Early Rehabilitation after Surgical Repair of Medial and Lateral Collateral Elbow Ligaments: A Report of Three Cases
Abstract
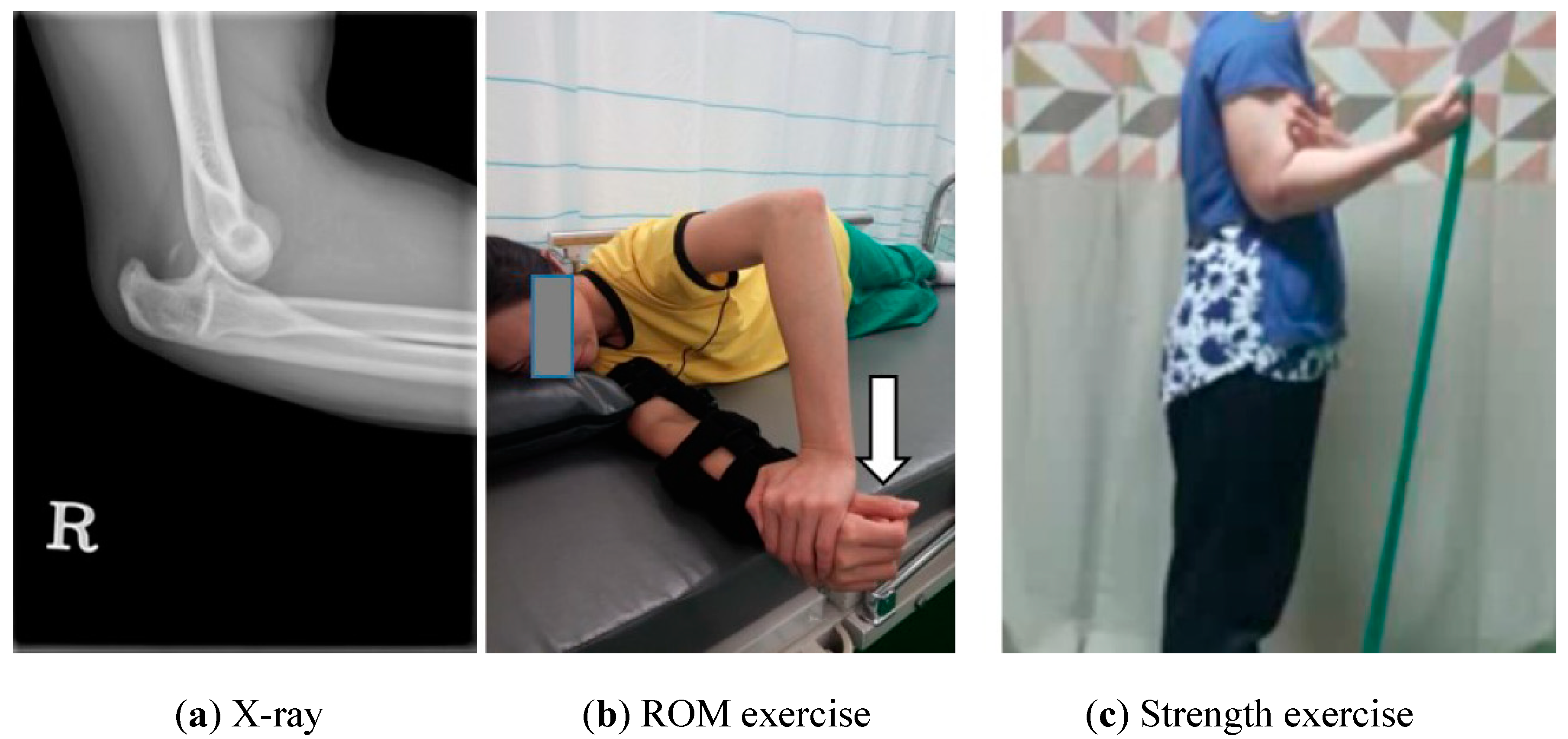
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Rehabilitation Procedure
2.3. Measurement: ROM, Strength, and Oxford Elbow Score
3. Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hackl, M.; Bercher, M.; Wegmann, K.; Müller, L.; Dargel, J. Functional anatomy of the lateral collateral ligament of the elbow. Arch. Orthop. Trauma Surg. 2016, 136, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M.A.; Ross, G. Acute elbow dislocations. Orthop. Clin. N. Am. 2008, 39, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, J.J.; Paul, S.; Hotchkiss, R.N.; Daluiski, A. Conservative management of elbow dislocations with an overhead motion protocol. J. Hand Surg. 2015, 40, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Kesmezacar, H.; Sarikaya, I.A. The results of conservatively treated simple elbow dislocations. Acta. Orthop. Traumatol. Turc. 2010, 44, 199–205. [Google Scholar] [CrossRef]
- Rettig, A.C.; Sherrill, C.; Snead, D.S.; Mendler, J.C.; Mieling, P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am. J. Sports Med. 2001, 29, 15–17. [Google Scholar] [CrossRef] [PubMed]
- Cain, E.L., Jr.; Andrews, J.R.; Dugas, J.R.; Wilk, K.E.; McMichael, C.S.; Walter, J.C.; Riley, R.S.; Arthur, S.T. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: Results in 743 athletes with minimum 2-year follow-up. Am. J. Sports Med. 2010, 38, 2426–2434. [Google Scholar] [CrossRef]
- Wilk, K.E.; Arrigo, C.; Andrews, J.R. Rehabilitation of the elbow in the throwing athlete. J. Orthop. Sports Phys. Ther. 1993, 17, 305–317. [Google Scholar] [CrossRef]
- Heo, Y.M.; Yi, J.W.; Lee, J.B.; Lee, D.H.; Park, W.K.; Kim, S.J. Unstable simple elbow dislocation treated with the repair of lateral collateral ligament complex. Clin. Orthop. Surg. 2015, 7, 241–247. [Google Scholar] [CrossRef] [Green Version]
- Wilk, K.E.; Arrigo, C.A.; Bagwell, M.S.; Rothermich, M.A.; Dugas, J.R. Repair of the ulnar collateral ligament of the elbow: Rehabilitation following internal brace surgery. J. Orthop. Sports Phys. Ther. 2019, 49, 253–261. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Cain, E.L.; Dugas, J.R.; Andrews, J.R. Rehabilitation of the Overhead Athlete’s Elbow. Sports Health 2012, 4, 404–414. [Google Scholar] [CrossRef] [Green Version]
- Alolabi, B.; Gray, A.; Ferreira, L.M.; Johnson, J.A.; Athwal, G.S.; King, G.J. Rehabilitation of the medial-and lateral collateral ligament-deficient elbow: An in vitro biomechanical study. J. Hand Ther. 2012, 25, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Reichel, L.M.; Milam, G.S.; Sitton, S.E.; Curry, M.C.; Mehlhoff, T.L. Elbow lateral collateral ligament injuries. J. Hand Surg. 2013, 38, 184–201. [Google Scholar] [CrossRef] [PubMed]
- Greiner, S.; Koch, M.; Kerschbaum, M.; Bhide, P.P. Repair and augmentation of the lateral collateral ligament complex using internal bracing in dislocations and fracture dislocations of the elbow restores stability and allows early rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3269–3275. [Google Scholar] [CrossRef] [PubMed]
- Manocha, R.H.; Kusins, J.R.; Johnson, J.A.; King, G.J. Optimizing the rehabilitation of elbow lateral collateral ligament injuries: A biomechanical study. J. Shoulder Elb. Surg. 2017, 26, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; So, W.-Y. Effects of Rehabilitation in Bankart Lesion in Non-athletes: A report of three cases. Open Med. 2019, 14, 369–375. [Google Scholar]
- CSMi. Humac Norm Users Guide; Computer Sports Medicine, Inc.: Stoughton, MA, USA, 2019. [Google Scholar]
- Guyver, P.; Cattell, A.; Hall, M.; Brinsden, M. Oxford elbow scores in an asymptomatic population. Ann. R. Coll. Surg. Engl. 2013, 95, 415–417. [Google Scholar] [CrossRef]
- Nesterenko, S.; Domire, Z.J.; Morrey, B.F.; Sanchez-Sotelo, J. Elbow strength and endurance in patients with a ruptured distal biceps tendon. J. Shoulder Elb. Surg. 2010, 19, 184–189. [Google Scholar] [CrossRef]
- Chang, K.-V.; Hung, C.-Y.; Han, D.-S.; Chen, W.-S.; Wang, T.-G.; Chien, K.-L. Early versus delayed passive range of motion exercise for arthroscopic rotator cuff repair: A meta-analysis of randomized controlled trials. Am. J. Sports Med. 2015, 43, 1265–1273. [Google Scholar] [CrossRef]
- Kluczynski, M.A.; Isenburg, M.M.; Marzo, J.M.; Bisson, L.J. Does early versus delayed active range of motion affect rotator cuff healing after surgical repair? A systematic review and meta-analysis. Am. J. Sports Med. 2016, 44, 785–791. [Google Scholar] [CrossRef]
- Arndt, J.; Clavert, P.; Mielcarek, P.; Bouchaib, J.; Meyer, N.; Kempf, J.-F.; French Society for Shoulder & Elbow (SOFEC). Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: A prospective randomized study. Orthop. Traumatol. Surg. Res. 2012, 98, S131–S138. [Google Scholar] [CrossRef] [Green Version]
- Keener, J.D.; Galatz, L.M.; Stobbs-Cucchi, G.; Patton, R.; Yamaguchi, K. Rehabilitation following arthroscopic rotator cuff repair: A prospective randomized trial of immobilization compared with early motion. JBJS 2014, 96, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Nandi, S.; Maschke, S.; Evans, P.J.; Lawton, J.N. The stiff elbow. Hand 2009, 4, 368–379. [Google Scholar] [CrossRef] [PubMed]
- Fusaro, I.; Orsini, S.; Kantar, S.S.; Sforza, T.; Benedetti, M.; Bettelli, G.; Rotini, R. Elbow rehabilitation in traumatic pathology. Musculoskelet. Surg. 2014, 98, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.M. Strength and hypertrophy with resistance training: Chasing a hormonal ghost. Eur. J. Appl. Physiol. 2012, 112, 1981–1983. [Google Scholar] [CrossRef] [PubMed]
- Carpinelli, R.N.; Otto, R.M.; Winett, R.A. A critical analysis of the ACSM position stand on resistance training: Insufficient evidence to support recommended training protocols. J. Prof. Exerc. Physiol. 2004, 7, 1–60. [Google Scholar]
- Meierbachtol, A.; Rohman, E.; Paur, E.; Bottoms, J.; Tompkins, M. Quantitative improvements in Hop Test scores after a 6-week neuromuscular training program. Sports Health 2017, 9, 22–29. [Google Scholar] [CrossRef] [Green Version]
- Barber-Westin, S.D.; Hermeto, A.A.; Noyes, F.R. A six-week neuromuscular training program for competitive junior tennis players. J. Strength Cond. Res. 2010, 24, 2372–2382. [Google Scholar] [CrossRef]
- Chen, L.-K.; Lee, W.-J.; Peng, L.-N.; Liu, L.-K.; Arai, H.; Akishita, M.; Asian Working Group for Sarcopenia. Recent advances in sarcopenia research in Asia: 2016 update from the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2016, 17, e1–e7. [Google Scholar] [CrossRef]
- Van Grinsven, S.; Van Cingel, R.; Holla, C.; Van Loon, C. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1128–1144. [Google Scholar] [CrossRef]
- Hübscher, M.; Zech, A.; Pfeifer, K.; Hänsel, F.; Vogt, L.; Banzer, W. Neuromuscular training for sports injury prevention: A systematic review. Med. Sci. Sports Exerc. 2010, 42, 413–421. [Google Scholar] [CrossRef]


| A | B | C | |
|---|---|---|---|
| Sex/age | Women/39 | Women/60 | Men/17 |
| Job | Housewife | Farmer | Student |
| Recreational sports | Swimming | Badminton | Judo |
| Cause and Mechanism | Trauma, Dislocation | Chronic, Degeneration | Trauma, Twist and hyper-extension |
| Surgery method | Open | Arthroscopy | Arthroscopy |
| Restoration of daily life | 6 weeks | 6 weeks | 6 weeks |
| Return to recreational activity | 6 months | 8 months | 4 months |
| Phase | Time | Exercise |
|---|---|---|
| Phase 1 | 7 days |
|
| Phase 2 | 3 weeks |
|
| Phase 3 | 6 weeks |
|
| Phase 4 | 3 months |
|
| Phase 5 | 6 months |
|
| Patients | 6 Weeks | 3 Months | 6 Months | 12 Months | 24 Months |
|---|---|---|---|---|---|
| Case A | 7 | 12 | 22 | 30 | 44 |
| Case B | 4 | 9 | 22 | 34 | 43 |
| Case C | 10 | 22 | 30 | 42 | 46 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.E.; Choi, Y.C.; Lee, J.Y. Early Rehabilitation after Surgical Repair of Medial and Lateral Collateral Elbow Ligaments: A Report of Three Cases. Int. J. Environ. Res. Public Health 2020, 17, 6133. https://doi.org/10.3390/ijerph17176133
Kim SE, Choi YC, Lee JY. Early Rehabilitation after Surgical Repair of Medial and Lateral Collateral Elbow Ligaments: A Report of Three Cases. International Journal of Environmental Research and Public Health. 2020; 17(17):6133. https://doi.org/10.3390/ijerph17176133
Chicago/Turabian StyleKim, Seong Eon, Yong Chul Choi, and Ji Young Lee. 2020. "Early Rehabilitation after Surgical Repair of Medial and Lateral Collateral Elbow Ligaments: A Report of Three Cases" International Journal of Environmental Research and Public Health 17, no. 17: 6133. https://doi.org/10.3390/ijerph17176133
APA StyleKim, S. E., Choi, Y. C., & Lee, J. Y. (2020). Early Rehabilitation after Surgical Repair of Medial and Lateral Collateral Elbow Ligaments: A Report of Three Cases. International Journal of Environmental Research and Public Health, 17(17), 6133. https://doi.org/10.3390/ijerph17176133






