Traffic Noise and Mental Health: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Question and Study Eligibility
2.2. Information Sources and Search
2.3. Study Selection and Data Collection
- study design,
- region,
- study population size,
- population characteristics (age and sex distributions),
- population sampling information (recruitment times, response and follow-up),
- outcomes considered and how they were assessed (instruments used),
- noise exposure sources considered,
- noise assessment, including the noise levels considered, and
- study results.
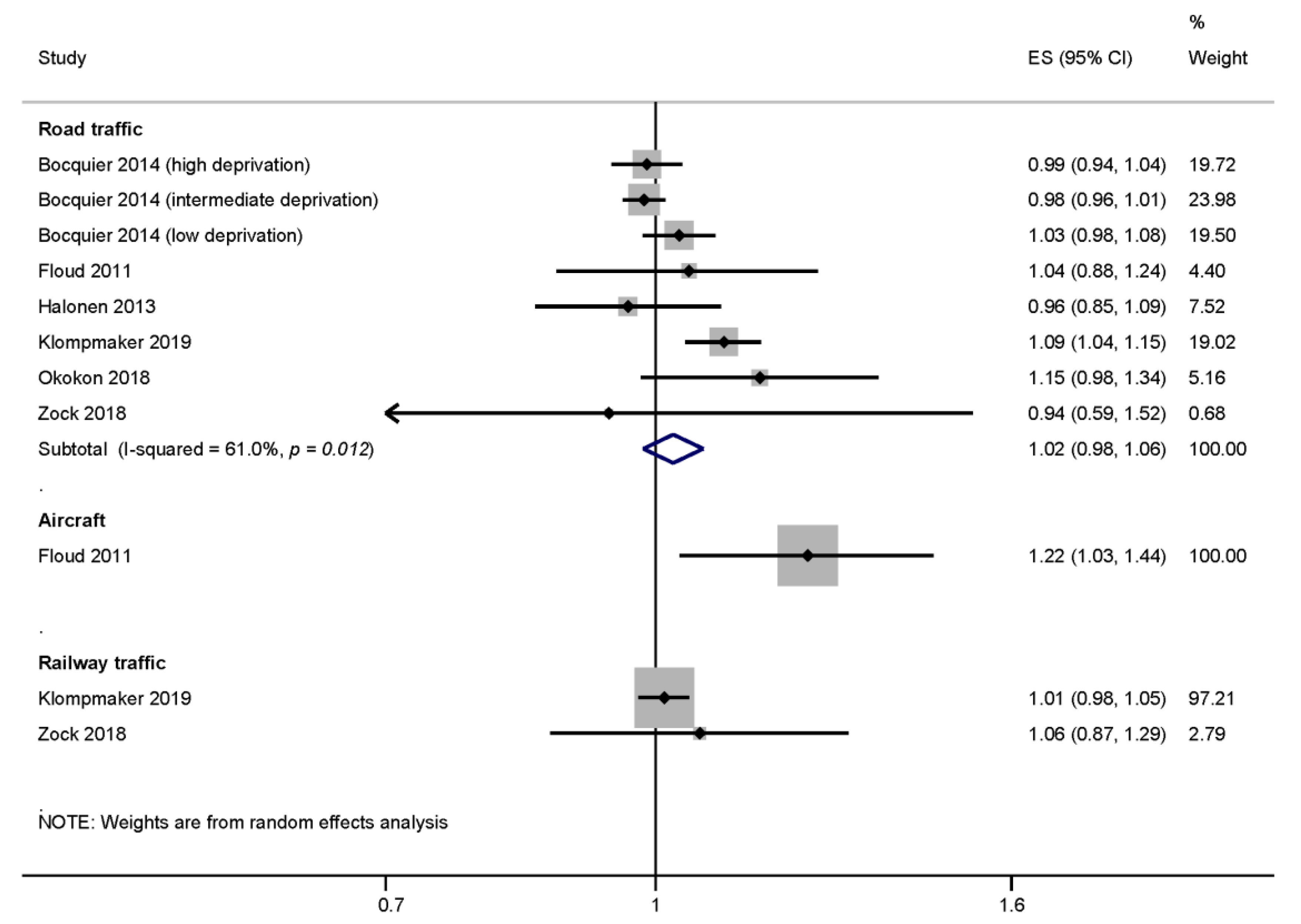
2.4. Meta-Analysis
- If risk estimates were reported for categories of noise, study-specific risk estimates per 10 dB linear increase of traffic noise were estimated by applying the generalized least-squares model for trend estimation of summarized dose-response data using the glst Stata package [16]. The generalized least squares for trend estimation takes into account the fact that the risk estimates from a single study do not fulfill the assumption of independence required of weighted linear regression. A generalized least-squares model was estimated for each applicable study separately as a fixed-effect model using the logarithm of the risk estimates as the dependent variable and average of the noise level categories (with the reference group set to zero) as the independent variable. If necessary, noise exposure values were converted to day-evening-night weighted-24 h means (LDEN) according to Brink et al. [17] prior to the modeling (see Table 2).
- The reported and self-calculated risk estimates per 10 dB Lden were pooled using a DerSimonian and Laird random-effects meta-analysis. The random-effects model was chosen because heterogeneity between study populations can be expected. This method weights each effect estimate by the inverse of its (within-study) variation and the heterogeneity between studies (between-study variation). The Stata package metan was used to conduct the random-effects meta-analysis and to create forest plots [18].
3. Results
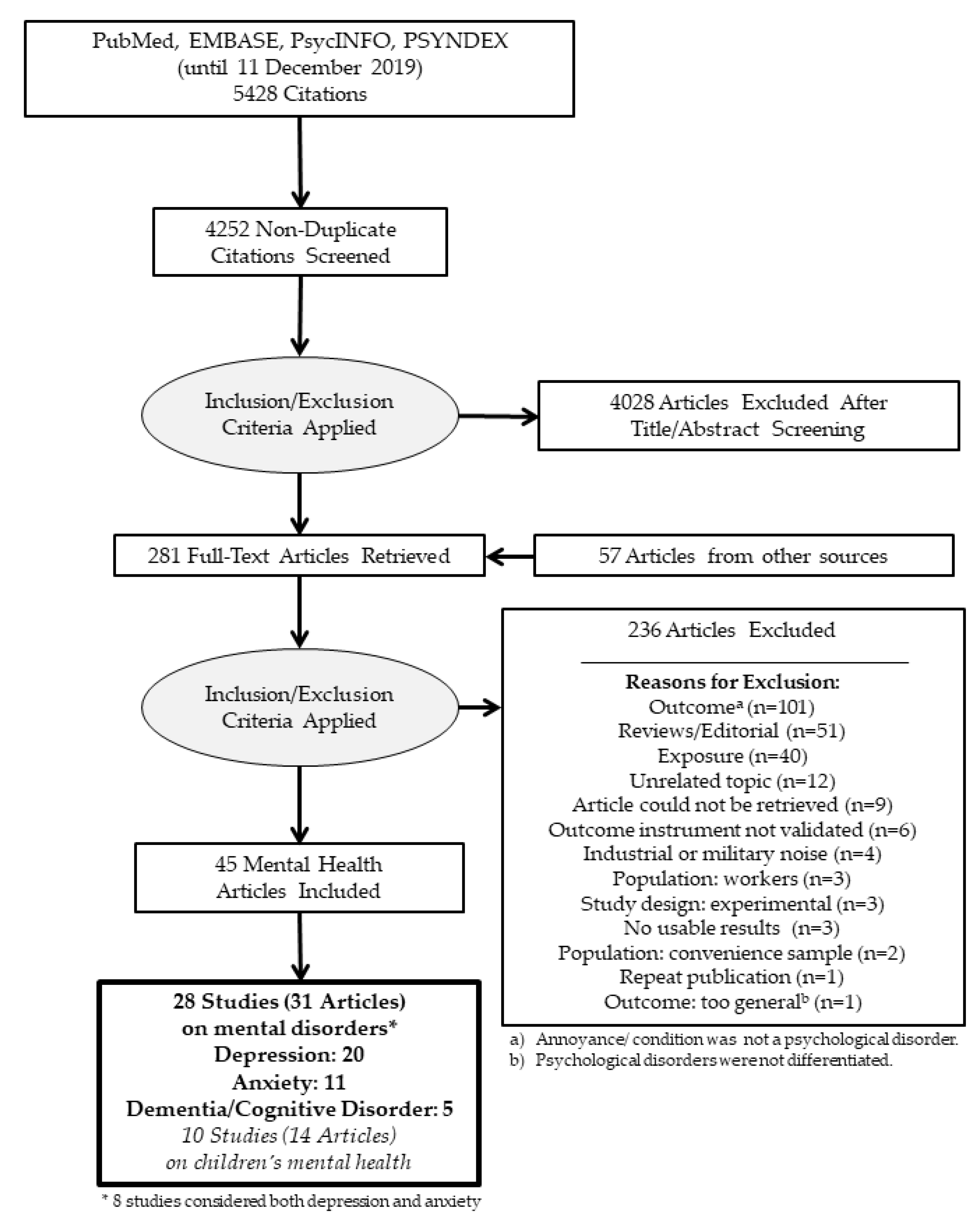
3.1. Study Selection
3.2. Depression
3.2.1. Synthesis of Results
3.2.2. Risk of Bias across Studies
3.3. Anxiety Disorders
3.3.1. Synthesis of Results for the Meta-Analysis
3.3.2. Risk of Bias across Studies
3.4. Dementia and Alzheimer’s Disease
Synthesis of Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- European Environment Agency. Environmental Noise in Europe—2020; European Environment Agency: Luxembourg, 2020. [Google Scholar]
- World Health Organization (WHO). Environmental Noise Guidelines for the European Region; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Clark, C.; Paunovic, K. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Quality of Life, Wellbeing and Mental Health. Int. J. Environ. Res. Public Health 2018, 15, 2400. [Google Scholar] [CrossRef] [Green Version]
- Clark, C.; Paunovic, K. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Cognition. Int. J. Environ. Res. Public Health 2018, 15, 285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, C.; Crumpler, C.; Notley, H. Evidence for Environmental Noise Effects on Health for the United Kingdom Policy Context: A Systematic Review of the Effects of Environmental Noise on Mental Health, Wellbeing, Quality of Life, Cancer, Dementia, Birth, Reproductive Outcomes, and Cognition. Int. J. Environ. Res. Public Health 2020, 17, 393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dzhambov, A.M.; Lercher, P. Road Traffic Noise Exposure and Depression/Anxiety: An Updated Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beutel, M.E.; Junger, C.; Klein, E.M.; Wild, P.; Lackner, K.; Blettner, M.; Binder, H.; Michal, M.; Wiltink, J.; Brahler, E.; et al. Noise Annoyance Is Associated with Depression and Anxiety in the General Population–The Contribution of Aircraft Noise. PLoS ONE 2016, 11, e0155357. [Google Scholar] [CrossRef]
- Guski, R.; Schreckenberg, D.; Schuemer, R. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Annoyance. Int. J. Environ. Res. Public Health 2017, 14, 1539. [Google Scholar] [CrossRef] [Green Version]
- Brink, M.; Schaffer, B.; Vienneau, D.; Foraster, M.; Pieren, R.; Eze, I.C.; Cajochen, C.; Probst-Hensch, N.; Roosli, M.; Wunderli, J.M. A survey on exposure-response relationships for road, rail, and aircraft noise annoyance: Differences between continuous and intermittent noise. Environ. Int. 2019, 125, 277–290. [Google Scholar] [CrossRef]
- Elmenhorst, E.M.; Griefahn, B.; Rolny, V.; Basner, M. Comparing the Effects of Road, Railway, and Aircraft Noise on Sleep: Exposure(-) Response Relationships from Pooled Data of Three Laboratory Studies. Int. J. Environ. Res. Public Health 2019, 16, 1073. [Google Scholar] [CrossRef] [Green Version]
- Basner, M.; Muller, U.; Elmenhorst, E.M. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep 2011, 34, 11–23. [Google Scholar] [CrossRef] [Green Version]
- Seidler, A.; Hegewald, J.; Seidler, A.L.; Schubert, M.; Wagner, M.; Droge, P.; Haufe, E.; Schmitt, J.; Swart, E.; Zeeb, H. Association between aircraft, road and railway traffic noise and depression in a large case-control study based on secondary data. Environ. Res. 2017, 152, 263–271. [Google Scholar] [CrossRef]
- Schubert, M.; Hegewald, J.; Freiberg, A.; Starke, K.R.; Augustin, F.; Riedel-Heller, S.G.; Zeeb, H.; Seidler, A. Behavioral and Emotional Disorders and Transportation Noise among Children and Adolescents: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 3336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weihofen, V.M.; Hegewald, J.; Euler, U.; Schlattmann, P.; Zeeb, H.; Seidler, A. Aircraft Noise and the Risk of Stroke: A Systematic Review and Meta-analysis. Dtsch. Arztebl. Int. 2019, 116, 237. [Google Scholar] [PubMed]
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Nicola, O.; Bellocco, R.; Greenland, S. GLST: Stata Module for Trend Estimation of Summarized Dose-Response Data; S452001; Boston College Department of Economics: Boston, MA, USA, 2005. [Google Scholar]
- Brink, M.; Schaffer, B.; Pieren, R.; Wunderli, J.M. Conversion between noise exposure indicators Leq24h, LDay, LEvening, LNight, Ldn and Lden: Principles and practical guidance. Int. J. Hyg. Environ. Health 2018, 221, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.; Bradburn, M.; Deeks, J.; Harbord, R.; Altman, D.; Sterne, J. Metan: Fixed- and random-effects meta-analysis. Stata J. 2008, 8, 3–28. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Babisch, W. Gesundheitliche Wirkungen von Umweltlärm. Ein Beitrag zur Standortbestimmung. Zeitschrift Lärmbekämpf. 2000, 47, 95–102. [Google Scholar]
- Banerjee, D. Research on road traffic noise and human health in India: Review of literature from 1991 to current. Noise Health 2012, 14, 113–118. [Google Scholar] [PubMed]
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and non-auditory effects of noise on health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef] [Green Version]
- Basner, M.; Brink, M.; Bristow, A.; de Kluizenaar, Y.; Finegold, L.; Hong, J.; Janssen, S.A.; Klaeboe, R.; Leroux, T.; Liebl, A.; et al. ICBEN review of research on the biological effects of noise 2011–2014. Noise Health 2015, 17, 57–82. [Google Scholar] [CrossRef] [Green Version]
- Clark, C.; Stansfeld, S.A. The effect of transportation noise on health and cognitive development: A review of recent evidence. Int. J. Comp. Psychol. 2007, 20, 145–158. [Google Scholar]
- de Jong, R.G. Review: Extraaural health effects of aircraft noise. Schriftenr Ver Wasser Boden Lufthyg. 1993, 88, 250–270. [Google Scholar] [PubMed]
- de Jong, R.G. Community response to noise: A review of recent developments. Environ. Int. 1990, 16, 515–522. [Google Scholar] [CrossRef]
- Ising, H.; Rebentisch, E. Zur Wirkung von Lärm auf den Menschen. Psychomed 1992, 4, 274–278. [Google Scholar]
- Ising, H.; Kruppa, B. Health effects caused by noise: Evidence in the literature from the past 25 years. Noise Health 2004, 6, 5–13. [Google Scholar]
- Kaltenbach, M.; Maschke, C.; Klinke, R. Health consequences of aircraft noise. Dtsch. Arztebl. Int. 2008, 105, 548–556. [Google Scholar] [CrossRef] [Green Version]
- Knipschild, P. VIII. Medical effects of aircraft noise: Review and literature. Int. Arch. Occup. Environ. Health 1977, 40, 201–204. [Google Scholar] [CrossRef]
- Laszlo, H.E.; McRobie, E.S.; Stansfeld, S.A.; Hansell, A.L. Annoyance and other reaction measures to changes in noise exposure–A review. Sci. Total Environ. 2012, 435–436, 551–562. [Google Scholar] [CrossRef]
- Lekaviciute, J.; Argalasova-Sobotova, L. Environmental noise and annoyance in adults: Research in Central, Eastern and South-Eastern Europe and Newly Independent States. Noise Health 2013, 15, 42–54. [Google Scholar] [CrossRef]
- Morrell, S.; Taylor, R.; Lyle, D. A review of health effects of aircraft noise. Aust. N. Z. J. Public Health 1997, 21, 221–236. [Google Scholar] [CrossRef]
- Schuemer, R.; Schuemer-Kohrs, A. Comparison of the annoyance due to railway noise and due to noise from other sources–A review of literature. Zeitschrift Lärmbekämpf. 1991, 38, 1–9. [Google Scholar]
- van Kamp, I.; Davies, H. Noise and health in vulnerable groups: A review. Noise Health 2013, 15, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Baudin, C.; Lefevre, M.; Champelovier, P.; Lambert, J.; Laumon, B.; Evrard, A.S. Aircraft noise and psychological Ill-health: The results of a cross-sectional study in France. Int. J. Environ. Res. Public Health 2018, 15, 1642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Floud, S.; Vigna-Taglianti, F.; Hansell, A.; Blangiardo, M.; Houthuijs, D.; Breugelmans, O.; Cadum, E.; Babisch, W.; Selander, J.; Pershagen, G.; et al. Medication use in relation to noise from aircraft and road traffic in six European countries: Results of the HYENA study. Occup. Environ. Med. 2011, 68, 518–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Generaal, E.; Timmermans, E.J.; Dekkers, J.E.C.; Smit, J.H.; Penninx, B. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychol. Med. 2019, 49, 149–161. [Google Scholar] [CrossRef] [Green Version]
- Generaal, E.; Hoogendijk, E.O.; Stam, M.; Henke, C.E.; Rutters, F.; Oosterman, M.; Huisman, M.; Kramer, S.E.; Elders, P.J.; Timmermans, E.J. Neighbourhood characteristics and prevalence and severity of depression: Pooled analysis of eight Dutch cohort studies. Br. J. Psychiatry 2019, 215, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Greiser, E.; Greiser, C. Risikofaktor Nächtlicher Fluglärm: Abschlussbericht Über Eine Fall-Kontroll-Studie zu Kardiovaskulären und Psychischen Erkrankungen im Umfeld des Flughafens Köln-Bonn; 3708 51 101; Umweltbundesamt: Dessau-Roßlau, Germany, 2010. [Google Scholar]
- Halonen, J.I.; Lanki, T.; Yli-Tuomi, T.; Turunen, A.W.; Pentti, J.; Kivimaki, M.; Vahtera, J. Associations of traffic noise with self-rated health and psychotropic medication use. Scand. J. Work Environ. Health 2014, 40, 235–243. [Google Scholar] [CrossRef] [Green Version]
- Leijssen, J.B.; Snijder, M.B.; Timmermans, E.J.; Generaal, E.; Stronks, K.; Kunst, A.E. The association between road traffic noise and depressed mood among different ethnic and socioeconomic groups. The HELIUS study. Int. J. Hyg. Environ. Health 2019, 222, 221–229. [Google Scholar] [CrossRef]
- Miyakawa, M.; Matsui, T.; Hiramatsu, K. Relationship between psychiatric disorder and disturbances of daily life to aircraft noise exposure-epidemiological study around Narita international airport. In INTER-NOISE and NOISE-CON Congress and Conference Proceedings; Institute of Noise Control Engineering: Istanbul, Turkey, 2007; pp. 3752–3759. [Google Scholar]
- Klompmaker, J.O.; Hoek, G.; Bloemsma, L.D.; Wijga, A.H.; van den Brink, C.; Brunekreef, B.; Lebret, E.; Gehring, U.; Janssen, N.A. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ. Int. 2019, 129, 525–537. [Google Scholar] [CrossRef]
- Okokon, E.O.; Yli-Tuomi, T.; Turunen, A.W.; Tiittanen, P.; Juutilainen, J.; Lanki, T. Traffic noise, noise annoyance and psychotropic medication use. Environ. Int. 2018, 119, 287–294. [Google Scholar] [CrossRef]
- Orban, E.; McDonald, K.; Sutcliffe, R.; Hoffmann, B.; Fuks, K.B.; Dragano, N.; Viehmann, A.; Erbel, R.; Jockel, K.H.; Pundt, N.; et al. Residential Road Traffic Noise and High Depressive Symptoms after Five Years of Follow-up: Results from the Heinz Nixdorf Recall Study. Environ. Health Perspect. 2016, 124, 578–585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreckenberg, D.; Eikmann, T.; Heer, C.; zur Nieden, A.; Heudorf, U. Fluglärm und Gesundheit in der Rhein-Main Region. 2005. Ergänzende Auswertung der RDF-Belästigungsstudie um die Fragen zur Gesundheit; 3941782002; SCR-Schreckenberg Consulting & Research (Hagen), Justus Liebig Universität (Gießen), Amt für Gesundheit (Frankfurt): Frankfurt am Main, Germany, 2009. [Google Scholar]
- Stansfeld, S.A.; Sharp, D.S.; Gallacher, J.; Babisch, W. Road traffic noise, noise sensitivity and psychological disorder. Psychol. Med. 1993, 23, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Stansfeld, S.; Gallacher, J.; Babisch, W.; Shipley, M. Road traffic noise and psychiatric disorder: Prospective findings from the Caerphilly Study. BMJ 1996, 313, 266–267. [Google Scholar] [CrossRef] [Green Version]
- Stansfeld, S.; Haines, M.; Berry, B.; Burr, M. Reduction of road traffic noise and mental health: An intervention study. Noise Health 2009, 11, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Sygna, K.; Aasvang, G.M.; Aamodt, G.; Oftedal, B.; Krog, N.H. Road traffic noise, sleep and mental health. Environ. Res. 2014, 131, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Tzivian, L.; Jokisch, M.; Winkler, A.; Weimar, C.; Dragano, N.; Erbel, R.; Jockel, K.H.; Moebus, S.; Hoffmann, B. Associations between outdoor and indoor noise, cognitive performance and depressive symptoms-results from HNR study. In Proceedings of the ISEE Young 2018: 3rd Early Career Researchers Conference on Environmental Epidemiology, Munich, Germany, 19–21 March 2018; p. A21. [Google Scholar]
- van Kamp, I.; Houthuijs, D.; van Wiechen, C.; Breugelmans, O. Environmental noise and mental health: Evidence from the Schiphol monitoring program. In INTER-NOISE and NOISE-CON Conference Proceedings; INTER-NOISE and NOISE-CON; Institute of Noise Control Engineering: Istanbul, Turkey, 2007; pp. 1177–1183. [Google Scholar]
- Zock, J.P.; Verheij, R.; Helbich, M.; Volker, B.; Spreeuwenberg, P.; Strak, M.; Janssen, N.A.H.; Dijst, M.; Groenewegen, P. The impact of social capital, land use, air pollution and noise on individual morbidity in Dutch neighbourhoods. Environ. Int. 2018, 121, 453–460. [Google Scholar] [CrossRef]
- He, S.; Smargiassi, A.; Low, N.; Bilodeau-Bertrand, M.; Ayoub, A.; Auger, N. Residential noise exposure and the longitudinal risk of hospitalization for depression after pregnancy: Postpartum and beyond. Environ. Res. 2019, 170, 26–32. [Google Scholar] [CrossRef]
- Almgren, H.; Van de Steen, F.; Razi, A.; Friston, K.; Marinazzo, D. The effect of global signal regression on DCM estimates of noise and effective connectivity from resting state fMRI. Neuroimage 2019, 208, 116435. [Google Scholar] [CrossRef]
- Tzivian, L. Traffic Noise Exposure and Mild Cognitive Impairment. In Proceedings of the Alzheimer’s Association International Conference, Alzheimers Dement, Chicago, IL, USA, 22–26 July 2018; p. 1381. [Google Scholar]
- Halonen, J.I.; Lanki, T.; Yli-Tuomi, T.; Turunen, A.W.; Pentti, J.; Vahtera, J.; Kivimäki, M. Traffic noise and psychotropic medication use. In Proceedings of the 42nd International Congress and Exposition on Noise Control Engineering 2013, INTER-NOISE 2013, Noise Control for Quality of Life, 2013, Innsbruck, Austria, 15–18 September 2013; pp. 4941–4947. [Google Scholar]
- Okokon, E.O.; Turunen, A.W.; Ung-Lanki, S.; Vartiainen, A.K.; Tiittanen, P.; Lanki, T. Road-Traffic noise: Annoyance, risk perception, and noise sensitivity in the Finnish adult population. Int. J. Environ. Res. Public Health 2015, 12, 5712–5734. [Google Scholar] [CrossRef] [Green Version]
- Bocquier, A.; Cortaredona, S.; Boutin, C.; David, A.; Bigot, A.; Sciortino, V.; Nauleau, S.; Gaudart, J.; Giorgi, R.; Verger, P. Is exposure to night-time traffic noise a risk factor for purchase of anxiolytic-hypnotic medication? A cohort study. Eur. J. Public Health 2014, 24, 298–303. [Google Scholar] [CrossRef] [Green Version]
- Jonah, B.A.; Bradley, J.S.; Dawson, N.E. Predicting individual subjective responses to traffic noise. J. Appl. Psychol. 1981, 66, 490–501. [Google Scholar] [CrossRef]
- Nivison, M.E.; Endresen, I.M. An analysis of relationships among environmental noise, annoyance and sensitivity to noise, and the consequences for health and sleep. J. Behav. Med. 1993, 16, 257–276. [Google Scholar] [CrossRef]
- Andersson, J.; Oudin, A.; Sundstrom, A.; Forsberg, B.; Adolfsson, R.; Nordin, M. Road traffic noise, air pollution, and risk of dementia–Results from the Betula project. Environ. Res. 2018, 166, 334–339. [Google Scholar] [CrossRef]
- Carey, I.M.; Anderson, H.R.; Atkinson, R.W.; Beevers, S.D.; Cook, D.G.; Strachan, D.P.; Dajnak, D.; Gulliver, J.; Kelly, F.J. Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ Open 2018, 8, e022404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linares, C.; Culqui, D.; Carmona, R.; Ortiz, C.; Diaz, J. Short-Term association between environmental factors and hospital admissions due to dementia in Madrid. Environ. Res. 2017, 152, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Fuks, K.B.; Wigmann, C.; Altug, H.; Schikowski, T. Road Traffic Noise at the Residence, Annoyance, and Cognitive Function in Elderly Women. Int. J. Environ. Res. Public Health 2019, 16, 1790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tzivian, L.; Dlugaj, M.; Winkler, A.; Weinmayr, G.; Hennig, F.; Fuks, K.B.; Vossoughi, M.; Schikowski, T.; Weimar, C.; Erbel, R.; et al. Long-Term Air Pollution and Traffic Noise Exposures and Mild Cognitive Impairment in Older Adults: A Cross-Sectional Analysis of the Heinz Nixdorf Recall Study. Environ. Health Perspect. 2016, 124, 1361–1368. [Google Scholar] [CrossRef] [Green Version]
- Petersen, R.C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 2004, 256, 183–194. [Google Scholar] [CrossRef]
- Peters, R.; Ee, N.; Peters, J.; Booth, A.; Mudway, I.; Anstey, K.J. Air pollution and dementia: A systematic review. J. Alzheimers Dis. 2019, 70, S145–S163. [Google Scholar] [CrossRef] [Green Version]
- Klaeboe, R.; Kolbenstvedt, M.; Clench-Aas, J.; Bartonova, A. Oslo traffic study–Part 1: An integrated approach to assess the combined effects of noise and air pollution on annoyance. Atmos. Environ. 2000, 34, 4727–4736. [Google Scholar] [CrossRef]
- Davies, H.W.; Vlaanderen, J.; Henderson, S.; Brauer, M. Correlation between co-exposures to noise and air pollution from traffic sources. OEM 2009, 66, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Foraster, M.; Deltell, A.; Basagaña, X.; Medina-Ramón, M.; Aguilera, I.; Bouso, L.; Grau, M.; Phuleria, H.C.; Rivera, M.; Slama, R. Local determinants of road traffic noise levels versus determinants of air pollution levels in a Mediterranean city. Environ. Res. 2011, 111, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Fecht, D.; Hansell, A.L.; Morley, D.; Dajnak, D.; Vienneau, D.; Beevers, S.; Toledano, M.B.; Kelly, F.J.; Anderson, H.R.; Gulliver, J. Spatial and temporal associations of road traffic noise and air pollution in London: Implications for epidemiological studies. Environ. Int. 2016, 88, 235–242. [Google Scholar] [CrossRef] [Green Version]
- Sartorius, N.; Üstün, T.B.; Lecrubier, Y.; Wittchen, H.-U. Depression comorbid with anxiety: Results from the WHO study on psychological disorders in primary health care. Br. J. Psychiatry 1996, 168, 38–43. [Google Scholar] [CrossRef]
- Mineka, S.; Watson, D.; Clark, L.A. Comorbidity of anxiety and unipolar mood disorders. Annu. Rev. Psychol. 1998, 49, 377–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldwin, C.L. Verbal collision avoidance messages during simulated driving: Perceived urgency, alerting effectiveness and annoyance. Ergonomics 2011, 54, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Sandelin, R.; Kowalski, J.; Ahnemark, E.; Allgulander, C. Treatment patterns and costs in patients with generalised anxiety disorder: One-Year retrospective analysis of data from national registers in Sweden. Eur. Psychiatry 2013, 28, 125–133. [Google Scholar] [CrossRef]
- Liu, X.; Ye, W.; Watson, P.; Tepper, P. Use of benzodiazepines, hypnotics, and anxiolytics in major depressive disorder: Association with chronic pain diseases. J. Appl. Psychol. 2010, 198, 544–550. [Google Scholar] [CrossRef]
- Alonso, J.; Lépine, J.-P. Overview of key data from the European Study of the Epidemiology of Mental Disorders (ESEMeD). J. Clin. Psychiat 2007, 68 (Suppl. 2), 3–9. [Google Scholar]
- Wang, P.S.; Angermeyer, M.; Borges, G.; Bruffaerts, R.; Chiu, W.T.; De Girolamo, G.; Fayyad, J.; Gureje, O.; Haro, J.M.; Huang, Y. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 177. [Google Scholar]
- ESEMeD/MHEDEA Investigators; Alonso, J.; Angermeyer, M.; Bernert, S.; Bruffaerts, R.; Brugha, T.; Bryson, H.; de Girolamo, G.; de Graaf, R.; Demyttenaere, K.; et al. Use of mental health services in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. 2004, 109, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Forbes, M.; Crome, E.; Sunderland, M.; Wuthrich, V. Perceived needs for mental health care and barriers to treatment across age groups. Aging Ment. Health 2017, 21, 1072–1078. [Google Scholar] [CrossRef] [PubMed]
- Vienneau, D.; Heritier, H.; Foraster, M.; Eze, I.C.; Schaffner, E.; Thiesse, L.; Rudzik, F.; Habermacher, M.; Kopfli, M.; Pieren, R.; et al. Facades, floors and maps–Influence of exposure measurement error on the association between transportation noise and myocardial infarction. Environ. Int. 2019, 123, 399–406. [Google Scholar] [CrossRef]
- Babisch, W. The Noise/Stress Concept, Risk Assessment and Research Needs. Noise Health 2002, 4, 1–11. [Google Scholar] [PubMed]
- Basner, M.; McGuire, S. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Effects on Sleep. Int. J. Environ. Res. Public Health 2018, 15, 519. [Google Scholar] [CrossRef] [Green Version]
- Halonen, J.I.; Vahtera, J.; Stansfeld, S.; Yli-Tuomi, T.; Salo, P.; Pentti, J.; Kivimaki, M.; Lanki, T. Associations between nighttime traffic noise and sleep: The Finnish public sector study. Environ. Health Perspect. 2012, 120, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Frei, P.; Mohler, E.; Roosli, M. Effect of nocturnal road traffic noise exposure and annoyance on objective and subjective sleep quality. Int. J. Hyg. Environ. Health 2014, 217, 188–195. [Google Scholar] [CrossRef]
- Wunderli, J.M.; Pieren, R.; Habermacher, M.; Vienneau, D.; Cajochen, C.; Probst-Hensch, N.; Roosli, M.; Brink, M. Intermittency ratio: A metric reflecting short-term temporal variations of transportation noise exposure. J. Expo. Sci. Environ. Epidemiol. 2016, 26, 575–585. [Google Scholar] [CrossRef]

| Inclusion | Exclusion | |
|---|---|---|
| Population | Adults sampled from the general population | Animal studies; occupational populations, non-representative (i.e., convenience) samples |
| Exposure | Road traffic, railway, or aircraft noise assessed objectively (i.e., measurements or noise modelling at place of residence) | Military aircraft noise; studies considering only neighborhood noise |
| Outcomes | Psychological complaints and disorders [in particular: dementia, vascular or Alzheimer, mild cognitive disorder (F00–F03, F06.7), depressive episodes (F32,–; F33,–) and anxiety disorders (F40,–)] (i.e., diagnosed disorders, e.g., self-reported, routine data; prescribed medications specific to a psychological disorder; validated screening instrument) | Annoyance; sleep disturbance; conditions not directly related to a clinical diagnosis; screening instrument was not validated |
| Converting | Road Traffic Noise | Railway Traffic Noise | Aircraft Noise |
|---|---|---|---|
| Leq24h to LDEN | Leq24h + 3.3 dB | Leq24h + 6.1 dB | Leq24h + 3.6 dB |
| LD to LDEN | LD + 2.0 dB Leq,16h + 1.5 dB | LD + 6.0 dB Leq,16h + 5.9 dB | LD + 2.1 dB Leq,16h + 2.3 dB |
| LDN to LDEN | LDN + 0.7 dB | LDN + 0.4 dB | LDN + 1.1 dB |
| LN to LDEN | LN + 8.0 dB | LN + 6.6 dB | LN + 9.9 dB |
| Study | Region(s) Study Design Quality Score (++,+,-) | Population | Outcome Assessment | Noise Source | Noise Measures | Noise Categories | Effect Estimates; Meta-Analysis (Yes, No with Reasons) |
|---|---|---|---|---|---|---|---|
| Baudin et al. 2018 [37] | France cross-sectional (-) | n = 1244 (M = 549, F = 695) 18–≥75 Years | GHQ-12 | Aircraft | LDEN Leq,24h LD, 6::00 a.m.-10:00 p.m. LN, (not specified) | <40 50–54 55–59 ≥60 dB | Odds Ratio (adjusted) yes |
| Floud et al. 2011 [38] | UK, NL, Sweden, Italy, Germany, Greece, cross-sectional (-) | n = 4861 (M = 2404, F = 2457) 45–70 Years | Anti-depressive use (last 2 weeks, self-reported) | Aircraft road | Leq, 7:00 a.m.-11:00 p.m. or Leq, 6::00 a.m.-10:00 p.m. LN, 11:00 p.m.-7:00 a.m. or LN, 10:00 p.m.-6:00 a.m. | LAeq,16h a 35–76 dB (aircraft) a 45–76 dB (road) LN a 30–70 dB (aircraft) a 45–70 dB (road) | Odds Ratio (adjusted) yes |
| Generaal et al. 2019a [39] | NL case-control/cross-sectional (-) | n = 2980 (M = 1007, F = 1973) 18–65 years | Recent diagnosis (major depression and dysthymia) based on CIDI b | Aircraft Road rail (combined) | LDEN | - | Odds Ratio (adjusted) no, exposure sources were not considered separately |
| Generaal et al. 2019b [40] | NL pooled analysis (-) | n = 32,487 ≥18 years 8 studies included | CIDI, PHQ-9, HADS-D, DES-D, 4DSQ, BDI-II | Aircraft Road rail (combined) | LDEN | - | Odds Ratio (adjusted) no, exposure sources were not considered separately |
| Greiser et al. 2010 [41] | Germany case-control (-) | n = 511,742 with depression: n = 3136 (M = 981, F = 2155) >39 years | Routine health insurance data c | aircraft | LN, 10:00 p.m.-6:00 a.m. Leq, 6:00 a.m.-10:00 p.m. Leq, 11:00 p.m.-1:00 a.m. Leq, 3:00 a.m.-5:00 a.m. Leq,24h | Leq,24h ≥35 dB otherwise ≥40 dB | Odds Ratio (adjusted) no, main noise effects not reported without interaction terms |
| He et al. 2019 [56] | Canada cohort (-) | F = 140,456 | Hospital records d | outdoor noise (mostly road) | Leq,24h LDEN LN, 11:00 p.m.-7:00 a.m. | <55 dB 55.0–59.9 dB 60.0–64.9 dB ≥65 dB | Hazard Ratio (adjusted) no, exposure sources were not considered separately |
| Halonen et al. 2013, 2014 [42,59] | Finland cross-sectional (-) | n = 15,611 (M = 3086, F = 12,525) 21–76 years | Anti-depressive use e | road | LDEN | ≤45 dB 45.1–50 dB 50.1–55 dB 55.1–60 dB >60 dB | Odds Ratio (adjusted) yes |
| Leijssen et al. 2019 [43] | NL cross-sectional (-) | n = 23,293 (M = 9920, F = 13,373) 18–70 years | PHQ-9 | road | Leq,24h | 45–54 dB 55–59 dB 60–64 dB 65–69 dB ≥70 dB | Odds Ratio (adjusted) yes |
| Klompmaker et al. 2019 [45] | NL cross-sectional (+) | n = 354,827 (M = 161,045, F = 193,782) ≥19 years | Prescriptions of antidepressants (ATC code e), K10 | road railway | LDEN | - | Odds Ratio (adjusted) yes |
| Miyakawa et al. 2007 [44] | Japan cross-sectional (-) | n = 188 (M = 101, F = 87) | GHQ-28 | aircraft | LDEN | 55–59 dB 59–65 dB | Odds Ratio (adjusted) no, noise was not measured for ‘unexposed’ sample |
| Okokon et al. 2018 [46] | Finland cross-sectional (-) | n = 5860 (M = 2497, F = 3363) 55.0 years | Anti-depressive use (a) 1 week, (b) 1–4 weeks, (c) 1–12 months, (d) over 1 year ago | road | LDEN | ≤45 dB, 45.1–50 dB, 50.1–55 dB, 55.1–60 dB ≥60 dB | Odds Ratio (adjusted) yes |
| Orban et al. 2016 [47] | Germany cohort (+) | n = 3300 (M = 1715, F = 1585) 45–74 years | CES-D Anti-depressive use (last week) | road | LDEN LN, 10:00 p.m.-6:00 a.m. | LDEN >55 vs. ≤55 dB; ≤55 dB >55–≤60 dB >60–≤65 dB >65 dB LN >50 dB | Relative Risks (adjusted) yes |
| Schreckenberg et al. 2009 [48] | Germany cross-sectional (-) | n = 2311 (M = 1034, F = 1276) <18–≥80 years | Daily use of mood-controlling, psychotropic drugs (last 12 months) | aircraft | Leq, 6:00 a.m.-10:00 p.m. LN, 10:00 p.m.-6:00 a.m. NAT55,6:00 a.m.-10:00 p.m. f NAT55, 10:00 p.m.-6:00 a.m. Lmax55, (6:00 a.m.-10:00 p.m.) f Lmax55, (10:00 p.m.-6:00 a.m.) | 40–45 dB 45–50 dB 50–55 dB 55–60 dB 60–65 dB For Leq,22-06h: reference < 40 dB | Odds Ratio (adjusted) yes |
| Seidler et al. 2017 [12] | Germany case-control (+) | n = 1,026,670 (77,295 cases, 578,246 controls) ≥40 years | Routine health insurance data g | Aircraft Road railway | Leq,24h. LN, 10:00 p.m.-6:00 a.m. (further measures considered for aircraft noise) | <40, max <50 dB <40, max ≥50 dB ≥40–<45 dB ≥50–<55 dB ≥55–<60 dB ≥60–<65 dB ≥65–<70 dB ≥70 dB; Continuous analysis h | Odds Ratio (adjusted) yes |
| Stansfeld et al. 1993, 1996 [49,50] | UK cohort (+) cross-sectional (-) | n = 2398 (only men) 50–64 Years | GHQ-30 | road | Leq,6:00 a.m.-10 p.m. | 51–55 dB 56–60 dB 61–65 dB 66–70 dB | Means/ Percent (adjusted) yes (unadjusted RRs derived from distributions in 1993 paper) |
| Stansfeld et al. 2009b [51] | UK intervention field study (-) | n = 387 households | CIS-R GHQ-28 | road | Leq,10:00 a.m.-5:00 p.m. L10 | - | Means/ Percent No intervention field study |
| Sygna et al. 2014 [52] | Norway cross-sectional (-) | n = 2898 (M = 1442, F = 1456) 18–˃78 years | HSCL-25 | road | LDEN | not reported | Odds Ratio (adjusted) yes |
| Tzivian et al. 2018 [58] | Germany cross-sectional (analysis within cohort) (+) | n = 2050 50–80 years | CES-D | road | LDEN | Binomial cut-off: 60 dB (LDEN) 55 dB (LN); <45 dB ≥45–<55 dB ≥55–<65 dB ≥65–<75 dB ≥75 continuous (starting at 0 dB) | Odds Ratio (adjusted) yes |
| van Kamp et al. 2007 [54] | NL longitudinal/ cross-sectional and panel study (+) | n = 6091 n = 2700 (longitudinal) ≥18 years | GHQ-12 | aircraft | LDEN LN,10:00 p.m.-6:00 a.m. | - | Odds Ratio (adjusted) yes |
| Zock et al. 2018 [55] | NL cross-sectional (analysis within cohort) (+) | n = 4450 0–≥65 years | Primary care data i | road railway | LDEN | - | Odds Ratio (adjusted) yes |
| Study | Region(s) Study Design Quality Score (++,+,-) | Population | Outcome Assessment | Noise Source | Noise Measures | Noise Categories | Effect Estimates; Meta-Analysis (Yes, No with Reasons) |
|---|---|---|---|---|---|---|---|
| Bocquier et al. 2014 [61] | France, Retrospective cohort (-) | n = 190,617 (M = 87,975, F = 102,642) 18–64 years | Prescriptions of anxiolytics, benzodiazepin-derivates and analogues (ATC code) a | road | LN, 10:00 p.m.-6:00 a.m. | <45 dB ≥45–<50 dB ≥50–<55 dB ≥55 dB | Odds Ratio (adjusted) yes |
| Floud et al. 2011 [38] | UK, NL, Sweden, Italy, Germany, Greece, cross-sectional (-) | n = 4861 (M = 2404, F = 2457) 45–70 Years | Use of anxiolytics (last 2 weeks, self-reported) | aircraft road | Leq, 7:00 a.m.-11:00 p.m. or Leq, 6:00 a.m.-10:00 p.m. Leq, 11:00 p.m.-7:00 a.m. or LN, 10:00 p.m.-6:00 a.m. | LAeq,16h b 35–76 dB (aircraft) b 45–76 dB (road) LN b 30–70 dB (aircraft) b 45–70 dB (road) | Odds Ratio (adjusted) yes |
| Generaal et al. 2019a [39] | NL case-control (-) | n = 2980 (M = 1007, F = 1973) 18–65 years | Recent diagnosis (anxiety disorder based on CIDI c) | Aircraft Road rail (combined) | LDEN | - | Odds Ratio (adjusted) no, exposure sources were not considered separately |
| Greiser et al. 2010 [41] | Germany case-control (-) | n = 511,742 with anxiety disorder: n = 2344 (M = 709, F = 1635) >39 years | Routine health insurance data d | aircraft | LN, 10:00 p.m.-6:00 a.m. Leq, 6:00 a.m.-10:00 p.m. Leq, 11:00 p.m.-1:00 a.m. Leq, 3:00 a.m.-5:00 a.m. Leq,24h | Leq,24h ≥35 dB otherwise ≥40 dB | Odds Ratio (adjusted) no, main noise effects not reported without interaction terms |
| Halonen et al. 2013 [59] | Finland cross-sectional (-) | n = 15,611 (M = 3086, F = 12,525) 21–76 years | Anxiolytics use (ATC code) | road | LDEN | ≤45 dB 45.1–50 dB 50.1–55 dB 55.1–60 dB >60 dB | Odds Ratio (adjusted) yes |
| Jonah et al. 1981 [62] | Canada cross-sectional (-) | n = 1150 (adults) | STAI | road | Leq,24h | 45–75 dB | Correlation coefficient no |
| Klompmaker et al. 2019 [45] | NL cross-sectional (+) | n = 354,827 (M = 161,045, F = 193,782) ≥19 years | Prescriptions of anxiolytics (ATC code e) | road railway | LDEN | - | Odds Ratio (adjusted) yes |
| Nivision & Endersen 1993 [63] | Norway, cross-sectional (-) | n = 82 | STAI | road | Leq,24h Lmax | - | Correlation coefficient no |
| Okokon et al. 2018 | Finland cross-sectional (-) | n = 5860 (M = 2497, F = 3363) 55.0 years | Use of anxiolytics (a) 1 week, (b) 1–4 weeks, (c) 1–12 months, (d) over 1 year ago | road | LDEN | ≤45 dB, 45.1–50 dB, 50.1–55 dB, 55.1–60 dB ≥ 60 dB | Odds Ratio (adjusted) yes |
| Stansfeld et al. 1993, 1996 [49,50] | UK cohort (+) cross-sectional (-) | n = 2398 (only men) 50–64 Years | GHQ-30 | road | Leq,6:00 a.m.-10:00 p.m. | 51–55 dB 56–60 dB 61–65 dB 66–70 dB | Means/ Percent (adjusted) yes (unadjusted RRs derived from distribution in 1993 paper) |
| Zock et al. 2018 [55] | NL cross-sectional (analysis within cohort) (+) | n = 4450 0–≥ 65 years | Primary care data f | road railway | LDEN | - | Odds Ratio (adjusted) -yes |
| Study | Region(s) Study Design Quality Score (++,+,-) | Population | Outcome Assessment | Noise Source | Noise Measures | Noise Categories | Effect Estimates; Meta-Analysis (Yes, No with Reasons) |
|---|---|---|---|---|---|---|---|
| Andersson et al. 2018 [64] | Sweden, Cohort (+) | n = 1721 (M = 985, F = 736) 55–85 years | Alzheimer’s disease and vascular dementia: Three-step procedure: general examination, examination by specialists and diagnosed by specialist a | road | Leq,24h | <55 dB ≥55 dB | Odds Ratio (adjusted) |
| Carey et al. 2018 [65] | UK, Cohort (+) | n = 130,978 (M = 65 130, F = 65,848) 50–79 years | Alzheimer’s disease and vascular dementia: Doctor’s diagnosis (from database) | road | LN, 11 p.m.-7:00 a.m. | Continuous analysis | Odds Ratio (adjusted) |
| Fuks et al. 2019 [67] | Germany, Cohort (+) | n = 288 (females only) 74.2 years (±2.2) | Cognitive function according to CERAD-Plus battery | road | LDEN LNIGHT | Odds Ratio (adjusted) | |
| Linares et al. 2017 [66] | Spain, longitudinal ecological time series study (–) | n = 3,116,897 | Dementia-related emergency hospital admissions (related to organic psychoses: ICD-9 b) | road | LN, 10:00 p.m.-8:00 a.m. Leq, 8:00 a.m.-10:00 p.m. | Continuous analysis | Correlation coefficient no |
| Tzivian et al. 2016 [68] | Germany cross-sectional (analysis within cohort) (+) | n = 2050 50–80 years | Mild cognitive impairment, test battery with ADAS and NAI c | road | LDEN LN,10:00 p.m.-6:00 a.m. | Dichotomized (cut point 60 dB (LDEN) and 55 dB (LN) <45 dB ≥45–<55 dB ≥55–<65 dB ≥65–<75 dB ≥75 Continuous | Odds Ratio (adjusted) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hegewald, J.; Schubert, M.; Freiberg, A.; Romero Starke, K.; Augustin, F.; Riedel-Heller, S.G.; Zeeb, H.; Seidler, A. Traffic Noise and Mental Health: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6175. https://doi.org/10.3390/ijerph17176175
Hegewald J, Schubert M, Freiberg A, Romero Starke K, Augustin F, Riedel-Heller SG, Zeeb H, Seidler A. Traffic Noise and Mental Health: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(17):6175. https://doi.org/10.3390/ijerph17176175
Chicago/Turabian StyleHegewald, Janice, Melanie Schubert, Alice Freiberg, Karla Romero Starke, Franziska Augustin, Steffi G. Riedel-Heller, Hajo Zeeb, and Andreas Seidler. 2020. "Traffic Noise and Mental Health: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 17: 6175. https://doi.org/10.3390/ijerph17176175
APA StyleHegewald, J., Schubert, M., Freiberg, A., Romero Starke, K., Augustin, F., Riedel-Heller, S. G., Zeeb, H., & Seidler, A. (2020). Traffic Noise and Mental Health: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(17), 6175. https://doi.org/10.3390/ijerph17176175







