Elucidating Mental Health Disorders among Rohingya Refugees: A Malaysian Perspective
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sampling Strategy
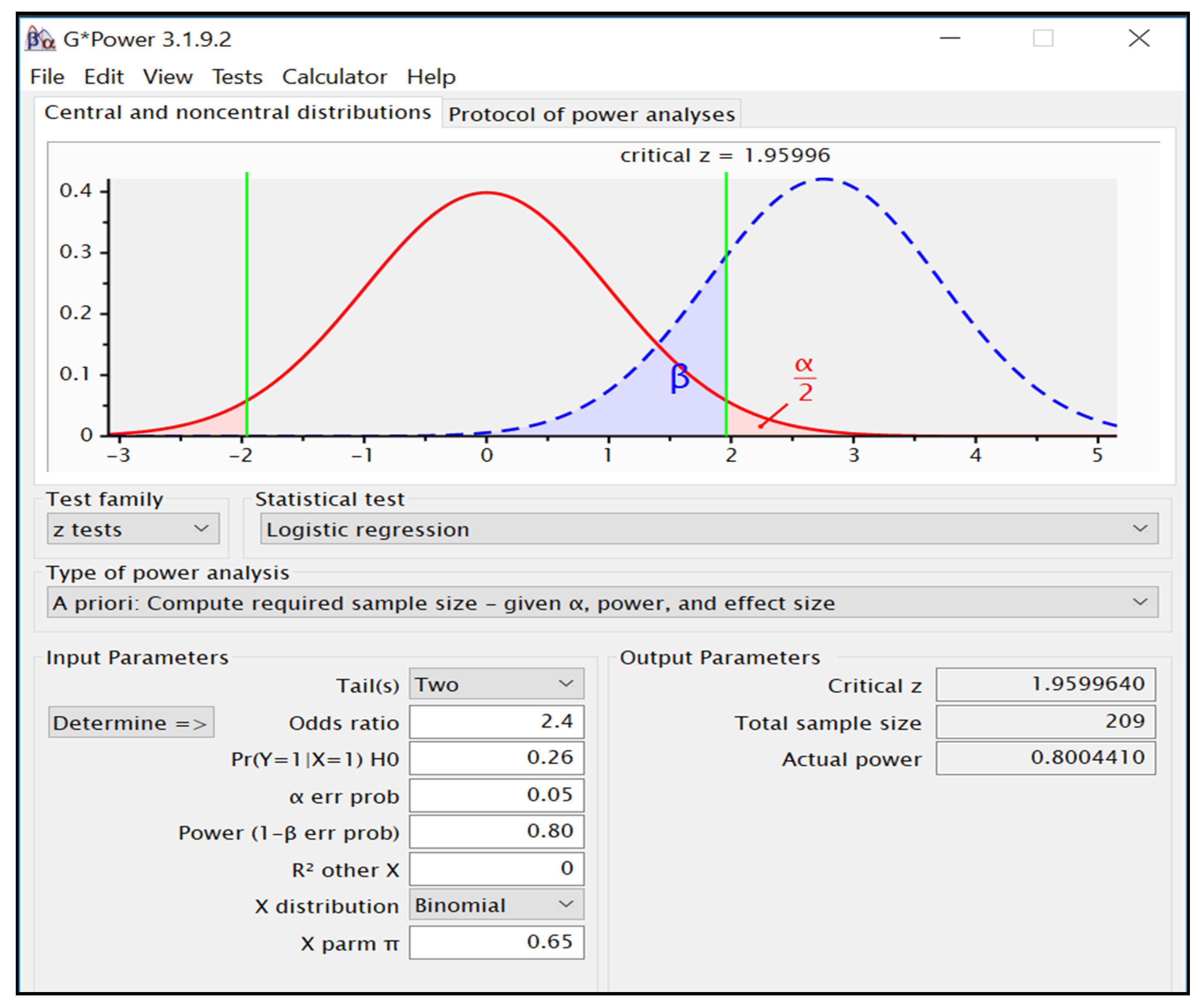
2.3. Sample Size Calculation
2.4. Data Collection
2.5. Measures
2.6. Analytic Approach
2.7. Ethics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B. Test of Multicollinearity
| Gender | Time in Malaysia | Physically Injured | Social Support | Food Security | Exposure to Violence | Employment | Education | |
|---|---|---|---|---|---|---|---|---|
| Gender | 0.144 | 0.298 | 0.056 | 0.135 | 0.090 | 0.631 | 0.270 | |
| Time in Malaysia | 0.144 | 0.030 | 0.116 | 0.069 | 0.182 | 0.177 | 0.103 | |
| Physically injured | 0.298 | 0.030 | 0.162 | 0.295 | 0.463 | 0.132 | 0.126 | |
| Social Support | 0.056 | 0.116 | 0.162 | 0.192 | 0.043 | 0.013 | 0.154 | |
| Food Security | 0.135 | 0.069 | 0.295 | 0.192 | 0.195 | 0.120 | 0.123 | |
| Exposure to violence | 0.090 | 0.182 | 0.463 | 0.043 | 0.195 | 0.010 | 0.036 | |
| Employment | 0.631 | 0.177 | 0.132 | 0.013 | 0.120 | 0.010 | 0.169 | |
| Education | 0.270 | 0.103 | 0.126 | 0.154 | 0.123 | 0.036 | 0.169 |
| Marital Status | Time in Malaysia | Physically Injured | Education | |
|---|---|---|---|---|
| Marital status | 0.153 | 0.172 | 0.149 | |
| Time in Malaysia | 0.153 | 0.030 | 0.103 | |
| Physically injured | 0.172 | 0.030 | 0.126 | |
| Education | 0.149 | 0.103 | 0.126 |
| Gender | Age (Years) | Separation from Family Members | Exposure to Violence | Physical Injuries | Food Security | |
|---|---|---|---|---|---|---|
| Gender | 0.125 | 0.401 | 0.090 | 0.298 | 0.135 | |
| Age (years) | 0.125 | 0.246 | 0.106 | 0.129 | 0.090 | |
| Separation from family members | 0.401 | 0.246 | 0.122 | 0.298 | 0.033 | |
| Exposure to violence | 0.090 | 0.106 | 0.122 | 0.463 | 0.195 | |
| Physical injuries | 0.298 | 0.129 | 0.298 | 0.463 | 0.295 | |
| Food security | 0.135 | 0.090 | 0.033 | 0.195 | 0.295 |
References
- Letchamanan, H. Myanmar’s Rohingya refugees in Malaysia: Education and the way forward. J. Int. Comp. Educ. 2013, 2, 86–97. [Google Scholar] [CrossRef]
- United Nations High Commissioner for Refugees (UNHCR). Figures at a Glance in Malaysia. 2020, p. 1. Available online: https://www.unhcr.org/en-my/figures-at-a-glance.html (accessed on 17 March 2020).
- Huennekes, J. Emotional remittances in the transnational lives of Rohingya families living in Malaysia. J. Refug. Stud. 2018, 31, 353–370. [Google Scholar] [CrossRef]
- Turrini, G.; Purgato, M.; Ballette, F.; Nosè, M.; Ostuzzi, G.; Barbui, C. Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. Int. J. Ment. Health Syst. 2017, 11, 51. [Google Scholar] [CrossRef] [PubMed]
- Shaw, S.A.; Pillai, V.; Ward, K.P. Assessing mental health and service needs among refugees in Malaysia. Int. J. Soc. Welfare. 2018, 28, 44–45. [Google Scholar] [CrossRef]
- Riley, A.; Varner, A.; Ventevogel, P.; Taimur Hasan, M.M.; Welton-Mitchell, C. Daily stressors, trauma exposure, and mental health among stateless Rohingya refugees in Bangladesh. Transcult Psychiatr. 2017, 54, 304–331. [Google Scholar] [CrossRef] [PubMed]
- Kirmayer, L.J.; Narasiah, L.; Munoz, M.; Rashid, M.; Ryder, A.G.; Guzder, J.; Hassan, G.; Rousseau, C.; Pottie, K. Common mental health problems in immigrants and refugees: General approach in primary care. CMAJ 2011, 183, 959–967. [Google Scholar] [CrossRef] [PubMed]
- UNHCR. Culture, Context and Mental Health of Rohingya Refugees: A Review for Staff in Mental Health and Psychosocial Support Programmes for Rohingya Refugees. Geneva, Switzerland, United Nations High Commissioner for Refugees (UNHCR). 2018. Available online: https://www.unhcr.org/5bbc6f014.pdf (accessed on 30 January 2020).
- Gosnell, N.M. Mental Health and Emotion Regulation among Refugee Students in Malaysia. Master’s Thesis, The University of Maryland, Washington, DC, USA, 2017. Available online: https://drum.lib.umd.edu/handle/1903/19268 (accessed on 30 January 2020).
- Low, S.K.; Tan, S.A.; Kok, J.K.; Nainee, S.; Viapude, G.N. The mental health of adolescent refugees in Malaysia people. Int. J. Soc. Sci. 2018, 4, 428–439. [Google Scholar]
- Tay, A.K.; Rees, S.; Miah, M.A.; Khan, S.; Badrudduza, M.; Morgan, K.; Azim, D.F.; Balasundaram, S.; Silove, D. Functional impairment as a proxy measure indicating high rates of trauma exposure, post-migration living difficulties, common mental disorders, and poor health amongst Rohingya refugees in Malaysia. Transl. Psychiatr. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Welton-Mitchell, C.; Bujang, N.A.; Hussin, H.; Husein, S.; Santoadi, F.; James, L.E. Intimate partner abuse among Rohingya in Malaysia: Assessing stressors, mental health, social norms and help-seeking to inform interventions. Intervention 2019, 17, 187–196. [Google Scholar] [CrossRef]
- Erdfelder, E.; Faul, F.; Lang, A.-G.; Buchner, A. Statistical power analyses using G * Power 3.1. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar]
- Feyera, F.; Mihretie, G.; Bedaso, A.; Gedle, D.; Kumera, G. Prevalence of depression and associated factors among Somali refugee at melkadida camp, southeast Ethiopia: A cross-sectional study. BMC Psychiatr. 2015, 15, 171. [Google Scholar] [CrossRef]
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 1–8. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Ng, C.G.; Amer Siddiq, A.N.; Aida, S.A.; Zainal, N.Z.; Koh, O.H. Validation of the Malay version of the Multidimensional Scale of Perceived Social Support (MSPSS-M) among a group of medical students in Faculty of Medicine, University Malaya. Asian J. Psychiatr. 2010, 3, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Gorsuch, R.L.; McPherson, S.E. Intrinsic/extrinsic measurement: I/E-Revised and single-item scales. J. Sci. Study Relig. 1989, 28, 348–352. [Google Scholar] [CrossRef]
- Kamaluddin, M.R.; Nasir, R.; Wan Sulaiman, W.S.; Khairudin, R.; Ahmad Zamani, Z. Validity and psychometric properties of Malay translated religious orientation scale-revised among Malaysian adult samples. Akademika 2017, 87, 133–144. [Google Scholar] [CrossRef]
- Radimer, K.; Olson, C.; Campbell, C. Development of indicators to assess hunger. J. Nutr. 1990, 120, 1544–1548. [Google Scholar] [CrossRef]
- Kendall, A.; Olson, C.M.; Frongillo, E.A. Relationship of hunger and food insecurity to food availability and consumption. J. Am. Diet. Assoc. 1996, 96, 1019–1024. [Google Scholar] [CrossRef]
- Zalilah, M.S.; Merlin, A. Assessment of food insecurity among low income households in kuala lumpur using the radimer/cornell food insecurity instrument—A validation study. Malays. J. Nutr. 2001, 7, 15–32. [Google Scholar]
- Lecrubier, Y.; Sheehan, D.V.; Weiller, E.; Amorim, P.; Bonora, I.; Sheehan, K.H.; Janavs, J.; Dunbar, G.C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatr. 1997, 12, 224–231. [Google Scholar] [CrossRef]
- International Business Machines (IBM) Corporation. IBM SPSS Statistics for Windows, Version 24.0.; IBM: Armonk, NY, USA, 2016; Available online: http://www-01.ibm.com/support/docview.wss?uid=swg21476197 (accessed on 30 January 2020).
- Craig, C.D.; Sossou, M.A.; Schnak, M.; Essex, H. Complicated grief and its relationship to mental health and well-being among Bosnian refugees after resettlement in the United States: Implications for practice, policy, and research. Traumatology 2008, 14, 103–115. [Google Scholar] [CrossRef]
- Bogic, M.; Ajdukovic, D.; Bremner, S.; Franciskovic, T.; Galeazzi, G.M.; Kucukalic, A.; Lecic-Tosevski, D.; Morina, N.; Popovski, M.; Schützwohl, M. Factors associated with mental disorders in long-settled war refugees: Refugees from the former Yugoslavia in Germany, Italy and the UK. Br. J. Psychiatr. 2012, 200, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Coffey, G.J.; Kaplan, I.; Sampson, R.C.; Tucci, M.M. The meaning and mental health consequences of long-term immigration detention for people seeking asylum. Soc. Sci. Med. 2010, 70, 2070–2079. [Google Scholar] [CrossRef] [PubMed]
- Keller, A.S.; Rosenfeld, B.; Trinh-Shevrin, C.; Meserve, C.; Sachs, E.; Leviss, J.A.; Singer, E.; Smith, H.; Wilkinson, J.; Kim, G.; et al. Mental health of detained asylum seekers. Lancet 2003, 362, 1721–1723. [Google Scholar] [CrossRef]
- Lindert, J.; von Ehrenstein, O.S.; Priebe, S.; Mielck, A.; Brähler, E. Depression and anxiety in labor migrants and refugees—A systematic review and meta-analysis. Soc. Sci. Med. 2009, 69, 246–257. [Google Scholar] [CrossRef]
- Carlson, E.B.; Rosser-Hogan, R. Cross-cultural response to trauma: A study of traumatic experiences and posttraumatic symptoms in Cambodian refugees. J. Trauma Stress. 1994, 7, 43–58. [Google Scholar] [CrossRef]
- Sabin, M.; Cardozo, B.L.; Nackerud, L.; Kaiser, R.; Varese, L. Factors associated with poor mental health among Guatemalan Refugees living in Mexico 20 years after civil conflict. J. Am. Med. Assoc. 2003, 290, 635–642. [Google Scholar] [CrossRef]
- Quosh, C.; Eloul, L.; Ajlani, R. Mental health of refugees and displaced persons in Syria and surrounding countries: A systematic review. Intervention 2013, 11, 276–294. [Google Scholar] [CrossRef]
- Onyut, L.P.; Neuner, F.; Ertl, V.; Schauer, E.; Odenwald, M.; Elbert, T. Trauma, poverty and mental health among Somali and Rwandese refugees living in an African refugee settlement—An epidemiological study. Confl. Health. 2009, 3, 6. [Google Scholar] [CrossRef]
- De Jong, J.T.V.M.; Komproe, I.H.; Van Ommeren, M.; El Masri, M.; Araya, M.; Khaled, N.; van De Put, W.; Somasundaram, D. Lifetime events and posttraumatic stress disorder in 4 postconflict settings. J. Am. Med. Assoc. 2001, 286, 555–562. [Google Scholar] [CrossRef]
- Robjant, K.; Robbins, I.; Senior, V. Psychological distress amongst immigration detainees: A cross-sectional questionnaire study. Br. J. Clin. Psychol. 2009, 48, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Mollica, R.F. The effect of trauma and confinement on functional health and mental health status of Cambodians living in Thailand-Cambodia border camps. J. Am. Med. Assoc. 1993, 270, 581–586. [Google Scholar] [CrossRef]
- Mugisha, J.; Muyinda, H.; Wandiembe, P.; Kinyanda, E. Prevalence and factors associated with Posttraumatic Stress Disorder seven years after the conflict in three districts in northern Uganda (The Wayo-Nero Study). BMC Psychiatr. 2015, 15, 170. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, H.N.; Ibrahim, H.; Goessmann, K.; Ismail, A.A.; Neuner, F. Post-Traumatic stress disorder and depression among Syrian refugees residing in the Kurdistan region of Iraq. Confl. Health. 2019, 13, 51. [Google Scholar] [CrossRef]
- Gerritsen, A.A.M.; Bramsen, I.; Devillé, W.; van Willigen, L.H.M.; Hovens, J.E.; van der Ploeg, H.M. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc. Psychiatr. Psychiatr. Epidemiol. 2006, 41, 18–26. [Google Scholar] [CrossRef]
- Blight, K.J.; Ekblad, S.; Persson, J.O.; Ekberg, J. Mental health, employment and gender. Cross-sectional evidence in a sample of refugees from Bosnia-Herzegovina living in two Swedish regions. Soc. Sci. Med. 2006, 62, 1697–1709. [Google Scholar] [CrossRef]
- Adeniyi, A.F.; Okafor, N.C.; Adeniyi, C.Y. Depression and physical activity in a sample of nigerian adolescents: Levels, relationships and predictors. Child Adolesc. Psychiatr. Ment. Health 2011, 5, 16. [Google Scholar] [CrossRef]
- Hill, J.P.; Lynch, M.E. The intensification of gender-related role expectations during early adolescence. In Girls at Puberty; Brooks-Gunn, J., Petersen, A.C., Eds.; Springer: Boston, MA, USA, 1983; pp. 201–228. [Google Scholar]
- Steel, Z.; Silove, D.; Phan, T.; Bauman, A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. Lancet 2002, 360, 1056–1062. [Google Scholar] [CrossRef]
- Steel, Z.; Chey, T.; Silove, D.; Marnane, C.; Bryant, R.A.; Van Ommeren, M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. J. Am. Med. Assoc. 2009, 302, 537–549. [Google Scholar] [CrossRef]
- Schweitzer, R.; Melville, F.; Steel, Z.; Lacherez, P. Trauma, post-migration living difficulties, and social support as predictors of psychological adjustment in resettled Sudanese refugees. Aust. N. Z. J. Psychiatr. 2006, 40, 179–187. [Google Scholar] [CrossRef]
- Momartin, S.; Steel, Z.; Coello, M.; Aroche, J.; Silove, D.M.; Brooks, R. A comparison of the mental health of refugees with temporary versus permanent protection visas. Med. J. Aust. 2006, 185, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Silove, D.; Steel, Z.; McGorry, P.; Mohan, P. Trauma exposure, postmigration stressors, and symptoms of anxiety, depression and post-traumatic stress in Tamil asylum-seekers: Comparison with refugees and immigrants. Acta Psychiatr. Scand. 1998, 97, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, R.D.; Brough, M.; Vromans, L.; Asic-Kobe, M. Mental health of newly arrived Burmese refugees in Australia: Contributions of pre-migration and post-migration experience. Aust. N. Z. J. Psychiatr. 2011, 45, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.E.; Davidson, G.R.; Schweitzer, R.D. Review of refugee mental health interventions following resettlement: Best practices and recommendations. Am. J. Orthopsychiatr. 2010, 80, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Perera, S.; Gavian, M.; Frazier, P.; Johnson, D.; Spring, M.; Westermeyer, J.; Butcher, J.; Halcon, L.; Robertson, C.; Savik, K.; et al. A longitudinal study of demographic factors associated with stressors and symptoms in african refugees. Am. J. Orthopsychiatr. 2013, 83, 448–472. [Google Scholar] [CrossRef]
- Marshall, G.N.; Schell, T.L.; Elliott, M.N.; Berthold, S.M.; Chun, C.A. Mental health of Cambodian refugees 2 decades after resettlement in the United States. J. Am. Med. Assoc. 2005, 294, 571–579. [Google Scholar] [CrossRef]
- Carlson, E.B.; Rosser-Hogan, R. Mental health status of cambodian refugees ten years after leaving their homes. Am. J. Orthopsychiatr. 1993, 63, 223–231. [Google Scholar] [CrossRef]
- Vaage, A.B.; Thomsen, P.H.; Silove, D.; Wentzel-Larsen, T.; Van Ta, T.; Hauff, E. Long-term mental health of Vietnamese refugees in the aftermath of trauma. Br. J. Psychiatr. 2010, 196, 122–125. [Google Scholar] [CrossRef]
- Sierau, S.; Schneider, E.; Nesterko, Y.; Glaesmer, H. Alone, but protected? Effects of social support on mental health of unaccompanied refugee minors. Eur. Child Adolesc. Psychiatry. 2019, 28, 769–780. [Google Scholar] [CrossRef]
- Oppedal, B.; Özer, S.; Şirin, S.R. Traumatic events, social support and depression: Syrian refugee children in Turkish camps. Vulnerable Child Youth Stud. 2018, 13, 46–59. [Google Scholar] [CrossRef]
- Singh, A.P.; Dubey, A.P. Role of social support as a mediator in negative stressful life event and somatic complaints of managerial personnel. Indian J Posit Psychol. 2015, 6, 249–254. [Google Scholar]
- Siriwardhana, C.; Adikari, A.; Pannala, G.; Siribaddana, S.; Abas, M.; Sumathipala, A.; Stewart, R. Prolonged internal displacement and common mental disorders in Sri Lanka: The COMRAID study. PLoS ONE 2013, 8, e64742. [Google Scholar] [CrossRef]
- Hamid, A.A.R.M.; Musa, S.A. Mental health problems among internally displaced persons in Darfur. Int. J. Psychol. 2010, 45, 278–285. [Google Scholar] [CrossRef]
- Maharaj, V.; Tomita, A.; Thela, L.; Mhlongo, M.; Burns, J.K. Food insecurity and risk of depression among refugees and immigrants in South Africa. J. Immigr. Minor Heal. 2017, 19, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Ghattas, H.; Sassine, A.B.J.; Seyfert, K.; Nord, M.; Sahyoun, N.R. Prevalence and correlates of food insecurity among palestinian refugees in Lebanon: Data from a household survey. PLoS ONE 2015, 10, e0130724. [Google Scholar] [CrossRef]
- Pinstrup-Andersen, P. Food security: Definition and measurement. Food Secur. 2009, 1, 5–7. [Google Scholar] [CrossRef]
- Momartin, S.; Silove, D.; Manicavasagar, V.; Steel, Z. Comorbidity of PTSD and depression: Associations with trauma exposure, symptom severity and functional impairment in Bosnian refugees resettled in Australia. J. Affect Disord. 2004, 80, 231–238. [Google Scholar] [CrossRef]
- Silove, D. The psychosocial effects of torture, mass human rights violations, and refugee trauma: Toward an integrated conceptual framework. J. Nerv. Ment. Dis. 1999, 187, 200–207. [Google Scholar] [CrossRef]
- Bailey, C.R.; Cordell, E.; Sobin, S.M.; Neumeister, A. Recent progress in understanding the pathophysiology of post-traumatic stress disorder. CNS Drugs 2013, 27, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Whittle, H.J.; Sheira, L.A.; Wolfe, W.R.; Frongillo, E.A.; Palar, K.; Merenstein, D.; Wilson, T.E.; Adedimeji, A.; Weber, K.M.; Adimora, A.A.; et al. Food insecurity is associated with anxiety, stress, and symptoms of posttraumatic stress disorder in a cohort of women with or at risk of HIV in the United States. J. Nutr. 2019, 149, 1393–1403. [Google Scholar] [CrossRef]
- Razum, O.; Zeeb, H.; Rohrmann, S. The ‘healthy migrant effect’–not merely a fallacy of inaccurate denominator figures. Int. J. Epidemiol. 2000, 29, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.; Dooley, B.; Benson, C. Theoretical perspectives on post-migration adaptation and psychological well-being among refugees: Towards a resource-based model. J. Refug. Stud. 2008, 21, 1–8. [Google Scholar] [CrossRef]
| Characteristics | Frequency n (%) | |
|---|---|---|
| Gender | Male | 116 (52.7) |
| Female | 104 (47.3) | |
| Age (Years) | 18–35 | 151 (68.6) |
| 36–55 | 51 (23.2) | |
| ≥56 | 18 (8.2) | |
| Marital status | Single | 39 (17.7) |
| Married | 176 (80.0) | |
| Divorced | 5 (2.3) | |
| Educational attainment | Less than secondary | 87 (39.5) |
| Secondary school | 119 (54.1) | |
| College | 14 (6.4) | |
| Employment status | Full time employment | 96 (43.6) |
| Part-time/Unemployed | 124 (56.4) | |
| Time spent in Malaysia (Months) | <12 | 14 (6.4) |
| 12–23 | 9 (4.1) | |
| 24–36 | 10 (4.5) | |
| >36 | 187 (85.0) | |
| Homelessness | Yes | 1 (0.5) |
| No | 219 (99.5) | |
| Separation from a family member | Yes | 160 (72.7) |
| No | 60 (27.3) | |
| Exposure to violence | Non-Exposed | 125 (56.8) |
| Exposed | 95 (43.2) | |
| Physical injuries (non-accidental) | Yes | 63 (28.6) |
| No | 157 (71.4) | |
| Perceived social support | Low/moderate | 91 (41.4) |
| High | 129 (58.6) | |
| Religious orientation * Mean (SD) | Overall a | 51.8 (8.0) |
| Intrinsic b | 32.8 (4.4) | |
| Extrinsic-Personal c | 13.6 (2.5) | |
| Extrinsic-Social c | 5.4 (3.6) | |
| Food security | Food secure | 64 (29.1) |
| Food insecure | 156 (70.9) | |
| MHDs | Frequency n (%) | 95% CI | |
|---|---|---|---|
| MDD | Yes | 71 (32.3) | 0.26, 0.39 |
| No | 149 (67.7) | - | |
| GAD | Yes | 92 (41.8) | 0.36, 0.48 |
| No | 128 (58.2) | - | |
| PTSD | Yes | 84 (38.2) | 0.32, 0.45 |
| No | 136 (61.8) | - |
| Variable | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| Crude OR (95% CI) | p-Value | Adjusted OR (95%CI) | p-Value | |
| Gender | ||||
| Male | 1 (Reference) | 1 (Reference) | ||
| Female | 1.58 (0.89, 2.78) | 0.117 * | 2.54 (1.21, 5.34) | 0.014 ** |
| Age (years) | ||||
| 18–35 | 1 (Reference) | |||
| 36–55 | 0.92 (0.47, 1.83) | 0.819 | - | - |
| ≥56 | 0.78 (0.26, 2,30) | 0.649 | - | - |
| Marital status | ||||
| Single | 1 (Reference) | |||
| Married | 0.75 (0.36, 1.55) | 0.437 | - | - |
| Divorced | 288 (0.00, 0.00) | 0.999 | - | - |
| Education | ||||
| Less than secondary | 1 (Reference) | 1 (Reference) | ||
| Secondary school | 0.68 (0.38, 1.23) | 0.200 * | 0.89 (0.45, 1.75) | 0.726 |
| College | 0.45 (0.12, 1.72) | 0.241 * | 0.68 (0.15, 3.23) | 0.631 |
| Employment status | ||||
| Full-time employment | 1 (Reference) | |||
| Part time/Unemployment | 1.41 (0.79, 2.50) | 0.248 * | - | - |
| Time spent in Malaysia (Months) | ||||
| <12 | 6.67 (2.00, 22.21) | 0.002 * | 6.95 (1.89, 25.57) | 0.004 ** |
| 12–23 | 3.33 (0.86, 12.90) | 0.081 * | 3.66 (0.81, 16.54) | 0.092 |
| 24–36 | 2.67 (0.74, 9.60) | 0.133 * | 2.77 (0.61, 12.54) | 0.185 |
| >36 | 1 (Reference) | 1 (Reference) | ||
| Homelessness | ||||
| Yes | 0.00 (0.00, 0.00) | 1.000 | - | - |
| No | 1 (Reference) | |||
| Separation from a family member | ||||
| Yes | 1.16 (0.61, 2.20) | 0.659 | - | - |
| No | 1 (Reference) | |||
| Exposure to violence | ||||
| Non-Exposed | 1 (Reference) | |||
| Exposed | 1.44 (0.82, 2.55) | 0.207 * | - | - |
| Physical injuries | - | - | ||
| Yes | 2.83 (1.54, 5.22) | 0.001 * | 3.25 (1.52, 6.96) | 0.002 ** |
| No | 1 (Reference) | 1 (Reference) | ||
| Perceived social support | ||||
| Low/Moderate | 2.71 (1.51, 4.84) | 0.001 * | 2.17 (1.13, 4.19) | 0.021 ** |
| High | 1 (Reference) | 1 (Reference) | ||
| Religious orientation (Overall) | 0.99 (0.96, 1.03) | 0.653 | - | - |
| Food security | ||||
| Food secure | 1 (Reference) | 1 (Reference) | ||
| Food insecure | 3.47 (1.64, 7.32) | 0.001 * | 2.77 (1.19, 6.47) | 0.019 ** |
| Variable | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| Crude OR (95% CI) | p-Value | Adjusted OR (95%CI) | p-Value | |
| Gender | ||||
| Male | 1 (Reference) | |||
| Female | 1.21 (0.71, 2.06) | 0.492 | - | - |
| Age (years) | ||||
| 18–35 | 1 (Reference) | |||
| 36–55 | 1.39 (0.73, 2.63) | 0.317 | - | - |
| ≥56 | 1.56 (0.59, 4.16) | 0.374 | - | - |
| Marital status | ||||
| Single | 1 (Reference) | 1 (Reference) | ||
| Married | 0.88 (0.43, 1.76) | 0.709 | 0.99 (0.47, 2.09) | 0.975 |
| Divorced | 5.18 (0.53, 50.65) | 0.158 * | 4.21 (0.41, 43.16) | 0.226 |
| Education | ||||
| Less than secondary | 1 (Reference) | 1 (Reference) | ||
| Secondary school | 0.97 (0.55, 1.70) | 0.906 | 0.97 (0.54, 1.75) | 0.911 |
| College | 0.35 (0.09, 1.35) | 0.128 * | 0.31 (0.08, 1.24) | 0.097 |
| Employment status | ||||
| Full-time employment | 1 (Reference) | |||
| Part time/Unemployment | 1.09 (0.64, 1.87) | 0.752 | - | - |
| Time spent in Malaysia (Months) | ||||
| <12 | 2.04 (0.68, 6.11) | 0.205 * | 2.14 (0.70, 6.56) | 0.185 |
| 12–23 | 1.91 (0.50, 7.34) | 0.347 | 1.67 (0.42, 6.73) | 0.468 |
| 24–36 | 1.53 (0.43, 5.46) | 0.515 | 1.47 (0.38, 5.67) | 0.580 |
| >36 | 1 (Reference) | 1 (Reference) | ||
| Homelessness | ||||
| Yes | 1 (Reference) | 1.000 | ||
| No | 0.00 (0.00, 0.00) | - | - | |
| Separation from a family member | ||||
| Yes | 0.92 (0.50, 1.67) | 0.780 | - | - |
| No | 1 (Reference) | |||
| Exposure to violence | ||||
| Non-Exposed | 1 (Reference) | |||
| Exposed | 1.02 (0.60, 1.75) | 0.940 | - | - |
| Physical injuries | ||||
| Yes | 1.67 (0.93, 3.01) | 0.089 * | 1.75 (0.94, 3.25) | 0.077 |
| No | 1 (Reference) | 1 (Reference) | ||
| Perceived social support | ||||
| Low/Moderate | 1.00 (0.58, 1.72) | 0.988 | - | - |
| High | 1 (Reference) | |||
| Religious orientation (Overall) | 0.98 (0.95, 1.02) | 0.268 | - | - |
| Food security | ||||
| Food secure | 1 (Reference) | |||
| Food insecure | 1.29 (0.71, 2.34) | 0.406 | - | - |
| Variable | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| Crude OR (95% CI) | p-Value | Adjusted OR (95%CI) | p-Value | |
| Gender | ||||
| Male | 1 (Reference) | 1 (Reference) | ||
| Female | 0.59 (0.34, 1.03) | 0.063 * | 0.60 (0.27, 1.35) | 0.217 |
| Age (years) | ||||
| 18–35 | 1 (Reference) | 1 (Reference) | ||
| 36–55 | 1.18 (0.62, 2.25) | 0.609 | 1.16 (0.45, 2.96) | 0.762 |
| ≥56 | 0.31 (0.09, 1.12) | 0.075 * | 0.36 (0.07, 1.95) | 0.237 |
| Marital status | ||||
| Single | 1 (Reference) | |||
| Married | 1.26 (0.61, 2.62) | 0.537 | - | - |
| Divorced | 3.00 (0.45, 20.24) | 0.259 | - | - |
| Education | ||||
| Less than secondary | 1 (Reference) | |||
| Secondary school | 0.96 (0.54, 1.70) | 0.889 | - | - |
| College | 1.64 (0.53, 5.08) | 0.395 | - | - |
| Employment status | ||||
| Full-time employment | 1 (Reference) | |||
| Part time/Unemployment | 0.97 (0.56, 1.68) | 0.923 | - | - |
| Time spent in Malaysia (Months) | ||||
| <12 | 0.85 (0.27, 2.63) | 0.776 | - | - |
| 12–23 | 0.44 (0.09, 2.16) | 0.309 | - | - |
| 24–36 | 0.65 (0.16, 2.61) | 0.548 | - | - |
| >36 | 1 (Reference) | |||
| Homelessness | ||||
| Yes | 1 (Reference) | 1.000 | ||
| No | 0.00 (0.00, 0.00) | - | - | |
| Separation from a family member | ||||
| Yes | 1.82 (0.96, 3.47) | 0.068 * | ||
| No | 1 (Reference) | - | - | |
| Exposure to violence | ||||
| Non-Exposed | 1 (Reference) | 1 (Reference) | ||
| Exposed | 34.39 (15.75, 75.10) | 0.000 * | 38.46 (16.27, 90.91) | 0.000 ** |
| Physical injuries | ||||
| Yes | 21.54 (9.86, 47.07) | 0.000 * | ||
| No | 1 (Reference) | - | - | |
| Perceived social support | ||||
| Low/Moderate | 0.94 (0.54, 1.64) | 0.834 | - | - - |
| High | 1 (Reference) | |||
| Religious orientation (Overall) | 1.03 (0.99, 1.06) | 0.154 * | 1.05 (0.99, 1.10) | 0.069 |
| Food security | ||||
| Food secure | 1 (Reference) | 1 (Reference) | - | |
| Food insecure | 3.71 (1.84, 7.50) | 0.000 * | 3.74 (1.41, 9.91) | 0.008 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaur, K.; Sulaiman, A.H.; Yoon, C.K.; Hashim, A.H.; Kaur, M.; Hui, K.O.; Sabki, Z.A.; Francis, B.; Singh, S.; Gill, J.S. Elucidating Mental Health Disorders among Rohingya Refugees: A Malaysian Perspective. Int. J. Environ. Res. Public Health 2020, 17, 6730. https://doi.org/10.3390/ijerph17186730
Kaur K, Sulaiman AH, Yoon CK, Hashim AH, Kaur M, Hui KO, Sabki ZA, Francis B, Singh S, Gill JS. Elucidating Mental Health Disorders among Rohingya Refugees: A Malaysian Perspective. International Journal of Environmental Research and Public Health. 2020; 17(18):6730. https://doi.org/10.3390/ijerph17186730
Chicago/Turabian StyleKaur, Kushilpal, Ahmad Hatim Sulaiman, Chee Kok Yoon, Aili Hanim Hashim, Manveen Kaur, Koh Ong Hui, Zuraida Ahmad Sabki, Benedict Francis, Sarbhan Singh, and Jesjeet Singh Gill. 2020. "Elucidating Mental Health Disorders among Rohingya Refugees: A Malaysian Perspective" International Journal of Environmental Research and Public Health 17, no. 18: 6730. https://doi.org/10.3390/ijerph17186730
APA StyleKaur, K., Sulaiman, A. H., Yoon, C. K., Hashim, A. H., Kaur, M., Hui, K. O., Sabki, Z. A., Francis, B., Singh, S., & Gill, J. S. (2020). Elucidating Mental Health Disorders among Rohingya Refugees: A Malaysian Perspective. International Journal of Environmental Research and Public Health, 17(18), 6730. https://doi.org/10.3390/ijerph17186730






