An Anti-Stigma Course for Occupational Therapy Students in Taiwan: Development and Pilot Testing
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participant Recruitment
2.2. Measures
2.2.1. Social Distance Scale
2.2.2. Questionnaires on Stigmatising Attitudes
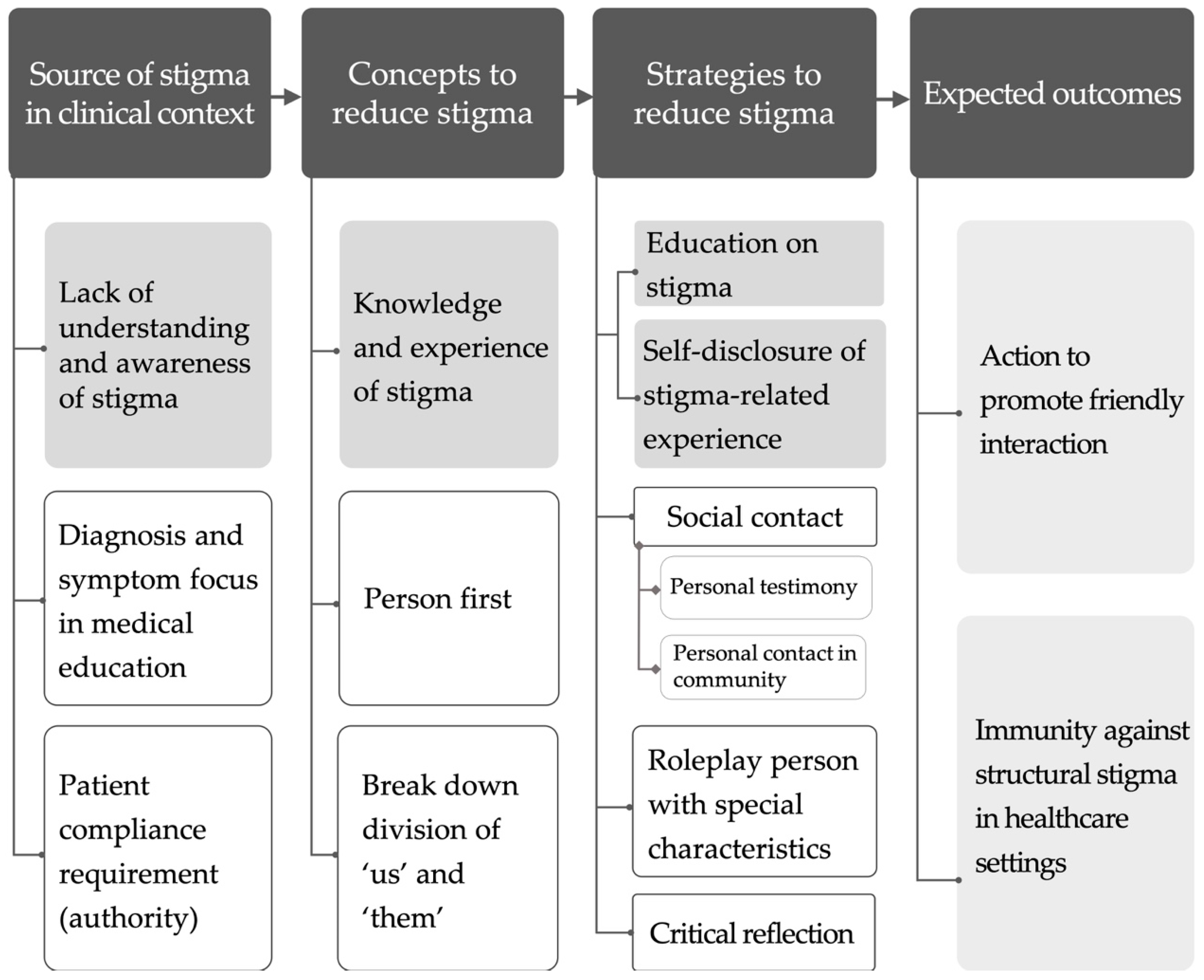
2.3. Anti-Stigma Course
2.4. Data Analyses
3. Results
3.1. Participant Characteristics
3.2. Evaluation Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jones, N.; Corrigan, P.W. Understanding Stigma. In The Stigma of Disease and Disability: Understanding Causes and Overcoming Injustices; Corrigan, P.W., Ed.; American Psychological Association: Washington, DC, USA, 2014; pp. 9–34. [Google Scholar]
- Morgan, A.J.; Reavley, N.J.; Jorm, A.F.; Beatson, R. Experiences of discrimination and positive treatment from health professionals: A national survey of adults with mental health problems. Aust. N. Z. J. Psychiatry 2016, 50, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Satchidanand, N.; Gunukula, S.K.; Lam, W.Y.; McGuigan, D.; New, I.; Symons, A.B.; Withiam-Leitch, M.; Akl, E.A. Attitudes of healthcare students and professionals toward patients with physical disability: A systematic review. Am. J. Phys. Med. Rehabil. 2012, 91, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Schulze, B.; Angermeyer, M.C. Subjective experiences of stigma. a focus group study of schizophrenic patients, their relatives and mental health professionals. Soc. Sci. Med. 2003, 56, 299–312. [Google Scholar] [CrossRef]
- Corrigan, P. How stigma interferes with mental health care. Am. Psychol. 2004, 59, 614–625. [Google Scholar] [CrossRef] [PubMed]
- Riffel, T.; Chen, S.P. Exploring the knowledge, attitudes, and behavioural responses of healthcare students towards mental illnesses-a qualitative study. Int. J. Environ. Res. Public Health 2019, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Ay, P.; Save, D.; Fidanoglu, O. Does stigma concerning mental disorders differ through medical education? A survey among medical students in Istanbul. Soc. Psychiatry Psychiatr. Epidemiol. 2006, 41, 63–67. [Google Scholar] [CrossRef]
- Abbey, S.; Charbonneau, M.; Tranulis, C.; Moss, P.; Baici, W.; Dabby, L.; Gautam, M.; Paré, M. Stigma and discrimination. Can. J. Psychiat. 2011, 56, 1–9. [Google Scholar]
- Sherwood, D.A. Healthcare curriculum influences on stigma towards mental illness: Core psychiatry course impact on pharmacy, nursing and social work student attitudes. Curr. Pharm. Teach. Learn. 2019, 11, 198–203. [Google Scholar] [CrossRef]
- Chang, S.; Ong, H.L.; Seow, E.; Chua, B.Y.; Abdin, E.; Samari, E.; Teh, W.L.; Chong, S.A.; Subramaniam, M. Stigma towards mental illness among medical and nursing students in Singapore: A cross-sectional study. BMJ Open 2017, 7, e018099. [Google Scholar] [CrossRef]
- Patten, S.B.; Remillard, A.; Phillips, L.; Modgill, G.; Szeto, A.C.; Kassam, A.; Gardner, D.M. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med. Educ. 2012, 12, 120. [Google Scholar] [CrossRef]
- Papish, A.; Kassam, A.; Modgill, G.; Vaz, G.; Zanussi, L.; Patten, S. Reducing the stigma of mental illness in undergraduate medical education: A randomized controlled trial. BMC Med. Educ. 2013, 13, 141. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martinez, C.; Sanchez-Martinez, V.; Sales-Orts, R.; Dinca, A.; Richart-Martinez, M.; Ramos-Pichardo, J.D. Effectiveness of direct contact intervention with people with mental illness to reduce stigma in nursing students. Int. J. Ment. Health Nurs. 2019, 28, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Knaak, S.; Patten, S.B. Building and Delivering Successful Anti-Stigma Programs for Healthcare Providers; Mental Health Commission of Canada: Calgary, AB, Canada, 2014. [Google Scholar]
- Knaak, S.; Patten, S. A grounded theory model for reducing stigma in health professionals in Canada. Acta Psychiatr. Scand. 2016, 134, s53–s62. [Google Scholar] [CrossRef] [PubMed]
- Knaak, S.; Ungar, T.; Patten, S. Seeing is believing: Biological information may reduce mental health stigma amongst physicians. Aust. N. Z. J. Psychiatry 2015, 49, 751–752. [Google Scholar] [CrossRef]
- Knaak, S.; Mantler, E.; Szeto, A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc. Manag. Forum 2017, 30, 111–116. [Google Scholar] [CrossRef]
- Mezirow, J. How Critical Reflection Triggers Transformative Learning. In Fostering Critical Reflection in Adulthood; Mezirow, J., Ed.; Jossey-Bass Publishers: San Francisco, CA, USA, 1990; pp. 1–6. [Google Scholar]
- Sukhera, J.; Chahine, S. Reducing mental illness stigma through unconscious bias-informed education. MedEdPublish 2016, 5. [Google Scholar] [CrossRef]
- Sukhera, J.; Watling, C. A framework for integrating implicit bias recognition into health professions education. Acad. Med. 2018, 93, 35–40. [Google Scholar] [CrossRef]
- Deb, T.; Lempp, H.; Bakolis, I.; Vince, T.; Waugh, W.; Henderson, C.; INDIGO READ Study Group. Responding to experienced and anticipated discrimination (READ): Anti-stigma training for medical students towards patients with mental illness—Study protocol for an international multisite non-randomised controlled study. BMC Med. Educ. 2019, 19, 41. [Google Scholar] [CrossRef]
- Bamgbade, B.A.; Barner, J.C.; Ford, K.H. Evaluating the impact of an anti-stigma intervention on pharmacy students’ willingness to counsel people living with mental illness. Community Ment. Health J. 2017, 53, 525–533. [Google Scholar] [CrossRef]
- Radmanović, M.B.; Burgić, S. Stigma and mental disorders in developmental age. Psychiatr. Danub. 2017, 29, 906–909. [Google Scholar]
- Link, B.G.; Cullen, F.T.; Frank, J.; Wozniak, J.F. The social rejection of former mental patients: Understanding why labels matter. Am. J. Sociol. 1987, 92, 1461–1500. [Google Scholar] [CrossRef]
- Lien, Y.J.; Kao, Y.C. Public beliefs and attitudes toward schizophrenia and depression in Taiwan: A nationwide survey. Psychiatry Res. 2019, 273, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.I.; Hsieh, C.E. Questionnaires on stigmatizing attitudes among healthcare students in Taiwan: Development and validation. BMC Med. Educ. 2020, 20, 59. [Google Scholar] [CrossRef] [PubMed]
- Ericsson, K.A.; Simon, H.A. Protocol Analysis: Verbal Reports as Data, Revised ed.; MIT Press: Cambridge, MA, USA, 1993. [Google Scholar]
- Aronson, L. Twelve tips for teaching reflection at all levels of medical education. Med. Teach. 2011, 33, 200–205. [Google Scholar] [CrossRef]
- Siegel, S.; Castellan, N.J. Nonparametric Statistics for the Behavioural Sciences, 2nd ed.; McGraw-Hill: New York, NY, USA, 1988. [Google Scholar]
- Helmus, K.; Schaars, I.K.; Wierenga, H.; de Glint, E.; van Os, J. Decreasing stigmatization: Reducing the discrepancy between “us” and “them”: An intervention for mental health care professionals. Front. Psychiatry 2019, 10, 243. [Google Scholar] [CrossRef]
- Friedrich, B.; Evans-Lacko, S.; London, J.; Rhydderch, D.; Henderson, C.; Thornicroft, G. Anti-stigma training for medical students: The Education Not Discrimination project. Br. J. Psychiatry 2013, 202, s89–s94. [Google Scholar] [CrossRef]
- Stier, A.; Hinshaw, S.P. Explicit and implicit stigma against individuals with mental illness. Aust. Psychol. 2007, 42, 106–117. [Google Scholar] [CrossRef]
- Fisher, R.J.; Katz, J.E. Social-desirability bias and the validity of self-reported values. Psychol. Mark. 2000, 17, 105–120. [Google Scholar] [CrossRef]
- Henderson, C.; Evans-Lacko, S.; Flach, C.; Thornicroft, G. Responses to mental health stigma questions: The importance of social desirability and data collection method. Can. J. Psychiatry 2012, 57, 152–160. [Google Scholar] [CrossRef]
- FitzGerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethics 2017, 18, 19. [Google Scholar] [CrossRef]
- Heim, E.; Henderson, C.; Kohrt, B.A.; Koschorke, M.; Milenova, M.; Thornicroft, G. Reducing mental health-related stigma among medical and nursing students in low- and middle-income countries: A systematic review. Epidemiol. Psychiatr. Sci. 2019, 29, e28. [Google Scholar] [CrossRef] [PubMed]
- Ungar, T.; Knaak, S.; Szeto, A.C. Theoretical and Practical Considerations for Combating Mental Illness Stigma in Health Care. Community Ment. Health J. 2016, 52, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.I.; Saint-Hilaire, M.; Thomas, C.A.; Tickle-Degnen, L. Stigma as a key determinant of health-related quality of life in Parkinson’s disease. Qual. Life Res. 2016, 25, 3037–3045. [Google Scholar] [CrossRef] [PubMed]
- Verhaeghe, M.; Bracke, P. Associative stigma among mental health professionals: Implications for professional and service user well-being. J. Health Soc. Behav. 2012, 53, 17–32. [Google Scholar] [CrossRef]
- Braveman, P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014, 129, 5–8. [Google Scholar] [CrossRef] [PubMed]
| Stage | Objectives | Activities/Assignments |
|---|---|---|
| Knowledge (cognition) | Understand the concept of stigma Understand the phenomena and influence of stigma in healthcare settings Identify social discrimination | Lecture Watch videos Movie “Mad World” In-class discussion |
| Experience (reflection) | Be aware of one’s own implicit stigma Be aware of one’s own stereotypes, prejudices, and discriminations against people with disorders/disabilities Experience the stigma-related feelings of people with disabilities and their caregivers | Accompanying a person with disability Roleplay a person with special characteristics ad his/her caregivers The human library ® |
| Action (practice) | Enhance friendly interaction between general society and persons with disorders/disabilities | Action project |
| Pre-Test | One-Year Follow-Up | |||
|---|---|---|---|---|
| Characteristics | Students Who Completed the Course (n = 16) | Students Who Dropped the Course (n = 11) | Students Who Completed the Course (n = 15) 2 | Students Who Dropped the Course (n = 10) 2 |
| Women (%) | 8 (50%) | 10 (91%) | 8 (53%) | 9 (90%) |
| Age, years (M ± SD) | 20.31 ± 1.195 | 19.91 ± 0.831 | 21 ± 1.254 | 21 ± 0.667 |
| SES 1 (M ± SD) | 3.44 ± 0.727 | 3.27 ± 0.467 | 3.27 ± 0.594 | 3.20 ± 0.422 |
| Have suffered from physical or mental illness | ||||
| Yes (%) | 0 | 1 (9%) | 1 (7%) | 1 (10%) |
| Have family members or friends with disabilities | ||||
| Yes (%) | 8 (50%) | 4 (36%) | 7 (47%) | 3 (30%) |
| Items | Pre-Test (T1) | Post-Test (T2) | One-Year Follow-Up (T3) | χ2 | Post Hoc Test |
|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | |||
| I would accept a person with mental illness as a neighbour. | 2.93 ± 0.88 | 2.20 ± 0.56 | 1.80 ± 0.68 | 14.93 ** | T1 > T3 |
| I would accept a person with mental illness as a co-worker. | 3.07 ± 0.62 | 2.07 ± 0.62 | 1.79 ± 0.70 | 19.4 *** | T1 > T2 T1 > T3 |
| I would accept a person with mental illness as a friend. | 2.40 ± 0.91 | 1.60 ± 0.63 | 1.53 ± 0.74 | 10.85 ** | - |
| I would accept a person with mental illness to rent my house. | 3.33 ± 0.62 | 2.27 ± 0.80 | 2.20 ± 0.86 | 16.18 *** | T1 > T2 T1 > T3 |
| I would recommend a person with mental illness for a job. | 2.60 ± 0.91 | 1.73 ± 0.88 | 1.73 ± 0.70 | 12.79 ** | T1 > T2 T1 > T3 |
| I would accept a person with mental illness as an in-law. | 3.33 ± 1.047 | 2.93 ± 0.80 | 2.93 ± 0.96 | 3.05 | - |
| I would accept a person with mental illness to take care of my child. | 4.07 ± 0.88 | 3.20 ± 1.01 | 3.27 ± 1.03 | 8.21 * | - |
| Domains | Pre-Test (T1) | Post-Test (T2) | One-Year Follow-Up (T3) | χ2 | Post Hoc Test |
|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | |||
| Stigmatising attitudes towards mental illness | |||||
| Deviant behaviour | 3.47 ± 0.95 | 2.13 ± 0.79 | 2.51 ± 0.77 | 13.62 ** | T1 > T2 T1 > T3 |
| Social isolation | 2.69 ± 0.85 | 2.04 ± 0.55 | 1.73 ± 0.34 | 14.80 ** | T1 > T2 T1 > T3 |
| Negative stereotype | 2.04 ± 0.68 | 1.52 ± 0.53 | 1.77 ± 0.79 | 6.37 * | - |
| Self-stigma | 2.27 ± 0.81 | 1.69 ± 0.62 | 2.11 ± 0.87 | 3.57 | - |
| Average | 2.62 ± 0.61 | 1.80 ± 0.48 | 2.00 ± 0.55 | 11.58 ** | T1 > T2 |
| Stigmatising attitudes towards children with emotional behavioural disorders (EBD) | |||||
| Rejective attitude | 2.41 ± 0.68 | 2.13 ± 0.35 | 1.98 ± 0.68 | 2.18 | - |
| Deviant behaviour | 2.95 ± 0.67 | 2.42 ± 0.68 | 2.34 ± 0.60 | 9.72 ** | T1 > T3 |
| Negative stereotype | 2.89 ± 0.70 | 2.33 ± 0.60 | 2.07 ± 0.63 | 10.33 ** | T1 > T3 |
| Average | 2.77 ± 0.57 | 2.31 ± 0.51 | 2.18 ± 0.57 | 8.78 * | T1 > T3 |
| Stigmatising attitudes towards disabilities | |||||
| Negative stereotype | 2.80 ± 1.01 | 2.51 ± 1.04 | 2.76 ± 1.02 | 4.50 | - |
| Pessimistic expectation | 2.69 ± 0.89 | 2.49 ± 0.69 | 2.51 ± 0.80 | 1.04 | - |
| Average | 2.74 ± 0.88 | 2.50 ± 0.82 | 2.63 ± 0.85 | 4.42 | - |
| Domains/Items | Drop | Complete 1 | Z | ||
|---|---|---|---|---|---|
| Pre-Test | One-Year Follow-Up | Change Scores | Change Scores | ||
| M ± SD | M ± SD | M ± SD | M ± SD | ||
| Stigmatising attitudes towards | |||||
| Mental illness | 2.27 ± 0.62 | 2.16 ± 0.66 | −0.11 ± 0.81 | −0.61 ± 0.78 | −1.73 |
| EBD 2 | 2.52 ± 0.90 | 2.39 ± 0.71 | −0.14 ± 0.92 | −0.59 ± 0.75 | −1.76 |
| Disability | 2.74 ± 0.88 | 3.22 ± 0.28 | −0.10 ± 1.04 | −0.11 ± 0.64 | 1.00 |
| Social Distance Scale | |||||
| As a neighbour | 2.40 ± 0.70 | 2.40 ± 0.97 | 0 ± 1.24 | −1.13 ± 0.83 | −2.27 * |
| As a co-worker | 2.20 ± 0.79 | 2.20 ± 0.79 | 0 ± 1.05 | −1.29 ± 0.83 | −2.74 ** |
| As a friend | 1.90 ± 0.57 | 2.10 ± 0.88 | 0.20 ± 0.79 | −0.87 ± 1.06 | −2.43 * |
| To rent house | 2.50 ± 0.53 | 2.80 ± 0.92 | 0.30 ± 0.95 | −1.13 ± 0.99 | −3.02 ** |
| Recommend job | 1.90 ± 0.57 | 1.80 ± 0.63 | −0.10 ± 0.57 | −0.87 ± 0.92 | −2.22 * |
| As an in-law | 3.10 ± 0.99 | 3.00 ± 0.94 | −0.10 ± 1.10 | −0.40 ± 1.06 | −0.78 |
| Take care of my child | 3.70 ± 0.68 | 3.40 ± 1.08 | −0.30 ± 0.82 | −0.80 ± 1.08 | −1.34 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, H.-I.; Hsieh, C.-E. An Anti-Stigma Course for Occupational Therapy Students in Taiwan: Development and Pilot Testing. Int. J. Environ. Res. Public Health 2020, 17, 5599. https://doi.org/10.3390/ijerph17155599
Ma H-I, Hsieh C-E. An Anti-Stigma Course for Occupational Therapy Students in Taiwan: Development and Pilot Testing. International Journal of Environmental Research and Public Health. 2020; 17(15):5599. https://doi.org/10.3390/ijerph17155599
Chicago/Turabian StyleMa, Hui-Ing, and Chu-En Hsieh. 2020. "An Anti-Stigma Course for Occupational Therapy Students in Taiwan: Development and Pilot Testing" International Journal of Environmental Research and Public Health 17, no. 15: 5599. https://doi.org/10.3390/ijerph17155599
APA StyleMa, H.-I., & Hsieh, C.-E. (2020). An Anti-Stigma Course for Occupational Therapy Students in Taiwan: Development and Pilot Testing. International Journal of Environmental Research and Public Health, 17(15), 5599. https://doi.org/10.3390/ijerph17155599




