Objective Church Environment Audits and Attendee Perceptions of Healthy Eating and Physical Activity Supports within the Church Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Data Collection
2.2. Measures
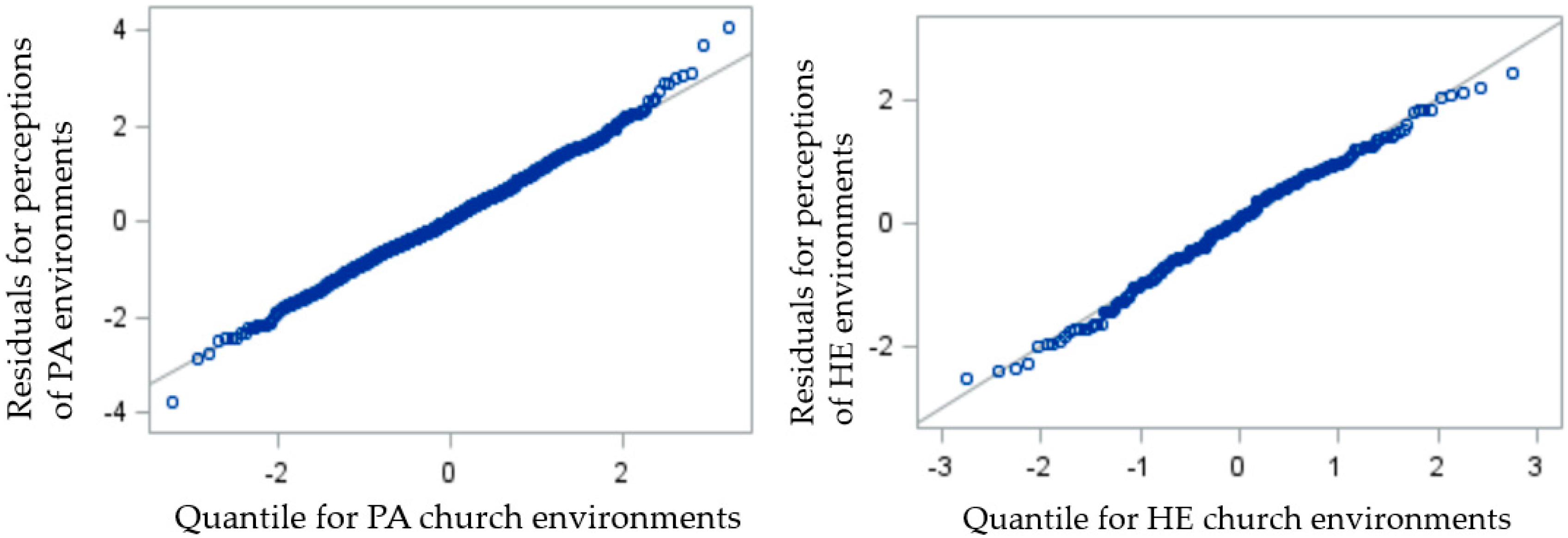
2.3. Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hill, J.O.; Wyatt, H.R.; Peters, J.C. Energy Balance and Obesity. Circulation 2012, 126, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Laredo-Aguilera, J.A.; Cobo-Cuenca, A.I.; Santacruz-Salas, E.; Martins, M.M.; Rodríguez-Borrego, M.A.; López-Soto, P.J.; Carmona-Torres, J.M. Levels of Physical Activity, Obesity and Related Factors in Young Adults Aged 18–30 during 2009–2017. Int. J. Environ. Res. Public Health 2019, 16, 4033. [Google Scholar] [CrossRef] [PubMed]
- Roger, V.; Go, A.S.; Lloyd-Jones, D.M.; Benjamin, E.J.; Berry, J.D.; Borden, W.B.; Bravata, D.M.; Dai, S.; Ford, E.S.; Fox, C.S.; et al. Heart Disease and Stroke Statistics—2012 Update: A Report from the American Heart Association. Circulation 2012, 125. [Google Scholar] [CrossRef]
- de Rezende, L.F.M.; de Sá, T.H.; Markozannes, G.; Rey-López, J.P.; Lee, I.-M.; Tsilidis, K.K.; Ioannidis, J.P.A.; Eluf-Neto, J. Physical activity and cancer: An umbrella Review of the Literature Including 22 Major Anatomical Sites and 770 000 Cancer Cases. Br. J. Sports Med. 2018, 52, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Bergmann, M.M.; Boeing, H.; Li, C.; Capewell, S. Healthy Lifestyle Behaviors and All-Cause Mortality among Adults in the United States. Prev. Med. 2012, 55, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Gamble, S.; Mawokomatanda, T.; Xu, F.; Chowdhury, P.P.; Pierannunzi, C.; Flegel, D.; Garvin, W.; Town, M. Surveillance for Certain Health Behaviors and Conditions among States and Selected Local Areas—Behavioral Risk Factor Surveillance System, United States, 2013 and 2014. MMWR Surveill. Summ. 2017, 66, 1–144. [Google Scholar] [CrossRef]
- Pew Research Center America’s Changing Religious Landscape. Available online: www.pewforum.org/files/2015/05/RLS-08-26-full-report.pdf (accessed on 16 April 2019).
- Bopp, M.; Peterson, J.A.; Webb, B.L. A Comprehensive Review of Faith-Based Physical Activity Interventions. Am. J. Lifestyle Med. 2012, 6, 460–478. [Google Scholar] [CrossRef]
- Wilcox, S.; Saunders, R.P.; Kaczynski, A.T.; Forthofer, M.; Sharpe, P.A.; Goodwin, C.; Condrasky, M.; Kennedy, V.L.; Jake-Schoffman, D.E.; Kinnard, D.; et al. Faith, Activity, and Nutrition Randomized Dissemination and Implementation Study: Countywide Adoption, Reach, and Effectiveness. Am. J. Prev. Med. 2018, 54, 776–785. [Google Scholar] [CrossRef]
- Wilcox, S.; Parrott, A.; Baruth, M.; Laken, M.; Condrasky, M.; Saunders, R.; Dowda, M.; Evans, R.; Addy, C.; Warren, T.Y.; et al. The Faith, Activity, and Nutrition Program. Am. J. Prev. Med. 2013, 44, 122–131. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An Ecological Approach to Creating Active Living Communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef]
- Kaczynski, A.T.; Robertson-Wilson, J.; Decloe, M. Interaction of perceived neighborhood walkability and self-efficacy on physical activity. J. Phys. Act. Health 2012, 9, 208–217. [Google Scholar] [CrossRef]
- Bandura, A. Social cognitive theory: An Agentic Perspective. Annu. Rev. Psychol. 2000, 52, 1–26. [Google Scholar] [CrossRef]
- Bai, H.; Wilhelm Stanis, S.A.; Kaczynski, A.T.; Besenyi, G.M. Perceptions of Neighborhood Park Quality: Associations with Physical Activity and Body Mass Index. Ann. Behav. Med. 2013, 45, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.; Atwood, J.R.; Yates, B. Key Elements for Church-Based Health Promotion Programs: Outcome-Based Literature Review. Public Health Nurs. 2002, 19, 401–411. [Google Scholar] [CrossRef]
- Williams, R.M.; Glanz, K.; Kegler, M.C.; Davis, E. A Study of Rural Church Health Promotion Environments: Leaders’ and Members’ Perspectives. J. Relig. Health 2012, 51, 148–160. [Google Scholar] [CrossRef]
- Baruth, M.; Wilcox, S.; Condrasky, M.D. Perceived Environmental Church Support Is Associated with Dietary Practices among African-American Adults. J. Am. Diet. Assoc. 2011, 111, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Arriola, K.R.J.; Hermstad, A.; Flemming, S.S.C.; Honeycutt, S.; Carvalho, M.L.; Cherry, S.T.; Davis, T.; Frazier, S.; Escoffery, C.; Kegler, M.C. Promoting Policy and Environmental Change in Faith-Based Organizations: Description and Findings From a Mini-Grants Program. Am. J. Health Promot. 2017, 31, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Arriola, K.R.J.; Hermstad, A.; Flemming, S.S.C.; Honeycutt, S.; Carvalho, M.L.; Cherry, S.T.; Davis, T.; Frazier, S.; Liang, L.; Escoffery, C.; et al. Promoting Policy and Environmental Change in Faith-Based Organizations: Outcome Evaluation of a Mini-Grants Program. Health Promot. Pract. 2016, 17, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.C.; Escoffery, C.; Alcantara, I.C.; Hinman, J.; Addison, A.; Glanz, K. Perceptions of Social and Environmental Support for Healthy Eating and Physical Activity in Rural Southern Churches. J. Relig. Health 2012, 51, 799–811. [Google Scholar] [CrossRef]
- U.S. Census Bureau. American FactFinder. Available online: https://factfinder.census.gov/faces/nav/jsf/pages/community_facts.xhtml (accessed on 13 January 2019).
- U.S. Census Bureau. Quick Facts. Available online: www.census.gov/quickfacts/ (accessed on 12 January 2019).
- Robert Wood Johnson Foundation. Building a Culture of Health, County by County. Available online: www.countyhealthrankings.org/ (accessed on 21 January 2019).
- Kaczynski, A.T.; Jake-Schoffman, D.E.; Peters, N.A.; Dunn, C.G.; Wilcox, S.; Forthofer, M. Development and Testing of the Church Environment Audit Tool. Am. J. Health Behav. 2018, 42, 17–26. [Google Scholar] [CrossRef]
- Bernhart, J.A.; La Valley, E.A.; Kaczynski, A.T.; Wilcox, S.; Jake-Schoffman, D.E.; Peters, N.; Dunn, C.G.; Hutto, B. Investigating Socioeconomic Disparities in the Potential Healthy Eating and Physical Activity Environments of Churches. J. Relig. Health 2020, 59, 1065–1079. [Google Scholar] [CrossRef] [PubMed]
- Cortina, J.M. What is Coefficient Alpha? An Examination of Theory and Applications. J. Appl. Psychol. 1993, 78, 98–104. [Google Scholar] [CrossRef]
- CDC Behavioral Risk Factor Surveillance System Survey Questionnaire. Available online: www.cdc.gov/brfss/questionnaires.htm (accessed on 28 June 2018).
- Wilcox, S.; Dowda, M.; Leviton, L.C.; Bartlett-Prescott, J.; Bazzarre, T.; Campbell-Voytal, K.; Carpenter, R.A.; Castro, C.M.; Dowdy, D.; Dunn, A.L.; et al. Active for Life. Am. J. Prev. Med. 2008, 35, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O. Dietary and Physical Activity Guidelines for Americans. Obes. Manag. 2008, 4, 317–318. [Google Scholar] [CrossRef]
- Allicock, M.; Johnson, L.-S.; Leone, L.; Carr, C.; Walsh, J.; Ni, A.; Resnicow, K.; Pignone, M.; Campbell, M. Promoting Fruit and Vegetable Consumption Among Members of Black Churches, Michigan and North Carolina, 2008–2010. Prev. Chronic Dis. 2013, 10, 120161. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: New York, NY, USA, 2013. [Google Scholar]
- Magee, L. R Squared Measures Based on Wald and Likelihood Ratio Joint Significance Tests. Am. Stat. 1990, 44, 250–253. [Google Scholar] [CrossRef]
- Lackey, K.J.; Kaczynski, A.T. Correspondence of Perceived vs. Objective Proximity to Parks and Their Relationship to Park-Based Physical Activity. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 53. [Google Scholar] [CrossRef]
- Barnes, T.L.; Bell, B.A.; Freedman, D.A.; Colabianchi, N.; Liese, A.D. Do People Really Know What Food Retailers Exist in Their Neighborhood? Examining GIS-Based and Perceived Presence of Retail Food Outlets in an Eight-County Region of South Carolina. Spat. Spatio-Temporal Epidemiol. 2015, 13, 31–40. [Google Scholar] [CrossRef]
- Resnick, B.; Jenkins, L.S. Testing the Reliability and Validity of the Self-Efficacy for Exercise Scale. Nurs. Res. 2000, 49, 154–159. [Google Scholar] [CrossRef]
- Stephens, J.D.; Althouse, A.; Tan, A.; Melnyk, B.M. The Role of Race and Gender in Nutrition Habits and Self-Efficacy: Results from the Young Adult Weight Loss Study. J. Obes. 2017, 2017, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wolkoff, P. Indoor Air Humidity, Air Quality, and Health—An overview. Int. J. Hyg. Environ. Health 2018, 221, 376–390. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.P. Indoor air quality and health. Atmos. Environ. 1999, 33, 4535–4564. [Google Scholar] [CrossRef]
- Ormandy, D.; Ezratty, V. Health and Thermal Comfort: From WHO Guidance to Housing Strategies. Energy Policy 2012, 49, 116–121. [Google Scholar] [CrossRef]
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and Non-Auditory Effects of Noise on Health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef]
- McColl, S.L.; Veitch, J.A. Full-Spectrum Fluorescent Lighting: A Review of Its Effects on Physiology and Health. Psychol. Med. 2001, 31, 949–964. [Google Scholar] [CrossRef]
- U.S. Department of Health & Human Services Facts & Statistics. Available online: https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html (accessed on 30 January 2019).
- Almeida, F.A.; Wall, S.S.; You, W.; Harden, S.M.; Hill, J.L.; Krippendorf, B.E.; Estabrooks, P.A. The Association between Worksite Physical Environment and Employee Nutrition, and Physical Activity Behavior and Weight Status. J. Occup. Environ. Med. 2014, 56, 779–784. [Google Scholar] [CrossRef]
- Jongeneel-Grimen, B.; Droomers, M.; van Oers, H.A.M.; Stronks, K.; Kunst, A.E. The Relationship between Physical Activity and the Living Environment: A Multi-Level Analyses Focusing on Changes over Time in Environmental Factors. Health Place 2014, 26, 149–160. [Google Scholar] [CrossRef]
- Ohri-Vachaspati, P.; Lloyd, K.; DeLia, D.; Tulloch, D.; Yedidia, M.J. A Closer Examination of the Relationship between Children’s Weight Status and the Food and Physical Activity Environment. Prev. Med. 2013, 57, 162–167. [Google Scholar] [CrossRef]
- Baruth, M.; Wilcox, S. Psychosocial Mediators of Physical Activity and Fruit and Vegetable Consumption in the Faith, Activity, and Nutrition Programme. Public Health Nutr. 2015, 18, 2242–2250. [Google Scholar] [CrossRef][Green Version]
- Baseman, J.G.; Revere, D.; Painter, I.; Toyoji, M.; Thiede, H.; Duchin, J. Public Health Communications and Alert Fatigue. BMC Health Serv. Res. 2013, 13, 295. [Google Scholar] [CrossRef]
| Church Characteristic | Mean (SD) | Range |
|---|---|---|
| Total physical activity opportunities | 6.44 (2.57) | 3.00–16.00 |
| Usable | 6.02 (2.67) | 2.00–16.00 |
| Good condition | 6.04 (2.64) | 2.00–16.00 |
| Indoor physical activity opportunities 1 | 4.04 (1.95) | 1.00–12.00 |
| Usable | 3.85 (2.01) | 1.00–12.00 |
| Good condition | 3.93 (1.98) | 1.00–12.00 |
| Outdoor physical activity opportunities 2 | 2.41 (1.32) | 0.00–8.00 |
| Usable | 2.17 (1.40) | 0.00–8.00 |
| Good condition | 2.11 (1.37) | 0.00–8.00 |
| Healthy eating opportunities 3 | 6.67 (1.18) | 2.00–9.00 |
| Usable | 6.35 (1.82) | 0.00–9.00 |
| Good condition | 6.39 (1.80) | 0.00–9.00 |
| Sample Characteristic | n | % |
|---|---|---|
| Total | 993 | 100 |
| Age | ||
| 18–34 years | 131 | 13.2 |
| 35–65 years | 610 | 61.4 |
| >65 years | 252 | 25.4 |
| Gender | ||
| Male | 299 | 30.1 |
| Female | 694 | 69.9 |
| Any college education | ||
| Yes | 547 | 55.1 |
| No | 446 | 44.9 |
| Weekly church attendance | ||
| Yes | 765 | 77.0 |
| No | 228 | 23.0 |
| Meets physical activity guidelines | ||
| Yes | 712 | 71.7 |
| No | 281 | 28.3 |
| Meets fruit/vegetable guidelines | ||
| Yes | 257 | 25.9 |
| No | 736 | 74.1 |
| Randomization | ||
| Delayed intervention | 379 | 38.2 |
| Early intervention | 614 | 61.8 |
| Duration of church attendance, years (Mean, SD) | 32.7 | 21.6 |
| Church physical activity environment score (Mean, SD) | 13.3 | 5.4 |
| Church healthy eating environment score (Mean, SD) | 14.4 | 2.3 |
| Perceptions of church physical activity environment (Mean, SD) 1 | 2.3 | 0.9 |
| Perceptions of church healthy eating environment (Mean, SD) 1 | 2.8 | 0.7 |
| Self-efficacy for physical activity (Mean, SD) 2 | 3.7 | 1.5 |
| Self-efficacy for healthy eating (Mean, SD) 2 | 4.8 | 1.4 |
| Outcome Variables | Bivariate Associations 1 t/r (p-Value) | B or OR (SE) | 95% CI for B/OR | R2 Adjusted (R2 Crude) 2 |
|---|---|---|---|---|
| Perceptions 3 | ||||
| Physical activity supports | 0.31 (p < 0.01) * | 0.03 (0.01) | 0.01, 0.05 * | 0.19 (0.01) 4 |
| Healthy eating supports | 0.22 (p < 0.01) * | 0.05 (0.02) | 0.02, 0.09 * | 0.22 (0.00) 4 |
| Self-efficacy 5 | ||||
| Physical activity | 0.07 (p = 0.02) * | 0.02 (0.02) | −0.02, 0.06 | 0.05 (0.00) |
| Healthy eating | 0.00 (p = 0.94) | −0.01 (0.02) | −0.05, 0.03 | 0.05 (0.00) |
| Meets guidelines 6 | ||||
| Physical activity 7 | 0.26 (p = 0.79) | 1.00 (0.01) | 0.97, 1.03 | 0.02 (0.00) |
| Healthy eating 8 | −0.72 (p = 0.47) | 1.02 (0.03) | 0.95, 1.09 | 0.03 (0.00) |
| Variables | B or Odds Ratio (SE) | 95% CI | R2 |
|---|---|---|---|
| Interaction Term Estimates—Perceptions of Church Environment Supports as Outcome 1,2 | |||
| Weekly Church Attendance × Physical Activity Opportunities | 0.00 (0.01) | (0.00, 0.01) | 0.19 3 |
| Weekly Church Attendance × Healthy Eating Opportunities | −0.04 (0.02) | (−0.08, −0.01) * | 0.23 3 |
| Interaction Term Estimates—Self-Efficacy for Health Behaviors as Outcome 1,4 | |||
| Weekly Church Attendance × Physical Activity Opportunities | −0.03 (0.02) | (−0.06, 0.02) | 0.06 |
| Weekly Church Attendance × Healthy Eating Opportunities | −0.04 (0.05) | (−0.14, 0.06) | 0.05 |
| Interaction Term Estimates—Health Behaviors as Outcome 1,5 | |||
| Weekly Church Attendance × Physical Activity Opportunities | 0.00 (0.02) | (−0.02, 0.01) | 0.02 |
| Weekly Church Attendance × Healthy Eating Opportunities | 0.03 (0.05) | (−0.07, 0.12) | 0.03 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wende, M.E.; Kaczynski, A.T.; Bernhart, J.A.; Dunn, C.G.; Wilcox, S. Objective Church Environment Audits and Attendee Perceptions of Healthy Eating and Physical Activity Supports within the Church Setting. Int. J. Environ. Res. Public Health 2020, 17, 3598. https://doi.org/10.3390/ijerph17103598
Wende ME, Kaczynski AT, Bernhart JA, Dunn CG, Wilcox S. Objective Church Environment Audits and Attendee Perceptions of Healthy Eating and Physical Activity Supports within the Church Setting. International Journal of Environmental Research and Public Health. 2020; 17(10):3598. https://doi.org/10.3390/ijerph17103598
Chicago/Turabian StyleWende, Marilyn E., Andrew T. Kaczynski, John A. Bernhart, Caroline G. Dunn, and Sara Wilcox. 2020. "Objective Church Environment Audits and Attendee Perceptions of Healthy Eating and Physical Activity Supports within the Church Setting" International Journal of Environmental Research and Public Health 17, no. 10: 3598. https://doi.org/10.3390/ijerph17103598
APA StyleWende, M. E., Kaczynski, A. T., Bernhart, J. A., Dunn, C. G., & Wilcox, S. (2020). Objective Church Environment Audits and Attendee Perceptions of Healthy Eating and Physical Activity Supports within the Church Setting. International Journal of Environmental Research and Public Health, 17(10), 3598. https://doi.org/10.3390/ijerph17103598






