The WHO and UNICEF Joint Monitoring Programme (JMP) Indicators for Water Supply, Sanitation and Hygiene and Their Association with Linear Growth in Children 6 to 23 Months in East Africa
Abstract
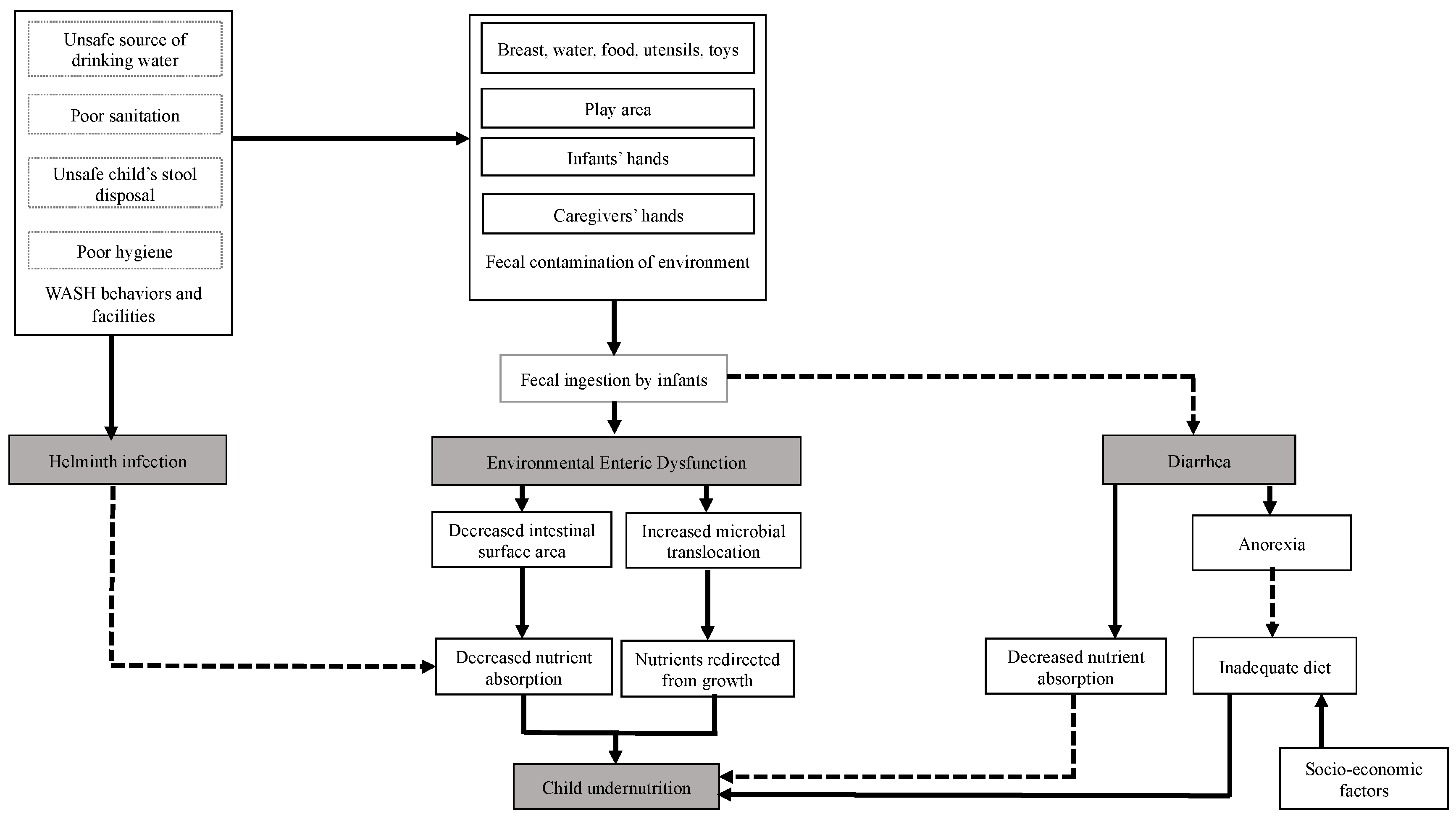
:1. Introduction
2. Methods
2.1. Study Population
2.2. Child Length
2.3. WASH Indicators
2.4. Covariates
2.5. Statistical Analyses
3. Results
3.1. Characteristics of the Study Populations
3.2. WASH Indicators and Child Length
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- UNICEF. Malnutrition in Children—UNICEF Data. Available online: http://data.unicef.org/topic/nutrition/malnutrition/ (accessed on 12 January 2019).
- Smith, L.C.; Haddad, L. Reducing child undernutrition: Past drivers and priorities for the post-MDG era. World Dev. 2015, 68, 180–204. [Google Scholar] [CrossRef] [Green Version]
- Akombi, B.J.; Agho, K.E.; Merom, D.; Renzaho, A.M.; Hall, J.J. Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006–2016). PLoS ONE 2017, 12, e0177338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bryce, J.; Coitinho, D.; Darnton-Hill, I.; Pelletier, D.; Pinstrup-Andersen, P. Maternal and child undernutrition: Effective action at national level. Lancet 2008, 371, 510–526. [Google Scholar] [CrossRef]
- Fregonese, F.; Siekmans, K.; Kouanda, S.; Druetz, T.; Ly, A.; Diabate, S.; Haddad, S. Impact of contaminated household environment on stunting in children aged 12–59 months in Burkina Faso. J. Epidemiol Commun. Health 2017, 71, 356–363. [Google Scholar] [CrossRef] [PubMed]
- van Cooten, M.H.; Bilal, S.M.; Gebremedhin, S.; Spigt, M. The association between acute malnutrition and water, sanitation, and hygiene among children aged 6–59 months in rural Ethiopia. Matern. Child Nutr. 2018, 12631, e12631. [Google Scholar] [CrossRef] [Green Version]
- Spears, D.; Ghosh, A.; Cumming, O. Open defecation and childhood stunting in India: An ecological analysis of new data from 112 districts. PLoS ONE 2013, 8, e73784. [Google Scholar] [CrossRef]
- Spears, D. How Much International Variation in Child Height Can Sanitation Explain? The World Bank: Washington, DC, USA, 2013. [Google Scholar]
- Ngure, F.M.; Reid, B.M.; Humphrey, J.H.; Mbuya, M.N.; Pelto, G.; Stoltzfus, R.J. Water, sanitation, and hygiene (WASH), environmental enteropathy, nutrition, and early child development: Making the links. Ann. N. Y. Acad. Sci. 2014, 1308, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Dearden, K.A.; Schott, W.; Crookston, B.T.; Humphries, D.L.; Penny, M.E.; Behrman, J.R. Children with access to improved sanitation but not improved water are at lower risk of stunting compared to children without access: A cohort study in Ethiopia, India, Peru, and Vietnam. BMC Public Health 2017, 17, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Checkley, W.; Gilman, R.H.; Black, R.E.; Epstein, L.D.; Cabrera, L.; Sterling, C.R.; Moulton, L.H. Effect of water and sanitation on childhood health in a poor Peruvian peri-urban community. Lancet 2004, 363, 112–118. [Google Scholar] [CrossRef]
- Cumming, O. Can water, sanitation and hygiene help eliminate stunting? Current evidence and policy implications. Matern. Child Nutr. 2016, 12, 91–105. [Google Scholar] [CrossRef]
- Checkley, W.; Buckley, G.; Gilman, R.H.; Assis, A.M.; Guerrant, R.L.; Morris, S.S.; Molbak, K.; Valentiner-Branth, P.; Lanata, C.F.; Black, R.E. Multi-country analysis of the effects of diarrhoea on childhood stunting. Int. J. Epidem. 2008, 37, 816–830. [Google Scholar] [CrossRef] [Green Version]
- Humphrey, J.H. Child undernutrition, tropical enteropathy, toilets, and handwashing. Lancet 2009, 374, 1032–1035. [Google Scholar] [CrossRef]
- Keusch, G.T.; Rosenberg, I.H.; Denno, D.M.; Duggan, C.; Guerrant, R.L.; Lavery, J.V.; Tarr, P.I.; Ward, H.D.; Black, R.E.; Nataro, J.P.; et al. Implications of acquired environmental enteric dysfunction for growth and stunting in infants and children living in low- and middle-income countries. Food Nutr. Bull. 2013, 34, 357–364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dangour, A.D.; Watson, L.; Cumming, O.; Boisson, S.; Che, Y.; Velleman, Y.; Cavill, S.; Allen, E.; Uauy, R. Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pickering, A.J.; Null, C.; Winch, P.J.; Mangwadu, G.; Arnold, B.F.; Prendergast, A.J.; Njenga, S.M.; Rahman, M.; Ntozini, R.; Benjamin-Chung, J.; et al. The WASH Benefits and SHINE trials: Interpretation of WASH intervention effects on linear growth and diarrhoea. Lancet Glob. Health 2019, 7, e1139–e1146. [Google Scholar] [CrossRef] [Green Version]
- Cumming, O.; Curtis, V. Implications of WASH Benefits trials for water and sanitation. Lancet Glob. Health 2018, 6, e613–e614. [Google Scholar] [CrossRef] [Green Version]
- WHO; UNICEF. The WHO/UNICEF Joint Monitoring Programme Estimates on WASH. Available online: http://washdata.org (accessed on 2 August 2020).
- Alagidede, P.; Alagidede, A.N. The public health effects of water and sanitation in selected West African countries. Public Health 2016, 130, 59–63. [Google Scholar] [CrossRef]
- Ezbakhe, F.; Pérez-Foguet, A. Estimating access to drinking water and sanitation: The need to account for uncertainty in trend analysis. Sci. Total Environ. 2019, 696, 133830. [Google Scholar] [CrossRef]
- WHO. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Rah, J.H.; Cronin, A.A.; Badgaiyan, B.; Aguayo, V.M.; Coates, S.; Ahmed, S. Household sanitation and personal hygiene practices are associated with child stunting in rural India: A cross-sectional analysis of surveys. BMJ Open 2015, 5, e005180. [Google Scholar] [CrossRef] [PubMed]
- Guerrant, R.L.; DeBoer, M.D.; Moore, S.R.; Scharf, R.J.; Lima, A.A. The impoverished gut—A triple burden of diarrhoea, stunting and chronic disease. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Mbuya, M.N.; Humphrey, J.H. Preventing environmental enteric dysfunction through improved water, sanitation and hygiene: An opportunity for stunting reduction in developing countries. Matern. Child Nutr. 2016, 12 (Suppl. 1), 106–120. [Google Scholar] [CrossRef] [Green Version]
- Kosek, M.N.; Guerrant, R.L.; Kang, G.; Bhutta, Z.; Yori, P.P.; Gratz, J.; Gottlieb, M.; Lang, D.; Lee, G.; Haque, R.; et al. Assessment of environmental enteropathy in the MAL-ED cohort study: Theoretical and analytic framework. Clin. Infect. Dis. 2014, 59 (Suppl. 4), S239–S247. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, L.; Cervantes, E.; Ortiz, R. Malnutrition and gastrointestinal and respiratory infections in children: A public health problem. Int. J. Environ. Res. Public Health 2011, 8, 1174–1205. [Google Scholar] [CrossRef] [Green Version]
- Kosek, M.N. The MAL-Ed Network Investiagtors. Causal pathways from enteropathogens to environmental enteropathy: Findings from the MAL-ED birth cohort study. EBioMedicine 2017, 18, 109–117. [Google Scholar] [CrossRef]
- Young, S.L.; Collins, S.M.; Boateng, G.O.; Neilands, T.B.; Jamaluddine, Z.; Miller, J.D.; Brewis, A.A.; Frongillo, E.A.; Jepson, W.E.; Melgar-Quiñonez, H.; et al. Development and validation protocol for an instrument to measure household water insecurity across cultures and ecologies: The Household Water InSecurity Experiences (HWISE) Scale. BMJ Open 2019, 9, e023558. [Google Scholar] [CrossRef]
- Young, S.L.; Boateng, G.O.; Jamaluddine, Z.; Miller, J.D.; Frongillo, E.A.; Neilands, T.B.; Collins, S.M.; Wutich, A.; Jepson, W.E.; Stoler, J. The Household Water InSecurity Experiences (HWISE) Scale: Development and validation of a household water insecurity measure for low-income and middle-income countries. BMJ Glob. Health 2019, 4, e001750. [Google Scholar] [CrossRef]
- Brewis, A.; Workman, C.; Wutich, A.; Jepson, W.; Young, S. Household water insecurity is strongly associated with food insecurity: Evidence from 27 sites in low- and middle-income countries. Am. J. Hum. Biol. 2020, 32, e23309. [Google Scholar] [CrossRef] [Green Version]
- Headey, D.; Nguyen, P.; Kim, S.; Rawat, R.; Ruel, M.; Menon, P. Is exposure to animal feces harmful to child nutrition and health outcomes? A multicountry observational analysis. Am. J. Trop. Med. Hyg. 2017, 96, 961–969. [Google Scholar] [CrossRef] [Green Version]
- Headey, D.; Hirvonen, K. Is Exposure to Poultry Harmful to Child Nutrition? An Observational Analysis for Rural Ethiopia. PLoS ONE 2016, 11, e0160590. [Google Scholar] [CrossRef] [PubMed]
- Luby, S.P.; Rahman, M.; Arnold, B.F.; Unicomb, L.; Ashraf, S.; Winch, P.J.; Stewart, C.P.; Begum, F.; Hussain, F.; Benjamin-Chung, J.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: A cluster randomised controlled trial. Lancet Glob. Health 2018, 6, e302–e315. [Google Scholar] [CrossRef] [Green Version]
- Null, C.; Stewart, C.P.; Pickering, A.J.; Dentz, H.N.; Arnold, B.F.; Arnold, C.D.; Benjamin-Chung, J.; Clasen, T.; Dewey, K.G.; Fernald, L.C.H.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: A cluster-randomised controlled trial. Lancet Glob. Health 2018, 6, e316–e329. [Google Scholar] [CrossRef] [Green Version]
- Humphrey, J.H.; Mbuya, M.N.N.; Ntozini, R.; Moulton, L.H.; Stoltzfus, R.J.; Tavengwa, N.V.; Mutasa, K.; Majo, F.; Mutasa, B.; Mangwadu, G.; et al. Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: A cluster-randomised trial. Lancet Glob. Health 2019, 7, e132–e147. [Google Scholar] [CrossRef] [Green Version]
- Dreibelbis, R.; Winch, P.J.; Leontsini, E.; Hulland, K.R.; Ram, P.K.; Unicomb, L.; Luby, S.P. The Integrated Behavioural Model for Water, Sanitation, and Hygiene: A systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC Public Health 2013, 13, 1015. [Google Scholar] [CrossRef] [Green Version]
| Country | Burundi | Ethiopia | Kenya | Malawi | Rwanda | Tanzania | Uganda | Zambia |
|---|---|---|---|---|---|---|---|---|
| Original datasets | 6493 | 10,937 | 21,718 | 6102 | 3926 | 10,898 | 5561 | 13,939 |
| Datasets with observations for WASH variables | 4536 | 5082 | 6641 | 3423 | 2511 | 4341 | 2641 | 5575 |
| Final datasets (observations without anthropometric measurements deleted) | 2226 | 2451 | 3978 | 1631 | 1177 | 2770 | 1370 | 2963 |
| Ladder | Characteristics |
|---|---|
| WATER | |
| Surface water | River, dam, lake, pond, stream, canal, or irrigation canal |
| Unimproved | Unprotected dug well or unprotected spring |
| Limited | Improved source 1 and collection time exceeds 30 min |
| Basic | Improved source 1 and collection time is no more than 30 min for roundtrip |
| Safely managed | Improved source 1 and available on premises and available when needed and free from fecal and chemical contamination 2 |
| SANITATION | |
| Open defecation | Disposal of human feces in fields, forests, bushes, open bodies of water, beaches and other open spaces, or with solid waste |
| Unimproved | Pit latrines without a slab, hanging latrines, or bucket latrines |
| Limited | Improved facilities 3 and shared between two or more households |
| Basic | Improved facilities 3 and not shared with other households |
| Safely managed (not included in analyses in this paper) | Improved facilities 3 and not shared with other households and extra excreta are safely disposed in situ or transported and treated off-site |
| HYGIENE | |
| No facility | No handwashing facility on premises |
| Limited | Handwashing facility on premises without soap and water |
| Basic | Handwashing facility on premises with soap and water |
| Burundi | Ethiopia | Kenya | Malawi | Rwanda | Tanzania | Uganda | Zambia | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 2226 | 2451 | 3978 | 1631 | 1177 | 2770 | 1370 | 2963 | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Child Characteristics | ||||||||||||||||
| Sex | ||||||||||||||||
| Male | 1113 | 50.0 | 1150 | 46.9 | 1935 | 48.6 | 811 | 49.7 | 578 | 49.1 | 1387 | 50.1 | 691 | 50.4 | 1462 | 49.3 |
| Female | 1112 | 50.0 | 1301 | 53.1 | 2043 | 51.4 | 820 | 50.3 | 599 | 50.9 | 1383 | 49.9 | 679 | 49.6 | 1501 | 50.7 |
| Stunting | 1002 | 45.0 | 697 | 28.4 | 815 | 20.5 | 509 | 31.2 | 351 | 29.8 | 764 | 27.6 | 348 | 25.4 | 1068 | 36.1 |
| Mean LAZ (SD) | −1.8 (1.2) | −0.8 (1.7) | −0.9 (1.4) | −1.2 (1.3) | −1.2 (1.5) | −1.2 (1.4) | −1.0 (1.5) | −1.3 (1.6) | ||||||||
| Stunting rates | 1002 | 45.0 | 697 | 28.4 | 815 | 20.5 | 509 | 31.2 | 351 | 29.8 | 764 | 27.6 | 348 | 25.4 | 1068 | 36.1 |
| Diarrhea in the past 2 weeks | 685 | 31.0 | 405 | 16.5 | 864 | 21.7 | 491 | 30.1 | 203 | 17.2 | 449 | 16.2 | 438 | 32.0 | 629 | 21.2 |
| Currently breastfed | 2084 | 93.6 | 2261 | 92.2 | 1820 | 45.7 | 1433 | 87.4 | 1138 | 96.7 | 2483 | 89.6 | 1144 | 83.5 | 2461 | 89.1 |
| Maternal and Household Characteristics | ||||||||||||||||
| Highest education level | ||||||||||||||||
| No education | 975 | 43.8 | 1483 | 60.5 | 423 | 10.6 | 181 | 11.1 | 137 | 11.6 | 537 | 19.4 | 130 | 9.5 | 321 | 10.8 |
| primary | 970 | 43.6 | 759 | 31.0 | 2150 | 54.0 | 1086 | 66.6 | 854 | 72.6 | 1765 | 63.7 | 810 | 59.1 | 1162 | 54.5 |
| Secondary | 271 | 12.1 | 151 | 6.2 | 1022 | 25.7 | 332 | 20.3 | 160 | 13.6 | 438 | 15.8 | 334 | 24.4 | 936 | 31.6 |
| Higher | 9 | 0.4 | 58 | 2.3 | 383 | 9.6 | 32 | 1.9 | 26 | 2.2 | 30 | 1.1 | 96 | 7.0 | 90 | 3.0 |
| Wealth index | ||||||||||||||||
| Poorest | 461 | 20.7 | 862 | 35.2 | 936 | 23.5 | 401 | 24.6 | 306 | 26.0 | 676 | 14.4 | 284 | 20.7 | 756 | 25.5 |
| Poor | 491 | 22.1 | 419 | 17.1 | 698 | 17.5 | 388 | 23.8 | 238 | 20.2 | 588 | 21.2 | 276 | 20.1 | 715 | 24.1 |
| Middle | 474 | 21.3 | 359 | 14.6 | 669 | 16.8 | 330 | 20.2 | 224 | 19.1 | 513 | 18.5 | 272 | 20.0 | 633 | 21.4 |
| Wealthier | 435 | 19.6 | 317 | 12.9 | 704 | 17.7 | 261 | 16.0 | 202 | 17.1 | 518 | 18.7 | 236 | 17.2 | 521 | 17.6 |
| Wealthiest | 365 | 16.4 | 494 | 20.2 | 970 | 24.4 | 251 | 15.4 | 207 | 17.6 | 475 | 17.1 | 301 | 22.0 | 338 | 11.4 |
| Area of residence | ||||||||||||||||
| Urban | 200 | 9.0 | 454 | 18.5 | 1622 | 40.8 | 216 | 13.2 | 205 | 17.4 | 759 | 27.4 | 295 | 21.5 | 896 | 30.2 |
| Rural | 2026 | 91.0 | 1997 | 81.5 | 2356 | 59.2 | 1415 | 86.8 | 972 | 82.6 | 2011 | 72.6 | 1075 | 78.5 | 2067 | 69.7 |
| WASH Indicators (JMP ladder) | ||||||||||||||||
| Drinking water | ||||||||||||||||
| Surface water | 116 | 5.3 | 272 | 11.1 | 702 | 18.1 | 51 | 3.1 | 123 | 10.4 | 388 | 14.0 | 129 | 9.5 | 358 | 12.2 |
| Unimproved | 296 | 13.2 | 769 | 31.4 | 411 | 10.6 | 187 | 11.6 | 193 | 16.4 | 750 | 27.1 | 164 | 12.0 | 885 | 30.3 |
| Limited | 726 | 30.4 | 628 | 25.7 | 552 | 14.2 | 593 | 36.6 | 392 | 33.3 | 546 | 19.8 | 566 | 41.6 | 361 | 12.4 |
| Basic | 917 | 40.7 | 503 | 20.6 | 953 | 24.5 | 593 | 36.6 | 355 | 30.2 | 472 | 17.1 | 305 | 22.4 | 877 | 30.0 |
| Safely managed | 170 | 10.4 | 273 | 11.2 | 1268 | 32.6 | 195 | 12.0 | 112 | 9.6 | 608 | 22.0 | 197 | 14.5 | 442 | 15.1 |
| Missing | 1 | 6 | 91 | 12 | 1 | 6 | 9 | 40 | ||||||||
| Sanitation | ||||||||||||||||
| Open defecation | 49 | 2.2 | 890 | 36.4 | 605 | 15.3 | 94 | 5.6 | 42 | 3.5 | 354 | 22.2 | 111 | 8.1 | 625 | 21.1 |
| Unimproved | 1003 | 45.0 | 1334 | 54.5 | 1388 | 35.0 | 211 | 12.9 | 303 | 25.8 | 484 | 30.3 | 724 | 53.1 | 1174 | 39.7 |
| Limited | 227 | 10.2 | 119 | 4.85 | 1174 | 29.6 | 528 | 32.4 | 209 | 17.8 | 338 | 21.2 | 253 | 18.5 | 476 | 16.1 |
| Basic | 947 | 42.5 | 103 | 4.2 | 793 | 20.0 | 798 | 48.9 | 620 | 52.8 | 419 | 26.3 | 277 | 20.3 | 683 | 23.1 |
| Missing | 0 | 0 | 5 | 17 | 3 | 1175 | 5 | 5 | ||||||||
| Hygiene | ||||||||||||||||
| No handwashing facility | 20 | 0.9 | 1105 | 45.2 | 30 | 4.8 | 266 | 16.4 | 8 | 6.4 | 464 | 16.7 | 541 | 39.7 | 43 | 4.1 |
| Limited | 2084 | 93.6 | 1180 | 48.3 | 351 | 57.0 | 1195 | 73.7 | 82 | 65.4 | 1028 | 37.1 | 468 | 34.3 | 732 | 70.0 |
| Basic | 121 | 5.5 | 158 | 6.4 | 235 | 38.1 | 161 | 9.9 | 35 | 28.2 | 1278 | 46.1 | 355 | 26.0 | 271 | 25.9 |
| Missing | 1 | 8 | 3362 | 9 | 1051 | 6 | 1917 | |||||||||
| Countries | JMP Ladder | Model I | Model II | R2 | Model III | R2 |
|---|---|---|---|---|---|---|
| Burundi | Unimproved | −0.03 | −0.06 | 0.25 | −0.06 | 0.25 |
| Limited | 0.01 | −0.04 | −0.04 | |||
| Basic | 0.03 | −0.02 | −0.02 | |||
| Safely managed | 0.19 *** | 0.06 | 0.07 | |||
| Ethiopia | Unimproved | −0.02 | 0.01 | 0.21 | 0.01 | 0.22 |
| Limited | −0.05 | −0.02 | −0.01 | |||
| Basic | −0.08 | −0.06 | −0.05 | |||
| Safely managed | 0.70 | 0.05 | 0.05 | |||
| Kenya | Unimproved | 0.04 | 0.01 | 0.20 | 0.01 | 0.21 |
| Limited | 0.05 * | 0.02 | 0.03 | |||
| Basic | 0.07 ** | 0.01 | 0.02 | |||
| Safely managed | 0.18 *** | 0.13 ** | 0.13 ** | |||
| Malawi | Unimproved | 0.04 | 0.03 | 0.09 | 0.03 | 0.10 |
| Limited | 0.11 | 0.07 | 0.08 | |||
| Basic | 0.06 | 0.02 | 0.03 | |||
| Safely managed | 0.12 * | 0.04 | 0.05 | |||
| Rwanda | Unimproved | −0.11 * | −0.10 ** | 0.23 | −0.10 ** | 0.23 |
| Limited | −0.07 | −0.05 | −0.05 | |||
| Basic | −0.02 | −0.02 | −0.02 | |||
| Safely managed | 0.07 | 0.01 | 0.01 | |||
| Tanzania | Unimproved | 0.03 | 0.02 | 0.24 | 0.03 | 0.24 |
| Limited | 0.11 | −0.02 | −0.01 | |||
| Basic | 0.06 | 0.02 | 0.02 | |||
| Safely managed | 0.14 *** | 0.08 * | 0.07 * | |||
| Uganda | Unimproved | 0.05 | 0.03 | 0.22 | 0.03 | 0.22 |
| Limited | 0.10 | 0.03 | 0.02 | |||
| Basic | 0.04 | 0.01 | 0.01 | |||
| Safely managed | 0.10* | 0.02 | 0.01 | |||
| Zambia | Unimproved | 0.01 | -0.01 | 0.20 | 0.01 | 0.20 |
| Limited | 0.04 | 0.03 | 0.03 | |||
| Basic | 0.04 | 0.01 | 0.01 | |||
| Safely managed | 0.13 *** | 0.05 | 0.05 |
| Countries | JMP Ladder | Model I | Model II | R2 | Model III | R2 |
|---|---|---|---|---|---|---|
| Burundi | Unimproved | 0.11 | 0.05 | 0.24 | 0.06 | 0.25 |
| Limited | 0.17 *** | 0.05 | 0.05 | |||
| Basic | 0.20 ** | 0.08 | 0.08 | |||
| Ethiopia | Unimproved | 0.06 | 0.08 ** | 0.21 | 0.09 ** | 0.22 |
| Limited | 0.06 * | 0.07 ** | 0.05* | |||
| Basic | 0.08 *** | 0.07 ** | 0.06 ** | |||
| Kenya | Unimproved | 0.05 * | −0.08 * | 0.20 | −0.08 * | 0.21 |
| Limited | 0.14 *** | −0.01 | −0.01 | |||
| Basic | 0.13 *** | −0.01 | −0.01 | |||
| Malawi | Unimproved | 0.03 | 0.02 | 0.09 | 0.03 | 0.10 |
| Limited | 0.02 | −0.04 | −0.04 | |||
| Basic | 0.02 | −0.02 | −0.02 | |||
| Rwanda | Unimproved | −0.02 | −0.02 | 0.23 | −0.02 | 0.23 |
| Limited | 0.03 | −0.08 | −0.07 | |||
| Basic | 0.06 | −0.05 | −0.04 | |||
| Tanzania | Unimproved | −0.04 | −0.04 * | 0.24 | −0.04 * | 0.24 |
| Limited | 0.09 *** | 0.07 * | 0.06 * | |||
| Basic | 0.11 *** | 0.08 ** | 0.06 * | |||
| Uganda | Unimproved | 0.01 | 0.03 | 0.22 | 0.03 | 0.22 |
| Limited | 0.08 | 0.09 | 0.10 | |||
| Basic | 0.12 * | 0.11 * | 0.11 * | |||
| Zambia | Unimproved | 0.04 | 0.02 | 0.20 | 0.02 | 0.20 |
| Limited | 0.08 ** | 0.04 | 0.04 | |||
| Basic | 0.06 | 0.02 | 0.02 |
| Countries | JMP Ladder | Model I | Model II | R2 | Model III | R2 |
|---|---|---|---|---|---|---|
| Burundi | Limited | −0.19 | −0.02 | 0.24 | −0.02 | 0.25 |
| Basic | 0.41 | −0.03 | −0.04 | |||
| Ethiopia | Limited | −0.03 | −0.03 | 0.21 | −0.03 | 0.25 |
| Basic | 0.08 * | 0.05 | 0.04 | |||
| Malawi | Limited | 0.04 | 0.02 | 0.09 | 0.03 | 0.09 |
| Basic | 0.07 | 0.05 | 0.05 | |||
| Tanzania | Limited | −0.01 | −0.02 | 0.23 | −0.02 | 0.24 |
| Basic | 0.08 *** | 0.03 | 0.03 | |||
| Uganda | Limited | 0.04 | −0.01 | 0.22 | −0.01 | 0.22 |
| Basic | 0.05 | 0.01 | 0.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rakotomanana, H.; Komakech, J.J.; Walters, C.N.; Stoecker, B.J. The WHO and UNICEF Joint Monitoring Programme (JMP) Indicators for Water Supply, Sanitation and Hygiene and Their Association with Linear Growth in Children 6 to 23 Months in East Africa. Int. J. Environ. Res. Public Health 2020, 17, 6262. https://doi.org/10.3390/ijerph17176262
Rakotomanana H, Komakech JJ, Walters CN, Stoecker BJ. The WHO and UNICEF Joint Monitoring Programme (JMP) Indicators for Water Supply, Sanitation and Hygiene and Their Association with Linear Growth in Children 6 to 23 Months in East Africa. International Journal of Environmental Research and Public Health. 2020; 17(17):6262. https://doi.org/10.3390/ijerph17176262
Chicago/Turabian StyleRakotomanana, Hasina, Joel J. Komakech, Christine N. Walters, and Barbara J. Stoecker. 2020. "The WHO and UNICEF Joint Monitoring Programme (JMP) Indicators for Water Supply, Sanitation and Hygiene and Their Association with Linear Growth in Children 6 to 23 Months in East Africa" International Journal of Environmental Research and Public Health 17, no. 17: 6262. https://doi.org/10.3390/ijerph17176262
APA StyleRakotomanana, H., Komakech, J. J., Walters, C. N., & Stoecker, B. J. (2020). The WHO and UNICEF Joint Monitoring Programme (JMP) Indicators for Water Supply, Sanitation and Hygiene and Their Association with Linear Growth in Children 6 to 23 Months in East Africa. International Journal of Environmental Research and Public Health, 17(17), 6262. https://doi.org/10.3390/ijerph17176262





