Collaborative Action on Fetal Alcohol Spectrum Disorder Prevention: Principles for Enacting the Truth and Reconciliation Commission Call to Action #33
Abstract
1. Introduction
2. Materials and Methods
3. Results
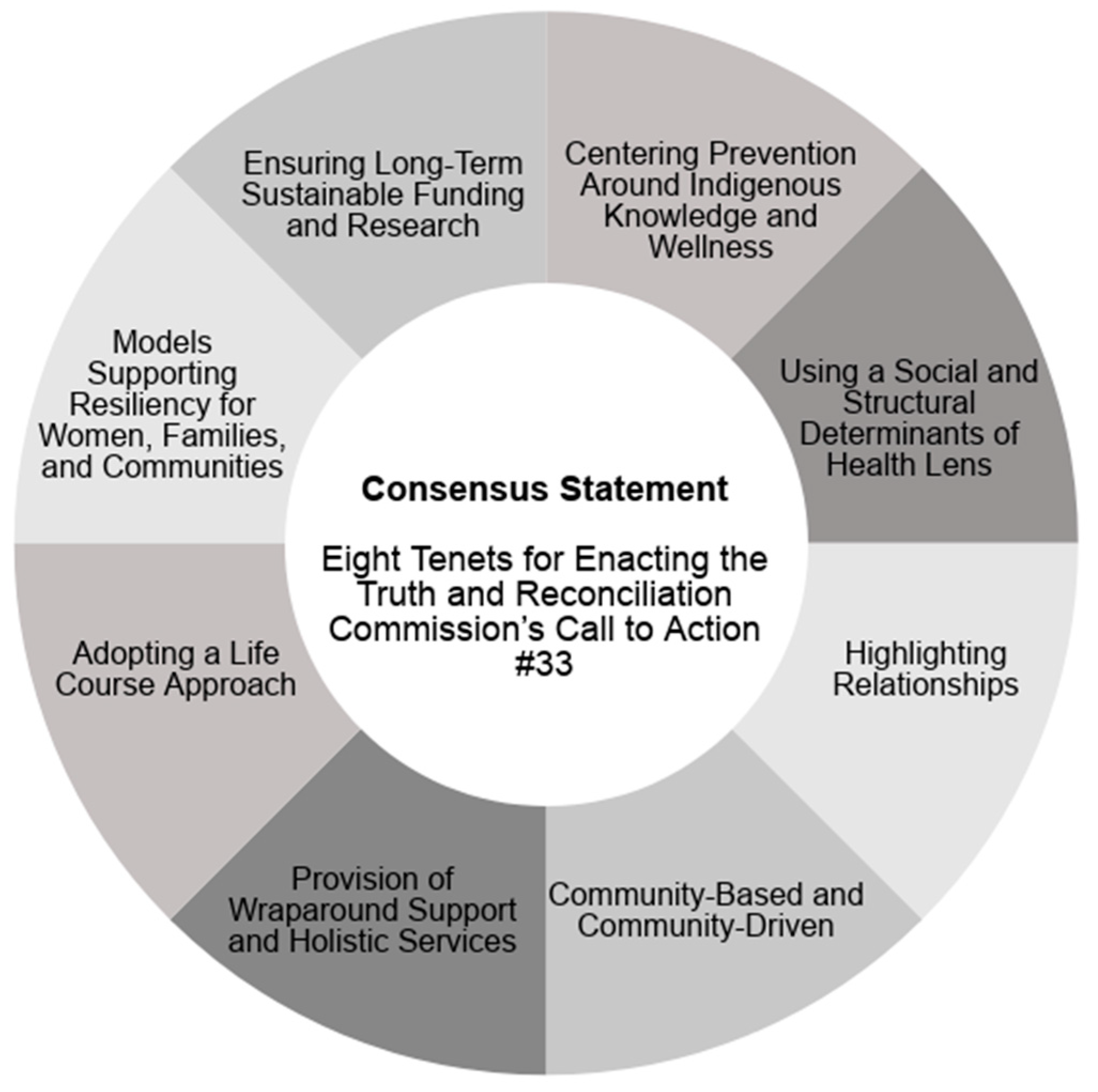
3.1. Consensus Statement: Eight Tenets for Enacting the Truth and Reconciliation Commission’s Call to Action #33
3.1.1. Tenet #1: Centering Prevention around Indigenous Knowledge and Wellness
3.1.2. Tenet #2: Using a Social and Structural Determinants of Health Lens
3.1.3. Tenet #3: Highlighting Relationships
3.1.4. Tenet #4: Community-Based and Community-Driven
3.1.5. Tenet #5: Provision of Wraparound Support and Holistic Services
3.1.6. Tenet #6: Adopting a Life Course Approach
3.1.7. Tenet #7: Models Supporting Resiliency for Women, Families, and Communities
3.1.8. Tenet #8: Ensuring Long-Term Sustainable Funding and Research
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- National Collaborating Centre for Aboriginal Health. Strong Women, Strong Nations: Aboriginal Maternal Health in British Columbia; National Collaborating Centre for Aboriginal Health: Prince George, BC, Canada, 2014. [Google Scholar]
- Skye, A.D. Aboriginal midwifery: A model for change. J. Aborig. Health 2010, 6, 28–37. [Google Scholar] [CrossRef]
- Tait, C.L. Fetal Alcohol Syndrome among Aboriginal People in Canada: Review and Analysis of the Intergenerational Links to Residential Schools; The Aboriginal Healing Foundation: Ottawa, ON, Canada, 2003. [Google Scholar]
- First Nations Child and Family Caring Society; Pauktuutit Inuit Women of Canada. FASD Training Study: Final Report; First Nations Child and Caring Society of Canada: Ottawa, ON, Canada, 2006. [Google Scholar]
- Johnston, S.; Boyle, J.S. Northern British Columbia Aboriginal mothers: Raising adolescents with Fetal Alcohol Spectrum Disorder. J. Transcult. Nurs. 2013, 24, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Poole, N.; Gelb, K.; Trainor, J. Preventing FASD through Providing Addictions Treatment and Related Supports for First Nations and Inuit Women in Canada—Summary; British Columbia Centre of Excellence for Women’s Health: Vancouver, BC, Canada, 2009. [Google Scholar]
- Aguiar, W.; Halseth, R. Aboriginal Peoples and Historic Trauma: The Processes of Intergenerational Transmission; National Collaborating Centre for Aboriginal Health Canada: Prince George, BC, Canada, 2015. [Google Scholar]
- Nagy, R. The truth and reconciliation commission of Canada: Genesis and design. Can. J. Law Soc. 2014, 29, 199–217. [Google Scholar] [CrossRef]
- Truth and Reconciliation Commission of Canada. Honouring the Truth, Reconciling for the Future: Summary of the Final Report of the Truth and Reconciliation Commission of Canada; TRC: Ottawa, ON, Canada, 2015. [Google Scholar]
- Evans-Campbell, T. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. J. Interpers. Violence 2008, 23, 316–338. [Google Scholar] [CrossRef]
- Gonzales, K.L.; Jacob, M.M.; Mercier, A.; Heater, H.; Nall Goes Behind, L.; Joseph, J.; Keurshner, S. An indigenous framework of the cycle of fetal alcohol spectrum disorder risk and prevention across the generations: Historical trauma, harm and healing. Ethn. Health 2018. [Google Scholar] [CrossRef] [PubMed]
- Muir, N.; Bohr, Y. Contemporary practice of traditional Aboriginal child rearing: A review. First Peoples Child Fam. Rev. 2014, 9, 66–79. [Google Scholar]
- Pacey, M. Fetal Alcohol Syndrome & Fetal Alcohol Spectrum Disorder among Aboriginal Canadians: Knowledge Gaps; National Collaborating Centre for Aboriginal Health: Prince George, BC, Canada, 2010. [Google Scholar]
- Popova, S.; Lange, S.; Probst, C.; Parunashvili, N.; Rehm, J. Prevalence of alcohol consumption during pregnancy and Fetal Alcohol Spectrum Disorders among the general and Aboriginal populations in Canada and the United States. Eur. J. Med Genet. 2017, 60, 32–48. [Google Scholar] [CrossRef]
- Bartlett, C.; Marshall, M.; Marshall, A. Integrative science: Enabling concepts within a journey guided by trees holding hands and two-eyed seeing. In Two-Eyed Seeing Knowledge Sharing Series; Institute for Integrative Science and Health, Ed.; Cape Breton University: Sydney, NSW, Australia, 2007. [Google Scholar]
- Greenwood, M.; Lindsay, N.; King, J.; Loewen, D. Ethical spaces and places: Indigenous cultural safety in British Columbia health care. Altern. Int. J. Indig. Peoples 2017, 13, 179–189. [Google Scholar] [CrossRef]
- Rowan, M.; Poole, N.; Shea, B.; Gone, J.P.; Myota, D.; Farag, M.; Hopkins, C.; Hall, L.; Mushquash, C.; Dell, C. Cultural interventions to treat addictions in Indigenous populations: Findings from a scoping study. Subst. Abuse Treat. Prev. Policy 2014, 9, 34. [Google Scholar] [CrossRef]
- Nathoo, T.; Poole, N. Indigenous Approaches to FASD Preven on: Indigenous Mothering; Centre of Excellence for Women’s Health: Vancouver, BC, Canada, 2017. [Google Scholar]
- Canada FASD Research Network; Thunderbird Partnership Foundation; Centre of Excellence for Women’s Health. Consensus Statement: Eight Tenets for Enacting the Truth and Reconciliation Commission’s Call to Action #33; Thunderbird Partnership Foundation: Bothwell, ON, Canada, 2017. [Google Scholar]
- Health Canada; Assembly of First Nations. First Nations Mental Wellness Continuum Framework; Health Canada: Ottawa, ON, Canada, 2015. [Google Scholar]
- First Nations Addictions Advisory Panel. Honouring Our Strengths: A Renewed Framework to Address Substance Use Issues among First Nations People in Canada; Minister of Health: Ottawa, ON, Canada, 2011.
- Restoule, B.M.; Hopkins, C.; Robinson, J.; Wiebe, P.K. First Nations mental wellness: Mobilizing change through partnership and collaboration. Can. J. Community Ment. Health 2015, 34, 89–109. [Google Scholar] [CrossRef]
- National Native Addictions Partnership Foundation Inc. Indigenous Wellness Framework and Outcomes; National Native Addictions Partnership Foundation Inc.: Bothwell, ON, Canada, 2015. [Google Scholar]
- Baydala, L.; Worrell, S.; Fletcher, F.; Letendre, L.; Letendre, S.; Ruttan, L. Making a place of respect: Lessons learned in carrying out consent protocol with First Nations Elders. Prog. Community Health Res. 2013, 7, 135–143. [Google Scholar] [CrossRef]
- Ruttan, L.; Letendre, S.; Letendre, L.; Fletcher, F.; Baydala, L.; Worrell, S. Wicubami: Honouring Alexis Nakota Sioux Ish?awimin (Elders) though kinship, language, spirit and research. Am. Indian Cult. Res. J. 2017, 41, 87–108. [Google Scholar]
- Shahram, S.Z. Understanding the life histories of pregnant-involved young Aboriginal women with substance use experiences in three Canadian cities. Qual. Health Res. 2017, 27, 249–259. [Google Scholar] [CrossRef]
- McKenzie, H.A.; Dell, C.A.; Fornssler, B. Understanding addictions among Indigenous people through social determinants of health frameworks and strengths-based approaches: A review of the research literature from 2013 to 2016. Curr. Addict. Rep. 2016, 3, 378–386. [Google Scholar] [CrossRef]
- Loppie, S.; Reading, C.; de Leeuw, S. Aboriginal Experiences with Racism and Its Impacts; National Collaborating Centre for Aboriginal Health: Prince George, BC, Canada, 2014. [Google Scholar]
- Grant, T.M.; Ernst, C.C.; Streissguth, A.; Stark, K. Preventing Alcohol and Drug Exposed Births in Washington State: Intervention Findings from Three Parent-Child Assistance Program Sites. Am. J. Drug Alcohol Abus. 2005, 31, 471–490. [Google Scholar] [CrossRef]
- Nathoo, T.; Poole, N.; Bryans, M.; Dechief, L.; Hardeman, S.; Marcellus, L.; Poag, E.; Taylor, M. Voices from the community: Developing effective community programs to support pregnant and early parenting women who use alcohol and other substances. First Peoples Child Fam. Rev. 2013, 8, 94–107. [Google Scholar]
- Motz, M.; Leslie, M.; Pepler, D.J.; Moore, T.E. Breaking the cycle: Measures of progress 1995–2005. J. Fas. Int. 2006, 4, e22. [Google Scholar]
- Sweeney, P.J.; Schwartz, R.M.; Mattis, N.G.; Vohr, B. The effect of integrating substance abuse treatment with prenatal care on birth outcome. J. Perinatol. 2000, 20, 219–224. [Google Scholar] [CrossRef]
- Innu Roundtable Secretariat. A Guide to the Innu Care Approach; Innu Roundtable Secretariat: Sheshatshiu, NL, Canada, 2017. [Google Scholar]
- Gerlach, A. “Circle of caring”: A First Nations worldview of child rearing. Can. J. Occup. Ther. 2008, 75, 18–25. [Google Scholar] [CrossRef]
- Advisory Panel for the Review of Federal Support for Fundamental Science. Investing in Canada’s Furture: Strengthening the Foundations of Canadian Research; Canada’s Fundamental Science Review: Ottawa, ON, Canada, 2017. [Google Scholar]
- Badry, D.; Felske, A.W. An examination of the social determinants of health as factors related to health, healing and prevention of foetal alcohol spectrum disorder in a northern context—The brightening our home fires project, Northwest Territories, Canada. Int. J. Circumpolar Health 2013, 72. [Google Scholar] [CrossRef]
- Best Start Resource Centre. The Sacred Journal from Preconception to Parenting; Best Start Resource Centre: Toronto, ON, Canada, 2012. [Google Scholar]
- Brady, C.; Johnson, F. Integrating the Life Course into MCH Service Delivery: From Theory to Practice. Matern. Child Health J. 2014, 18, 380–388. [Google Scholar] [CrossRef]
- Little Bear, L. Jagged Worldviews Colliding; UTP Distribution: Toronto, ON, Canada, 2000. [Google Scholar]
- Tait, C. Transformative change: Can a community-based ethical framework improve FASD prevention and interventions in Indigenous health? In Proceedings of Fetal Alcohol Canadian Expertise (FACE) Research Roundtable; Department of Psychiatry, University of Saskatchewan: Saskatoon, SK, Canada, 2012. [Google Scholar]
- Johnston, A. To Case Study or Not to Case Study: Our Experience with the Canadian Government’s Evaluation Practices and the Use of Case Studies as an Evaluation Methodology for First Nations Programs. Can. J. Program Eval. 2013, 28, 21–42. [Google Scholar]
- Johnston, A. The Waawiyeyaa Evaluation Tool; Johnston Research: Toronto, ON, Canada, 2010. [Google Scholar]
- Nota Bene Consulting Group; British Columbia Centre of Excellence for Women’s Health. Community/System Outcomes: Culturally Relevant Reporting and Accountability. In Evaluation of FASD Prevention and FASD Support Programs; British Columbia Centre of Excellence for Women’s Health: Vancouver, BC, Canada, 2013. [Google Scholar]
- Pei, J.; Tremblay, M.; Carlson, E.; Poth, C. PCAP in Alberta First Nation Communities: Evaluation Report; Policy Wise for Children & Families in collaboration with the University of Alberta: Edmonton, AB, Canada, 2017. [Google Scholar]
- Pei, J.; Carlson, E.; Tremblay, M.; Poth, C. Exploring the contributions and suitability of relational and community-centered fetal alcohol spectrum disorder (FASD) prevention work in First Nation communities. Birth Defects Res. 2019. [Google Scholar] [CrossRef]
- Tait, C. Ethical programming: Towards a community-centred approach to mental health and addiction programming in Aboriginal communities. Pimatisiwin 2008, 6, 29–60. [Google Scholar]
- Curtis, M.G. Preconception care: Clinical and policy implications of the preconception agenda. J. Clin. Outcomes Manag. 2010, 17, 167–172. [Google Scholar]
- Symons, M.; Pedruzzi, R.A.; Bruce, K.; Milne, E. A systematic review of prevention interventions to reduce prenatal alcohol exposure and fetal alcohol spectrum disorder in indigenous communities. BMC Public Health 2018, 18, 1227. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolfson, L.; Poole, N.; Morton Ninomiya, M.; Rutman, D.; Letendre, S.; Winterhoff, T.; Finney, C.; Carlson, E.; Prouty, M.; McFarlane, A.; et al. Collaborative Action on Fetal Alcohol Spectrum Disorder Prevention: Principles for Enacting the Truth and Reconciliation Commission Call to Action #33. Int. J. Environ. Res. Public Health 2019, 16, 1589. https://doi.org/10.3390/ijerph16091589
Wolfson L, Poole N, Morton Ninomiya M, Rutman D, Letendre S, Winterhoff T, Finney C, Carlson E, Prouty M, McFarlane A, et al. Collaborative Action on Fetal Alcohol Spectrum Disorder Prevention: Principles for Enacting the Truth and Reconciliation Commission Call to Action #33. International Journal of Environmental Research and Public Health. 2019; 16(9):1589. https://doi.org/10.3390/ijerph16091589
Chicago/Turabian StyleWolfson, Lindsay, Nancy Poole, Melody Morton Ninomiya, Deborah Rutman, Sherry Letendre, Toni Winterhoff, Catherine Finney, Elizabeth Carlson, Michelle Prouty, Audrey McFarlane, and et al. 2019. "Collaborative Action on Fetal Alcohol Spectrum Disorder Prevention: Principles for Enacting the Truth and Reconciliation Commission Call to Action #33" International Journal of Environmental Research and Public Health 16, no. 9: 1589. https://doi.org/10.3390/ijerph16091589
APA StyleWolfson, L., Poole, N., Morton Ninomiya, M., Rutman, D., Letendre, S., Winterhoff, T., Finney, C., Carlson, E., Prouty, M., McFarlane, A., Ruttan, L., Murphy, L., Stewart, C., Lawley, L., & Rowan, T. (2019). Collaborative Action on Fetal Alcohol Spectrum Disorder Prevention: Principles for Enacting the Truth and Reconciliation Commission Call to Action #33. International Journal of Environmental Research and Public Health, 16(9), 1589. https://doi.org/10.3390/ijerph16091589




