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Cogswell, M.E.; Flanders, W.D.; Hong, Y.; Zhang, Z.; Loustalot, F.; Gillespie, C.; Merritt, R.; Hu, F.B. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012, 307, 1273–1283. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [PubMed]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Abraham, C.; Whittington, C.; McAteer, J.; Gupta, S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychol. 2009, 28, 690–701. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.E.; Ma, J.; Azar, K.M.; Bennett, G.G.; Peterson, E.D.; Zheng, Y.; Riley, W.; Stephens, J.; Shah, S.H.; Suffoletto, B.; et al. Current Science on Consumer Use of Mobile Health for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation 2015. [Google Scholar] [CrossRef]
- Lewis, Z.H.; Lyons, E.J.; Jarvis, J.M.; Baillargeon, J. Using an electronic activity monitor system as an intervention modality: A systematic review. BMC Public Health 2015, 15, 585. [Google Scholar] [CrossRef]
- Danova, T. Just 3.3 Million Fitness Trackers Were Sold in the US in the Past Year. Available online: http://www.businessinsider.com/33-million-fitness-trackers-were-sold-in-the-us-in-the-past-year-2014-5 (accessed on 18 May 2016).
- Lee, J.M.; Kim, Y.; Welk, G.J. Validity of Consumer-Based Physical Activity Monitors. Med. Sci. Sports Exerc. 2014, 46, 1840–1848. [Google Scholar] [CrossRef]
- Lyons, E.J.; Lewis, Z.H.; Mayrsohn, B.G.; Rowland, J.L. Behavior change techniques implemented in electronic lifestyle activity monitors: A systematic content analysis. J. Med. Internet Res. 2014, 16, e192. [Google Scholar] [CrossRef]
- Michie, S.; Ashford, S.; Sniehotta, F.F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, M.G.; Whitlock, E.P.; DePue, J.; Planning Comm Addressing, M. Multiple behavioral risk factor interventions in primary care summary of research evidence. Am. J. Prev. Med. 2004, 27, 61–79. [Google Scholar] [CrossRef] [PubMed]
- Spring, B.; Ockene, J.K.; Gidding, S.S.; Mozaffarian, D.; Moore, S.; Rosal, M.C.; Brown, M.D.; Vafiadis, D.K.; Cohen, D.L.; Burke, L.E.; et al. Better Population Health Through Behavior Change in Adults A Call to Action. Circulation 2013, 128, 2169–2176. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.; Kerry, S.M.; Victor, C.R.; Ekelund, U.; Woodcock, A.; Iliffe, S.; Whincup, P.H.; Beighton, C.; Ussher, M.; Limb, E.S.; et al. A Primary Care Nurse-Delivered Walking Intervention in Older Adults: PACE (Pedometer Accelerometer Consultation Evaluation)-Lift Cluster Randomised Controlled Trial. PLoS Med. 2015, 12, e1001783. [Google Scholar] [CrossRef] [PubMed]
- Normansell, R.; Smith, J.; Victor, C.; Cook, D.G.; Kerry, S.; Iliffe, S.; Ussher, M.; Fox-Rushby, J.; Whincup, P.; Harris, T. Numbers are not the whole story: A qualitative exploration of barriers and facilitators to increased physical activity in a primary care based walking intervention. BMC Public Health 2014, 14, 19. [Google Scholar] [CrossRef]
- Patel, A.; Schofield, G.M.; Kolt, G.S.; Keogh, J.W.L. Perceived Barriers, Benefits, and Motives for Physical Activity: Two Primary-Care Physical Activity Prescription Programs. J. Aging Phys. Act. 2013, 21, 85–99. [Google Scholar]
- Franklin, N.C.; Lavie, C.J.; Arena, R.A. Personal health technology: A new era in cardiovascular disease prevention. Postgrad. Med. 2015, 127, 150–158. [Google Scholar] [CrossRef]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar]
- O’Driscoll, R.; Turicchi, J.; Beaulieu, K.; Scott, S.; Matu, J.; Deighton, K.; Finlayson, G.; Stubbs, J. How well do activity monitors estimate energy expenditure? A systematic review and meta-analysis of the validity of current technologies. Br. J. Sports Med. 2020, 54, 332–340. [Google Scholar]
- Lewis, Z.H.; Ottenbacher, K.J.; Fisher, S.R.; Jennings, K.; Brown, A.F.; Swartz, M.C.; Lyons, E.J. Testing activity monitors’ effect on health: Study protocol for a randomized controlled trial among older primary care patients. JMIR Res. Protoc. 2016, 5, e59. [Google Scholar]
- Lewis, Z.H.; Ottenbacher, K.J.; Fisher, S.R.; Jennings, K.; Brown, A.F.; Swartz, M.C.; Martinez, E.; Lyons, E.J. The feasibility and RE-AIM evaluation of the TAME health pilot study. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 106. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, E.P.; Orleans, C.T.; Pender, N.; Allan, J. Evaluating primary care behavioral counseling interventions: An evidence-based approach. Am. J. Prev. Med. 2002, 22, 267–284. [Google Scholar] [CrossRef]
- D’Agostino, R.; Vasan, R.; Pencina, M.; Wolf, P.; Cobain, M.; Massaro, J.; Kannel, W. Cardiovascular Disease (10-Year Risk). Available online: https://www.framinghamheartstudy.org/risk-functions/cardiovascular-disease/10-year-risk.php (accessed on 7 October 2015 ).
- Rikli, R.E.; Jones, C.J. The Reliability and Validity of a 6-Minute Walk Test as a Measure of Physical Endurance in Older Adults. J. Aging Phys. Act. 1998, 6, 363–375. [Google Scholar] [CrossRef]
- Berntsen, S.; Hageberg, R.; Aandstad, A.; Mowinckel, P.; Anderssen, S.A.; Carlsen, K.H.; Andersen, L.B. Validity of physical activity monitors in adults participating in free-living activities. Br. J. Sports Med. 2010, 44, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Freiberger, E.; de Vreede, P.; Schoene, D.; Rydwik, E.; Mueller, V.; Frändin, K.; Hopman-Rock, M. Performance-based physical function in older community-dwelling persons: A systematic review of instruments. Age Ageing 2012, 41, 712–721. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual, Second Edition, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Pescatello, L.S.; Arena, R.; Riebe, D.; Thompson, P.D. ACSM’s Guidelines for Exercise Testing Prescription, 9th ed.; American College of Sports Medicine: Baltimore, MD, USA, 2013. [Google Scholar]
- McHorney, C.A.; Ware, J.E.; Raczek, A.E. The Mos 36-Item Short-Form Health Survey (SF-36). 2. Psychometric and Clinical-Tests of Validity in Measuring Physical and Mental-Health Constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef]
- Cella, D.; Gershon, R.; Bass, M.; Rothrock, N. Assessment Center. Available online: http://www.nihpromis.org/Measures/availableinstruments (accessed on 21 October 2015).
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155. [Google Scholar] [CrossRef]
- Little, R.J. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Cadmus-Bertram, L.A.; Marcus, B.H.; Patterson, R.E.; Parker, B.A.; Morey, B.L. Randomized Trial of a Fitbit-Based Physical Activity Intervention for Women. Am. J. Prev. Med. 2015, 49, 414–418. [Google Scholar] [CrossRef]
- Aittasalo, M.; Miilunpalo, S.; Kukkonen-Harjula, K.; Pasanen, M. A randomized intervention of physical activity promotion and patient self-monitoring in primary health care. Prev. Med. 2006, 42, 40–46. [Google Scholar] [CrossRef]
- van der Weegen, S.; Verwey, R.; Spreeuwenberg, M.; Tange, H.; van der Weijden, T.; de Witte, L. It’s LiFe! Mobile and Web-Based Monitoring and Feedback Tool Embedded in Primary Care Increases Physical Activity: A Cluster Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e184. [Google Scholar] [CrossRef] [PubMed]
- Ashe, M.C.; Winters, M.; Hoppmann, C.A.; Dawes, M.G.; Gardiner, P.A.; Giangregorio, L.M.; Madden, K.M.; McAllister, M.M.; Wong, G.; Puyat, J.H.; et al. “Not just another walking program”: Everyday Activity Supports You (EASY) model—A randomized pilot study for a parallel randomized controlled trial. Pilot Feasibility Stud. 2015, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: The Activity Counseling Trial: A randomized controlled trial. JAMA 2001, 286, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Collins, N.M.; Collins, C.S.; West, C.P.; Lerman, L.O.; Lerman, A. Digital health interventions for the prevention of cardiovascular disease: A systematic review and meta-analysis. Mayo Clin. Proc. 2015, 90, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Berra, K.; Rippe, J.; Manson, J.E. Making Physical Activity Counseling a Priority in Clinical Practice. J. Am. Med. Assoc. 2015, 314, 2617–2618. [Google Scholar] [CrossRef]
| Electronic Activity Monitor | Pedometer | All | |
|---|---|---|---|
| n (%) | |||
| Age, years; mean (SD) | 64 (5.1) | 63.2 (5.7) | 63.6 (5.3) |
| Female | 17 (85) | 13 (65) | 30 (75) |
| Non-Hispanic White | 12 (60) | 14 (70) | 26 (65) |
| Hispanic | 3 (15) | 2 (10) | 5 (12.5) |
| Black/African American | 4 (20) | 3 (15) | 7 (17.5) |
| Other | 1 (5) | 1 (5) | 2 (5) |
| Electronic Activity Monitor (n = 20) | Pedometer (n = 20) | Effect Size | |||
|---|---|---|---|---|---|
| mean (SD)/median † (IQR) | |||||
| Primary Outcomes | Baseline | Follow-up | Baseline | Follow-up | |
| Framingham non-laboratory risk score | 16.5 (12.2) | 16.6 (13.2) | 21.2 (13.6) | 21.2 (12.6) | −0.01 |
| Six-minute walk, ft. | 1487.4 (310.3) | 1561.0 (353.6) | 1568.4 (354.6) | 1642.9 (287.3) | −0.01 |
| Moderate/Vigorous Activity, minutes | 22.6 (21.5) | 33.8 (27.6) | 40.0 (33.9) | 40.2 (37.5) | 0.78 |
| Secondary Outcomes | |||||
| † Heart/Vascular age, years | 71.0 (20.0) | 69.0 (23.0) | 79.5 (17.0) | 78.0 (20.0) | 0.03 |
| Weight, kg | 81.7 (10.7) | 81.9 (11.2) | 94.1 (40.5) | 86.8 (13.6) | 0.22 |
| BMI, kg/m2 | 30.0 (3.2) | 30.0 (3.5) | 30.6 (3.1) | 30.5 (3.1) | 0.13 |
| Waist to Hip ratio | 0.8 (0.8) | 0.8 (0.1) | 0.9 (0.9) | 0.8 (0.1) | 0.45 |
| Systolic blood pressure, mmHg * | 125.0 (11.6) | 125.0 (14.5) | 134.8 (15.8) | 134.3 (14.6) | −0.00 |
| Diastolic blood pressure, mmHg | 79.6 (10.5) | 80.0 (9.8) | 83.1 (9.0) | 83.4 (10.0) | 0.01 |
| Resting pulse, bpm | 69.4 (11.4) | 69.1 (14.0) | 76.3 (10.3) | 76.5 (11.9) | −0.05 |
| † Chair stand, sec | 13.0 (9.5) | 13.3 (7.2) | 14.8 (3.3) | 13.8 (4.4) | 0.49 |
| † Tandem balance, sec | 10.0 (4.6) | 10.0 (0.0) | 10.0 (0.0) | 10.0 (0.0) | 0.46 |
| † 8 feet up and go, sec | 5.9 (2.2) | 6.0 (2.5) | 6.0 (2.0) | 5.9 (1.9) | 0.49 |
| † PROMIS Physical Function | 26.0 (16.0) | 31.0 (11) | 36.5 (11.0) | 37.0 (12.0) | 0.07 |
| † SF-36: Physical functioning | 65.0 (50.0) | 70.0 (55.0) | 80.0 (26.0) | 80.0 (19.0) | 0.27 |
| † SF-36: Physical health role limitations | 56.3 (56.3) | 62.5 (56.3) | 68.8 (51.6) | 75.0 (46.9) | 0.26 |
| † SF-36: Emotional role limitations | 75.0 (58.3) | 75.0 (41.7) | 91.7 (62.5) | 79.2 (45.8) | 0.20 |
| † SF-36: Energy/fatigue | 50.0 (18.8) | 50.0 (25.0) | 53.1 (20.3) | 62.5 (20.3) | −0.31 |
| † SF-36: Emotional well-being | 65.0 (30.0) | 75.0 (20.0) | 72.5 (18.0) | 80.0 (16.0) | −0.22 |
| † SF-36: Social functioning | 62.5 (50.0) | 75.0 (37.5) | 75.0 (56.3) | 75.0 (53.1) | 0.08 |
| † SF-36: Pain | 45.0 (47.5) | 45.0 (55.0) | 62.5 (55.6) | 67.5 (47.5) | −0.04 |
| † SF-36: General health | 61.1 (19.4) | 66.7 (19.4) | 62.5 (22.6) | 59.7 (26.4) | 0.39 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewis, Z.H.; Ottenbacher, K.J.; Fisher, S.R.; Jennings, K.; Brown, A.F.; Swartz, M.C.; Martinez, E.; Lyons, E.J. Effect of Electronic Activity Monitors and Pedometers on Health: Results from the TAME Health Pilot Randomized Pragmatic Trial. Int. J. Environ. Res. Public Health 2020, 17, 6800. https://doi.org/10.3390/ijerph17186800
Lewis ZH, Ottenbacher KJ, Fisher SR, Jennings K, Brown AF, Swartz MC, Martinez E, Lyons EJ. Effect of Electronic Activity Monitors and Pedometers on Health: Results from the TAME Health Pilot Randomized Pragmatic Trial. International Journal of Environmental Research and Public Health. 2020; 17(18):6800. https://doi.org/10.3390/ijerph17186800
Chicago/Turabian StyleLewis, Zakkoyya H., Kenneth J. Ottenbacher, Steve R. Fisher, Kristofer Jennings, Arleen F. Brown, Maria C. Swartz, Eloisa Martinez, and Elizabeth J. Lyons. 2020. "Effect of Electronic Activity Monitors and Pedometers on Health: Results from the TAME Health Pilot Randomized Pragmatic Trial" International Journal of Environmental Research and Public Health 17, no. 18: 6800. https://doi.org/10.3390/ijerph17186800
APA StyleLewis, Z. H., Ottenbacher, K. J., Fisher, S. R., Jennings, K., Brown, A. F., Swartz, M. C., Martinez, E., & Lyons, E. J. (2020). Effect of Electronic Activity Monitors and Pedometers on Health: Results from the TAME Health Pilot Randomized Pragmatic Trial. International Journal of Environmental Research and Public Health, 17(18), 6800. https://doi.org/10.3390/ijerph17186800






