Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16–19
Abstract
1. Introduction
2. Material and Methods
2.1. Physical Activity
2.2. Screen Time
2.3. Sleep Quantity and Quality
2.4. Covariates
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Vyazovskiy, V.V. Sleep, recovery, and metaregulation: Explaining the benefits of sleep. Nat. Sci. Sleep 2015, 7, 171–184. [Google Scholar] [CrossRef]
- Kalak, N.; Lemola, S.; Brand, S.; Holsboer-Trachsler, E.; Grob, A. Sleep duration and subjective psychological well-being in adolescence: A longitudinal study in Switzerland and Norway. Neuropsychiatr. Dis. Treat. 2014, 10, 1199–1207. [Google Scholar] [CrossRef]
- Jaworska, N.; MacQueen, G. Adolescence as a unique developmental period. J. Psychiatry Neurosci. 2015, 40, 291–293. [Google Scholar]
- National Sleep Foundation. 2006 Teens and Sleep. Sleep in America Polls. Available online: www.sleepfoundation.org/article/sleep-america-polls/2006-teens-and-sleep (accessed on 27 January 2019).
- Roberts, R.E.; Duong, H.T. Depression and insomnia among adolescents: A prospective perspective. J. Affect. Disord. 2012, 148, 66–71. [Google Scholar] [CrossRef]
- Zapata Roblyer, M.I.; Grzywacz, J.G. Demographic and Parenting Correlates of Adolescent Sleep Functioning. J. Child Fam. Stud. 2015, 24, 3331–3340. [Google Scholar] [CrossRef] [PubMed]
- Matricciani, L.; Olds, T.; Petkov, J. In search of lost sleep: Secular trends in the sleep time of school-aged children and adolescents. Sleep Med. Rev. 2012, 16, 203–211. [Google Scholar] [CrossRef]
- Snell, E.K.; Adam, E.K.; Duncan, G.J. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007, 78, 309–323. [Google Scholar] [CrossRef]
- Baum, K.T.; Desai, A.; Field, J.; Miller, L.E.; Rausch, J.; Beebe, D.W. Sleep restriction worsens mood and emotion regulation in adolescents. J. Child Psychol. Psychiatry 2014, 55, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Kronholm, E.; Puusniekka, R.; Jokela, J.; Villberg, J.; Urrila, A.S.; Paunio, T.; Välimaa, R.; Tynjälä, J. Trends in self-reported sleep problems, tiredness, and related school performance among Finnish adolescents from 1984 to 2011. J. Sleep Res. 2015, 24, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, M.; Borowik, A.; Michallet, A.S.; Perrin, C.; Monneret, D.; Faure, P.; Levy, P.; Pépin, J.L.; Wuyam, B.; Flore, P. Sleep quality, sleep duration and physical activity in obese adolescents: Effects of exercise training. Pediatr. Obes. 2016, 11, 26–32. [Google Scholar] [CrossRef]
- Olds, T.S.; Maher, C.A.; Matricciani, L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep 2011, 34, 1299–1307. [Google Scholar] [CrossRef]
- Lang, C.; Kalak, N.; Brand, S.; Holsboer-Trachsler, E.; Puhse, U.; Gerber, M. The relationship between physical activity and sleep from mid adolescence to early adulthood. A systematic review of methodological approaches and meta-analysis. Sleep Med. Rev. 2016, 28, 28–41. [Google Scholar] [CrossRef]
- Foti, K.E.; Eaton, D.K.; Lowry, R.; McKnight-Ely, L.R. Sufficient sleep, physical activity, and sedentary behaviors. Am. J. Prev. Med. 2011, 41, 596–602. [Google Scholar] [CrossRef]
- Stone, M.R.; Stevens, D.; Faulkner, G.E. Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Prev. Med. 2013, 56, 112–117. [Google Scholar] [CrossRef]
- Brand, S.; Gerber, M.; Beck, J.; Hatzinger, M.; Pühse, U.; Holsboer-Trachsler, E. High exercise levels are related to favorable sleep patterns and psychological functioning in adolescents: A comparison of athletes and controls. J. Adolesc. Health 2010, 46, 133–141. [Google Scholar] [CrossRef]
- Holmberg, L.I.; Hellberg, D. Behavioral and other characteristics of relevance for health in adolescents with self-perceived sleeping problems. Int. J. Adolesc. Med. Health 2008, 20, 353–365. [Google Scholar] [CrossRef]
- Ortega, F.B.; Ruiz, J.R.; Labayen, I.; Kwak, L.; Harro, J.; Oja, L.; Veidebaum, T.; Sjöström, M. Sleep duration and activity levels in Estonian and Swedish children and adolescents. Eur. J. Appl. Physiol. 2011, 111, 2615–2623. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Levy, S.S. Assessment of health-enhancing physical activity. Methodological issues. In Health Enhancing Physical Activity; Oja, P., Borms, J., Eds.; Meyer & Meyer Sport: Oxford, UK, 2004; pp. 239–270. [Google Scholar]
- Carter, B.; Rees, P.; Hale, L.; Bhattacharjee, D.; Paradkar, M.S. Association Between Portable Screen-Based Media Device Access or Use and Sleep Outcomes: A Systematic Review and Meta-analysis. JAMA Pediatr. 2016, 170, 1202–1208. [Google Scholar] [CrossRef]
- Anderson, M.; Jiang, J. Teens, Social Media & Technology 2018. Pew Research Center. May 2018. Available online: https://www.pewinternet.org/2018/05/31/teens-social-media-technology-2018/ (accessed on 22 April 2019).
- Johansson, A.E.; Petrisko, M.A.; Chasens, E.R. Adolescent sleep and the impact of technology use before sleep on daytime function. J. Pediatr. Nurs. 2016, 31, 498–504. [Google Scholar] [CrossRef]
- Chen, M.-Y.; Wang, E.K.; Jeng, Y.-J. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health 2006, 6, 59. [Google Scholar]
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Jakobsen, R.; Lundervold, A.J.; Sivertsen, B. Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open 2015, 5, e006748. [Google Scholar] [CrossRef]
- Punamaki, R.L.; Wallenius, M.; Nygard, C.H.; Saarni, L.; Rimpela, A. Use of information and communication technology (ICT) and perceived health in adolescence: The role of sleeping habits and waking-time tiredness. J. Adolesc. 2007, 30, 569–585. [Google Scholar] [CrossRef]
- Yen, C.F.; Ko, C.H.; Yen, J.Y.; Cheng, C.P. The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. Sleep 2008, 31, 1515–1525. [Google Scholar] [CrossRef]
- Adam, E.K.; Snell, E.K.; Pendry, P. Sleep timing and quantity in ecological and family context: A nationally representative time-diary study. J. Fam. Psychol. 2007, 21, 4–19. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: https://wwwn.cdc.gov/nchs/nhanes (accessed on 12 July 2017).
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- Metcalf, B.S.; Curnow, J.S.; Evans, C.; Voss, L.D.; Wilkin, T.J. Technical reliability of the CSA activity monitor: The Early Bird study. Med. Sci. Sports Exerc. 2002, 34, 1533–1537. [Google Scholar] [CrossRef]
- Ekelund, U.; Sjostrom, M.; Yngve, A.; Poortvliet, E.; Nilsson, A.; Froberg, K.; Wedderkopp, N.; Westerterp, K. Physical activity assessed by activity monitor and doubly labeled water in children. Med. Sci. Sports Exerc. 2001, 33, 275–281. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Cho, M.H. Preliminary reliability of the five-item physical activity questionnaire. J. Phys. Ther. Sci. 2016, 28, 3393–3397. [Google Scholar] [CrossRef]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report; U.S. Department of Health and Human Services: Washington, DC, USA, 2008. Available online: http://www.health.gov/paguidelines (accessed on 9 February 2018).
- Council on Communications and Media. Children, adolescents, and the media. Pediatrics 2013, 132, 958–961. [Google Scholar] [CrossRef]
- Bansil, P.; Kuklina, E.V.; Merritt, R.K.; Yoon, P.W. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: Results from the National Health and Nutrition Examination Survey, 2005 to 2008. J. Clin. Hypertens. 2011, 13, 739–743. [Google Scholar] [CrossRef]
- Foerster, M.; Henneke, A.; Chetty-Mhlanga, S.; Röösli, M. Impact of Adolescents’ Screen Time and Nocturnal Mobile Phone-Related Awakenings on Sleep and General Health Symptoms: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 518. [Google Scholar] [CrossRef]
- Finger, J.D.; Mensink, G.B.; Banzer, W.; Lampert, T.; Tylleskär, T. Physical activity, aerobic fitness and parental socio-economic position among adolescents: The German Health Interview and Examination Survey for Children and Adolescents 2003-2006 (KiGGS). Int. J. Behav. Nutr. Phys. Act. 2014, 11, 43. [Google Scholar] [CrossRef]
- U.S. Census Bureau, Population Division, Fertility & Family Statistics Branch. Current Population Survey: Definitions and Explanations. 2004. Available online: http://www.census.gov/population/www/cps/cpsdef.html (accessed on 15 December 2017).
- CDC National Center for Health Statistics. Specifying Weighting Parameters. 2013. Available online: https://www.cdc.gov/nchs/tutorials/nhanes/surveydesign/weighting/intro.htm (accessed on 11 August 2017).
- Tynjälä, J.; Kannas, L.; Levälahti, E.; Valimaa, R. Perceived sleep quality and its precursors in adolescents. Health Promot. Int. 1999, 14, 155–166. [Google Scholar] [CrossRef][Green Version]
- Adams, S.K.; Williford, D.N.; Vaccaro, A.; Kisler, T.S.; Francis, A.; Newman, B. The young and the restless: Socializing trumps sleep, fear of missing out, and technological distractions in first-year college students. Int. J. Adolesc. Youth 2017, 22, 337–348. [Google Scholar] [CrossRef]
- Adams, S.K.; Daly, J.F.; Williford, D.N. Article Commentary: Adolescent Sleep and Cellular Phone Use: Recent Trends and Implications for Research. Health Serv. Insights 2013, 6, 99–103. [Google Scholar] [CrossRef]
- Van der Lely, S.; Frey, S.; Garbazza, C.; Wirz-Justice, A.; Jenni, O.G.; Steiner, R.; Wolf, S.; Cajochen, C.; Bromundt, V.; Schmidt, C. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J. Adolesc. Health 2015, 56, 113–119. [Google Scholar] [CrossRef]
- Falbe, J.; Davison, K.K.; Franckle, R.L.; Ganter, C.; Gortmaker, S.L.; Smith, L.; Land, T.; Taveras, E.M. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015, 135, 368–375. [Google Scholar] [CrossRef]
- King, D.L.; Gradisar, M.; Drummond, A.; Lovato, N.; Wessel, J.; Micic, G.; Douglas, P.; Delfabbro, P. The impact of prolonged violent video-gaming on adolescent sleep: An experimental study. J. Sleep Res. 2013, 22, 137–143. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between Sleep and Exercise: A Systematic Review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar]
- Suppiah, H.T.; Low, C.Y.; Chia, M. Effects of sport specific training intensity on sleep patterns and psychomotor performance in adolescent athletes. Pediatr. Exerc. Sci. 2016, 28, 588–595. [Google Scholar] [CrossRef]
- Pesonen, A.K.; Sjöstén, N.M.; Matthews, K.A.; Heinonen, K.; Martikainen, S.; Kajantie, E.; Tammelin, T.; Eriksson, J.G.; Strandberg, T.; Räikkönen, K. Temporal associations between daytime physical activity and sleep in children. PLoS ONE 2011, 6, e22958. [Google Scholar] [CrossRef]
- Maher, J.P.; Ra, C.; OʼConnor, S.G.; Belcher, B.R.; Leventhal, A.; Margolin, G.; Dunton, G.F. Associations Between Maternal Mental Health and Well-being and Physical Activity and Sedentary Behavior in Children. J. Dev. Behav. Pediatr. 2017, 38, 385–394. [Google Scholar] [CrossRef]
- Hajian Tilaki, K. Methodological issues of confounding in analytical epidemiologic studies. Caspian J. Intern. Med. 2012, 3, 488–495. [Google Scholar]
| Variables | Total | Male | Female | p-Value |
|---|---|---|---|---|
| N = 542 | n = 277 (49.3%) | n = 265 (50.7%) | ||
| Age (yrs) | 17.4 ± 0.1 | 17.5 ± 0.1 | 17.3 ± 0.1 | 0.111 |
| Race/ethnicity | ||||
| Non-Hispanic White (n%) | 123 (58.7) | 61 (59.6) | 62 (57.9) | 0.594 |
| Non-Hispanic black (n%) | 202 (17.4) | 107 (18.4) | 95 (16.5) | |
| Mexican American (n%) | 174 (11.6) | 88 (12.2) | 86 (11.0) | |
| Others (n%) | 43 (12.3) | 21 (9.8) | 22 (14.6) | |
| Parent education | ||||
| High school or less (n%) | 280 (44.1) | 149 (49.0) | 131 (39.2) | 0.194 |
| College or above (n%) | 235 (55.9) | 115 (51.0) | 120 (60.8) | |
| PIR | ||||
| PIR below poverty <1 (n%) | 156 (17.5) | 82 (20.6) | 74 (14.4) | 0.186 |
| PIR at or above poverty ≥1 (n%) | 365 (82.5) | 184 (79.4) | 181 (85.6) | |
| Body Mass Index (kg/m2) | 24.2 ± 0.4 | 24.5 ± 0.5 | 23.9 ± 0.5 | 0.318 |
| Underweight & (n%) | 14 (2.8) | 7 (2.8) | 7 (2.8) | 0.645 |
| Normal or Healthy Weight (n%) | 338 (65.5) | 174 (62.2) | 164 (68.8) | |
| Overweight (n%) | 86 (15.6) | 43 (16.3) | 43 (14.8) | |
| Obese (n%) | 103 (16.1) | 52 (18.8) | 51 (13.6) | |
| Sleep quantity (h) | 7.3 ± 0.1 | 7.3 ± 0.1 | 7.3 ± 0.2 | 0.738 |
| Sufficient sleep @ (n%) | 264 (48.7) | 133 (48.3) | 131 (49.2) | 0.9 |
| Poor sleep quality (n%) | 238 (43.8) | 119 (44.3) | 119 (43.4) | 0.886 |
| Poor SQI | ||||
| SQI = 0 (n%) | 304 (56.2) | 158 (55.7) | 146 (56.6) | 0.286 |
| SQI = 1 (n%) | 178 (32.7) | 98 (35.5) | 80 (30.0) | |
| SQI = 2+ (n%) | 59 (11.1) | 21 (8.8) | 38 (13.4) | |
| Total physical activity (min/day) | 24.7 ± 1.6 | 32.5 ± 2.5 | 17.1 ± 1.9 | <0.001* |
| Meet PA recommendation # (n%) | 187 (32.6) | 127 (44.7) | 60 (20.7) | <0.001* |
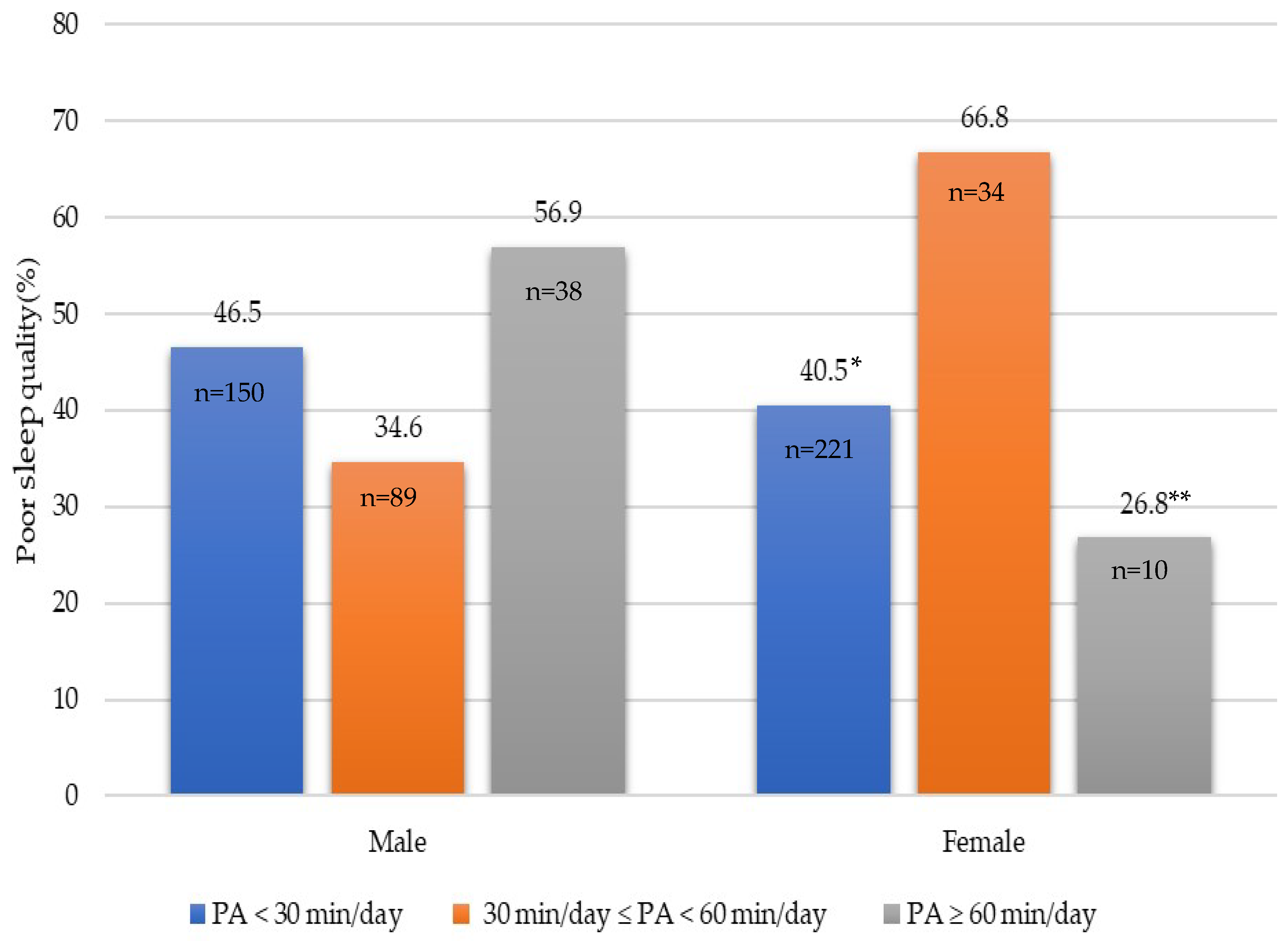
| Less active <30 min/day (n%) | 371 (70.7) | 150 (56.9) | 221 (84.2) | <0.001* |
| Active ≥30 and <60 min/day (n%) | 123 (21.4) | 89 (30.2) | 34 (12.8) | 0.003* |
| Very active ≥ 60 min/day (n%) | 48 (7.9) | 38 (13.0) | 10 (2.9) | <0.001* |
| Screen time (h/day) | 4.6 ± 0.2 | 5.0 ± 0.2 | 4.1 ± 0.3 | 0.017* |
| Meet screen time recommendation $ (n%) | 131 (32.3) | 54 (28.0) | 77 (36.5) | 0.097 |
| Meet both PA and screen time recommendation (n%) | 34 (8.6) | 18 (9.2) | 16 (8.1) | 0.725 |
| Total | Sufficient Sleep @ | Classified as Poor Sleep Quality | Sleep Quality Index (2+ Sleep-Related Problems) | |||
|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Meet PA recommendation # | 0.50 (0.26, 0.94) | 0.033 * | 0.89 (0.44, 1.80) | 0.727 | 1.10 (0.40, 3.04) | 0.848 |
| P values for meeting PA recommendation * sex | 0.472 | 0.459 | 0.474 | |||
| Meet screen time recommendation $ | 0.75 (0.45, 1.26) | 0.256 | 0.45 (0.22, 0.91) | 0.028 * | 0.60 (0.18, 2.05) | 0.393 |
| P values for meeting screen time recommendation * sex | 0.027* | 0.793 | 0.757 | |||
| Meet both PA and screen time recommendation | 0.64 (0.22, 1.86) | 0.387 | 0.57 (0.25, 1.30) | 0.163 | 0.42 (0.06, 3.11) | 0.373 |
| p values for meeting both * sex | 0.836 | 0.043* | 0.192 | |||
| Males | ||||||
| Meet PA recommendation # | 0.90 (0.42, 1.93) | 0.776 | 0.73 (0.26, 2.07) | 0.529 | 0.81 (0.16, 4.09) | 0.784 |
| Meet Screen time recommendation $ | 1.03 (0.54, 1.95) | 0.933 | 0.44 (0.19, 1.00) | 0.046 * | 0.81 (0.12, 5.26) | 0.812 |
| Meet both PA and screen time recommendation | 0.76 (0.23, 2.52) | 0.630 | 0.27 (0.07, 0.99) | 0.048 * | 1.15 (0.10, 13.32) | 0.903 |
| Females | ||||||
| Meet PA recommendation # | 0.25 (0.08, 0.77) | 0.019 * | 1.19 (0.48, 2.96) | 0.692 | 1.72 (0.55, 5.37) | 0.329 |
| Meet screen time recommendation $ | 0.48 (0.24, 0.96) | 0.038 * | 0.44 (0.21, 0.94) | 0.036 * | 0.53 (0.11, 2.61) | 0.412 |
| Meet both PA and screen time recommendation | 0.46 (0.08, 2.66) | 0.357 | 1.15 (0.38, 3.49) | 0.791 | 0.10 (0.01, 1.33) | 0.078 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, F.; Adams, S.K.; Cohen, S.A.; Earp, J.E.; Greaney, M.L. Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16–19. Int. J. Environ. Res. Public Health 2019, 16, 1524. https://doi.org/10.3390/ijerph16091524
Xu F, Adams SK, Cohen SA, Earp JE, Greaney ML. Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16–19. International Journal of Environmental Research and Public Health. 2019; 16(9):1524. https://doi.org/10.3390/ijerph16091524
Chicago/Turabian StyleXu, Furong, Sue K. Adams, Steven A. Cohen, Jacob E. Earp, and Mary L. Greaney. 2019. "Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16–19" International Journal of Environmental Research and Public Health 16, no. 9: 1524. https://doi.org/10.3390/ijerph16091524
APA StyleXu, F., Adams, S. K., Cohen, S. A., Earp, J. E., & Greaney, M. L. (2019). Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16–19. International Journal of Environmental Research and Public Health, 16(9), 1524. https://doi.org/10.3390/ijerph16091524







