Nutrition-Related Adverse Outcomes in Endurance Sports Competitions: A Review of Incidence and Practical Recommendations
Abstract
:1. Introduction
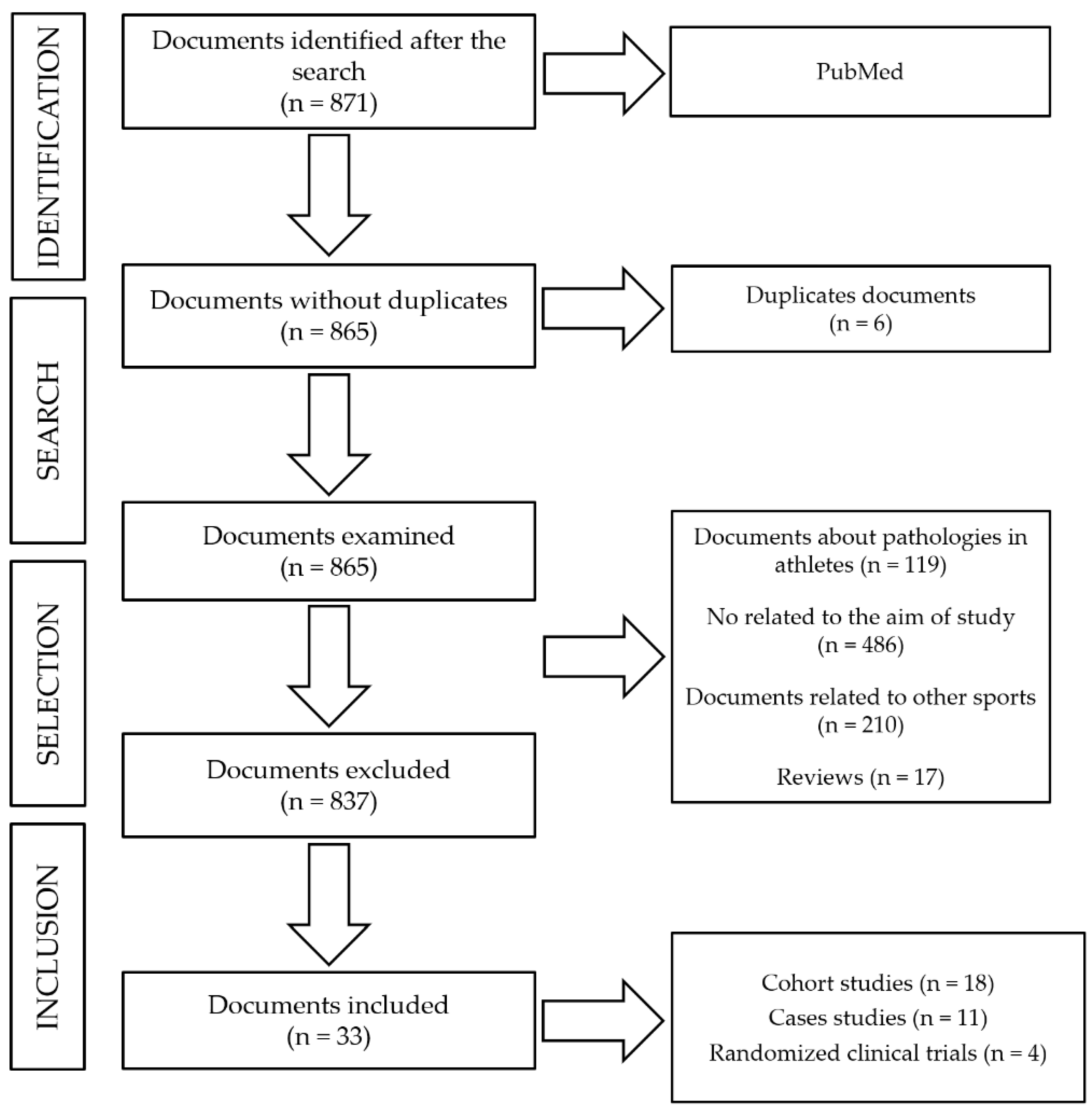
2. Materials and Methods
- Human studies related to adverse outcomes that occur in endurance and ultra-endurance athletes during competitions.
- Type of study: cohort-study, case studies or clinical trials.
- Published in English or Spanish.
- Articles published from 2008 to 2019.
- Study: authors and year of publication
- Objective: purpose for which the study was carried out.
- Sample: number of subjects trained for the activities, sports discipline, and sex.
- Sports competition: type of competition where adverse outcomes detected, place and year of occurrence.
- Adverse outcomes: type of adverse effect found.
- -
- Incidence: number or % of cases of adverse outcomes suffered by athletes during the competition.
- -
- Causes: established after the investigation, triggers of said problems suffered during the competition
- Conclusions: obtained from the research and reached by the authors themselves.
3. Results
4. Discussion
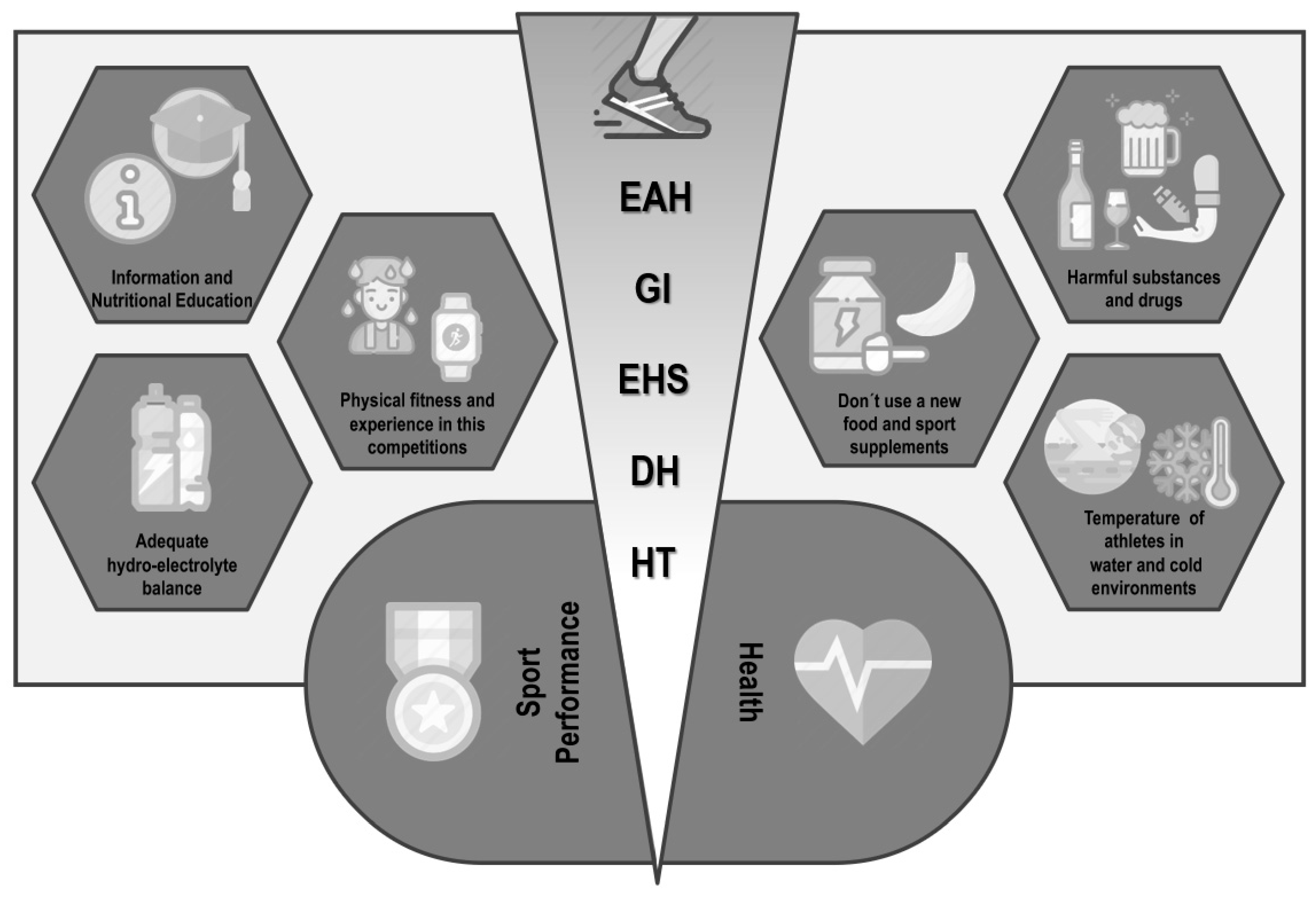
4.1. Exercise-Associated Hyponatremia (EAH) and Dehydration (DH)
4.2. Gastrointestinal (GI) Problems during Physical Exercise
4.3. Stress Heat Stroke (EHS) during Physical Exercise under Extreme Weather Conditions
4.4. Hypothermia (HT)
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
References
- Ganio, M.S.; Klau, J.F.; Casa, D.J.; Armstrong, L.E.; Maresh, C.M. Effect of caffeine on sport-specific endurance performance: A systematic review. J. Strength Cond. Res. 2009, 23, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.R. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 2000, 32, 70. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, R.; Cuenca, E.; Maté-Muñoz, J.L.; Garca-Fernández, P.; Paya, N.S.; Estevan, M.D.C.L.; Veiga-Herreros, P.; Garnacho-Castaño, M. Effects of beetroot juice supplementation on cardiorespiratory endurance in athletes. A systematic review. Nutrients 2017, 9, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pate, R.R.; Branch, J.D. Training for endurance sport. Med. Sci. Sports Exerc. 1992, 24, S340–S343. [Google Scholar] [CrossRef]
- Jeukendrup, A.E. Nutrition for endurance sports: Marathon, triathlon, and road cycling. J. Sports Sci. 2011, 29, S91–S99. [Google Scholar] [CrossRef]
- Pedrinolla, A.; Volti, G.L.; Galvano, F.; Schena, F.; Perciavalle, V.; Di Corrado, D. Bioenergetics and psychological profile of an ultra endurance walker. J. Sports Med. Phys. Fit. 2017, 58, 549–554. [Google Scholar]
- Krabak, B.J.; Waite, B.; Lipman, G. Injury and illnesses prevention for ultramarathoners. Curr. Sports Med. Rep. 2013, 12, 183–189. [Google Scholar] [CrossRef]
- Six, C.; Aboukais, S.; Giron, S.; D’Oliveira, J.-C.; Peloux-Petiot, F.; Franke, F.; Terrien, H.; Dassonville, F.; Deniau, J.; Ambert-Balay, K.; et al. Outbreak of diarrhoeal illness in participants in an obstacle adventure race, Alpes-Maritimes, France, June 2015. Eurosurveillance 2016, 21. [Google Scholar] [CrossRef]
- Urdampilleta, A.; Martínez-Sanz, J.M. Medical and nutritional risk and dietary planning in mountaineering. Eur. J. Hum. Mov. 2012, 28, 35–66. [Google Scholar]
- López-Gómez, J.A.; Martínez-Sanz, J.M.; Martínez-Rodríguez, A.; Ortiz-Moncada, R. Planificación dietético-nutricional para llevar a cabo una Ultramaratón, la Transvulcania: Informe de caso. Revista Española Nutrición Humana Dietética 2016, 20, 120. [Google Scholar] [CrossRef] [Green Version]
- Hoffman, M.D.; Joslin, J.; Rogers, I.R. Management of suspected fluid balance issues in participants of wilderness endurance events. Curr. Sports Med. Rep. 2017, 16, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Cairns, R.S.; Hew-Butler, T. Incidence of exercise-associated hyponatremia and its association with nonosmotic stimuli of arginine vasopressin in the GNW100s ultra-endurance marathon. Clin. J. Sport Med. 2015, 25, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Danz, M.; Tönjes, P.M.; Pöttgen, K.; Hinkelbein, J.; Braunecker, S. Hyponatremia among triathletes in the ironman European Championship. N. Engl. J. Med. 2016, 374, 997–998. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.; Jones, N.; Martin, D.; Kipps, C. ‘Too much of a coincidence’: Identical twins with exertional heatstroke in the same race. BMJ Case Rep. 2016, 2016. [Google Scholar] [CrossRef]
- Grundstein, A.J.; Hosokawa, Y.; Casa, U.J. Fatal exertional heat stroke and american football players: The need for regional heat-safety guidelines. J. Athl. Train. 2018, 53, 43–50. [Google Scholar] [CrossRef] [Green Version]
- Katch, R.K.; Scarneo, S.E.; Adams, W.M.; Armstrong, L.E.; Belval, L.N.; Stamm, J.M.; Casa, U.J. Top 10 research questions related to preventing sudden death in sport and physical activity. Res. Q. Exerc. Sport 2017, 88, 251–268. [Google Scholar] [CrossRef]
- Stearns, R.L.; Casa, D.J.; O’Connor, F.G.; Lopez, R. A tale of two heat strokes: A comparative case study. Curr. Sports Med. Rep. 2016, 15, 94–97. [Google Scholar] [CrossRef] [Green Version]
- Fudge, J. Exercise in the cold: Preventing and managing hypothermia and frostbite injury. Sports Health 2016, 8, 133–139. [Google Scholar] [CrossRef] [Green Version]
- Montain, S.J.; Latzka, W.A.; Sawka, M.N. Control of thermoregulatory sweating is altered by hydration level and exercise intensity. J. Appl. Physiol. 1995, 79, 1434–1439. [Google Scholar] [CrossRef]
- Whitney, E.N.; Rolfes, S.R. Understanding Nutrition; Thomson/Wadsworth: London, UK, 2008; ISBN 9780495116868. [Google Scholar]
- Waterman, J.J.; Kapur, R. Upper gastrointestinal issues in athletes. Curr. Sports Med. Rep. 2012, 11, 99–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Oliveira, E.P.; Burini, R.C.; Jeukendrup, A. Gastrointestinal complaints during exercise: Prevalence, etiology, and nutritional recommendations. Sports Med. 2014, 44, S79–S85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Oliveira, E.P. Runner’s diarrhea: What is it, what causes it, and how can it be prevented? Curr. Opin. Gastroenterol. 2017, 33, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Parkkali, S.; Joosten, R.; Fanoy, E.; Pijnacker, R.; Van Beek, J.; Brandwagt, D.; Van Pelt, W. Outbreak of diarrhoea among participants of a triathlon and a duathlon on 12 July 2015 in Utrecht, The Netherlands. Epidemiol. Infect. 2017, 145, 2176–2184. [Google Scholar] [CrossRef] [Green Version]
- Meyer, D.J.; Costantino, A.; Spano, S. An assessment of diarrhea among long-distance backpackers in the Sierra Nevada. Wilderness Environ. Med. 2017, 28, 4–9. [Google Scholar] [CrossRef] [Green Version]
- Magee, P.J.; Gallagher, A.; McCormack, J.M. High prevalence of dehydration and inadequate nutritional knowledge among University and Club level athletes. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 158–168. [Google Scholar] [CrossRef]
- Brustia, R.; Enrione, G.; Catuzzo, B.; Cavoretto, L.; Campagnoni, M.P.; Visetti, E.; Cauchy, E.; Ziegler, S.; Giardini, G. Results of a Prospective Observational Study on Mountaineering Emergencies in Western Alps: Mind your head. High Alt. Med. Biol. 2016, 17, 116–121. [Google Scholar] [CrossRef]
- Chlíbková, D.; Rosemann, T.; Posch, L.; Matoušek, R.; Knechtle, B. Pre- and post-race hydration status in hyponatremic and non-hyponatremic ultra-endurance athletes. Chin. J. Physiol. 2016, 59, 173–183. [Google Scholar] [CrossRef]
- Joslin, J.; Mularella, J.; Bail, A.; Wojcik, S.; Cooney, D.R. Mandatory rest stops improve athlete safety during event medical coverage for ultramarathons. Prehosp. Disaster Med. 2016, 31, 43–45. [Google Scholar] [CrossRef]
- Stuempfle, K.J.; Hoffman, M.D. Gastrointestinal distress is common during a 161-km ultramarathon. J. Sports Sci. 2015, 33, 1–8. [Google Scholar] [CrossRef]
- Hoffman, M.D.; Hew-Butler, T.; Stuempfle, K.J. Exercise-associated hyponatremia and hydration status in 161-km ultramarathoners. Med. Sci. Sports Exerc. 2013, 45, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Rüst, C.A. Higher prevalence of exercise-associated hyponatremia in triple iron ultra-triathletes than reported for ironman triathletes. Chin. J. Physiol. 2012, 55, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Mexia, R.; Vold, L.; Heier, B.T.; Nygård, K. Gastrointestinal disease outbreaks in cycling events: Are preventive measures effective? Epidemiol. Infect. 2012, 141, 517–523. [Google Scholar] [CrossRef]
- Hoffman, M.D.; Stuempfle, K.J.; Rogers, I.R.; Weschler, L.B.; Hew-Butler, T. Hyponatremia in the 2009 161-km Western States Endurance Run. Int. J. Sports Physiol. Perform. 2012, 7, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.D.; Fogard, K. Factors related to successful completion of a 161-km ultramarathon. Int. J. Sports Physiol. Perform. 2011, 6, 25–37. [Google Scholar] [CrossRef]
- Bruso, J.R.; Hoffman, M.D.; Rogers, I.R.; Lee, L.; Towle, G.; Hew-Butler, T. Rhabdomyolysis and Hyponatremia: A cluster of five cases at the 161-km 2009 Western States Endurance Run. Wilderness Environ. Med. 2010, 21, 303–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffiths, S.L.; Salmon, R.L.; Mason, B.W.; Elliott, C.; Thomas, D.R.; Davies, C. Using the internet for rapid investigation of an outbreak of diarrhoeal illness in mountain bikers. Epidemiol. Infect. 2010, 138, 1704–1711. [Google Scholar] [CrossRef] [PubMed]
- Kipps, C.; Sharma, S.; Pedoe, D.T. The incidence of exercise-associated hyponatraemia in the London marathon. Br. J. Sports Med. 2009, 45, 14–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chlíbková, D.; Knechtle, B.; Rosemann, T.; Tomášková, I.; Novotny, J.; Žákovská, A.; Uher, T. Rhabdomyolysis and exercise-associated hyponatremia in ultra-bikers and ultra-runners. J. Int. Soc. Sports Nutr. 2015, 12, 29. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, L.E.; Lee, E.C.; Casa, U.J.; Johnson, E.C.; Ganio, M.S.; McDermott, B.P.; Vingren, J.L.; Oh, H.M.; Williamson, K.H.; Oh, H.M.; et al. Exertional hyponatremia and serum sodium change during ultraendurance cycling. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 139–147. [Google Scholar] [CrossRef]
- Cutrufello, P.T.; Dixon, C.B.; Zavorsky, G.S. Hydration assessment among marathoners using urine specific gravity and bioelectrical impedance analysis. Res. Sports Med. 2016, 24, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Valentino, T.R.; Stuempfle, K.J.; Kern, M.; Hoffman, M.D. The influence of hydration state on thermoregulation during a 161-km ultramarathon. Res. Sports Med. 2016, 24, 197–206. [Google Scholar] [CrossRef]
- Knechtle, B.; Gnädinger, M.; Knechtle, P.; Imoberdorf, R.; Kohler, G.; Ballmer, P.; Rosemann, T.; Senn, O. Prevalence of exercise-associated hyponatremia in male ultraendurance athletes. Clin. J. Sport Med. 2011, 21, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Gomm, E.; Grimaldi, R.; Galloway, R.; Sharma, S.; Simpson, W.; Cottingham, R. Successful out-of-hospital therapy for heatstroke in three marathon runners with a novel core body cooling device: CAERvest ®. Scand. J. Med. Sci. Sports 2016, 26, 854–855. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.S.; Rodeia, S.C.; Silvestre, J.; Póvoa, P. Exertional heat stroke and acute liver failure: A late dysfunction. BMJ Case Rep. 2016, 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, W.O.; Dorman, J.C.; Bergeron, M.F. Recurrent heat stroke in a runner: Race simulation testing for return to activity. Med. Sci. Sports Exerc. 2016, 48, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.M.; Hoffman, M.D. Hiker fatality from severe hyponatremia in Grand Canyon National Park. Wilderness Environ. Med. 2015, 26, 371–374. [Google Scholar] [CrossRef]
- Severac, M.; Orban, J.-C.; Leplatois, T.; Ichai, C. A near-fatal case of exercise-associated hyponatremia. Am. J. Emerg. Med. 2014, 32, 813.e1–813.e2. [Google Scholar] [CrossRef]
- Hostler, D.; Franco, V.; Martin-Gill, C.; Roth, R.N. Recognition and treatment of exertional heat illness at a Marathon Race. Prehosp. Emerg. Care 2014, 18, 456–459. [Google Scholar] [CrossRef]
- Bhangu, A.; Parmar, R. Detection and management of hypothermia at a large outdoor endurance event in the United Kingdom. Wilderness Environ. Med. 2010, 21, 141–145. [Google Scholar] [CrossRef] [Green Version]
- Castro, R.R.T.; Mendes, F.S.; Nóbrega, A.C.L. Risk of hypothermia in a New Olympic Event: The 10-km marathon swim. Clinics 2009, 64, 351–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rae, D.E.; Knobel, G.J.; Mann, T.; Swart, J.; Tucker, R.; Noakes, T.D. Heatstroke during endurance exercise: Is there evidence for excessive endothermy? Med. Sci. Sports Exerc. 2008, 40, 1193–1204. [Google Scholar] [CrossRef] [PubMed]
- Hew-Butler, T.; Rosner, M.H.; Fowkes-Godek, S.; Dugas, J.P.; Hoffman, M.D.; Lewis, D.P.; Maughan, R.J.; Miller, K.C.; Montain, S.J.; Rehrer, N.J.; et al. Statement of the third international exercise-associated hyponatremia consensus development conference, Carlsbad, California, 2015. Clin. J. Sport Med. 2015, 25, 303–320. [Google Scholar] [CrossRef] [PubMed]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar] [PubMed] [Green Version]
- Domínguez, R.; Mata-Ordoñez, F.; Sánchez-Oliver, A.J. Nutrición Deportiva Aplicada: Guía para Optimizar el Rendimiento; ICB Editores: Málaga, España, 2017; ISBN 978-84-9021-488-6. [Google Scholar]
- Sierra Quintana, E.; Martínez Caballero, C.M.; Batista Pardo, S.A.; Abella Barraca, S.; de la Vieja Soriano, M. Nontraumatic medical emergencies in mountain rescues. Emergencias 2017, 29, 339–342. [Google Scholar]
- Edouard, P.; Depiesse, F.; Branco, P.; Alonso, J.-M. Analyses of Helsinki 2012 European Athletics Championships injury and illness surveillance to discuss elite athletes risk factors. Clin. J. Sport Med. 2014, 24, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Ordoñez, F.M.; Valenzuela, P.L.; Gimenez, J.; Tur, C.; Ferreria, D.; Domínguez, R.; Sánchez-Oliver, A.; Sanz, J.M.M. Carbohydrate availability and physical performance: Physiological overview and practical recommendations. Nutrients 2019, 11, 1084. [Google Scholar] [CrossRef] [Green Version]
- Chey, W.; Kurlander, J.; Eswaran, S. Irritable bowel syndrome. JAMA 2015, 313, 982. [Google Scholar] [CrossRef] [Green Version]
- Lis, D.; Stellingwerff, T.; Shing, C.M.; Ahuja, K.; Fell, J. Exploring the popularity, experiences, and beliefs surrounding gluten-free diets in Nonceliac athletes. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 37–45. [Google Scholar] [CrossRef]
- Casa, D.J.; DeMartini, J.K.; Bergeron, M.F.; Csillan, D.; Eichner, E.R.; Lopez, R.M.; Ferrara, M.S.; Miller, K.C.; O’Connor, F.; Sawka, M.N.; et al. National athletic trainers’ association position statement: Exertional heat illnesses. J. Athl. Train. 2015, 50, 986–1000. [Google Scholar] [CrossRef] [Green Version]
- Pryor, R.R.; Bennett, B.L.; O’Connor, F.G.; Young, J.M.; Asplund, C.A. Medical evaluation for exposure extremes: Heat. Wilderness Environ. Med. 2015, 26, 69–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asplund, C.A.; Creswell, L.L. Hypothesised mechanisms of swimming-related death: A systematic review. Br. J. Sports Med. 2016, 50, 1360–1366. [Google Scholar] [CrossRef] [PubMed]
- Nuckton, T.J.; Claman, D.M.; Goldreich, D.; Wendt, F.C.; Nuckton, J.G. Hypothermia and afterdrop following open water swimming: The Alcatraz/San Francisco swim study. Am. J. Emerg. Med. 2000, 18, 703–707. [Google Scholar] [CrossRef] [PubMed]
| Study | Objectives | Sample | Sporting Competition | Adverse Outcomes | Incidence | Causes | Conclusions |
|---|---|---|---|---|---|---|---|
| Parkkali et al. (2017) [24] | -To determine the origin and prevalence of GI problems in participants in triathlon y duathlon -To adopt preventative measures for future events. | 239 athletes -80 F -159 M | Triathlon and duathlon, The Netherlands (2015) | Acute GI illnesses | GI illnesses: 73 cases (30.5%) -Stomach pain: 52 cases (71%) -Nausea: 56 cases (77%) -Diarrhea: 43 cases (59%) -Vomiting: 28 cases (38%) | Consumption of energy drinks and ingestion of sips of water from the canal in which the swimming event took place. | -The rate of appearance of the symptoms in the 2 days after the event suggested a viral origin, which was confirmed by the detection of norovirus in feces samples. -The open-water swimming events were the most probable source of the infection. -No food or drink, except the energy drinks, was associated with the GI illnesses. |
| Meyer et al. (2017) [25] | -To evaluate the incidence of diarrhea in a hiking trail. -To determine the seriousness and causes of this GI problem. | 737 athletes -281 F -420 M -36 unspecified | John Muir Trail (JMT), long-distance hiking trail, USA (2014) | GI problems: diarrhea. | Diarrhea: 121 cases (16.4%) -Mild: 99 cases (82%) -Moderate: 16 cases (13%) -Severe: 6 cases (5%) | Fecal contamination of the natural sources of water ingested, together with poor handwashing on the trail. | -The incidence of diarrhea is relatively low compared with other long-distance trails in the USA. -By following standard hygiene recommendations and using filtration or treatment methods for the water, the prevalence of GI problems in this type of event could be reduced. |
| Magee et al. (2017) [26] | To evaluate the hydration and physical state of university athletes according to the sports and disciplines practiced. | 429 athletes Runners: -54 M Cyclists: -7 F -22 M | -Runners: 5 cycles of 2 km on uneven terrain. -Cyclists: cycles of 100 km with a rise in altitude of 1000 m. Ireland (2016) | DH | Total DH: 187 cases (43.6%) -Runners, post-training: 6 cases (12%) -Cyclists, post-training: 13 cases (45%) | Lack of knowledge about the liquid requirements and nutritional values of the athletes. | -Many athletes consume insufficient liquid during physical exercise. -The opportunities to drink water and other liquids during the events are too limited. -There are more drinks-breaks during team sports; even so, the participants do not consume enough water to avoid DH. |
| Brustia et al. (2016) [27] | -To obtain information about the risks involved in mountain sports, so that adequate information can be supplied. -To develop recommendations for health and safety teams. | 202 athletes | Endurance sports in the French Alps, at 2500 m altitude. (2013) | Injuries due to cold and HT. | Injuries due to cold: 13 cases (6.4%) Due to HT: 9 cases (4.4%) | Exposure to high altitudes for long periods of time, in addition to the use of thermal protection inferior to that used by climbers in winter. | -The medical risks and trauma cases produced at high altitude affected 1% of the participants. -Head injuries and traumas are the most frequent types at high altitude. -Altitude sickness and cold-related injuries are more frequent in summer, during climbing activities. |
| Chlíbková et al. (2016) [28] | To determine the state of hydration before and after a competition and the incidence of EAH in ultra-endurance athletes. | 113 athletes -25 F -88 M | Ultra-endurance in the Czech Republic. (2012–2013) -4 cycle races of 24 h in the mountains. -3 foot races: 2 of 24 h and 1 of 100 km | DH and EAH. | EAH: 13 cases (11.5%) DH: 30 cases (27%) | Loss of sodium in the sweat during the races. Over-ingestion of drinks and greater retention of liquids. | -Incidence of EAH greater than that reported previously in ultra-endurance athletes. -Hyper-hydration before the race did not protect the athletes. -The results obtained indicate that the concentration of sodium [Na+] in the blood is still the only viable way of determining EAH in endurance athletes. |
| Danz et al. (2016) [13] | To evaluate the rates of EAH in an Ironman competition. | 1089 athletes -157 F -932 M | Ironman championships held in Europe (2005–2013) | EAH. | EAH: 115 cases (10.6%) -Mild: 95 cases (8.7%) -Severe: 17 cases (1.6%) -Critical: 3 cases (0.3%) | Association between: -EAH and F -EAH and those that took longer to complete the events. | -EAH has a high incidence among Ironman competitors. -F competitors and those that took ≥9 h seem to be more susceptible to EAH. |
| Joslin et al. (2016) [29] | To determine the number of medical complications related to EHS and the number of competitors who, for this reason, did not complete the race. | 326 athletes | Ultra-marathons of various stages, in the Amazonian jungle, Brazil (2008–2013) | EHS. | Heat related problems: 29 cases (8.9%) | Incorrect acclimatization before the event and inappropriate rest between stages. | Obligatory rests during ultra-endurance competitions in tropical conditions are probably the best way to improve the safety of the athletes and their acclimatization to the heat. |
| Stuempfle et al. (2015) [30] | To examine the incidence, the seriousness, and the time of appearance of symptoms of GI problems in athletes who complete the event, and in those who do not. | 272 athletes -56 F -216 M | Ultra-marathon of 161 km, USA. (2013) | GI illnesses. | GI symptoms: 261 cases (96%) -Nausea: 157 cases (60.3%) -Vomiting: 92 cases (35.4%) -Stomach cramps: 83 cases (31.9%) -Intestinal cramps: 63 cases (24.1%) -Diarrhea: 58 cases (22.2%) -GI hemorrhages: 4 cases (1.5%) | Multifactorial origin, including an altered physiology, mechanical factors, and the intake of water and food before the competition. | -GI symptoms were experienced by most of the runners (96.0%). -The results obtained seem to confirm that GI symptoms are very common during ultra-marathons; in particular, nausea, a key problem that can determine whether or not a competitor can complete the event. |
| Cairns et al. (2015) [12] | -To examine the incidence of EAH during and after an ultra-marathon. -To evaluate the non-osmotic stimuli with distinct concentrations of arginine and vasopressin in runners suffering hyponatremia. | 15 athletes -3 F -12 M | Ultra-endurance, Great North Walk (GNW) 100s, Australia. (2013) | EAH. | EAH: 10 cases (66.7%) | High consumption of alcohol, rise in body weight during the event, low body weight, female sex, slow pace, lack of experience in these competitions. | -EAH incidence of 67% in endurance athletes, which highlights the need to improve the information and education, to minimize the risk of EAH. -The incidence of EAH was greater in F than in M. |
| Hoffman et al. (2013) [31] | -To analyze cases of EAH. -To define the relationship between [Na+] and changes in body eight. -To examine the interactions between the incidence of EAH, ambient temperature, and hydration state. | 887 athletes | WSER ultra-marathon, 161 km, USA. (2009–2012) | DH and EAH. | DH: 164 cases (18.5%) EAH: 101 cases (15.1%) | The ambient temperature and an inverse relationship between [Na+] and the percentage change in body weight. | -The incidence of EAH may be higher in ultra-marathons of 161 km, especially at higher temperatures—when the over-hydration is lower and DH is greater. -Although weight loss does not seem to have an adverse effect on performance, ultra-endurance athletes should not take excessive supplementary Na or drink too much liquid. |
| Rüst et al. (2012) [32] | To investigate the prevalence of EAH in masculine triathletes competing in the Triple Iron triathlon. | 45 M | “Triple Iron” Triathlon, Germany. (2007) | EAH. | EAH: 8 cases (17.8%) | Excessive intake of liquids, more inappropriate secretion of ADH and complications in the mobilization of Na+. | -The prevalence of EAH in this event is greater, based on existing reports on Ironman athletes. -In comparison with marathon runners, the athletes studied here, who compete for >24 h, seem to have a greater risk of developing EAH. |
| Mexia et al. (2013) [33] | -To evaluate risk factors associated with GI problems. -To determine the use of preventative measures. -To compare the findings with those of previous years regarding GI problems and evaluate risk and protective factors. | 11721 athletes | “Birkebeinerrittet” mountain bike race, Norway. (2010) | GI illnesses. | Diarrhea: 572 cases (4.9%) | Exposure to mud in the face or mouth during the competition. The absence of a mudguard increased the risk. | -Exposure to mud with fecal contamination is a risk factor. The environmental measures that could reduce this exposure include the elimination of grazing livestock from close to the track and the reduction in the size of muddy areas. -Improvement of preventative strategies. |
| Hoffman et al. (2012) [34] | -To determine the incidence of EAH, the associated biochemical parameters, and risk factors. -To check if there is an association between the [Na+] in the blood after the race and the changes in body mass of the participants. | 47 athletes | Ultramarathon WSER de 161 Km, EEUU. (2009) | EAH and associated nausea | EAH: 14 cases (30%) Nausea: 22 cases (46.8%) | It is associated with DH, since it suggests that the loss of sodium can be a factor in the development of EAH during events of long duration at high temperatures. | -EAH may be a common condition (incidence of 30%) among the finalists of an ultra-marathon. -It is not unusual for athletes with EAH to suffer DH. -The development of EAH was not related to age, sex or the time taken to complete the event, but the athletes with EAH had participated in fewer ultra- marathons. |
| Hoffman et al. (2011) [35] | To explore demographic characteristics and problems that affect the sport performance during an ultra-marathon. | 489 athletes | WSER ultra-marathon (161 km) and Vermont 100, North America. (2009) | Medicinal- nutritional problems that prevented 232 participants from completing the event | Nausea and/or vomiting: 92 cases (39.6%) DH: 11 cases (4.7%) Inadequately heat acclimatization: 65 cases (28.1%) | The ambient temperature, the amount of training, or experience in successfully completing this type of event. | -More than half of the ultra-marathon runners suffered a problem that prevented them from finishing the competition and led to an average of 21 days of recovery and preparation for later races. -Nausea and/or vomiting are an important problem that limits the performance of participants in ultra-marathons. -The athletes affected by nausea and/or vomiting took longer to complete the race than those not suffering these symptoms. |
| Bruso et al. (2010) [36] | To explore risk factors associated with development of EAH and rhabdomyolysis during an ultra-marathon. | 400 athletes | WSER ultra-marathon (161 km), USA. (2009) | EAH. | EAH: 5 cases (1.25%) | The causes of the appearance of EAH in this competition have not been established. | -One consistent characteristic was that all 5 individuals affected received a normal saline solution, intravenously, as part of their initial treatment. -Extreme precaution is recommended in the use of normal saline solution, given intravenously, especially if there are symptoms of cerebral encephalopathy, which could be worsened by this action. |
| Griffiths et al. (2010) [37] | To investigate the causes of an outbreak of diarrhea during a mountain bike competition. | 347 athletes -45 F -299 M -3 unspecified | Mountain bike competition, UK. (2008) | GI illnesses. | GI illnesses: 161 cases (46.5%) -Diarrhea: 151 cases (43.5%) -Abdominal pain: 131 cases (37.7%) -Nausea: 91 cases (26.2%) -Vomiting: 31 cases (8.9%) -Blood in feces: 15 cases (4.3%) | Outbreak caused by Campylobacter and spread by the accidental ingestion of mud, as well as by the use of water contaminated in the same way to fill the water bottles. | -The successful use of the Internet, to carry out a quick and efficient investigation into an outbreak of diarrhea and other symptoms associated with a mountain bike competition, was demonstrated. -The microbiological risks are an inherent part of this type of sport and the hygiene measures must be very strict to minimize the risk of infection. |
| Kipps et al. (2011) [38] | To determine the incidence of EAH in the runners who participate in a marathon. | 88 athletes | London marathon, United Kingdom. (2003) | EAH. | EAH: 11 cases (12.5%) | Some runners probably started the race in a state of hyperhydration. | -A significant proportion (12.5%) of the participants developed asymptomatic EAH after completing the race. Although they consumed more fluids, the ingestion of fluids was not related to the increase in body weight. -4 of the 11 runners with hyponatremia lost weight during the race, reinforcing the idea of an additional factor in the development of EAH. |
| Chlíbková et al. (2015) [39] | -Identification of athletes that develop EAH and rhabdomyolysis simultaneously. -To study hyponatremic and normonatremic athletes and try to find biochemical factors common to both EAH and rhabdomyolysis. | 145 athletes | 7 ultra-endurance races in the Czech Republic (2012–2013): -5 cycle races (24 h, mountain and trilogy) -2 foot races (24 h and 100 km) | EAH (113 completed the competition) | EAH: 13 cases (11.5%) | Secretion of arginine and vasopressin (antidiuretic hormone), and loss of liquid from muscle. | -Rhabdomyolysis induced by the exercise was more frequent in hyponatremic athletes than in normonatremic athletes. -The incidence of rhabdomyolysis tended to be greater among ultra-runners than among mountain cyclists. -The mechanism that could explain the relationship between rhabdomyolysis and EAH was not determined. |
| Study | Objectives | Sample | Sporting Competition | Adverse Outcomes | Incidence | Causes | Conclusions |
|---|---|---|---|---|---|---|---|
| Armstrong et al. (2017) [40] | -To evaluate the state of cyclists who began the competition with normal plasma [Na+], but finished it with 130 mmol/L. -Comparison of the values of these cyclists with those of a control group of 31 normonatremic cyclists. | 33 M | Open-air cycling competition, “Hotter’N Hell Hundred” (164 km), USA. (2016) | EAH. | EAH: 2 cases (6%) | Recommendations about the total intake of liquids and the change in the concentration of [Na+] determined the development of this condition. | -Each athlete must develop their own personalized plan for water intake, which includes measures during training, such as the calculation of the rate of sweating. -The precision of this method depends on the coincidence in the field simulation, regarding the environmental conditions and the intensity of the exercise. |
| Cutrufello et al. (2016) [41] | -To examine the relationship between the density of the urine, the bioelectrical impedance, and the body mass, before and after a marathon. -To check the hypothesis regarding the loss of body mass and of total body water that marathon runners experience. | 35 athletes -10 F -25 M | Marathon in the USA (2015) | Hydration state. | Hyperhydration: 22 cases (62.8%) | Lack of knowledge about hydration in this type of competition. | -The body mass values seem to reflect changes in hydration, but not when using the values of a single athlete. -The hydration regime before and after a marathon should be considered in future investigations, and the time of completion of the race should be compared with the bioelectrical impedance results. |
| Valentino et al. (2016) [42] | -To determine if DH (defined as body mass losses ≥3%) leads to critical changes in body temperature during an ultra-marathon of 161 km. -To check if the hydration state directly affects the body temperature. | 30 athletes -7 F -23 M | WSER ultra-marathon (161 km), USA (2014) | Hydration state (Only 20 athletes managed to complete the race) | DH: 10 cases (50%) GI illnesses: 5 cases (16.7%) | The athletes who lost a higher percentage of body mass completed the race more quickly. | -The losses of body mass (3–4%) were not related to the state of HT. -To avoid losses of body mass ≥2% during such events, it is not necessary to achieve a state of hyperhydration since it does not prevent HT. |
| Knechtle et al. (2011) [43] | -To investigate the prevalence of EAH in athletes in ultra-endurance sports modalities. -Comparison of the prevalence of EAH in these athletes with that in marathon runners and Ironman triathletes. | 200 athletes | Ultra-endurance races in Switzerland (2007–2009): -Swimming marathon in open water -2 cycling marathons -2 running marathons, 1 race of 100 km | EAH. | EAH: 12 cases (6%) | Consumption of alcohol and a high frequency of intake of liquid. | -The mean prevalence of EAH among the athletes studied was 6%. -The prevalence of EAH was higher than that found elsewhere for marathon, ultra-marathon, and Ironman competitors. |
| Study | Objectives | Sample | Sporting Competition | Adverse Outcomes | Incidence | Causes | Conclusions |
|---|---|---|---|---|---|---|---|
| Gomm et al. (2016) [44] | To demonstrate the effectiveness and safety of a portable medical device for chilling that acts on the endothermic surface. | 3 M | 2 marathons, UK. (2015) | EHS and other, related problems. | EHS: 3 cases (100%) Vomiting: 1 case (33.3%) | Environmental conditions during the competitions. | -The basis of the treatment is rapid attention and cooling; the fastest cooling rates were with water and ice baths. This reduced complications, being associated with a better long-term prognosis. |
| Six et al. (2016) [8] | To identify the source of infection and document the reach of an outbreak of acute gastroenteritis that occurred during an obstacle adventure race. | 729 athletes -332 F -397 M | Obstacle adventure race (13 km, 22 obstacles), France. (2015) | GI illnesses. | Acute gastroenteritis: 375 cases (50.3%) | Person to person transmission of a norovirus, the source of which was contaminated sewage sludge. | -A series of recommendations should be proposed to reduce the risk of infection among athletes in this type of event. -The runners in and organizers of these events should be aware of the possible risks involved in accidental ingestion of dirty water, avoiding areas contaminated by animal feces. |
| Carvalho et al. (2016) [45] | Identification, diagnosis, and evolution of an athlete who suffered from EHS together with other medical complications during a marathon. | 1 M | Marathon (the subject only completed 16 km), Portugal. (2016) | EHS and related complications. | EHS: 1 case (100%) Hypoglycemia: 1 case (100%) | Climatic changes and certain non-prescribed medicines could have been the causes. | -The athlete was cooled down in the hospital emergency department after only a few hours of the EHS, which may have contributed to the good outcome and recovery. -This works shows the importance of identifying risk factors, such as intake of medications that affect heat dissipation (antihistamines, anticholinergics, or calcium antagonists), sleep deprivation, and DH. |
| Smith et al. (2016) [14] | Analysis of the case of monozygotic twins that collapsed after EHS and during the same event, in relatively cold weather. | 2 M Monozygotic twins | 35-km race, UK. (2016) | EHS. | EHS: 2 cases (100%) | Causes unknown; the subjects denied sleep deprivation and felt hydrated before the start of the race. | -The development of EHS is multifactorial; however, the combination of the responsibilities of the pace of the race, the additional resistance of the backpack weight, and a genetic predisposition are likely to have played an important role. |
| Roberts et al. (2016) [46] | -Analysis of the case of an athlete who collapsed in two different marathons due to EHS and did not finish either races. -To study a simulation of the return to physical activity, to avoid repeating the circumstances of previous competitions. | 1 M | Two marathons, 6 weeks apart. The athlete dropped out of both after 20 km. USA. (2009) | EHS. | EHS: 1 case (100%) | Genetic causes of the EHS were discounted and an inadequate heat tolerance during these competitions was considered as the possible cause. | -The challenge of achieving an adequate hydro-electrolytic balance increases the risk of suffering from EHS during these competitions. -A quick response of spectators and colleagues, to ask for medical help, is crucial to reduce the risks associated with EHS. -To ensure a successful completion of these events, adequate heat tolerance should be guaranteed, as runners may be susceptible to EHS in cold conditions. |
| Myers et al. (2015) [47] | -To demonstrate the diagnostic challenges and the importance of proper management in cases of EAH. -To confirm that treatment with high volumes of an isotonic solution may delay recovery and may even lead to death. | 1 F | Hiking in the Grand Canyon National Park, approximately 10 km, USA (2008) | EAH and other, related problems. | EAH: 1 case (100%) -Vomiting: 1 case (100%) | Overhydration combined with fluid retention caused by the secretion of arginine-vasopressin. | -The first symptoms of EAH include nausea, vomiting, and headache, which progress rapidly to confusion, altered mental status, seizures, and death if not treated in time. -The recognition of EAH and its treatment with hypertonic saline solution is a safe and effective option. In addition, for sporting events that take place in areas with a desert climate, it would be beneficial to have sodium detection tests and to be able to administer hypertonic saline solutions |
| Severac et al. (2014) [48] | -To analyze the case of an athlete that, after completing an Ironman event, went to the emergency department with a headache, nausea, and confusion. -To study the causes that triggered the EAH. | 1 F | Ironman, France (2012) | EAH and other, related problems. | EAH: 1 case (100%) -Nausea: 1 case (100%) | -Excess fluid consumption compared to the losses of body fluids. | -EAH remains a complication with few diagnoses in endurance sports. In more severe cases, a correct and timely treatment allows complete neurological recovery. -Risk factors have been identified, such as: female sex, use of anti-inflammatories and diuretics, excessively cold or hot weather, the duration and intensity of the event, and excessive fluid intake |
| Hostler et al. (2014) [49] | To analyze the case of a half-marathon athlete that suffered EHS during a race in relatively mild conditions and compare it with cases of other runners who also suffered EHS in similar climatic conditions. | 1 M | Half-marathon, USA. (2012) | EHS. | EHS: 1 case (100%) | -The climatic conditions in an urban stretch of direct sunlight near the finish line. | -EHS requires active cooling therapy but this is rare during a half-marathon; however, EHS can occur even in relatively mild conditions. -The climatic conditions must be directly monitored at multiple points throughout the race, since it is possible for the temperature to be estimated in a single place that is not representative of the heat load on the participants |
| Bhangu et al. (2010) [50] | -To evaluate if body temperature contributed to the abandonment of an event by competitors. -To evaluate the agreement between the measurements made using oral and tympanic thermometers. | 4700 athletes | “Adventure raid”: an open-air event incorporating climbing, swimming, rafting. United Kingdom. (2009) | HT. | HT: 64 cases (1.4%) | -The climatic conditions and the swimming stages contributed to a decline in body temperature of the participants. | -The diagnosis of the doctors did not always coincide with the data obtained using the thermometers, regarding the existence of hypothermia or not in the runners. -The values of the tympanic and oral thermometers had little agreement. |
| Castro et al. (2009) [51] | To address the risks of HT and hypoglycemia during an open-water swimming competition, to alert doctors about the potential dangers of this type of competition | 12 athletes -5 F -7 M | Official open-water swimming competition (10 km), Brazil. (2008) | HT and hypoglycemia. | HT: 10 cases (83%) Hypoglycemia: 0 cases (all but one of the athletes received several doses of maltodextrin) | -Exposure to water for a prolonged period (at least two hours), contributing to the reduction of body temperature. | -HT is a common phenomenon, even in swimmers competing in relatively warm water. Therefore, it could be an important medical concern in such events. -The measurement of body temperature should be a key factor during competitions with these characteristics. |
| Rae et al. (2008) [52] | To determine why only 4 of the 35,627 athletes competing in cycling races were hospitalized by EHS, and whether the exercise alone could have raised their body temperature enough to cause EHS. | 4 M | 3 cyclists that participated in races, completing 80–109 km, died shortly after, South Africa. (2002) Another athlete, who completed 56 km in the “Two Oceans” marathon, South Africa. (2006) | EHS and other, related problems. | EHS: 4 cases (100%) -Vomiting: 2 cases (50%) -EAH: 1 case (25%) | -High rates of heat production in unfavorable environmental conditions caused a progressive build-up of body heat. | -The HT of the cases studied may have been the result of failure in the heat-loss mechanisms. -These cases could have been due to excessive endothermia, triggered by physical exertion. A correct diagnosis of excessive endothermia in cases of heat stroke in mild to moderate environmental conditions and the immediate initiation of cooling in all cases of EHS are crucial. |
| Incidence (%) | ||||
|---|---|---|---|---|
| DH | EAH | GI | HT | EHS |
| 392/1918 (20.4%) | 290/2829 (10.3%) | 1302/13,852 (9.4%) | 13/202 (6.4%) | n.r. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Sanz, J.M.; Fernández Nuñez, A.; Sospedra, I.; Martínez-Rodríguez, A.; Domínguez, R.; González-Jurado, J.A.; Sánchez-Oliver, A.J. Nutrition-Related Adverse Outcomes in Endurance Sports Competitions: A Review of Incidence and Practical Recommendations. Int. J. Environ. Res. Public Health 2020, 17, 4082. https://doi.org/10.3390/ijerph17114082
Martínez-Sanz JM, Fernández Nuñez A, Sospedra I, Martínez-Rodríguez A, Domínguez R, González-Jurado JA, Sánchez-Oliver AJ. Nutrition-Related Adverse Outcomes in Endurance Sports Competitions: A Review of Incidence and Practical Recommendations. International Journal of Environmental Research and Public Health. 2020; 17(11):4082. https://doi.org/10.3390/ijerph17114082
Chicago/Turabian StyleMartínez-Sanz, José Miguel, Ana Fernández Nuñez, Isabel Sospedra, Alejandro Martínez-Rodríguez, Raúl Domínguez, José Antonio González-Jurado, and Antonio J. Sánchez-Oliver. 2020. "Nutrition-Related Adverse Outcomes in Endurance Sports Competitions: A Review of Incidence and Practical Recommendations" International Journal of Environmental Research and Public Health 17, no. 11: 4082. https://doi.org/10.3390/ijerph17114082
APA StyleMartínez-Sanz, J. M., Fernández Nuñez, A., Sospedra, I., Martínez-Rodríguez, A., Domínguez, R., González-Jurado, J. A., & Sánchez-Oliver, A. J. (2020). Nutrition-Related Adverse Outcomes in Endurance Sports Competitions: A Review of Incidence and Practical Recommendations. International Journal of Environmental Research and Public Health, 17(11), 4082. https://doi.org/10.3390/ijerph17114082











