Toward an Integrative Nursing Curriculum: Combining Team-Based and Problem-Based Learning with Emergency-Care Scenario Simulation
Abstract
1. Introduction
2. Material and Methods
- ➢
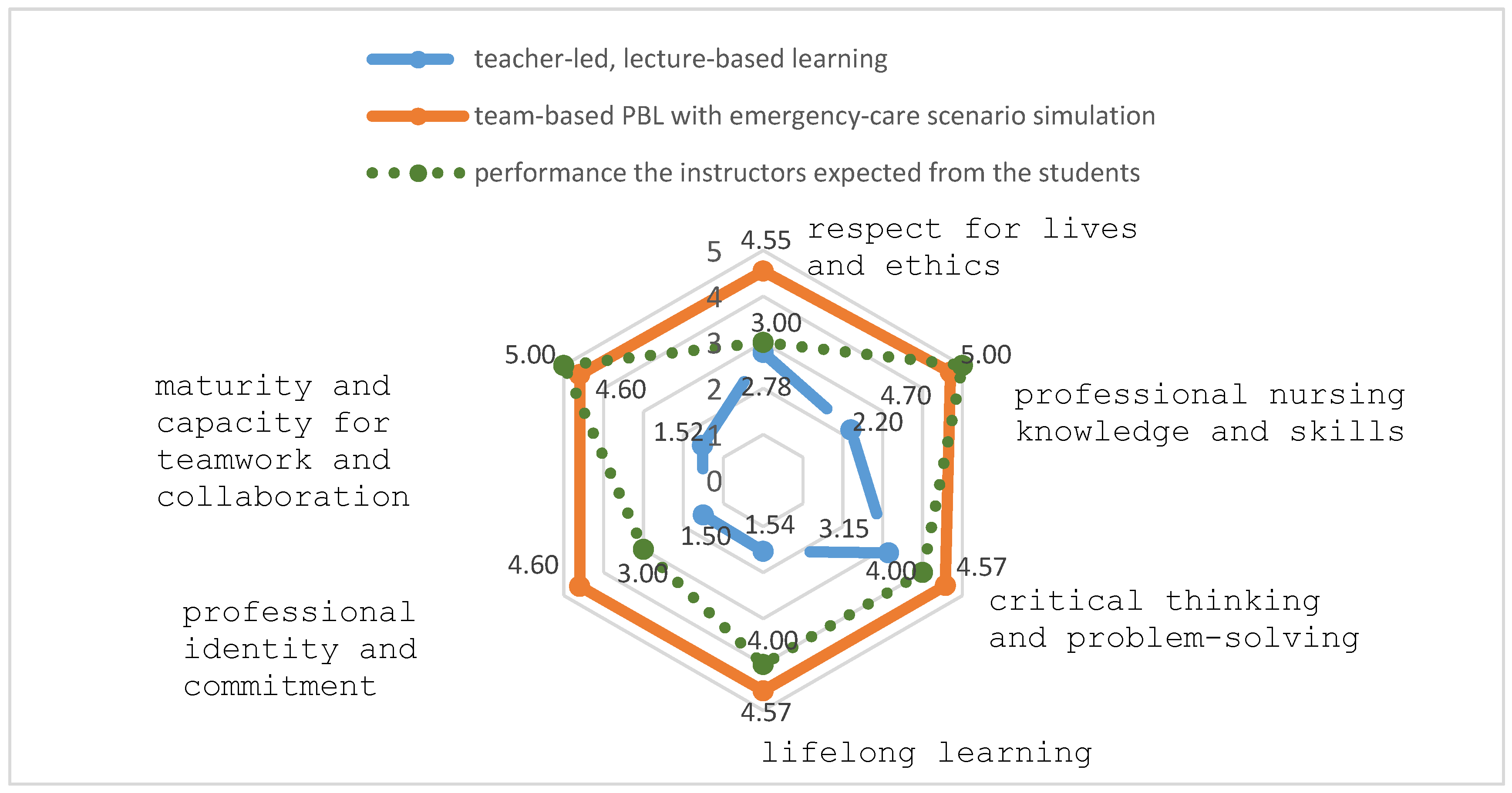
- To compare how two different groups of students, namely, students exposed to the integrative curriculum vs. students exposed to traditional teaching methods, performed on tests designed to gauge their core nursing competencies.
- ➢
- To compare the students’ actual performance on tests of their core nursing competencies with the performance that instructors expected from them.
- ➢
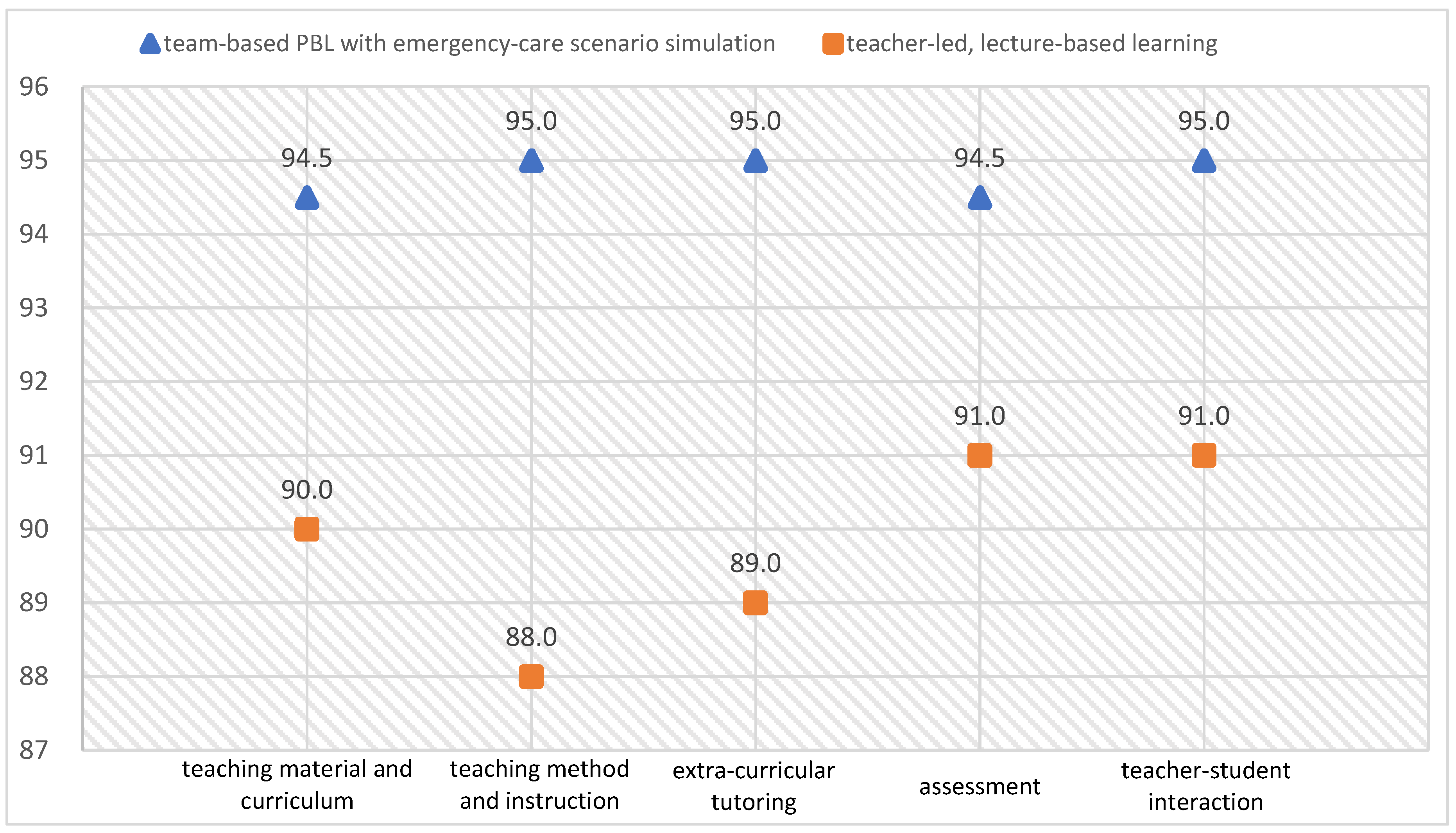
- To compare how the two different groups of students, namely, students exposed to the integrative curriculum vs. students exposed to traditional teaching methods evaluated their teacher’s performance.
2.1. Participants and Research Design
2.2. Toward an Integrative Curriculum: Combining Team-Based Problem-Based Learning (PBL) with Emergency-Care Scenario Simulation
2.3. Teaching Procedure
2.4. Measures
2.4.1. Scale of Core Nursing Competencies
2.4.2. Teacher Performance Evaluation Scale
2.4.3. Students’ Reflection Logs
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. The Calculation Results for TOPSIS
| Criterion | |||||
|---|---|---|---|---|---|
| Alternative | Teaching Material and Curriculum | Teaching Method and Instruction | Extra-Curricular Tutoring | Assessment | Teacher–Student Interaction |
| Traditional Teaching Methods | 0.689655 | 0.679562 | 0.683686 | 0.693642 | 0.69174 |
| Integrative Curriculum | 0.724138 | 0.733618 | 0.729777 | 0.72032 | 0.722146 |
| Criterion | |||||
|---|---|---|---|---|---|
| Alternative | Teaching Material and Curriculum | Teaching Method and Instruction | Extra-Curricular Tutoring | Assessment | Teacher–Student Interaction |
| Traditional Teaching Methods | 0.137931 | 0.135912 | 0.136737 | 0.138728 | 0.138348 |
| Integrative Curriculum | 0.144828 | 0.146724 | 0.145955 | 0.144064 | 0.144429 |
| Criterion | |||||
|---|---|---|---|---|---|
| Ideal Solution | Teaching Material and Curriculum | Teaching Method and Instruction | Extra-Curricular Tutoring | Assessment | Teacher–Student Interaction |
| P+ | 0.144828 | 0.146724 | 0.145955 | 0.144064 | 0.144429 |
| P− | 0.137931 | 0.135912 | 0.136737 | 0.138728 | 0.138348 |
| Alternative | S+ | S− | Ci | Rank |
|---|---|---|---|---|
| Traditional Teaching Methods | 0.017745 | 0 | 0 | 2 |
| Integrative Curriculum | 0 | 0.017745 | 1 | 1 |
References
- Ministry of Health and Welfare. National Health Insurance Annual Statistical Report 2018. 2019. Available online: https://www.mohw.gov.tw/cp-4574-49817-2.html (accessed on 12 December 2019).
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Campo, T.; Comer, A.; Evans, D.D.; Kincaid, K.; Norton, L.; Ramirez, E.; Smith, A.; Stackhouse, K.; Wilbeck, J. Practice standards for the emergency nurse practitioner specialty. Adv. Emerg. Nurs. J. 2018, 40, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Harley, C.; Pini, S.; Kenyon, L.; Daffu-O’Reilly, A.; Velikova, G. Evaluating the experiences and support needs of people living with chronic cancer: Development and initial validation of the Chronic Cancer Experiences Questionnaire (CCEQ). BMJ Support. Palliat. Care 2019, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Vipond, J.; Mennenga, H.A. Screening, Brief Intervention, and Referral to Treatment by Emergency Nurses: A Review of the Literature. J. Emerg. Nurs. 2019, 45, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Lam, S.K.K.; Kwong, E.W.Y.; Hung, M.S.Y.; Pang, S.M.C.; Chien, W.T. Emergency nurses’ perceptions of their roles and practices during epidemics: A qualitative study. Br. J. Nurs. 2019, 28, 523–527. [Google Scholar] [CrossRef] [PubMed]
- Servant-Miklos, V.F.C. Fifty Years on: A Retrospective on the World’s First Problem-based Learning Programme at McMaster University Medical School. Health Prof. Edu. 2019, 5, 3–12. [Google Scholar] [CrossRef]
- Hmelo-Silver, C. Problem-based learning: What and how do students learn? Educ. Psychol. Rev. 2004, 16, 235–266. [Google Scholar] [CrossRef]
- Kong, L.N.; Qin, B.; Zhou, Y.Q.; Mou, S.Y.; Gao, H.M. The effectiveness of problem-based learning on development of nursing students’ critical thinking: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2014, 51, 458–469. [Google Scholar] [CrossRef]
- Li, Y.; Wang, X.; Zhu, X.R.; Zhu, Y.S.; Sun, J. Effectiveness of problem-based learning on the professional communication competencies of nursing students and nurses: A systematic review. Nurs. Edu. Pract. 2019, 37, 45–55. [Google Scholar] [CrossRef]
- Lee, Y.L.; Gau, B.S.; Chang, M.; Yang, H.L.; Tsai, S. The Application of Problem-based Learning in a Pediatric Nursing Bachelor Program. J. Med. Edu. 2007, 11, 284–296. [Google Scholar]
- Lee, S.H.; Lin, Y.J.; Yen, W.J.; Liao, W.C.; Yuan, S.C.; Kuo, P.C.; Kuo, C.P.; Lee, S.; Lee, M.C. Learning Experiences of Junior Nursing Students in a Pilot Learning Experiences of Junior Nursing Students in a Pilot Problem-Based Learning Program. Chung Shan Med. J. 2010, 21, 79–89. [Google Scholar] [CrossRef]
- Tang, L.C.; Tsai, C.H.; Tsai, C.S. Intrinsic motivation in problem-based learning: A preliminary study of promoting elements in wwo Taiwan universities. J. Health Sci. 2008, 10, 65–76. [Google Scholar] [CrossRef]
- Chiu, W.H.; Chao, S.Y. A Reflection on innovative nursing teaching strategies following an experience training competitors for the worldskills competition. J. Nurs. 2018, 65, 26–31. [Google Scholar]
- Nation, L.M.; Tweddell, S.; Rutter, P. The applicability of a validated team-based learning student assessment instrument to assess United Kingdom pharmacy students’ attitude toward team-based learning. J. Edu. Eval. Health Prof. 2016, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Roberts, C.; Ayton, T.; Mellis, C. Implementation of modified team-based learning within a problem based learning medical curriculum: A focus group study. BMC Med. Edu. 2018, 18, 74. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Haq, I.; Bleasel, J.; Roberts, C.; Garsia, R.; Randal, N.; Mellis, C. Team-based learning (TBL): A community of practice. BMC Med. Edu. 2019, 19, 369. [Google Scholar] [CrossRef] [PubMed]
- Pham, J.C.; Story, J.L.; Hicks, R.W.; Shore, A.D.; Morlock, L.L.; Cheung, D.S.; Kelen, G.D.; Pronovost, P.J. National study on the frequency, types, causes, and consequences of voluntarily reported Emergency Department medication errors. J. Emerg. Med. 2011, 40, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Tanaka, K.; Takano, T.; Kato, N.; Watanabe, M.; Miyaoka, H. Analysis of risk of medical errors using structural-equation modelling: A 6-month prospective cohort study. BMJ Qual. Saf. 2012, 21, 784–790. [Google Scholar] [CrossRef]
- Saintsing, D.; Gibson, L.M.; Pennington, A.W. The novice nurse and clinical decision-making: How to avoid errors. J. Nurs. Manag. 2011, 19, 354–359. [Google Scholar] [CrossRef]
- Lewis, K.A.; Ricks, T.N.; Rowin, A.; Ndlovu, C.; Goldstein, L.; McElvogue, C. Does simulation training for acute care nurses improve patient safety outcomes: A systematic review to inform Evidence-based practice. Worldviews Evid. Based Nurs. 2019, 16, 389–396. [Google Scholar] [CrossRef]
- Kenaszchuk, C.; MacMillan, K.; van Soeren, M.; Reeves, S. Interprofessional simulated learning: Short term associations between simulation and interprofessional collaboration. BMC Med. 2011, 9, 29. [Google Scholar] [CrossRef]
- ZarifSanaiey, N.; Amini, M.; Saadat, F. A comparison of educational strategies for the acquisition of nursing student’s performance and critical thinking: Simulation-based training vs. integrated training (simulation and critical thinking strategies). BMC Med. Edu. 2016, 16, 294. [Google Scholar] [CrossRef] [PubMed]
- Motola, I.; Devine, L.; Chung, H.S.; Sullivan, J.E.; Issenberg, B. Simulation in healthcare education: A best evidence practical guide [AMEE Guide No. 82]. Med. Teach. 2013, 35, 1511–1530. [Google Scholar] [CrossRef] [PubMed]
- Norman, J. A systematic review of the literature on simulation in nursing education. ABNF J. 2012, 23, 24–28. [Google Scholar] [PubMed]
- Grant, A.W.; Buckley, D.J. Nurse experiences and confidence in treating critically ill and injured patients following the completion of the First Line Emergency Care Course. Australas. Emerg. Care 2019, 22, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Hyland, J.R.; Hawkins, M.C. High-fidelity human simulation in nursing education: A review of literature and guide for implementation. Teach. Learn. Nurs. 2009, 4, 14–21. [Google Scholar] [CrossRef]
- Newman, M.A. Theory Development in Nursing; Davis Company: Philadelphia, PA, USA, 1979. [Google Scholar]
- Pavlish, C.P.; Pharris, M.D. Community-based Collaborative Action Research: A Nursing Approach; Jones and Bartlett: Sudbury, MA, USA, 2012. [Google Scholar]
- Hwang, C.L.; Yoon, K. Multiple Attribute Decision Making: Methods and Applications; Springer: New York, NY, USA, 1981. [Google Scholar]
- Shin, S.; Park, J.H.; Kim, J.H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ. Today 2015, 35, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Wosinski, J.; Belcher, A.E.; Dürrenberger, Y.; Allin, A.C.; Stormacq, C.; Gerson, L. Facilitating problem-based learning among undergraduate nursing students: A qualitative systematic review. Nurse Educ. Today 2018, 60, 67–74. [Google Scholar] [CrossRef]
- Darling-Hammond, L.; Flook, L.; Cook-Harvey, C.; Barron, B.; Osher, D. Implications for educational practice of the science of learning and development. Appl. Dev. Sci. 2019, 24, 97–140. [Google Scholar] [CrossRef]
| Stage | Task |
|---|---|
| Analysis & Design | Integrating social and healthcare needs, identifying causes of accidents and injuries, and defining the goals of the various nursing disciplines |
| Defining instructional themes and designing specific lesson plans | |
| Development | Developing lesson plans, setting the learning goals for each emergency-care scenario, and formulating the scenario content |
| Rechecking/confirming the teaching and learning strategies to be used in the course including the particular steps that will be followed to integrate team-based PBL with emergency-care scenario simulations | |
| Confirming the evaluation tools that will be used to measure student outcomes | |
| Implementation & Application | Team arrangement and task assignment |
| The team-based PBL case discussion | |
| Evaluation | Evaluating learning outcomes |
| Understanding the reactions of students and instructors | |
| Improving and revising the lesson plans |
| Stage | Step | PBL Themes | Teaching Methods | Teaching Content |
|---|---|---|---|---|
| I | 1 | Defining healthcare problems and needs (time: 10 min) | Lecture and instruction Team-based discussion | Providing emergency-care scenario cases for the team-based PBL Collaborative study of the emergency-care scenario cases to identify crucial facts and clues, with the aim of determining what kinds of care should be provided. |
| 2 | Exploring the areas of knowledge students have mastered previously (time: 20 min) | Team-based discussion | Applying past pathophysiology knowledge and nursing care skills to explore the possible health needs in the emergency-care scenario cases | |
| 3 | Forming assumptions and identifying possible mechanisms (time: 15 min) | Team inquiry Instructor-guided discussion of assumptions and mechanisms | Applying prior knowledge and skills to establish causal relationships, potential biopathological mechanisms, and relevant assumptions Developing nursing care options Reading the prepared reference material to think critically about the feasibility of implementing nursing care | |
| II | 4 | Defining learning issues (time: 10 min) | Team-based discussion Logical induction | Setting learning goals Logical induction after team-based discussion to confirm primary and secondary learning goals Constructing a conceptual framework based on learning content |
| 5 | Self-study & application of nursing skills (time: 45 min) | Self-learning, i.e., self-directed inquiry Demonstration and practice | Providing learning resources Students acquire, analyze, and apply new knowledge and skills in order to develop possible nursing-care options Nursing-care skills demonstration and practice | |
| III | 6 | The integration of new knowledge and skills with prior knowledge to solve case problems (time: 50 min) | Scenario simulation Skills practice and demonstration | Class presentations Simulating situational communication and collaboration to solve the healthcare problems in the scenario cases Hands-on skills practice and demonstration |
| 7 | Evaluation and reflection (time: 50 min) | Team observation, discussion, and reflection | Feedback and evaluation Knowledge and skills revision |
| Teaching Manual | Content |
|---|---|
| Scenario Case | Topic: A middle-aged father with severe chest pain |
| Preface | Students’ prerequisite knowledge: basic medical science, medical-surgical nursing |
| Learning goals: developing and integrating nursing students’ competencies in cardiovascular medicine and nursing knowledge, emergency-care skills, communication, and teamwork and collaboration | |
| Lesson plan summary: briefly explaining the content of the lesson plan and the theme to be explored | |
| Class management: the distribution of scenario case material every week | |
| Scenario Content | Mr. Chang, 50 years old, comes to the emergency department for medical treatment because of his shortness of breath and his difficulties walking. Over the past week, his feet have been swollen, his weight has increased by 2 kg, and his whole body has felt weak and tired. In the middle of the night, he often wakes up with difficulty breathing. Today, just by moving around, he once again feels shortness of breath and breaks into a cold sweat. He therefore goes to an emergency department for treatment. The doctor’s diagnosis is CHF FC: III/IV. You are an emergency nurse; please show us how you will carry out your nursing assessment. |
| Main background information: | |
| Medical history: The patient has had a history of hypertension for the past 5 years, but he has not been taking medication according to the doctor’s orders. After taking a short rest, he usually recovers enough to catch his breath and continue with his activities. | |
| Emergency vital signs: TPR: 36 °C, 90 times/min, 26 times/min, BP: 160/90 mmHg. SpO2: 93%. | |
| Evaluation data from a systematic physical examination: | |
| Respiratory system: auscultation of lung-breath sounds reveals rales in the lower lobes on of the lungs | |
| Teaching Guide | Key learning points in the scenario simulation case: |
| Systematically collect information relating to this patient’s circulatory problems—both subjective and objective information | |
| Common nursing problems for emergency patients with circulatory disturbance | |
| Emergency nursing management of patients with decreased cardiac output | |
| Key Points | Decreased cardiac output |
| CHF (congestive heart failure) | |
| Learning Issues | Introducing the key points that students must discuss in this scenario-simulation case: |
| Myocardial tissue perfusion system | |
| Emergency treatment and management of decreased cardiac output | |
| Definition of heart failure and its pathophysiology and treatment/management | |
| Raising Questions | Use the key points of study to write out brief questions for which the instructors’ guidance is sought |
| Example: How do I help the patient get relief from the symptoms of dyspnea, such as gasping for breath? | |
| References | Brief reference materials provided by the instructors: |
| Pathophysiological signs of patients with heart failure | |
| Emergency care for patients with heart failure |
| Criterion | |||||
|---|---|---|---|---|---|
| Alternative | Teaching Material and Curriculum | Teaching Method and Instruction | Extra-Curricular Tutoring | Assessment | Teacher-Student Interaction |
| Traditional Teaching Methods | 90 | 88 | 89 | 91 | 91 |
| Integrative Curriculum | 94.5 | 95 | 95 | 94.5 | 95 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.-Y.; Wang, Y.-h. Toward an Integrative Nursing Curriculum: Combining Team-Based and Problem-Based Learning with Emergency-Care Scenario Simulation. Int. J. Environ. Res. Public Health 2020, 17, 4612. https://doi.org/10.3390/ijerph17124612
Huang C-Y, Wang Y-h. Toward an Integrative Nursing Curriculum: Combining Team-Based and Problem-Based Learning with Emergency-Care Scenario Simulation. International Journal of Environmental Research and Public Health. 2020; 17(12):4612. https://doi.org/10.3390/ijerph17124612
Chicago/Turabian StyleHuang, Cheng-Yi, and Ya-huei Wang. 2020. "Toward an Integrative Nursing Curriculum: Combining Team-Based and Problem-Based Learning with Emergency-Care Scenario Simulation" International Journal of Environmental Research and Public Health 17, no. 12: 4612. https://doi.org/10.3390/ijerph17124612
APA StyleHuang, C.-Y., & Wang, Y.-h. (2020). Toward an Integrative Nursing Curriculum: Combining Team-Based and Problem-Based Learning with Emergency-Care Scenario Simulation. International Journal of Environmental Research and Public Health, 17(12), 4612. https://doi.org/10.3390/ijerph17124612





