Pollution, Health, and the Moderating Role of Physical Activity Opportunities
Abstract
:1. Introduction
1.1. Theoretical Background and Literature Review
1.1.1. Overall Health, Physical Health, and Mental Health
1.1.2. Pollution and Health
1.1.3. Physical Activity Opportunities and Health
1.1.4. The Moderating Role of Physical Activity Opportunities
2. Materials and Methods
2.1. Data Collection, Measures, and Variables
2.1.1. Pollution
2.1.2. Health
2.1.3. Physical Activity Opportunities
2.1.4. Controls
2.2. Empirical Analysis
3. Results
3.1. Descriptive Statistics
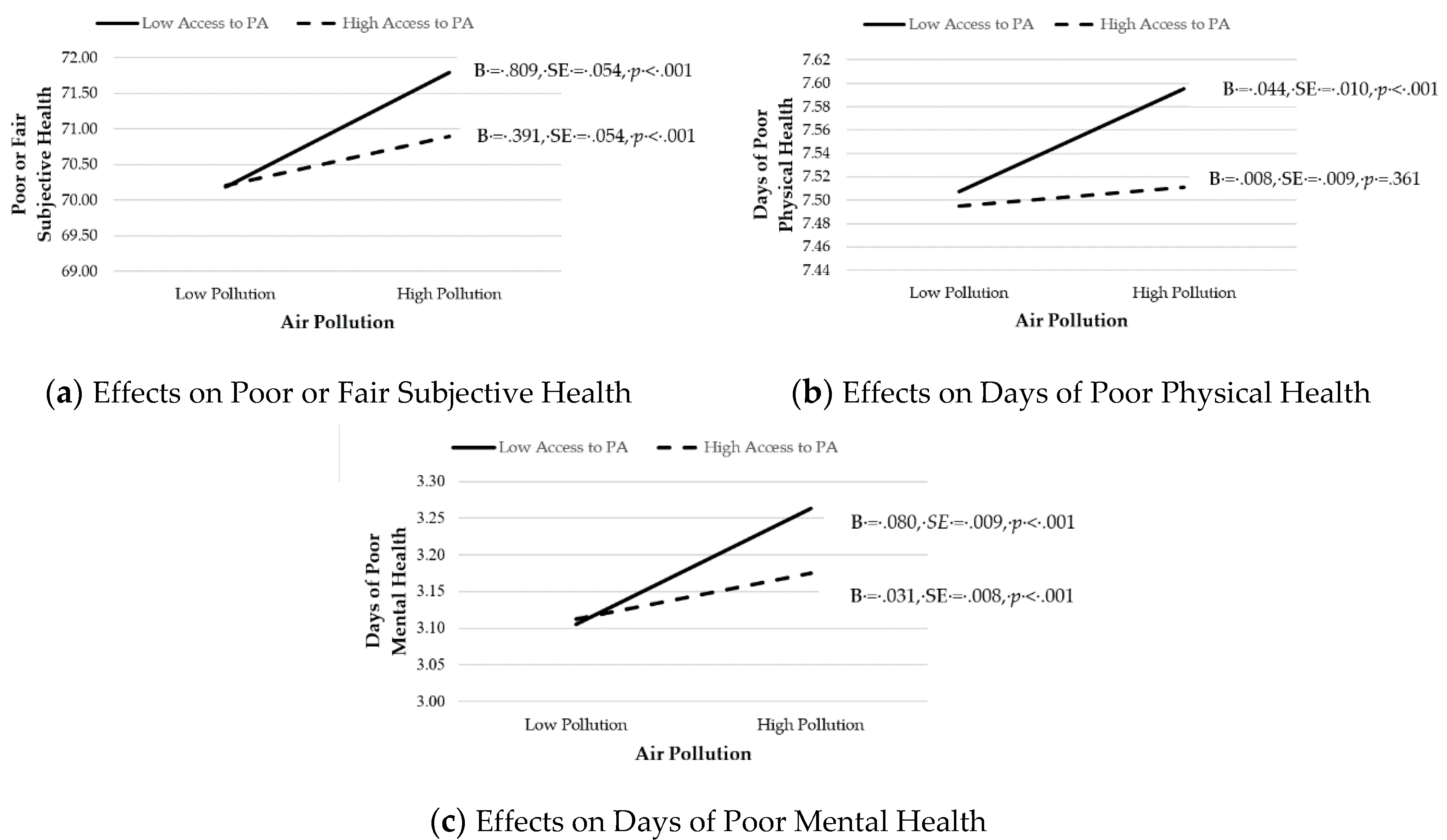
3.2. Hypothesis Testing
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Special Report. Global Warming of 1.5 °C. Available online: https://www.ipcc.ch/sr15/ (accessed on 13 May 2020).
- Crowley, T.J. Causes of climate change over the past 1000 years. Science 2000, 289, 270–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goel, P.K. Water Pollution: Causes, Effects and Control; New Age International: New Delhi, India, 2006; pp. 1–4. [Google Scholar]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242. [Google Scholar] [CrossRef]
- Schwarzenbach, R.P.; Egli, T.; Hofstetter, T.B.; Von Gunten, U.; Wehrli, B. Global water pollution and human health. Annu. Rev. Environ. Resour. 2010, 35, 109–136. [Google Scholar] [CrossRef]
- Welsch, H. Environmental welfare analysis: A life satisfaction approach. Ecol. Econ. 2007, 62, 544–551. [Google Scholar] [CrossRef]
- Landrigan, P.; Fuller, R.; Acosta, N.J.R.; Adeyi, O.; Arnold, R.; Basu, N.; Balde, A.B.; Bertollini, R.; Boufford, J.I.; Breysse, P.N.; et al. The Lancet Commission on pollution and health. Lancet 2017, 391, 462–512. [Google Scholar] [CrossRef] [Green Version]
- Roberts, J.D.; Voss, J.D.; Knight, B. The association of ambient air pollution and physical inactivity in the United States. PLoS ONE 2014, 9, e90143. [Google Scholar] [CrossRef]
- Hankey, S.; Marshall, J.D.; Brauer, M. Health impacts of the built environment: Within-urban variability in physical inactivity, air pollution, and ischemic heart disease mortality. Environ. Health Perspect. 2012, 120, 247–253. [Google Scholar] [CrossRef]
- Global Recommendations on Physical Activity for Health. Available online: http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf (accessed on 26 September 2016).
- Physical Activity Guidelines for Americans. Be Active, Healthy, and Happy! 2008. Available online: https://health.gov/our-work/physical-activity/previous-guidelines/2008-physical-activity-guidelines (accessed on 14 May 2020).
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Downward, P.; Dawson, P.; Mills, T.C. Sports participation as an investment in (subjective) health: A time series analysis of the life course. J. Public Health 2016, 38, e504–e510. [Google Scholar] [CrossRef] [Green Version]
- Wicker, P.; Coates, D.; Breuer, C. The effect of a four-week fitness program on satisfaction with health and life. Int. J. Environ. Res. Public Health 2015, 60, 41–47. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, Z. Industrial water pollution, water environment treatment, and health risks in China. Environ. Pollut. 2016, 218, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Wicker, P.; Orlowski, J. Coping with adversity: Physical activity as a moderator in adaption to bereavement. J. Public Health 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Humphreys, B.R. Sports participation and happiness: Evidence from US microdata. J. Econ. Psychol. 2012, 33, 776–793. [Google Scholar] [CrossRef] [Green Version]
- Downward, P.; Rasciute, S. Does sport make you happy? An analysis of the well-being derived from sports participation. Int. Rev. Appl. Econ. 2011, 25, 331–348. [Google Scholar] [CrossRef]
- Pope, C.A., III; Dockery, D.W. Health effects of fine particulate air pollution: Lines that connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef] [PubMed]
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Azizullah, A.; Khattak, M.N.K.; Richter, P.; Häder, D. Water pollution in Pakistan and its impact on public health—A review. Environ. Int. 2011, 37, 479–497. [Google Scholar] [CrossRef]
- Halder, J.N.; Islam, M.N. Water pollution and its impact on the human health. J. Environ. Human 2015, 2, 36–46. [Google Scholar] [CrossRef]
- Ebenstein, A. The consequences of industrialization: Evidence from water pollution and digestive cancers in China. Rev. Econ. Stat. 2012, 94, 186–201. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Guan, D.; Tao, S.; Wang, X.; He, K. A review of air pollution impact on subjective well-being: Survey versus visual psychophysics. J. Clean Prod. 2018, 184, 959–968. [Google Scholar] [CrossRef]
- Welsch, H. Environment and happiness: Valuation of air pollution using life satisfaction data. Ecol. Econ. 2006, 58, 801–813. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, X.; Chen, X. Happiness in the air: How does a dirty sky affect mental health and subjective well-being? J. Environ. Econ. Manag. 2017, 85, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Brinkel, J.; Kahn, M.H.; Kraemer, A. A systematic review of arsenic exposure and its social and mental health effects with special reference to Bangladesh. Int. J. Environ. Res. Public Health 2009, 6, 1609–1619. [Google Scholar] [CrossRef] [Green Version]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Dolan, P.; Peasgood, T.; White, M. Do we really know what makes us happy? A review of the economic literature on the factors associated with subjective well-being. J. Econ. Psychol. 2014, 29, 94–122. [Google Scholar] [CrossRef]
- Humphreys, B.R.; McLeod, L.; Ruseski, J.E. Physical activity and health outcomes: Evidence from Canada. Health Econ. 2014, 23, 33–54. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.R.; Nicol, C.W.; Bredin, S.S.D. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Downward, P.; Dawson, P. Is it pleasure or health from leisure that we benefit from most? An analysis of well-being alternatives and implications for policy. Soc. Indic. Res. 2016, 126, 443–465. [Google Scholar] [CrossRef] [Green Version]
- Wicker, P.; Frick, B. Intensity of physical activity and subjective well-being: An empirical analysis of the WHO recommendations. J. Public Health 2017, 39, e19–e26. [Google Scholar] [CrossRef]
- Edwards, M.B.; Cunningham, G. Examining the associations of perceived community racism with self-reported physical activity levels and health among older racial minority adults. J. Phys. Act. Health 2013, 10, 932–939. [Google Scholar] [CrossRef]
- Wicker, P.; Breuer, C.; Pawlowski, T. Promoting sport for all to age-specific target groups–The impact of sport infrastructure. Eur. Sport Manag. Q. 2009, 9, 103–118. [Google Scholar] [CrossRef]
- Norman, G.J.; Nutter, S.K.; Ryan, S.; Sallis, J.F.; Calfas, K.J.; Patrick, K. Community design and access to recreational facilities as correlates of adolescent physical activity and body-mass index. J. Phys. Act. Health 2006, 3, S118–S128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pawlowski, T.; Breuer, C.; Leyva, J. Sport opportunities and local well-being: Is sport a local amenity? In The Economics of Sport, Health and Happiness: The Promotion of Well-Being Through Sporting Activities; Rodriguez, P., Késenne, S., Humphreys, B.R., Eds.; Edward Elgar: Cheltenham, UK, 2011; pp. 223–244. [Google Scholar]
- Madsen, K.A.; Gosliner, W.; Woodward-Lopez, G.; Crawford, P.B. Physical activity opportunities associated with fitness and weight status among adolescents in low-income communities. Arch. Pediatr. Adolesc. Med. 2009, 163, 1014–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, F.; Liu, Y.; Lü, J.; Liang, L.; Harmer, P. Ambient air pollution in China poses a multifaceted health threat to outdoor physical activity. J. Epidemiol. Community Health 2015, 69, 201–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tainio, M.; de Nazelle, A.J.; Götschi, T.; Kahlmeier, S.; Rojas-Rueda, D.; Nieuwenhuijsen, M.J.; de Sá, T.H.; Kelly, P.; Woodcock, J. Can air pollution negate the health benefits of cycling and walking? Prev. Med. 2016, 87, 233–236. [Google Scholar] [CrossRef] [Green Version]
- Lü, J.; Liang, L.; Feng, Y.; Li, R.; Liu, Y. Air pollution exposure and physical activity in China: Current knowledge, public health implications, and future research needs. Int. J. Environ. Res. Public Health 2015, 12, 14887–14897. [Google Scholar] [CrossRef]
- Andersen, Z.J.; de Nazelle, A.; Mendez, M.A.; Garcia-Aymerich, J.; Hertel, O.; Tjønneland, A.; Overvard, K.; Raaschou-Nielsen, O.; Nieuwenhuijsen, M.J. A study of the combined effects of physical activity and air pollution on mortality in elderly urban residents: The Danish Diet, Cancer, and Health Cohort. Environ. Health Perspect. 2015, 123, 557–563. [Google Scholar] [CrossRef] [Green Version]
- Strosnider, H.M.; Chang, H.H.; Darrow, L.A.; Liu, Y.; Vaidyanathan, A.; Strickland, M.J. Age-specific associations of ozone and fine particulate matter with respiratory emergency department visits in the United States. Am. J. Respir. Crit. Care Med. 2019, 199, 882–890. [Google Scholar] [CrossRef]
- Talbott, E.O.; Rager, J.R.; Brink, L.L.; Benson, S.M.; Bilonick, R.A.; Wu, W.C.; Han, Y.Y. Trends in acute myocardial infarction hospitalization rates for US States in the CDC tracking network. PLoS ONE 2013, 8, e64457. [Google Scholar] [CrossRef] [Green Version]
- McDonald, Y.J.; Jones, N.E. Drinking water violations and environmental justice in the United States, 2011–2015. Am. J. Public Health 2018, 108, 1401–1407. [Google Scholar] [CrossRef]
- Roh, T.; Lynch, C.F.; Weyer, P.; Wang, K.; Kelly, K.M.; Ludewig, G. Low-level arsenic exposure from drinking water is associated with prostate cancer in Iowa. Environ. Res. 2017, 159, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Rozelle, S.; Xu, Q.; Yu, N.; Zhou, T. Social Engagement and Elderly Health in China: Evidence from the China Health and Retirement Longitudinal Survey (CHARLS). Int. J. Environ. Res. Public Health 2019, 16, 278. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.W.; Balluz, L.S.; Heath, G.W.; Moriarty, D.G.; Ford, E.S.; Giles, W.H.; Mokdad, A.H. Associations between recommended levels of physical activity and health-related quality of life Findings from the 2001 Behavioral Risk Factor Surveillance System (BRFSS) survey. Prev. Med. 2003, 37, 520–528. [Google Scholar] [CrossRef]
- Wardoku, R.; Blair, C.; Demmer, R.; Prizment, A. Association between physical inactivity and health-related quality of life in adults with coronary heart disease. Maturitas 2019, 128, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Holt, J.B.; Lu, H.; Wheaton, A.G.; Ford, E.S.; Greenlund, K.J.; Croft, J.B. Multilevel regression and poststratification for small-area estimation of population health outcomes: A case study of chronic obstructive pulmonary disease prevalence using the behavioral risk factor surveillance system. Am. J. Epidemiol. 2014, 179, 1025–1033. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Holt, J.B.; Yun, S.; Lu, H.; Greenlund, K.J.; Croft, J.B. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the behavioral risk factor surveillance system. Am. J. Epidemiol. 2015, 182, 127–137. [Google Scholar] [CrossRef] [Green Version]
- Jamal, A.; King, B.A.; Neff, L.J.; Whitmill, J.; Babb, S.D.; Graffunder, C.M. Current cigarette smoking among adults—United States, 2005–2015. Morb. Mortal. Wkly. Rep. 2016, 65, 1205–1211. [Google Scholar] [CrossRef] [Green Version]
- Dixon, J.B. The effect of obesity on health outcomes. Mol. Cell Endocrinol. 2010, 316, 104–108. [Google Scholar] [CrossRef]
- Gundersen, C.; Ziliak, J.P. Food insecurity and health outcomes. Health Aff. 2015, 34, 1830–1839. [Google Scholar] [CrossRef] [Green Version]
- Sommers, B.D.; Gawande, A.A.; Baicker, K. Health insurance coverage and health—What the recent evidence tells us. N. Engl. J. Med. 2017, 377, 586–593. [Google Scholar] [CrossRef]
- Chen, E.; Miller, G.E. Socioeconomic status and health: Mediating and moderating factors. Annu. Rev. Clin. Psychol. 2013, 9, 723–749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd ed.; Taylor & Francis Ltd.: New York, NY, USA, 2003; pp. 255–301. [Google Scholar] [CrossRef]
- Cunningham, G.B.; Ahn, N.Y. Moderation in sport management research: Room for growth. Meas. Phys. Educ. Exerc. Sci. 2019, 23, 310–313. [Google Scholar] [CrossRef]
- Hair, J.; Black, W.; Babin, B.; Anderson, R.E. Tatham, R.L. Multivariate Data Analysis, 6th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2010; p. 186. [Google Scholar]
- McCullough, B.P.; Orr, M.; Kellison, T. Sport ecology: Conceptualizing an emerging subdiscipline within sport management. J. Sport Manag. 2020, 1–12. [Google Scholar] [CrossRef]
- Cunningham, G.; McCullough, B.P.; Hohensee, S. Physical activity and climate change attitudes. Clim. Chang. 2020, 159, 61–74. [Google Scholar] [CrossRef]
| Variable | Description | n | M | SD | Min | Max |
|---|---|---|---|---|---|---|
| AirPollution | Average daily PM2.5 | 3070 | 9021 | 1978 | 3000 | 19.700 |
| WaterPollution | Presence of drinking water violations in the county (0 = no; 1 = yes) | 3099 | 0.371 | 0.483 | 0.000 | 1000 |
| AccesstoPA | Percent of county residents with access to physical activity opportunities | 3098 | 62.454 | 23.247 | 0.000 | 100.000 |
| PoorFairHealth | Percent of county residents with poor or fair subjective health ratings. | 3104 | 17.930 | 4753 | 8121 | 40.991 |
| PhysUnhealthyDays | Average number of physically unhealthy days among county residents | 3104 | 3991 | 0.707 | 2449 | 7062 |
| MenUnhealthyDays | Average number of mentally unhealthy days among county residents | 3104 | 4168 | 0.605 | 2533 | 6.14 |
| Smokers | Percent of smokers | 3104 | 17.462 | 3619 | 5909 | 41.491 |
| Obesity | Percent of adults with obesity | 3104 | 32.874 | 5442 | 12.400 | 57.700 |
| FoodInsecure | Percent of food insecure | 3104 | 13.237 | 3941 | 2900 | 36.300 |
| Uninsured | Percent Uninsured | 3103 | 13.592 | 6250 | 2683 | 42.397 |
| SomeCollege | Percent of population with some college | 3104 | 57.804 | 11.810 | 15.175 | 100.000 |
| Population | Number of residents (in thousand) | 3104 | 104.574 | 335.340 | 0.088 | 10,105.518 |
| 65plus | Percent of population aged 65 or older | 3104 | 19.311 | 4701 | 4830 | 57.857 |
| Rural | Percent of population rural | 3097 | 59.273 | 31.044 | 0.000 | 100.000 |
| Female | Percent of population that is female | 3104 | 49.859 | 2273 | 26.835 | 56.871 |
| White | Percent of population that is white | 3104 | 76.195 | 20120 | 2690 | 97.890 |
| Income | Median household income (in thousand dollar) | 3103 | 52.754 | 13.730 | 25.385 | 140.382 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Smokers | --- | ||||||||
| 2. Uninsured | 0.093 ** | --- | |||||||
| 3. SomeCollege | −0.537 ** | −0.441 ** | --- | ||||||
| 4. Unemployed | 0.439 ** | 0.026 | −0.382 ** | --- | |||||
| 5. 65 plus | −0.137 ** | −0.023 | −0.057 ** | 0.028 | --- | ||||
| 6. Rural | 0.201 ** | 0.185 ** | −0.321 ** | 0.061 ** | 0.480 ** | --- | |||
| 7. Female | 0.006 | −0.103 ** | 0.246 ** | −0.006 | 0.084 ** | −0.177 ** | --- | ||
| 8. White | −0.108 ** | −0.472 ** | 0.264 ** | −0.295 ** | 0.389 ** | 0.304 ** | 0.039 * | --- | |
| 9. Obesity | 0.496 ** | 0.059 ** | −0.372 ** | 0.239 ** | −0.102 ** | 0.174 ** | 0.040 * | −0.089 ** | --- |
| 10. FoodInsecure | 0.596 ** | 0.295 ** | −0.424 ** | 0.535 ** | −0.063 ** | 0.071 ** | 0.087 ** | −0.424 ** | 0.368 ** |
| 11. log_Population | −0.107 ** | −0.267 ** | 0.258 ** | −0.008 | −0.445 ** | −0.778 ** | 0.277 ** | −0.199 ** | −0.123 ** |
| 12. log_Income | −0.635 ** | −0.339 ** | 0.622 ** | −0.436 ** | −0.260 ** | −0.399 ** | 0.03 | 0.169 ** | −0.422 ** |
| 13. AirPollution | 0.314 ** | −0.143 ** | −0.161 ** | 0.177 ** | −0.289 ** | −0.221 ** | 0.231 ** | −0.053 ** | 0.262 ** |
| 14. WaterPollution | −0.055** | 0.019 | −0.015 | 0.102 ** | −0.083 ** | −0.178 ** | 0.010 | −0.119 ** | −0.037 * |
| 15. AccesstoPA | −0.300 ** | −0.278 ** | 0.387 ** | −0.082 ** | −0.179 ** | −0.594 ** | 0.105 ** | −0.007 | −0.289 ** |
| 16. PoorFairHealth | 0.728 ** | 0.414 ** | −0.664 ** | 0.495 ** | −0.159 ** | 0.088 ** | 0.022 | −0.537 ** | 0.417 ** |
| 17. PhysUnhealthyDays | 0.811 ** | 0.216 ** | −0.624 ** | 0.548 ** | −0.064 ** | 0.121 ** | 0.072 ** | −0.273 ** | 0.391 ** |
| 18. MenUnhealthyDays | 0.756 ** | 0.101 ** | −0.557 ** | 0.490 ** | −0.018 | 0.075 ** | 0.167 ** | −0.144 ** | 0.356 ** |
| 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
| 10. FoodInsecure | --- | ||||||||
| 11. log_Population | −0.048 ** | --- | |||||||
| 12. log_Income | −0.684 ** | 0.405 ** | --- | ||||||
| 13. AirPollution | 0.240 ** | 0.430 ** | −0.036 * | --- | |||||
| 14. WaterPollution | 0.039 * | 0.216 ** | 0.037 * | −0.004 | --- | ||||
| 15. AccesstoPA | −0.261 ** | 0.522 ** | 0.447 ** | 0.000 | 0.119 ** | --- | |||
| 16. PoorFairHealth | 0.708 ** | −0.084 ** | −0.723 ** | 0.284 ** | 0.043 * | −0.341 ** | --- | ||
| 17. PhysUnhealthyDays | 0.702 ** | −0.033 | −0.712 ** | 0.315 ** | 0.058 ** | −0.290 ** | 0.891 ** | --- | |
| 18. MenUnhealthyDays | 0.638 ** | 0.070 ** | −0.621 ** | 0.400 ** | 0.082 ** | −0.234 ** | 0.781 ** | 0.934 ** | --- |
| Model 1a | Model 2a | Model 3a | ||||
|---|---|---|---|---|---|---|
| Variable | B | SE | B | SE | B | SE |
| Smokers | 0.551 *** | 0.015 | 0.541 *** | 0.015 | 0.545 *** | 0.015 |
| Uninsured | 0.068 *** | 0.009 | 0.077 *** | 0.009 | 0.081 *** | 0.009 |
| SomeCollege | −0.067 *** | 0.004 | −0.051 *** | 0.004 | −0.045 *** | 0.004 |
| Unemployed | 0.284 *** | 0.031 | 0.287 *** | 0.03 | 0.294 *** | 0.03 |
| 65plus | −0.069 *** | 0.010 | −0.045 *** | 0.010 | −0.041 *** | 0.010 |
| Rural | −0.007 *** | 0.002 | −0.012 *** | 0.002 | −0.012 *** | 0.002 |
| Female | 0.173 *** | 0.017 | 0.133 *** | 0.016 | 0.126 *** | 0.016 |
| White | −0.080 *** | 0.002 | −0.085 *** | 0.002 | −0.086 *** | 0.002 |
| Obesity | −0.022 ** | 0.007 | −0.037 *** | 0.007 | −0.036 *** | 0.007 |
| FoodInsecure | 0.024 | 0.014 | −0.011 | 0.014 | −0.023 | 0.014 |
| log_Population | −0.36 *** | 0.09 | −0.808 *** | 0.095 | −0.812 *** | 0.095 |
| log_Income | −11.041 *** | 0.648 | −11.58 *** | 0.627 | −11.679 *** | 0.623 |
| AirPollution (AP) | 0.573 *** | 0.042 | 0.6 *** | 0.042 | ||
| WaterPollution (WP) | 0.162 *** | 0.033 | 0.163 *** | 0.032 | ||
| AccesstoPA (APA) | −0.149 ** | 0.044 | −0.198 *** | 0.045 | ||
| AP × APA | −0.209 *** | 0.031 | ||||
| WP × APA | −0.023 | 0.033 | ||||
| Model 1b | Model 2b | Model 3b | ||||
|---|---|---|---|---|---|---|
| Variable | B | SE | B | SE | B | SE |
| Smokers | 0.100 *** | 0.003 | 0.100 *** | 0.003 | 0.101 *** | 0.003 |
| Uninsured | 0.002 | 0.002 | 0.002 | 0.002 | 0.003 | 0.002 |
| SomeCollege | −0.012 *** | 0.001 | −0.011 *** | 0.001 | −0.010 *** | 0.001 |
| Unemployed | 0.069 *** | 0.005 | 0.068 *** | 0.005 | 0.068 *** | 0.005 |
| 65plus | −0.003 | 0.002 | −0.002 | 0.002 | −0.001 | 0.002 |
| Rural | 0.000 | 0.000 | −0.001 * | 0.000 | −0.001 ** | 0.000 |
| Female | 0.026 *** | 0.003 | 0.025 *** | 0.003 | 0.024 *** | 0.003 |
| White | −0.001 | 0.000 | −0.001 * | 0.000 | −0.001 * | 0.000 |
| ObeseAdults | -0.012 *** | 0.001 | −0.013 *** | 0.001 | −0.013 *** | 0.001 |
| FoodInsecure | 0.023 *** | 0.002 | 0.022 *** | 0.002 | 0.021 *** | 0.002 |
| log_Population | 0.100 *** | 0.015 | 0.074 *** | 0.017 | 0.075 *** | 0.017 |
| log_Income | −1.313 *** | 0.111 | −1.314 *** | 0.110 | −1.323 *** | 0.110 |
| AirPollution (AP) | 0.024 *** | 0.007 | 0.026 *** | 0.007 | ||
| WaterPollution (WP) | 0.033 *** | 0.006 | 0.034 *** | 0.006 | ||
| AccesstoPA (PA) | −0.019 * | 0.008 | −0.024 ** | 0.008 | ||
| AP × PA | −0.018 ** | 0.006 | ||||
| WP × PA | −0.005 | 0.006 | ||||
| Model 1c | Model 2c | Model 3c | ||||
|---|---|---|---|---|---|---|
| Variable | B | SE | B | SE | B | SE |
| Smokers | 0.082 *** | 0.003 | 0.082 *** | 0.003 | 0.083 *** | 0.003 |
| Uninsured | −0.001 | 0.002 | 0.000 | 0.002 | 0.000 *** | 0.002 |
| SomeCollege | −0.014 *** | 0.001 | −0.012 *** | 0.001 | −0.011 *** | 0.001 |
| Unemployed | 0.056 *** | 0.005 | 0.054 *** | 0.005 | 0.054 *** | 0.005 |
| 65plus | 0.004 ** | 0.002 | 0.007 *** | 0.002 | 0.007 *** | 0.002 |
| Rural | 0.000 | 0.000 | −0.001 | 0.000 | −0.001 * | 0.000 |
| Female | 0.037 *** | 0.003 | 0.034 *** | 0.003 | 0.033 *** | 0.003 |
| White | 0.003 *** | 0.000 | 0.003 *** | 0.000 | 0.003 *** | 0.000 |
| ObeseAdults | −0.010 *** | 0.001 | −0.012 *** | 0.001 | −0.012 *** | 0.001 |
| FoodInsecure | 0.030 *** | 0.002 | 0.027 *** | 0.002 | 0.026 *** | 0.002 |
| log_Population | 0.189 *** | 0.015 | 0.138 *** | 0.016 | 0.138 *** | 0.016 |
| log_Income | −0.503 *** | 0.109 | −0.527 *** | 0.107 | −0.539 *** | 0.107 |
| AirPollution (AP) | 0.052 *** | 0.007 | 0.055 *** | 0.007 | ||
| WaterPollution (WP) | 0.043 *** | 0.006 | 0.043 *** | 0.006 | ||
| AccesstoPA (PA) | −0.014 | 0.008 | −0.020 ** | 0.008 | ||
| AP × PA | −0.024 *** | 0.005 | ||||
| WP × PA | −0.007 | 0.006 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunningham, G.B.; Wicker, P.; McCullough, B.P. Pollution, Health, and the Moderating Role of Physical Activity Opportunities. Int. J. Environ. Res. Public Health 2020, 17, 6272. https://doi.org/10.3390/ijerph17176272
Cunningham GB, Wicker P, McCullough BP. Pollution, Health, and the Moderating Role of Physical Activity Opportunities. International Journal of Environmental Research and Public Health. 2020; 17(17):6272. https://doi.org/10.3390/ijerph17176272
Chicago/Turabian StyleCunningham, George B., Pamela Wicker, and Brian P. McCullough. 2020. "Pollution, Health, and the Moderating Role of Physical Activity Opportunities" International Journal of Environmental Research and Public Health 17, no. 17: 6272. https://doi.org/10.3390/ijerph17176272






