Psychosocial Determinants of Quality of Life and Active Aging. A Structural Equation Model
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Latent Variables. Description of Tasks Related
2.3. Procedure
2.4. Structural Analysis
3. Results
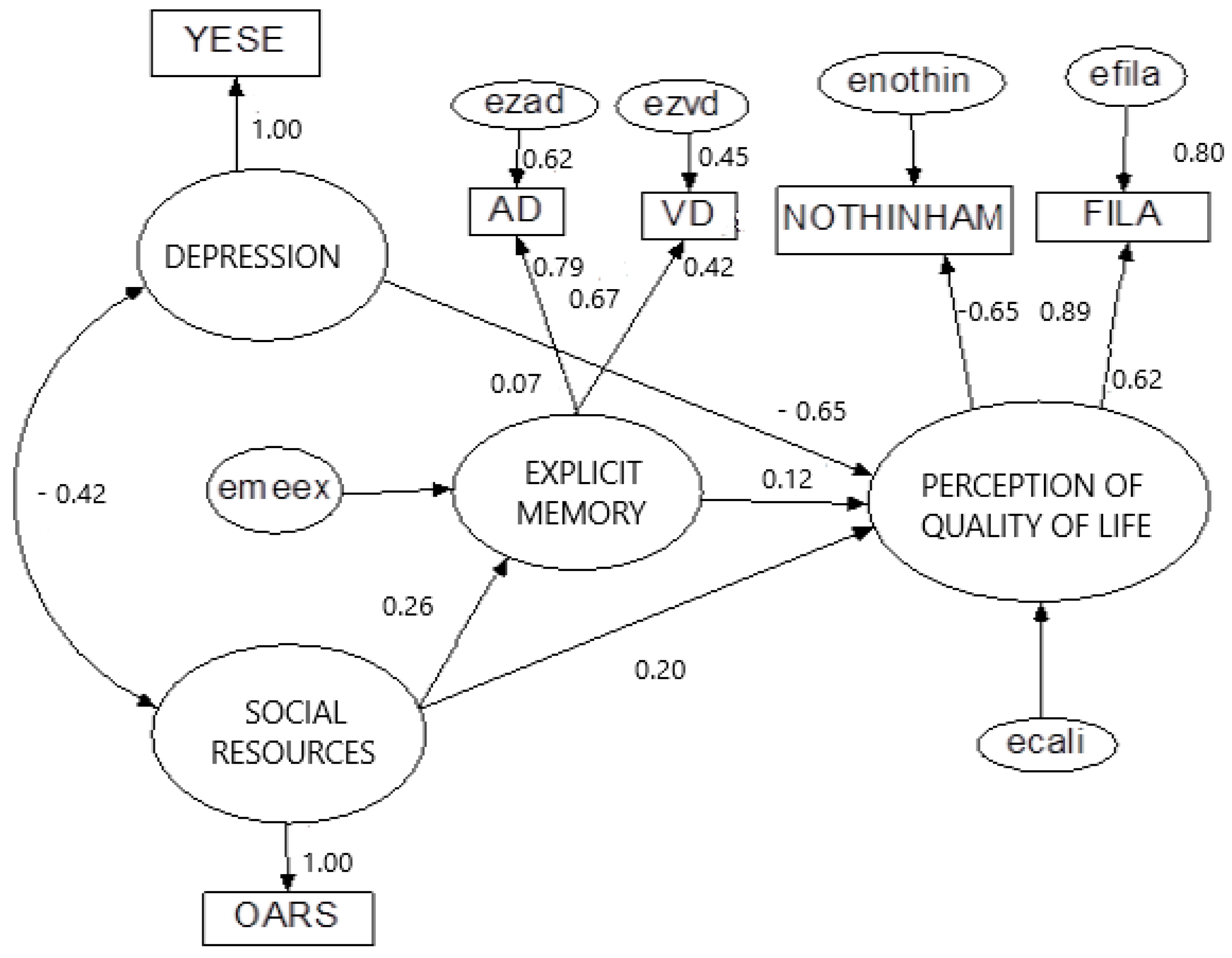
- The accessibility of social resources varied negatively with depression (−0.42) and positively with explicit memory (0.26). A person with good availability of social resources could reduce depression and improve explicit memory.
- The latent variables of social resources, depression, and explicit memory directly influenced the perception of quality of life, with a negative value for depression (−0.65) and a positive value for social resources (0.20) and explicit memory (0.12).
- The latent variable perception of quality of life is represented by two objective variables which mean “feel satisfaction in life” (0.89) and “have a good perception about health” (−0.65) (note that a lower score in the Nottingham Health Profile implies a better perception of health, due to the negative estimate value).
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Department of Economic and Social Affairs. World Population Ageing 2019; United Nations: New York, NY, USA, 2019; pp. 1–2. [Google Scholar]
- Department of Economic and Social Affairs. World Population Ageing 2015; United Nations: New York, NY, USA, 2015; pp. 9–34. [Google Scholar]
- Statistics National Institute (INE). Demography and Population. INEbase 2019. Available online: https://www.ine.es/jaxi/Tabla.htm?path=/t20/e245/p08/l0/&file=03002.px&L=0 (accessed on 18 July 2020).
- Ateca-Amestoy, V.; Ugidos, A. The Impact of Different Types of Resource Transfers on Individual Wellbeing: An Analysis of Quality of Life Using CASP-12. Soc. Indic. Res. 2011, 110, 973–991. [Google Scholar] [CrossRef]
- Hsu, H.-C. Associations of City-Level Active Aging and Age Friendliness with Well-Being among Older Adults Aged 55 and Over in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 4303. [Google Scholar] [CrossRef] [PubMed]
- Naah, F.L.; Njong, A.M.; Kimengsi, J.N. Determinants of Active and Healthy Ageing in Sub-Saharan Africa: Evidence from Cameroon. Int. J. Environ. Res. Public Heal. 2020, 17, 3038. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Active Ageing: A policy Framework; A contribution of the World Health Organization to the Second United Nations World Assembly on Ageing, Madrid, Spain, April 2002; World Health Organization: Geneva, Switzerland, 2002; pp. 12–30. [Google Scholar]
- Active Aging Group; European Commission (EC); United Nations Economic Commission for Europe (UNECE). Active Ageing Index (AAI): Concept, Methodology and Final Results. UNECE Grant No: ECE/Gc/2012/003; European Centre: Vienna, Australia, 2013. [Google Scholar]
- European Commission (EC); United Nations Economic Commission for Europe (UNECE). 2018 Active Ageing Index. Analytical Report June 2019. UNECE Grant No: ECE/Gc/2012/003; European Centre: Vienna, Australia, 2019. [Google Scholar]
- Bowling, A. Enhancing later life: How older people perceive active ageing? Aging Ment. Health 2008, 12, 293–301. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef]
- Bowling, A.; Dieppe, P. What is successful ageing and who should define it? BMJ 2005, 331, 1548–1551. [Google Scholar] [CrossRef]
- A Parslow, R.; Lewis, V.J.; Nay, R. Successful Aging: Development and Testing of a Multidimensional Model Using Data From a Large Sample of Older Australians. J. Am. Geriatr. Soc. 2011, 59, 2077–2083. [Google Scholar] [CrossRef]
- Silverstein, M.; Parker, M.G. Leisure Activities and Quality of Life among the Oldest Old in Sweden. Res. Aging 2002, 24, 528–547. [Google Scholar] [CrossRef]
- Zakzanis, K.K.; Leach, L.; Kaplan, E. On the nature and pattern of neurocognitive function in major depressive disorder. Neuropsychiatry Neuropsychol. Behav. Neurol. 1998, 11, 111–119. [Google Scholar]
- Hussenoeder, F.S.; Jentzsch, D.; Matschinger, H.; Hinz, A.; Kilian, R.; Riedel-Heller, S.G.; Conrad, I. Depression and quality of life in old age: A closer look. Eur. J. Ageing 2020, 1–9. [Google Scholar] [CrossRef]
- Cadzow, R.B.; Servoss, T.J. The association between perceived social support and health among patients at a free urban clinic. J. Natl. Med Assoc. 2009, 101, 243–250. [Google Scholar] [CrossRef]
- Deng, J.; Hu, J.; Wu, W.; Dong, B.; Wu, H. Subjective well-being, social support, and age-related functioning among the very old in China. Int. J. Geriatr. Psychiatry 2009, 25, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Beutel, M.E.; Glaesmer, H.; Wiltink, J.; Marian, H.; Brähler, E. Life satisfaction, anxiety, depression and resilience across the life span of men. Aging Male 2009, 13, 32–39. [Google Scholar] [CrossRef]
- Marsillas, S.; De Donder, L.; Kardol, T.; Van Regenmortel, S.; Dury, S.; Brosens, D.; Smetcoren, A.-S.; Braña, T.; Varela, J. Does active ageing contribute to life satisfaction for older people? Testing a new model of active ageing. Eur. J. Ageing 2017, 14, 295–310. [Google Scholar] [CrossRef] [PubMed]
- Hung, J.-Y.; Lu, K.-S. Research on the Healthy Lifestyle Model, Active Ageing, and Loneliness of Senior Learners. Educ. Gerontol. 2013, 40, 353–362. [Google Scholar] [CrossRef]
- Galli, R.; Moriguchi, E.H.; Bruscato, N.M.; Horta, R.L.; Pattussi, M.P. Active aging is associated with low prevalence of depressive symptoms among Brazilian older adults. Rev. Bras. Epidemiologia 2016, 19, 307–316. [Google Scholar] [CrossRef]
- Shirbeigi, M.; Esmaili, Z.; Sarmadi, M.R.; Moradi, A. Study and comparing 3 groups of active, passive, and ecotourist old age people on their mental health and happiness living in Illam City, Iran. Salman-Iran. J. Ageing 2016, 4, 40–48. [Google Scholar]
- Leś, A.; Guszkowska, M.; Piotrowska, J.; Rutkowska, I. Changes in perceived quality of life and subjective age in older women participating in Nordic Walking classes and memory training. J. Sports Med. Phys. Fit. 2019, 59, 1783–1790. [Google Scholar] [CrossRef]
- Romero, L.P.D.L.; Lévy, J.P.; Fernández, T.; Ballesteros, S. Modeling Active Aging and Explicit Memory: An Empirical Study. Health Soc. Work. 2015, 40, 183–190. [Google Scholar] [CrossRef]
- Wechsler, D. Wechsler Memory Scale—III [Technical Manual]; TEA: Madrid, Spain, 2004. [Google Scholar]
- Yesavage, J.A. Development and validation of GDS. J. Psychiatry 1983, 17, 37–49. [Google Scholar]
- Duke University Centers for the Study of Aging and Human Development. Multidimensional Functional Assessment: The OARS Methodology; Duke University: Durham, NC, USA, 1978. [Google Scholar]
- Lawton, M.P. Philadelphia Geriatric Center Morale Scale. Ph.D. Thesis, Autonomous University of Madrid, Madrid, Spain, 1990. [Google Scholar]
- Alonso, J.; Antó, J.M.; Moreno, C. Spanish version of the Nottingham Health Profile: Translation and preliminary validity. Am. J. Public Heal. 1990, 80, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Himanshu, H.; Arokiasamy, P.A.; Talukdar, B. Illustrative effects of social capital on health and quality of life among older adult in India: Results from WHO-SAGE India. Arch. Gerontol. Geriatr. 2019, 82, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Verhaeghen, P.; Geraerts, N.; Marcoen, A. Memory Complaints, Coping, and Well-Being in Old Age. Gerontologist 2000, 40, 540–548. [Google Scholar] [CrossRef] [PubMed]
- De Guzman, A.B.; Lagdaan, L.F.M.; Lagoy, M.L.V. The Role of Life-Space, Social Activity, and Depression on the Subjective Memory Complaints of Community-Dwelling Filipino Elderly: A Structural Equation Model. Educ. Gerontol. 2014, 41, 348–360. [Google Scholar] [CrossRef]
- O’Luanaigh, C.; O’Connell, H.; Chin, A.-V.; Hamilton, F.; Coen, R.; Walsh, C.; Walsh, J.; Caokley, D.; Cunningham, C.; Lawlor, B. Loneliness and cognition in older people: The Dublin Healthy Ageing study. Aging Ment. Heal. 2012, 16, 347–352. [Google Scholar] [CrossRef]
- Zunzunegui, M.V.R.E.; Alvarado, B.E.; Del Ser, T.; Otero, A. Social Networks, Social Integration, and Social Engagement Determine Cognitive Decline in Community-Dwelling Spanish Older Adults. J. Gerontol. Ser. B 2003, 58, S93–S100. [Google Scholar] [CrossRef]
- James, B.D.; Wilson, R.S.; Barnes, L.L.; Bennett, D.A. Late-Life Social Activity and Cognitive Decline in Old Age. J. Int. Neuropsychol. Soc. 2011, 17, 998–1005. [Google Scholar] [CrossRef]
- Binstock, R.; George, L. Handbook of Aging and the Social Sciences, 5th ed.; Academic Press: Cambridge, MA, USA, 2001. [Google Scholar]
- Lee, P.-L.; Lan, W.; Yen, T.-W. Aging Successfully: A Four-Factor Model. Educ. Gerontol. 2011, 37, 210–227. [Google Scholar] [CrossRef]
- Malone, J.C.; Liu, S.R.; Vaillant, G.E.; Rentz, R.M.; Waldinger, R.J. Midlife Eriksonian psychosocial development: Setting the stage for late-life cognitive and emotional health. Dev. Psychol. 2015, 52, 496–508. [Google Scholar] [CrossRef]
- Elosua, P. Subjective Values of Quality of Life Dimensions in Elderly People. A SEM Preference Model Approach. Soc. Indic. Res. 2010, 104, 427–437. [Google Scholar] [CrossRef]
- Merriam, S.B.; Kee, Y. Promoting Community Wellbeing: The Case for Lifelong Learning for Older Adults. Adult Educ. Q. 2014, 64, 128–144. [Google Scholar] [CrossRef]
- De Haro, A.E.; Lopez, S.M.D.M.; Aroca, J.A.S. Perception of the quality of life in older woman and their active ageing through socio educational activities in the social centers. RIE 2015, 33, 471. [Google Scholar] [CrossRef]
- Al-Dhafiri, A.M. The role of social work services in improving the living standards of the elderly in Kuwait an empirical study. Education 2014, 135, 177–196. [Google Scholar]
- Lak, A.; Rashidghalam, P.; Myint, P.K.; Baradaran, H.R. Comprehensive 5P framework for active aging using the ecological approach: An iterative systematic review. BMC Public Health 2020, 20, 1–22. [Google Scholar] [CrossRef]
- Jeste, D.V.; Blazer, D.G.; Buckwalter, K.C.; Cassidy, K.-L.K.; Fishman, L.; Gwyther, L.P.; Levin, S.M.; Phillipson, C.; Rao, R.R.; Schmeding, E.; et al. Age-Friendly Communities Initiative: Public Health Approach to Promoting Successful Aging. Am. J. Geriatr. Psychiatry 2016, 24, 1158–1170. [Google Scholar] [CrossRef]
- Mohammadi, E.; Allahyari, T.; Kakhaki, A.D.; Saraei, H.; Fereshtehnejad, S. Analysis of Being Active Based on Older Adults’ Experience: A Qualitative Study of Active Aging Strategies. Iran. J. Ageing 2017, 11, 504–517. [Google Scholar] [CrossRef]
- Bar-Netzera, R.; Bocos, M. Active ageing and effective learning for enhance quality of life. EpSBS 2016, 544–551. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2001. [Google Scholar]
- Lévy Mangin, J.P.; Varela, J. Modeling Covariance Structures in Social Sciences, Key Issues, Advanced and Special Contributions; Netbiblo: Coruña, Spain, 2006. [Google Scholar]
| Variables in Model | ||
|---|---|---|
| Latent Variable | Reliability | Extracted Variance |
| Depression | 1 | 1 |
| Explicit memory | 0.71 | 0.53 |
| Perceived quality of life | 0.75 | 0.60 |
| Social resources | 1 | 1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
León, L.P.d.; Mangin, J.P.L.; Ballesteros, S. Psychosocial Determinants of Quality of Life and Active Aging. A Structural Equation Model. Int. J. Environ. Res. Public Health 2020, 17, 6023. https://doi.org/10.3390/ijerph17176023
León LPd, Mangin JPL, Ballesteros S. Psychosocial Determinants of Quality of Life and Active Aging. A Structural Equation Model. International Journal of Environmental Research and Public Health. 2020; 17(17):6023. https://doi.org/10.3390/ijerph17176023
Chicago/Turabian StyleLeón, Laura Ponce de, Jean Pierre Lévy Mangin, and Soledad Ballesteros. 2020. "Psychosocial Determinants of Quality of Life and Active Aging. A Structural Equation Model" International Journal of Environmental Research and Public Health 17, no. 17: 6023. https://doi.org/10.3390/ijerph17176023
APA StyleLeón, L. P. d., Mangin, J. P. L., & Ballesteros, S. (2020). Psychosocial Determinants of Quality of Life and Active Aging. A Structural Equation Model. International Journal of Environmental Research and Public Health, 17(17), 6023. https://doi.org/10.3390/ijerph17176023






