Latent Health Risk Classes Associated with Poor Physical and Mental Outcomes in Workers with COPD from Central Appalachian U.S. States
Abstract
1. Introduction
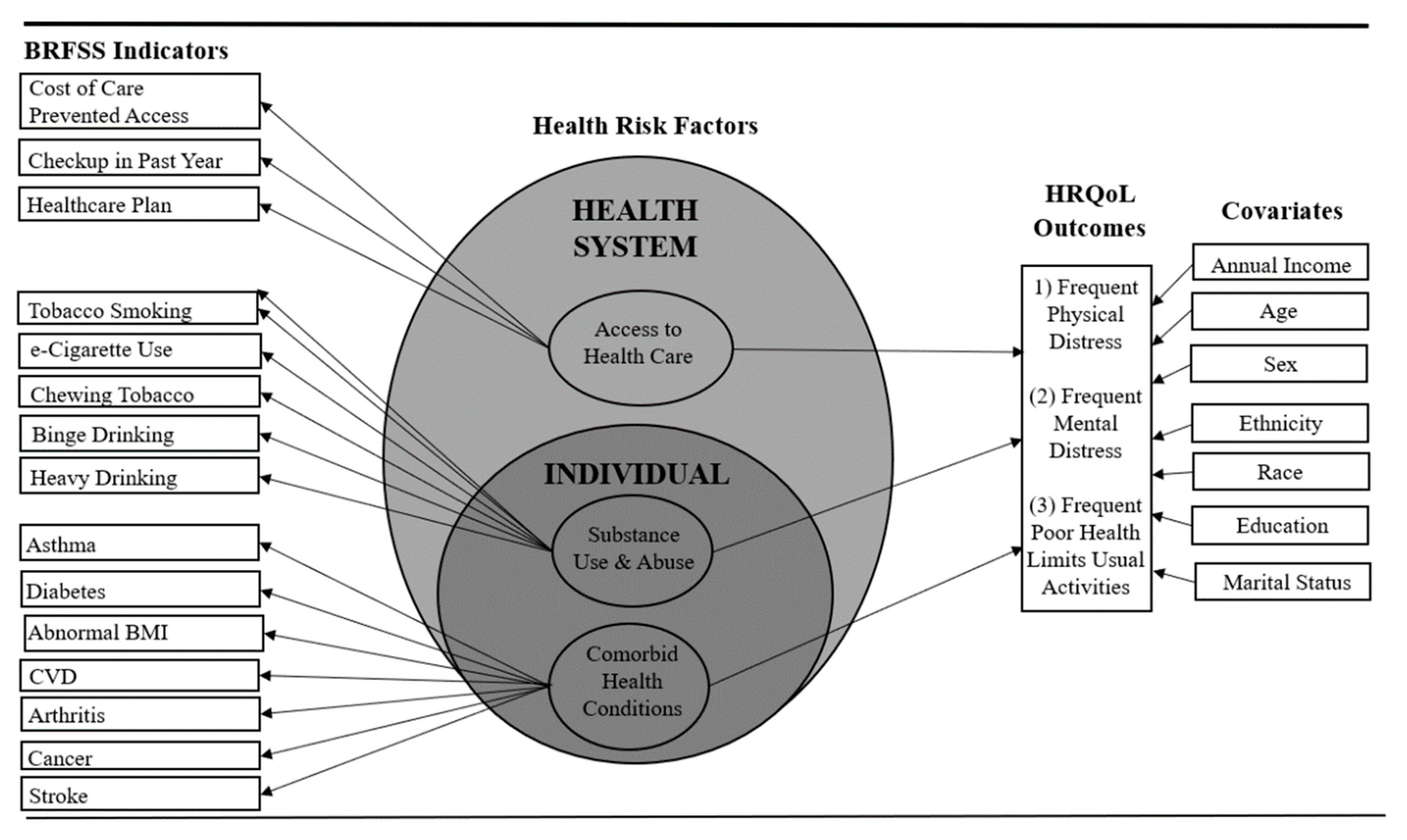
2. Materials and Methods
3. Results
3.1. Demographic Characteristics
3.2. Preliminary Logistic Regression Analyses
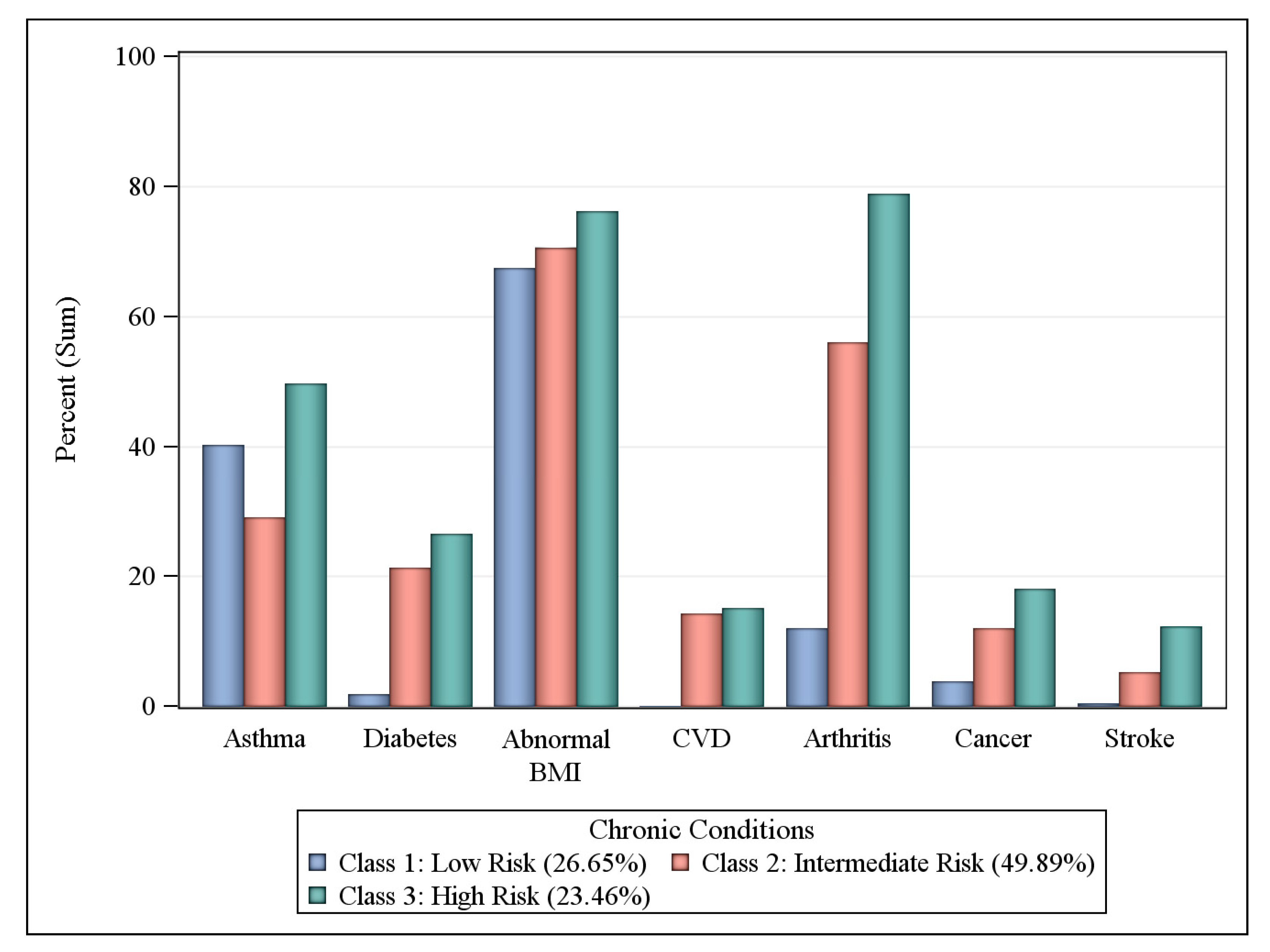
3.3. Comorbid Health Condition Risk Classes
3.4. Substance Use and Abuse Risk Classes
3.5. Health Care Access Risk Classes
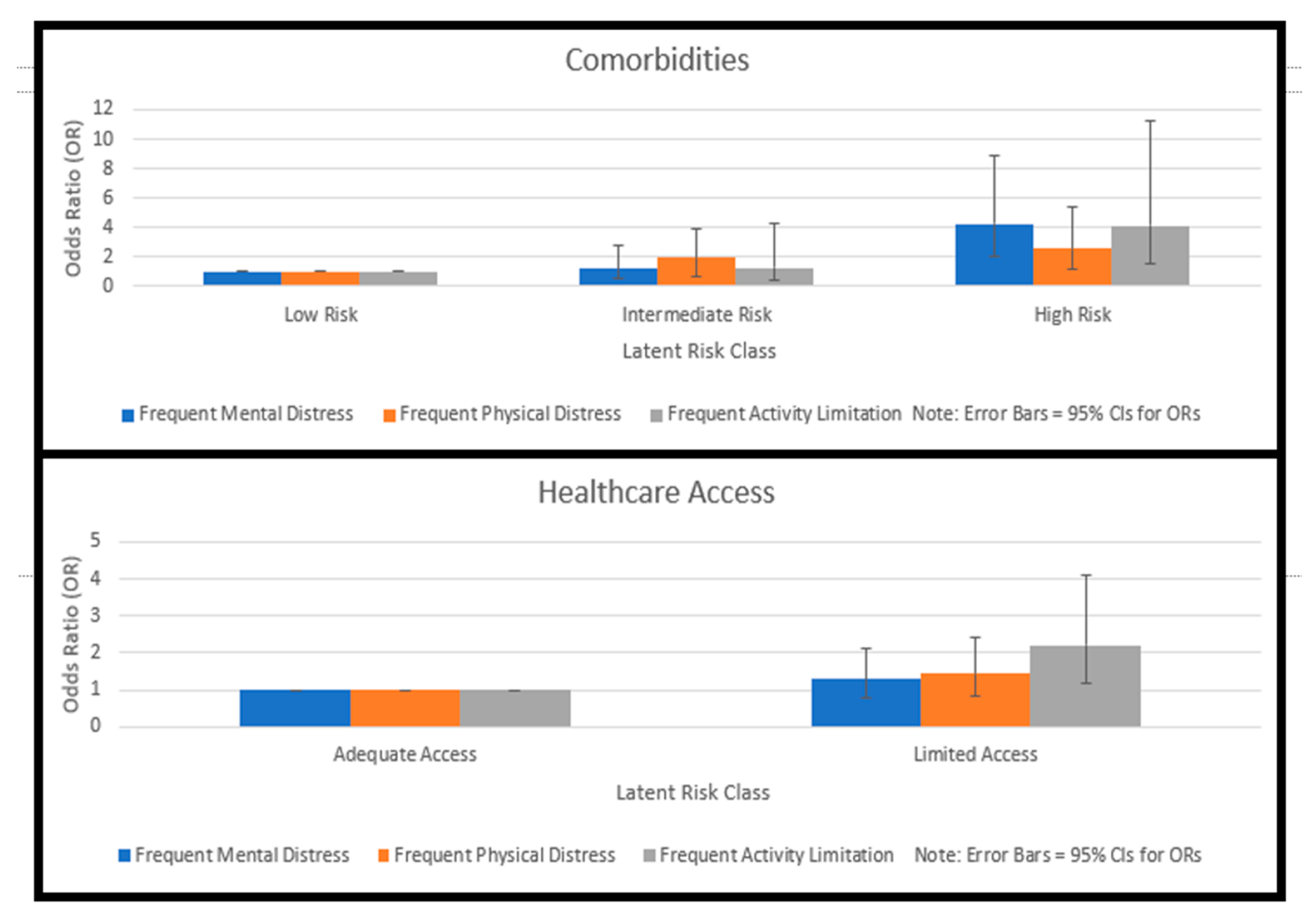
3.6. Influence of Risk Classes on HRQoL Outcomes
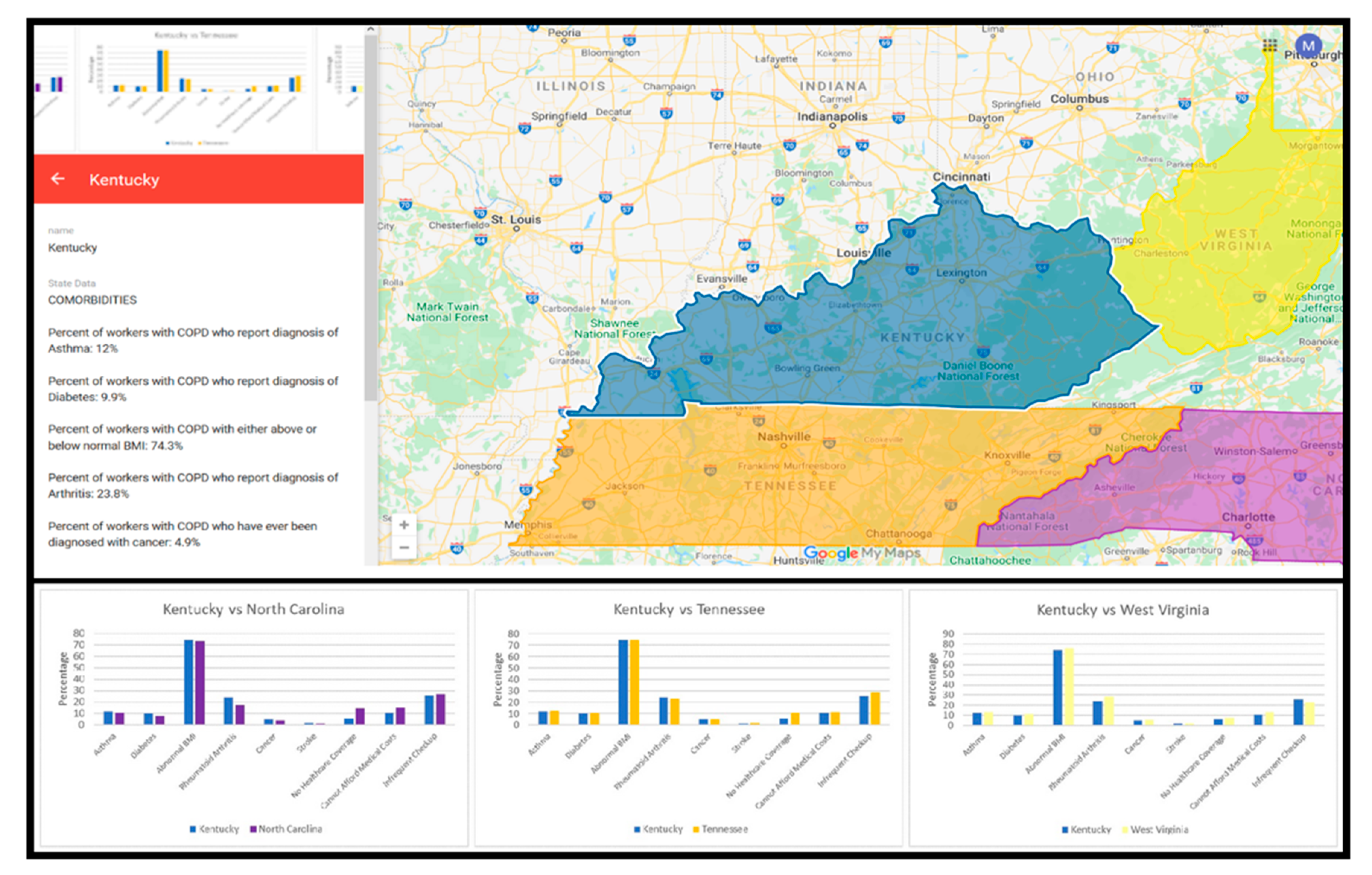
3.7. GIS Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Greenlund, K.J.; Liu, Y.; Deokar, A.J.; Wheaton, A.G.; Croft, J.B. Association of chronic obstructive pulmonary disease with increased confusion or memory loss and functional limitations among adults in 21 states, 2011 behavioral risk factor surveillance system. Prev. Chron. Dis. 2016, 13, 150428. [Google Scholar] [CrossRef] [PubMed]
- Wheaton, A.G.; Cunningham, T.J.; Ford, E.S.; Croft, J.B. Employment and activity limitations among adults with chronic obstructive pulmonary disease—United States, 2013. MMWR 2015, 64, 289–295. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4584881/ (accessed on 15 September 2020). [PubMed]
- Tselebis, A.; Pachi, A.; Ilias, I.; Kosmas, E.; Bratis, D.; Moussas, G.; Tzanakis, N. Strategies to improve anxiety and depression in patients with COPD: A mental health perspective. Neuropsychiatr. Dis. Treat. 2016, 12, 297–328. Available online: https://psycnet.apa.org/record/2016-07269-001 (accessed on 15 September 2020). [CrossRef] [PubMed]
- Maurer, J.; Rebbapragada, V.; Borson, S.; Goldstein, R.; Kunik, M.E.; Yohannes, A.M.; Hanania, N.A. Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest 2008, 134, 43S–56S. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Croft, J.B.; Mannino, D.M.; Wheaton, A.G.; Zhang, X.; Giles, W.H. COPD surveillance—United States, 1999–2011. Chest 2013, 144, 284–305. [Google Scholar] [CrossRef]
- Appalachian Regional Commission. Health disparities in Appalachia: COPD Mortality in Appalachia. Available online: https://www.arc.gov/assets/research_reports/Mortality_COPD.pdf (accessed on 11 August 2020).
- Appalachian Regional Commission. Health Disparities in Appalachia: Mortality. Creating a Culture of Health in Appalachia. Available online: https://www.arc.gov/assets/research_reports/Health_Disparities_in_Appalachia_Mortality_Domain.pdf (accessed on 11 August 2020).
- Raju, S.; Keet, C.A.; Paulin, L.M.; Matsui, E.C.; Peng, R.D.; Hansel, N.N.; McCormack, M.C. Rural residence and poverty are independent risk factors for chronic obstructive pulmonary disease in the United States. Am. J. Respir. Crit. Care Med. 2019, 199, 961–969. [Google Scholar] [CrossRef]
- Holt, J.B.; Zhang, X.; Presley-Cantrell, L.; Croft, J.B. Geographic disparities in chronic obstructive pulmonary disease (COPD) hospitalization among medicare beneficiaries in the United States. Int. J. Chron. Obs. Pulmon. Dis. 2011, 6, 321–328. [Google Scholar] [CrossRef]
- Horsley, N.; Slavova, S.; Bunn, T.; Sanderson, W.T. Occupational exposure to airborne particulate matter and its effects on chronic obstructive pulmonary disease in Kentucky. Am. J. Respir. Crit Care Med. 2020, 201, A4917. [Google Scholar] [CrossRef]
- Balmes, J.; Becklake, M.; Blanc, P.; Henneberger, P.; Kreiss, K.; Mapp, C. American thoracic society statement: Occupational contribution to the burden of airway disease. Am. J. Resp. Crit Care Med. 2003, 167, 787–797. [Google Scholar]
- Hnizdo, E.; Sullivan, P.A.; Bang, K.M.; Wagner, G. Association between chronic obstructive pulmonary disease and employment by industry and occupation in the US population: A study of data from the third national health and nutrition examination survey. Am. J. Epidemiol. 2002, 156, 738–746. [Google Scholar] [CrossRef]
- Bepko, J.; Mansalis, K. Common occupational disorders: Asthma, COPD, dermatitis, and musculoskeletal disorders. Am. Fam. Physician 2016, 93, 1000C–1006C. [Google Scholar]
- DiBonaventura, M.; Paulose-Ram, R.; Su, J.; McDonald, M.; Zou, K.H.; Wagner, J.S.; Shah, H. The impact of COPD on quality of life, productivity loss, and resource use among the elderly United States workforce. COPD 2012, 9, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Boschetto, P.; Quintavalle, S.; Miotto, D.; Cascio, N.L.; Zeni, E.; Mapp, C.E. Chronic obstructive pulmonary disease (COPD) and occupational exposures. J. Occup. Med. Toxicol. 2006, 1, 1–11. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Blanc, P.D. Occupation and COPD: A brief review. J. Asthma 2012, 49, 2–4. [Google Scholar] [CrossRef] [PubMed]
- van der Molen, H.F.; de Groene, G.J.; Hulshof, C.T.J.; Frings-Dresen, M.H.W. Association between work and chronic obstructive pulmonary disease (COPD). J. Clin. Med. 2018, 7, 335. [Google Scholar] [CrossRef]
- Liu, Y.; Lee, K.; Perez-Padilla, R.; Hudson, N.L.; Mannino, D.M. Outdoor and indoor air pollution and COPD-related diseases in high- and low-income countries. Int. J. Tuberc. Lung Dis. 2008, 12, 115–127. [Google Scholar]
- Mackenbach, J.P.; Stronks, K.; Kunst, A.E. The contribution of medical care to inequalities in health: Differences between socio-economic groups in decline of mortality from conditions amenable to medical intervention. Soc. Sci. Med. 1989, 29, 369–376. [Google Scholar] [CrossRef]
- Liu, Y.; Wheaton, A.G.; Murphy, L.B.; Xu, F.; Croft, J.B.; Greenlund, K.J. Chronic obstructive pulmonary disease and arthritis among US adults, 2016. Prev. Chronic Dis. 2019, 16, E93. [Google Scholar] [CrossRef]
- Kiley, J.P.; Gibbons, G.H. COPD national action plan: Addressing a public health need together. Chest 2017, 152, 698–699. Available online: https://journal.chestnet.org/article/S0012-3692(17)32673-9/abstract (accessed on 15 September 2020). [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q 1988, 15, 351–377. [Google Scholar] [CrossRef]
- McDaniel, J.T. Prevalence of chronic obstructive pulmonary disease: County-level risk factors based on the social ecological model. Perspect. Public Health 2018, 138, 200–208. [Google Scholar] [CrossRef] [PubMed]
- National Center for Chronic Disease Prevention and Health Promotion (U.S.). Measuring Healthy Days: Population Assessment of Health-Related Quality of Life [PDF File]. Available online: https://www.cdc.gov/hrqol/pdfs/mhd.pdf (accessed on 11 August 2020).
- Fontana, L.; Lee, S.; Capitanelli, I.; Re, A.; Maniscalco, M.; Mauriello, M.C.; Iavicoli, I. Chronic obstructive pulmonary disease in farmers: A systematic review. J. Occup. Environ. Med. 2017, 59, 775–788. [Google Scholar] [CrossRef]
- Trupin, L.; Earnest, G.; San Pedro, M.; Balmes, J.R.; Eisner, M.D.; Yelin, E.; Blanc, P.D. The occupational burden of chronic obstructive pulmonary disease. Eur. Respir. J. 2003, 22, 462–469. [Google Scholar] [CrossRef]
- Stellefson, M.; Paige, S.R.; Barry, A.; Wang, M.Q.; Apperson, A. Risk factors associated with physical and mental distress in people who report a COPD diagnosis: Latent class analysis of 2016 behavioral risk factor surveillance system data. Int. J. Chron. Obs. Pulmon. Dis. 2019, 14, 809–822. [Google Scholar] [CrossRef] [PubMed]
- Spruit, M.A.; Pitta, F.; McAuley, E.; ZuWallack, R.L.; Nici, L. Pulmonary rehabilitation and physical activity in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2015, 192, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Dransch, D.; Rotzoll, H.; Poser, K. The contribution of maps to the challenges of risk communication to the public. Int. J. Digit. Earth 2010, 3, 292–311. [Google Scholar] [CrossRef]
- Stokols, D. Translating social ecological theory into guidelines for community health promotion. Am. J. Health Promot. 1996, 10, 282–298. [Google Scholar] [CrossRef]
- Jiang, Y.; Zack, M.M. A latent class modeling approach to evaluate behavioral risk factors and health-related quality of life. Prev. Chron. Dis. 2011, 8, A137. Available online: http://www.cdc.gov/pcd/issues/2011/nov/10_0296.htm (accessed on 15 September 2020).
- Li, C.; Ford, E.S.; Mokdad, A.H.; Balluz, L.S.; Brown, D.W.; Giles, W.H. Clustering of cardiovascular disease risk factors and health-related quality of life among US adults. Value Health 2008, 11, 689–699. [Google Scholar] [CrossRef]
- Bang, K.M.; Syamlal, G.; Mazurek, J.M. Prevalence of chronic obstructive pulmonary disease in the U.S. working population: Analysis of data from the 1997-2004 National Health Interview Survey. COPD 2009, 6, 380–387. [Google Scholar] [CrossRef]
- Croft, J.B.; Wheaton, A.G.; Liu, Y.; Xu, F.; Lu, H.; Matthews, K.A.; Holt, J.B. Urban-rural county and state differences in chronic obstructive pulmonary disease-United States, 2015. MMWR 2018, 67, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Monga, N.; Rehm, J.; Fischer, B.; Brissette, S.; Bruneau, J.; El-Guebaly, N.; Bahl, S. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007, 88, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wall, M.; Amemiya, Y. Latent class regression on latent factors. Biostatistics 2006, 7, 145–163. [Google Scholar] [CrossRef] [PubMed]
- Vermunt, J.; Magidson, J. Latent Class Cluster Analysis. In Applied Latent Class. Analysis; Hagenaars, J., McCutcheon, A., Eds.; Cambridge University Press: Cambridge, UK, 2002; pp. 89–106. [Google Scholar] [CrossRef]
- Henry, K.L.; Muthén, B. Multilevel latent class analysis: An application of adolescent smoking typologies with individual and contextual predictors. Struct. Equ. Model. 2010, 17, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Vitality. Britain’s Healthiest Workplace: 2018 Findings. Available online: https://www.vitality.co.uk/business/healthiest-workplace/findings/ (accessed on 11 August 2020).
- Accenture. It’s Not 1 in 4, It’s All of Us: Why Supporting the Mental Health of Younger Workers Starts with Organizational Culture. Available online: https://www.accenture.com/_acnmedia/PDF-112/Accenture-Its-Not-1-4-Brochure (accessed on 11 August 2020).
- Xiao, T.; Qiu, H.; Chen, Y.; Zhou, X.; Wu, K.; Ruan, X.; Wang, N.; Fu, C. Prevalence of anxiety and depression symptoms and their associated factors in mild COPD patients from community settings, Shanghai, China: A cross-sectional study. BMC Psychiatry 2018, 18, 89. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Freeman, J. The Stressed Sex: Uncovering the Truth about Men, Women, and Mental Health, 1st ed.; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- McManus, S.; Meltzer, H.; Brugha, T.; Bebbington, P.E.; Jenkins, R. Adult Psychiatric Morbidity in England: Results of a Household Survey; Health and Social Care Information Centre: Leeds, UK, 2009; Available online: https://openaccess.city.ac.uk/id/eprint/23647/1/ (accessed on 15 September 2020).
- Ohayon, M. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med. Rev. 2002, 6, 97–111. [Google Scholar] [CrossRef]
- Chandra, P.S.; Saraf, G.; Bajaj, A.; Satyanarayana, V.A. The current status of gender-sensitive mental health services for women–findings from a global survey of experts. Arch. Womens Ment. Health 2019, 22, 759–770. [Google Scholar] [CrossRef]
- Williams, D.R.; Yu, Y.; Jackson, J.S.; Anderson, N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J. Health Psychol. 1997, 2, 335–351. [Google Scholar] [CrossRef]
- Neighbors, H.W.; Sellers, S.L.; Zhang, R.; Jackson, J.S. Goal-striving stress and racial differences in mental health. Race Soc. Probl. 2011, 3, 51–62. [Google Scholar] [CrossRef]
- Kessler, R.C. Stress, social status, and psychological distress. J. Health Soc. Behav. 1979, 20, 259–272. [Google Scholar] [CrossRef]
- Kocabas, A.; Ozyilmas, E. The effects of socioeconomic status on health outcomes in patients with COPD. Eur. Resp. J. 2016, 48, PA1030. [Google Scholar] [CrossRef]
- Mirowsky, J.; Ross, C.E. Education, Social Status, and Health; Aldine De Gruyter: New York, NY, USA, 2003. [Google Scholar]
- Dohrenwend, B.P.; Levav, I.; Shrout, P.E.; Schwartz, S.; Naveh, G.; Link, B.G.; Skodol, A.E.; Stueve, A. Socioeconomic status and psychiatric disorders: The causation-selection issue. Science 1992, 255, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Bracke, P.; van de Straat, V.; Missinne, S. Education, mental health, and education-labor market misfit. J. Health Soc. Behav. 2014, 55, 442–459. [Google Scholar] [CrossRef] [PubMed]
- Goesling, B. The rising significance of education for health? Soc. Forces 2007, 85, 1621–1644. [Google Scholar] [CrossRef]
- Miech, R.; Pampel, F.; Kim, J.; Rogers, R.G. The enduring association between education and mortality: The role of widening and narrowing disparities. Am. Soc. Rev. 2011, 76, 913–934. [Google Scholar] [CrossRef]
- Mirowsky, J.; Ross, C.E. Education and self-rated health cumulative advantage and its rising importance. Res. Aging 2008, 30, 93–122. [Google Scholar] [CrossRef]
- Subramanian, S.V.; Huijts, T.; Avendano, M. Self-reported health assessments in the 2002 world health survey: How do they correlate with education? B World Health Organ. 2010, 88, 131–138. [Google Scholar] [CrossRef]
- Pascal, O.I.; Trofor, A.C.; Lotrean, L.M.; Filipeanu, D.; Trofor, L. Depression, anxiety and panic disorders in chronic obstructive pulmonary disease patients: Correlations with tobacco use, disease severity and quality of life. Tob. Induc. Dis. 2017, 15, 23. [Google Scholar] [CrossRef]
- Hillas, G.; Perlikos, F.; Tsiligianni, I.; Tzanakis, N. Managing comorbidities in COPD. Int. J. Chron. Obs. Pulmon. Dis. 2015, 10, 95–109. [Google Scholar] [CrossRef]
- Dhamane, A.D.; Witt, E.A.; Su, J. Associations between COPD severity and work productivity, health-related quality of life, and health care resource use: A cross-sectional analysis of national survey data. JOEM 2016, 58, e191–e197. [Google Scholar] [CrossRef]
- Li, Y.R.; Gibson, J.M. Health and air quality benefits of policies to reduce coal-fired power plant emissions: A case study in North Carolina. Environ. Sci. Technol. 2014, 48, 10019–10027. [Google Scholar] [CrossRef] [PubMed]
- Kravchenko, J.; Akushevich, I.; Abernethy, A.P.; Holman, S.; Ross, W.G., Jr.; Lyerly, H.K. Long-term dynamics of death rates of emphysema, asthma, and pneumonia and improving air quality. Int. J. Chron. Obs. Pulmon. Dis. 2014, 9, 613–627. [Google Scholar] [CrossRef] [PubMed]


| Demographic Characteristic | No of Employed Adults with COPD 1, n = 1326 (% 2) | Frequent Mental Distress, % (95% CI) 2 n = 261 (19.68%) | Frequent Physical Distress, % (95% CI) 2 n = 278 (20.97%) | Frequent Usual Activity Limitation, % (95% CI) 2 n = 148 (11.16%) |
|---|---|---|---|---|
| Age | ||||
| 18–44 years | 379 (28.6) | 42.9 (36.9, 48.9) | 29.1 (23.8, 34.5) | 28.4 (21.1, 35.7) |
| 45–64 years | 736 (55.5) | 49.8 (43.7, 55.9) | 57.2 (51.4, 63.0) | 58.1 (50.1, 66.1) |
| ≥65 years | 211 (15.9) | 7.3 (4.1, 10.4) | 13.7 (9.6, 17.7) | 13.5 (8.0, 19.0) |
| Sex | ||||
| Male | 566 (42.7) | 33.3 (27.6, 39.1) | 39.6 (33.8, 45.3) | 37.2 (29.4, 45.0) |
| Female | 760 (57.3) | 66.7 (60.9, 70.4) | 60.4 (54.7, 66.2) | 62.8 (55.0, 70.6) |
| Race | ||||
| White | 1155 (87.1) | 89.9 (86.2, 93.6) | 87.3 (83.4, 91.2) | 89.8 (84.9, 94.7) |
| Black or African American | 106 (8.0) | 5.4 (2.7, 8.2) | 9.1 (5.7, 12.4) | 4.8 (1.3, 8.2) |
| American Indian or Alaskan Native | 53 (4.0) | 4.7 (2.1, 7.2) | 3.6 (1.4, 5.8) | 5.4 (1.8, 9.1) |
| Hispanic | ||||
| Yes | 30 (2.3) | 3.1 (1.0, 5.2) | 2.2 (0.4, 3.9) | 2.7 (0.1, 5.3) |
| No | 1290 (97.3) | 96.9 (94.8, 99.0) | 97.8 (96.1, 99.6) | 97.3 (94.7, 99.9) |
| Education | ||||
| <High school degree | 148 (11.2) | 13.8 (9.6, 18.0) | 13.0 (9.0, 16.7) | 18.2 (12.0, 24.5) |
| Grade 12 or GED | 524 (39.5) | 40.6 (34.6, 46.6) | 37.9 (32.2, 43.6) | 32.4 (24.9, 40.0) |
| College 1–3 years | 392 (29.6) | 33.7 (28.0, 39.5) | 35.7 (30.1, 41.4) | 37.8 (30.0, 45.7) |
| College ≥4 years | 258 (19.5) | 11.9 (7.9, 15.8) | 13.4 (9.3, 17.4) | 11.5 (6.3, 16.6) |
| Annual Income | ||||
| USD <20,000 | 232 (17.5) | 30.9 (24.9, 36.8) | 30.0 (24.2, 35.8) | 32.0 (23.8, 40.2) |
| USD 20,000–34,999 | 316 (23.8) | 31.3 (25.3, 37.3) | 27.9 (22.2, 33.6) | 29.6 (21.6, 37.6) |
| USD 35,000–49,999 | 211 (15.9) | 14.3 (9.8, 18.9) | 16.7 (11.9, 21.4) | 16.00 (9.6, 22.4) |
| USD 50,000–74,999 | 184 (13.9) | 12.2 (7.9, 16.4) | 12.9 (8.7, 17.2) | 10.4 (5.0, 15.8) |
| USD ≥75,000 | 213 (16.1) | 11.3 (7.2, 15.4) | 12.5 (8.3, 16.7) | 12.0 (6.3, 17.7) |
| Marital Status | ||||
| Married | 629 (47.4) | 40.4 (34.4, 46.4) | 43.8 (37.8, 49.7) | 41.8 (33.8, 49.8) |
| Divorced | 292 (22.0) | 25.0 (19.7, 30.0) | 25.7 (20.6, 30.9) | 23.3 (16.4, 30.2) |
| Widowed | 126 (9.5) | 8.5 (5.1, 11.8) | 9.8 (6.3, 13.3) | 16.4 (10.4, 22.5) |
| Separated | 42 (3.2) | 2.7 (0.7, 4.7) | 3.3 (1.2, 5.4) | 2.7 (0.1, 5.4) |
| Never married | 187 (14.1) | 17.3 (12.7, 21.9) | 14.1 (10.0, 18.2) | 12.3 (7.0, 17.7) |
| Unmarried couple | 45 (3.4) | 6.2 (3.2, 9.1) | 3.3 (1.2, 5.4) | 3.4 (0.5, 6.4) |
| Health Risk Domain | Frequent Mental Distress | Frequent Physical Distress | Frequent Activity Limitation | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Substance Use and Abuse | ||||||
| Low Risk (n = 300) | 1.00 2 | ref | 1.00 2 | ref | 1.00 2 | ref |
| Intermediate Risk (n = 347) | 0.90 | 0.42, 1.94 | 1.02 | 0.53, 1.95 | 0.71 | 0.29, 1.75 |
| High Risk (n = 482) | 1.23 | 0.67, 2.29 | 1.35 | 0.77, 2.37 | 0.69 | 0.33, 1.44 |
| Comorbidities | ||||||
| Low Risk (n = 316) | 1.00 2 | ref | 1.00 2 | ref | 1.00 2 | ref |
| Intermediate Risk (n = 545) | 1.21 | 0.53, 2,74 | 1.69 | 0.73, 3.90 | 1.28 | 0.39, 4.23 |
| High Risk (n = 282) | 4.25 ** | 2.03, 8.89 | 2.54 * | 1.19, 5.41 | 4.15 ** | 1.53, 11.29 |
| Healthcare Access | ||||||
| Adequate Access (n = 1093) | 1.00 2 | ref | 1.00 2 | ref | 1.00 2 | ref |
| Limited Access (n = 233) | 1.28 | 0.77, 2.11 | 1.43 | 0.84, 2.43 | 2.22 ** | 1.19, 4.11 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stellefson, M.; Wang, M.Q.; Balanay, J.A.G.; Wu, R.; Paige, S.R. Latent Health Risk Classes Associated with Poor Physical and Mental Outcomes in Workers with COPD from Central Appalachian U.S. States. Int. J. Environ. Res. Public Health 2020, 17, 6798. https://doi.org/10.3390/ijerph17186798
Stellefson M, Wang MQ, Balanay JAG, Wu R, Paige SR. Latent Health Risk Classes Associated with Poor Physical and Mental Outcomes in Workers with COPD from Central Appalachian U.S. States. International Journal of Environmental Research and Public Health. 2020; 17(18):6798. https://doi.org/10.3390/ijerph17186798
Chicago/Turabian StyleStellefson, Michael, Min Qi Wang, Jo Anne G. Balanay, Rui Wu, and Samantha R. Paige. 2020. "Latent Health Risk Classes Associated with Poor Physical and Mental Outcomes in Workers with COPD from Central Appalachian U.S. States" International Journal of Environmental Research and Public Health 17, no. 18: 6798. https://doi.org/10.3390/ijerph17186798
APA StyleStellefson, M., Wang, M. Q., Balanay, J. A. G., Wu, R., & Paige, S. R. (2020). Latent Health Risk Classes Associated with Poor Physical and Mental Outcomes in Workers with COPD from Central Appalachian U.S. States. International Journal of Environmental Research and Public Health, 17(18), 6798. https://doi.org/10.3390/ijerph17186798







