Association of Summer Heat Waves and the Probability of Preterm Birth in Minnesota: An Exploration of the Intersection of Race and Education
Abstract
1. Introduction
2. Materials and Methods
2.1. Outcome and Exposure
2.2. Covariates
2.3. Statistical Analysis
Race_Ethnicity + B5 × Metro + B6 × Year
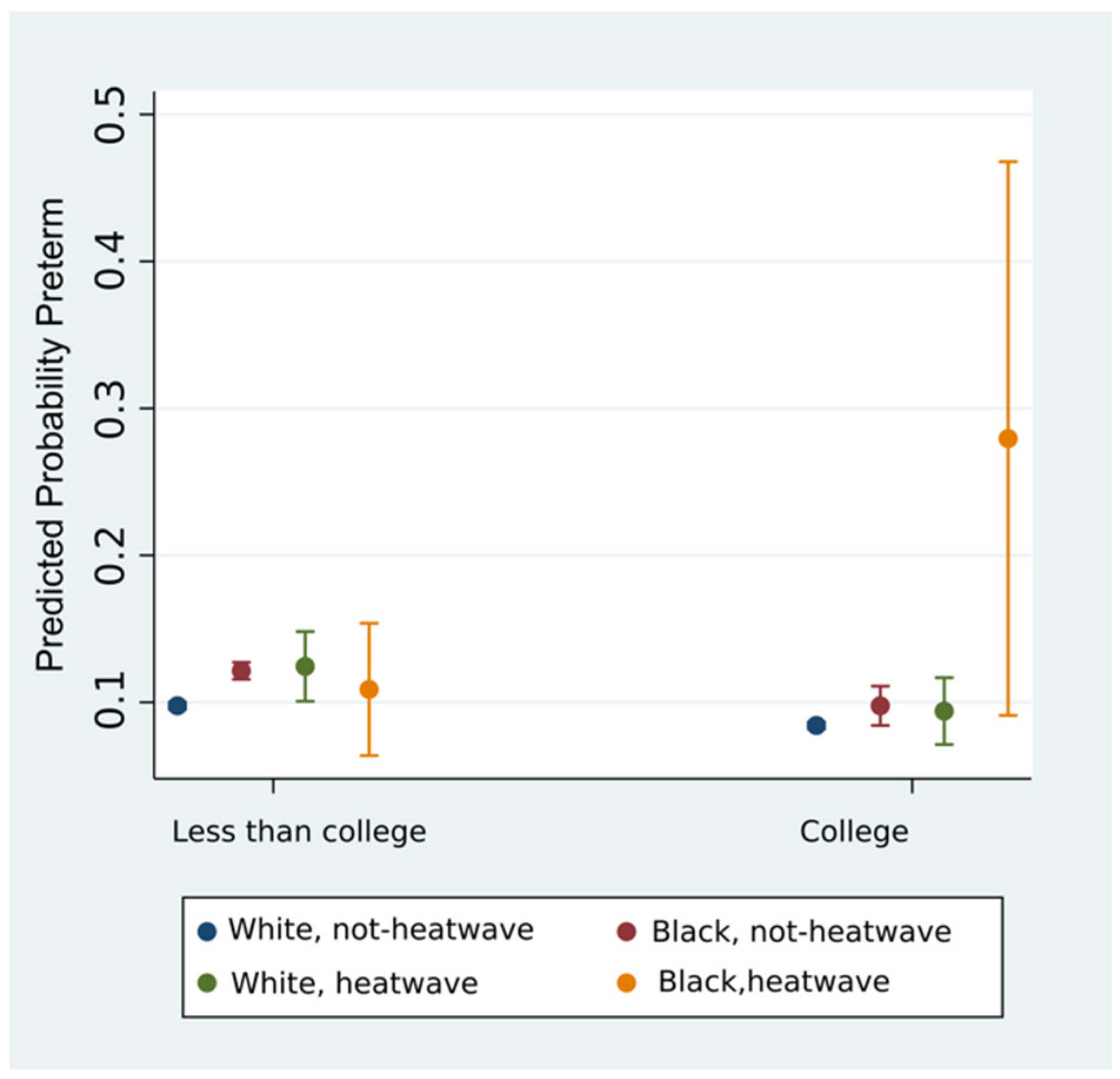
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Blencowe, H.; Cousens, S.; Oestergaard, M.Z.; Chou, D.; Moller, A.; Narwal, R.; Adler, A.; Garcia, C.V.; Rohde, S.; Say, L.; et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries : A systematic analysis and implications. Lancet 2012, 379, 2162–2172. [Google Scholar] [CrossRef]
- Hodek, J.M.; von der Schulenburg, J.M.; Mittendorf, T. Measuring economic consequences of preterm birth-methodological recommendations for the evaluation of personal burden on children and their caregivers. Health Econ. Rev. 2011, 1, 1–10. [Google Scholar] [CrossRef]
- Ferré, C.; Callaghan, W.; Olson, C.; Sharma, A.; Barfield, W. Effects of Maternal Age and Age-Specific Preterm Birth Rates on Overall Preterm Birth Rates—United States, 2007 and 2014. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 1181–1184. [Google Scholar] [CrossRef]
- Martin, J.A.; Osterman, M.J. Describing the Increase in Preterm Births in the United States, 2014–2016. NCHS Data Brief 2018, 2015, 1–8. [Google Scholar]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Coley, S.L.; Nichols, T.R.; Rulison, K.L.; Aronson, R.E.; Brown-Jeffy, S.L.; Morrison, S.D.; Coley, S.L.; Nichols, T.R.; Rulison, K.L.; Aronson, R.E.; et al. Race, Socioeconomic Status, and Age: Exploring Intersections in Preterm Birth Disparities among Teen Mothers. Int. J. Popul. Res. 2015, 2015, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Raglan, G.B.; Lannon, S.M.; Jones, K.M.; Schulkin, J. Racial and Ethnic Disparities in Preterm Birth Among American Indian and Alaska Native Women. Matern. Child Health J. 2015, 20, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, F.; Monet, B.; Ducruet, T.; Chaillet, N.; Audibert, F. Effect of maternal age on the risk of preterm birth: A large cohort study. PLoS ONE 2018, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, A.A.M.; Simões, V.M.F.; Barbieri, M.A.; Bettiol, H.; Lamy-Filho, F.; Coimbra, L.C.; Alves, M.T.S.S.B. Young maternal age and preterm birth. Paediatr. Perinat. Epidemiol. 2003, 17, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Reagan, P.B.; Salsberry, P.J. Race and ethnic differences in determinants of preterm birth in the USA: Broadening the social context. Soc. Sci. Med. 2005, 60, 2217–2228. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.A.; Heck, K.; Egerter, S.; Marchi, K.S.; Dominguez, T.P.; Cubbin, C.; Fingar, K.; Pearson, J.A.; Curtis, M. The role of socioeconomic factors in Black-White disparities in preterm birth. Am. J. Public Health 2015, 105, 694–702. [Google Scholar] [CrossRef] [PubMed]
- McGrady, G.A.; Sung, J.F.C.; Rowley, D.L.; Hogue, C.J.R. Preterm Delivery and Low Birth Weight among First-Born Infants of Black and White College Graduates. Am. J. Epidemiol. 1992, 136, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Malig, B.; Ostro, B. High ambient temperature and the risk of preterm delivery. Am. J. Epidemiol. 2010, 172, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Samet, J.M. Relation between elevated ambient temperature and mortality: A review of the epidemiologic evidence. Epidemiol. Rev. 2002, 24, 190–202. [Google Scholar] [CrossRef]
- Hajat, S.; Armstrong, B.; Baccini, M.; Biggeri, A.; Bisanti, L.; Russo, A.; Paldy, A.; Menne, B.; Kosatsky, T. Impact of high temperatures on mortality: Is there an added heat wave effect? Epidemiology 2006, 17, 632–638. [Google Scholar] [CrossRef]
- Carolan-Olah, M.; Frankowska, D. High environmental temperature and preterm birth: A review of the evidence. Midwifery 2014, 30, 50–59. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, C.; Wang, L. Temperature exposure during pregnancy and birth outcomes: An updated systematic review of epidemiological evidence. Environ. Pollut. 2017, 225, 700–712. [Google Scholar] [CrossRef]
- Vicedo-cabrera, A.M.; Iñíguez, C.; Barona, C.; Ballester, F. Exposure to elevated temperatures and risk of preterm birth in Valencia, Spain. Environ. Res. 2014, 134, 210–217. [Google Scholar] [CrossRef]
- Ha, S.; Liu, D.; Zhu, Y.; Kim, S.S.; Sherman, S.; Mendola, P. Ambient Temperature and Early Delivery of Singleton Pregnancies. Environ. Health Perspect. 2016, 125, 453–459. [Google Scholar] [CrossRef]
- Basu, R.; Chen, H.; Li, D.-K.; Avalos, L.A. The impact of maternal factors on the association between temperature and preterm delivery. Environ. Res. 2017, 154, 109–114. [Google Scholar] [CrossRef]
- Dadvand, P.; Basagaña, X.; Sartini, C.; Figueras, F.; Vrijheid, M.; de Nazelle, A.; Sunyer, J.; Nieuwenhuijsen, M.J. Climate extremes and the length of gestation. Environ. Health Perspect. 2011, 119, 1449–1453. [Google Scholar] [CrossRef] [PubMed]
- Avalos, L.A.; Chen, H.; Li, D.K.; Basu, R. The impact of high apparent temperature on spontaneous preterm delivery: A case-crossover study. Environ. Health Glob. Access Sci. Source 2017, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- He, J.-R.; Liu, Y.; Xia, X.-Y.; Ma, W.-J.; Lin, H.-L.; Kan, H.-D.; Lu, J.-H.; Feng, Q.; Mo, W.-J.; Wang, P.; et al. Ambient Temperature and the Risk of Preterm Birth in Guangzhou, China (2001–2011). Environ. Health Perspect. 2015, 124, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, V.; Díaz, J.; Ortiz, C.; Carmona, R.; Sáez, M.; Linares, C. Short term effect of air pollution, noise and heat waves on preterm births in Madrid (Spain). Environ. Res. 2016, 145, 162–168. [Google Scholar] [CrossRef]
- Sun, S.; Weinberger, K.R.; Spangler, K.R.; Eliot, M.N.; Braun, J.M.; Wellenius, G.A. Ambient temperature and preterm birth: A retrospective study of 32 million US singleton births. Environ. Int. 2019, 126, 7–13. [Google Scholar] [CrossRef]
- Asta, F.; Michelozzi, P.; Badaloni, C.; Davoli, M.; Schifano, P. OP II—3 Effect modification by socio-economic position and green spaces of short-term exposure to heat and air pollutants on preterm-birth risk. a time series study in rome, 2001–2013. Occup. Environ. Med. 2018, 75, A3–A4. [Google Scholar]
- Walfisch, A.; Kabakov, E.; Friger, M.; Sheiner, E. Trends, seasonality and effect of ambient temperature on preterm delivery. J. Matern. Neonatal Med. 2017, 30, 2483–2487. [Google Scholar] [CrossRef]
- Ilango, S.D.; Weaver, M.; Sheridan, P.; Schwarz, L.; Clemesha, R.E.S.; Bruckner, T.; Basu, R.; Gershunov, A.; Benmarhnia, T. Extreme heat episodes and risk of preterm birth in California, 2005–2013. Environ. Int. 2020, 137, 105541. [Google Scholar] [CrossRef]
- Lee, S.J.; Hajat, S.; Steer, P.J.; Filippi, V. A time-series analysis of any short-term effects of meteorological and air pollution factors on preterm births in London, UK. Environ. Res. 2008, 106, 185–194. [Google Scholar] [CrossRef]
- Wolf, J.; Armstrong, B. The association of season and temperature with adverse pregnancy outcome in two german states, a time-series analysis. PLoS ONE 2012, 7, 1–8. [Google Scholar] [CrossRef]
- Auger, N.; Naimi, A.I.; Smargiassi, A.; Lo, E.; Kosatsky, T. Extreme heat and risk of early delivery among preterm and term pregnancies. Epidemiology 2014, 25, 344–350. [Google Scholar] [CrossRef]
- Kloog, I.; J, M.S.; Coull, B.A.; Nordio, F.; Schwartz, J.D. Using Satellite-Based Spatiotemporal Resolved Air Temperature Exposure to Study the Association between Ambient Air Temperature and Birth Outcomes in Massachusetts. Environ. Health Perspect. 2015, 123, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Lin, Y.; Ma, Y.; Zhang, L.; Zhang, X.; Li, L.; Zhang, S.; Cheng, Y.; Zhou, X.; Lin, H.; et al. The association between ambient temperature and preterm birth in Shenzhen, China: A distributed lag non-linear time series analysis. Environ. Health Glob. Access Sci. Source 2016, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lucy, M.C.; Safranski, T.J. Heat stress in pregnant sows : Thermal responses and subsequent performance of sows and their offspring. Mol. Reprod. Dev. 2017, 84, 946–956. [Google Scholar] [CrossRef] [PubMed]
- Dreiling, C.E.; Carman, F.S.; Brown, D.E. Maternal Endocrine and Fetal Metabolic Responses to Heat Stress. J. Dairy Sci. 1991, 74, 312–327. [Google Scholar] [CrossRef]
- Yackerson, N.; Piura, B.; Sheiner, E. The influence of meteorological factors on the emergence of preterm delivery and preterm premature rupture of membrane. J. Perinatol. 2008, 28, 707–711. [Google Scholar] [CrossRef]
- Meehl, G.A.; Tebaldi, C. More Intense, More Frequent, and Longer Lasting Heat Waves in the 21st Century. Science 2016, 305, 994–997. [Google Scholar] [CrossRef]
- Mora, C.; Dousset, B.; Caldwell, I.R.; Powell, F.E.; Geronimo, R.C.; Bielecki, C.R.; Counsell, C.W.W.; Dietrich, B.S.; Johnston, E.T.; Louis, L.V.; et al. Global risk of deadly heat. Nat. Clim. Chang. 2017, 7, 501–506. [Google Scholar] [CrossRef]
- MDH. Minnesota State, County and Community Health Board Vital Statistics Trend Reports. Available online: http://www.health.state.mn.us/divs/chs/trends/index.html (accessed on 4 May 2018).
- Manson, S.; Schroeder, J.; Van Riper, D.; Ruggles, S. IPUMS National Historical Geographic Information System: Version 13.0 [Database]; Minneapolis, MN, USA, 2018. Available online: https://www.nhgis.org/ (accessed on 28 August 2020).
- Behrman, R.E.; Butler, A.S. Preterm Birth: Causes, Consequences, and Prevention; National Academies Press: Washington, DC, USA, 2007; ISBN 9780309101592. [Google Scholar]
- Skupski, D.W.; Owen, J.; Kim, S.; Fuchs, K.M.; Albert, P.S.; Grantz, K.L. Estimating Gestational Age from Ultrasound Fetal Biometrics. Obstet. Gynecol. 2017, 130, 433–441. [Google Scholar] [CrossRef]
- ACOG. Methods for Estimating the Due Date. Obstet. Gynecol. 2017, 129, 959–960. [Google Scholar]
- Smith, T.T.; Zaitchik, B.F.; Gohlke, J.M. Heat waves in the United States: Definitions, patterns and trends. Clim. Chang. 2013, 118, 811–825. [Google Scholar] [CrossRef] [PubMed]
- Blixt, P.; DeVries, A.; Dunlap, S.; Evans, A.; Galatowitsch, S.; Krause, T.; Kvale, W.; Maine, J.; Maki, G.; Menier, B.; et al. Minnesota Extreme Heat Toolkit; Minnesota Department of Health: St. Paul, MN, USA, 2012. [Google Scholar]
- NWS. Hourly Temperature, and DewPoint Temperature, Automated Surface Observing System (ASOS) Data for Minneapolis St. Paul Airport, 2009–2015; National Weather Service: Minneapolis, MN, USA, 2017. [Google Scholar]
- Brooke Anderson, G.; Bell, M.L.; Peng, R.D. Methods to calculate the heat index as an exposure metric in environmental health research. Environ. Health Perspect. 2013, 121, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- Rothfusz, L.P. The heat index equation (or, more than you ever wanted to know about heat index). NWS South Reg. Tech. Attach. 1990, SR/SSD, 90-23. Available online: https://wonder.cdc.gov/wonder/help/Climate/ta_htindx.PDF (accessed on 31 August 2020).
- Schaaf, J.M.; Liem, S.M.S.; Mol, B.W.J.; Abu-Hanna, A.; Ravelli, A.C.J. Ethnic and Racial Disparities in the Risk of Preterm Birth: A Systematic Review and Meta-Analysis. Am. J. Perinatol. 2013, 30, 433–450. [Google Scholar] [PubMed]
- Joseph, R.M.; O’Shea, T.M.; Allred, E.N.; Heeren, T.; Kuban, K.K. Maternal educational status at birth, maternal educational advancement, and neurocognitive outcomes at age 10 years among children born extremely preterm. Pediatr. Res. 2018, 83, 767–777. [Google Scholar] [CrossRef]
- Parker, J.; Schoendorf, K.; Kiely, J. Associations between Measures of Socioeconomic Status, Birth Weight, Small for Gestational Age, and Premature Delivery in the United States. Ann. Epidemiol. 1994, 4, 271–278. [Google Scholar] [CrossRef]
- Wang, J.; Williams, G.; Guo, Y.; Pan, X.; Tong, S. Maternal exposure to heatwave and preterm birth in Brisbane, Australia. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 1631–1641. [Google Scholar] [CrossRef]
- Collins, J.W.; Butler, A.G.; Epidemiology, S.; May, N.; Collins, J.W.; Butler, A.G. Racial Differences in the Prevalence of Small-for-Dates Infants among College-Educated Women. Epidemiology 2019, 8, 315–317. [Google Scholar] [CrossRef]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Chideya, S.; Marchi, K.S.; Metzler, M.; Posner, S. Socioeconomic Status in Health Research: One Size Does Not Fit All. JAMA 2005, 294, 2879–2888. [Google Scholar] [CrossRef]
- Kramer, M.R.; Hogue, C.R. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol. Rev. 2009, 31, 84–98. [Google Scholar] [CrossRef]
- Voelkel, J.; Hellman, D.; Sakuma, R.; Shandas, V. Assessing Vulnerability to Urban Heat: A Study of Disproportionate Heat Exposure and Access to Refuge by Socio-Demographic Status in Portland, Oregon. Int. J. Environ. Res. Public Health 2018, 15, 640. [Google Scholar] [CrossRef]
- Madrigano, J.; Ito, K.; Johnson, S.; Kinney, P.L.; Matte, T. A Case-Only Study of Vulnerability to Heat Wave–Related Mortality in New York City (2000–2011). Environ. Health Perspect. 2015, 123, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, S.J.; Shandas, V.; Pendleton, N. The Effects of Historical Housing Policies on Resident Exposure to Intra-Urban Heat: A Study of 108 US Urban Areas. Climate 2020, 8, 12. [Google Scholar] [CrossRef]
- Mccarthy, D.; Radley, D.C.; Hayes, S.L. Aiming Higher, 2015 Edition ed; The Commonwealth Fund: Washington, DC, USA, 2015. [Google Scholar]
- IPCC. Summary for Policymakers; IPCC: Geneva, Switzerland, 2014; ISBN 9789291691432. [Google Scholar]
- Kalkstein, L.S.; Smoyer, K.E. The impact of climate change on human health: Some international implications. Experientia 1993, 49, 969–979. [Google Scholar] [CrossRef] [PubMed]
| n = 154,157 | ||||
|---|---|---|---|---|
| Gestational Age (Weeks) | ||||
| <37 | >37 | |||
| Exposure Status Prior Seven Days | n | % | n | % |
| Mean heat index < 37 °C | 14,542 | 98.6 | 137,664 | 98.8 |
| Mean heat index ≥ 37 °C | 212 | 1.4 | 1739 | 1.3 |
| Race/Ethnicity | n | % | n | % |
| White, non-Hispanic | 10,394 | 70.45 | 103,611 | 74.32 |
| Black, non-Hispanic | 1821 | 12.34 | 13,334 | 9.57 |
| AIAN a, non-Hispanic | 337 | 2.28 | 2273 | 1.63 |
| Asian, non-Hispanic | 1112 | 7.54 | 9950 | 7.14 |
| Hispanic | 1063 | 7.20 | 9970 | 7.15 |
| Unknown | 27 | 0.18 | 265 | 0.19 |
| Age category | n | % | n | % |
| <18 | 231 | 1.57 | 1582 | 1.13 |
| 18 to <25 | 3158 | 21.40 | 28,648 | 20.55 |
| 25 to <40 | 10,825 | 73.37 | 105,657 | 75.79 |
| ≥40 | 540 | 3.66 | 3516 | 2.52 |
| Residence | n | % | n | % |
| Outside seven-county metro MSP b | 6297 | 42.68 | 60,676 | 43.53 |
| Inside seven-county metro MSP | 8457 | 57.32 | 78,727 | 56.47 |
| Educational attainment (available 2009–2015) | n | % | n | % |
| Less than high school education | 1782 | 12.08 | 13,832 | 9.92 |
| High school education | 7601 | 51.52 | 67,806 | 48.64 |
| College education | 5371 | 36.4 | 57,765 | 41.44 |
| 2009–2015, Births Occurring June 1–September 30 | ||
|---|---|---|
| Summer Births | n = 154,157 | |
| RR a (95% CI) | Adjusted RR (95% CI) | |
| Mean 7-day heat index ≥ 37 °C b | 1.14 (1.00–1.30) | 1.13 (0.99–1.28) |
| Race/Ethnicity c | ||
| Black | 1.21 (1.15–1.27) | |
| AIAN | 1.31 (1.18–1.46) | |
| Asian | 1.07 (1.00–1.13) | |
| Hispanic | 0.96 (0.90–1.02) | |
| Unknown | 0.95 (0.67–1.36) | |
| Age of mother d | ||
| 18 to <25 | 0.85 (0.74–0.96) | |
| 25 to <40 | 0.86 (0.76–0.98) | |
| ≥40 | 1.22 (1.05–1.41) | |
| Mother’s education e | ||
| High school grad | 0.93 (0.88–0.98) | |
| College grad | 0.79 (0.74–0.84) | |
| Metro residence f | 1.02 (0.99–1.06) | |
| Intercept | 0.09 (0.09–0.10) | 0.12 (0.11–0.14) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, M.L.; Hardeman, R.R. Association of Summer Heat Waves and the Probability of Preterm Birth in Minnesota: An Exploration of the Intersection of Race and Education. Int. J. Environ. Res. Public Health 2020, 17, 6391. https://doi.org/10.3390/ijerph17176391
Smith ML, Hardeman RR. Association of Summer Heat Waves and the Probability of Preterm Birth in Minnesota: An Exploration of the Intersection of Race and Education. International Journal of Environmental Research and Public Health. 2020; 17(17):6391. https://doi.org/10.3390/ijerph17176391
Chicago/Turabian StyleSmith, M. Luke, and Rachel R. Hardeman. 2020. "Association of Summer Heat Waves and the Probability of Preterm Birth in Minnesota: An Exploration of the Intersection of Race and Education" International Journal of Environmental Research and Public Health 17, no. 17: 6391. https://doi.org/10.3390/ijerph17176391
APA StyleSmith, M. L., & Hardeman, R. R. (2020). Association of Summer Heat Waves and the Probability of Preterm Birth in Minnesota: An Exploration of the Intersection of Race and Education. International Journal of Environmental Research and Public Health, 17(17), 6391. https://doi.org/10.3390/ijerph17176391






