Spatiotemporal Distribution of Hand, Foot, and Mouth Disease in Guangdong Province, China and Potential Predictors, 2009–2012
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Surveillance Data of HFMD
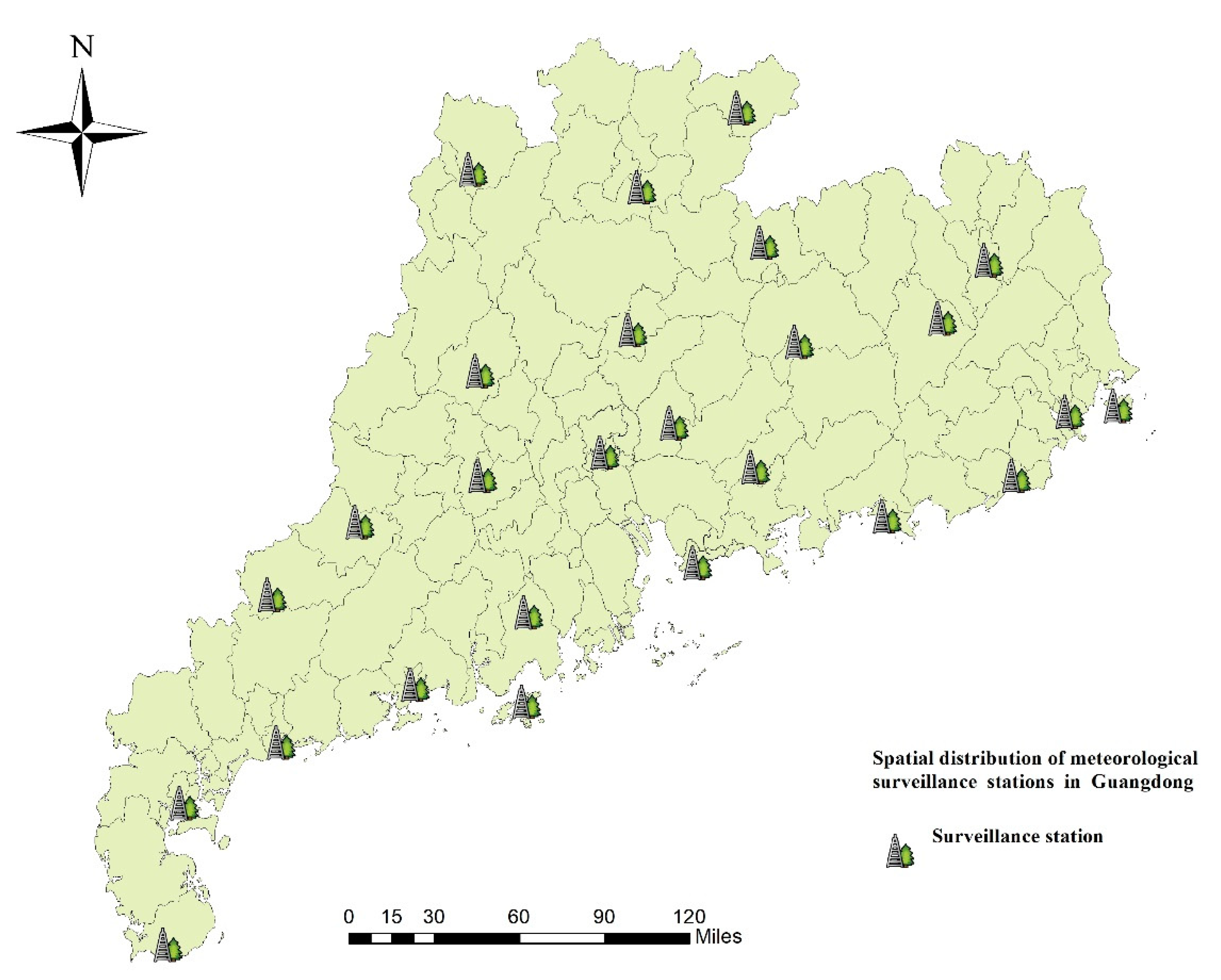
2.3. Potential Predictors Data
2.4. Statistical Methods
2.4.1. Bayesian Spatiotemporal Model
2.4.2. Geographical Detectors
3. Results
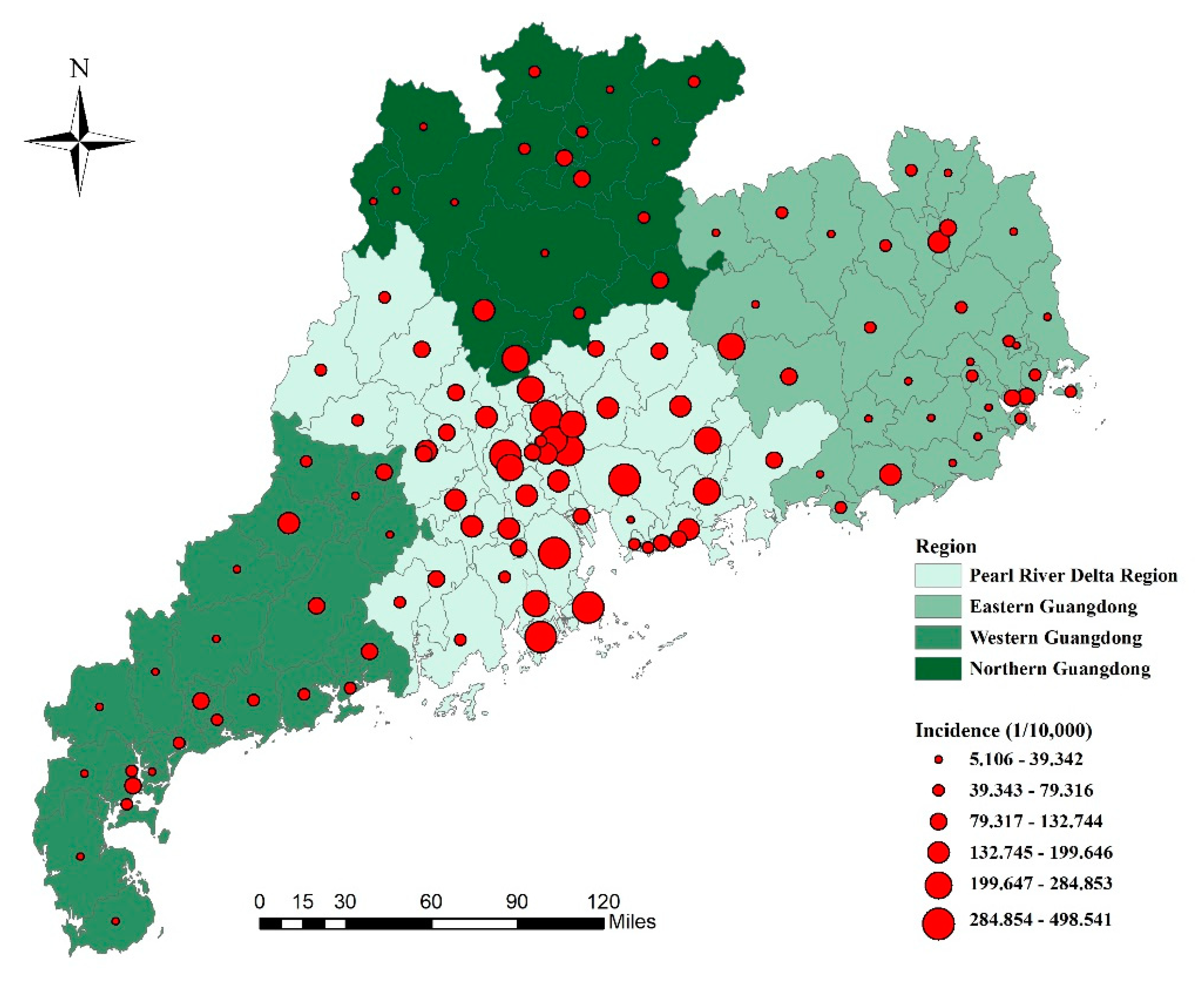
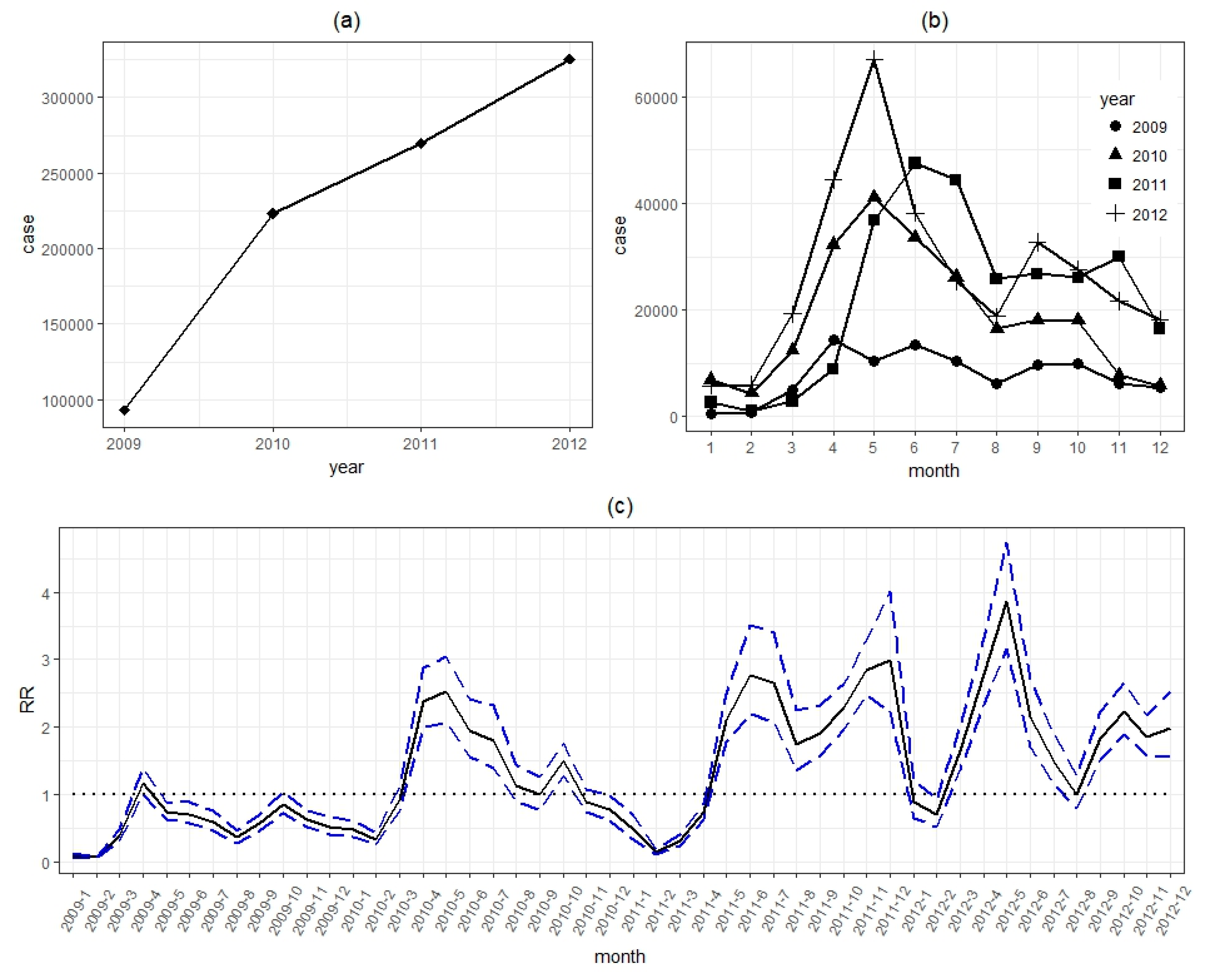
3.1. Descriptive Statistics
3.2. Model Selection
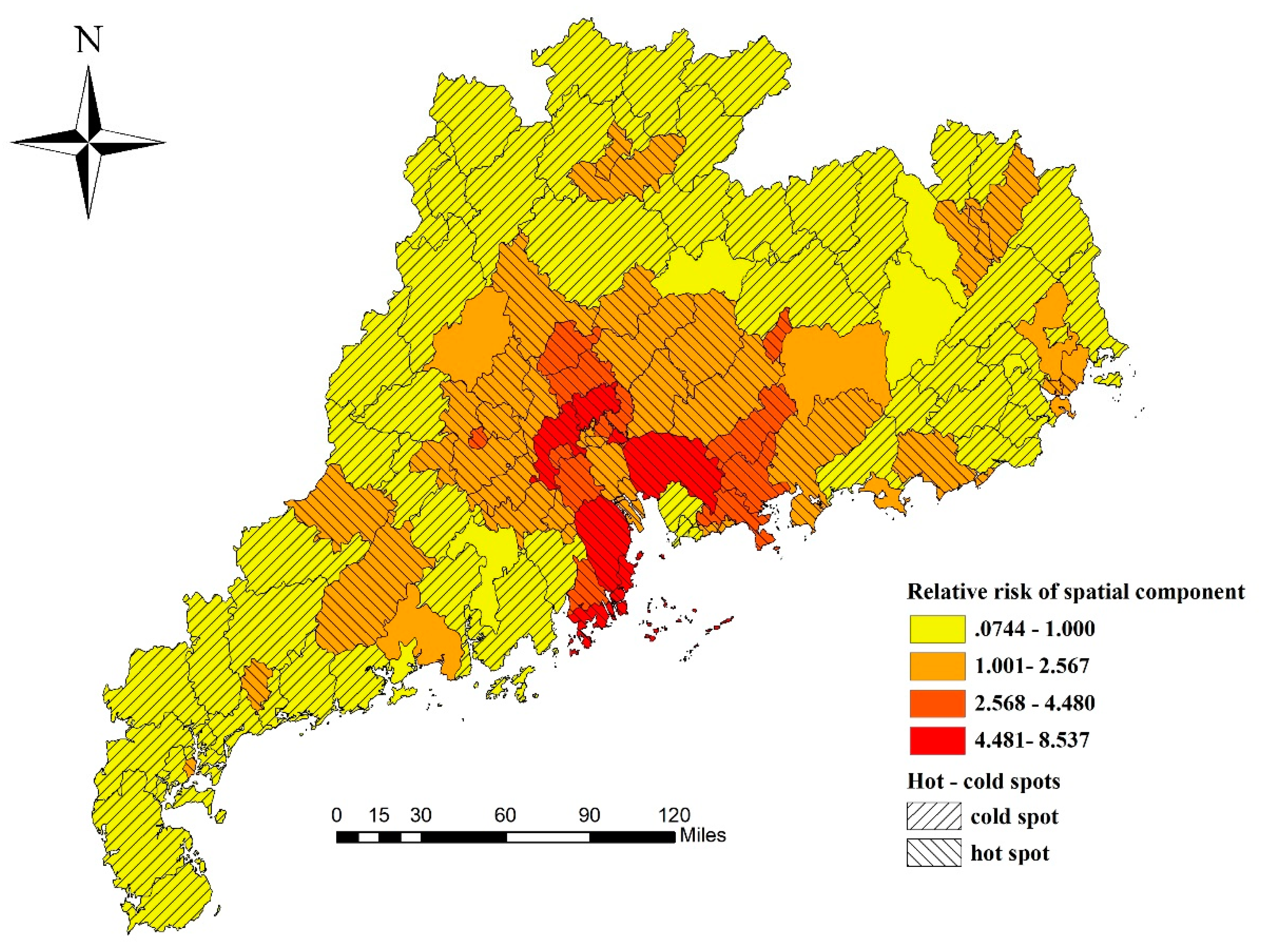
3.3. Spatial Distribution
3.4. Temporal Distribution
3.5. Spatiotemporal Interaction Patterns
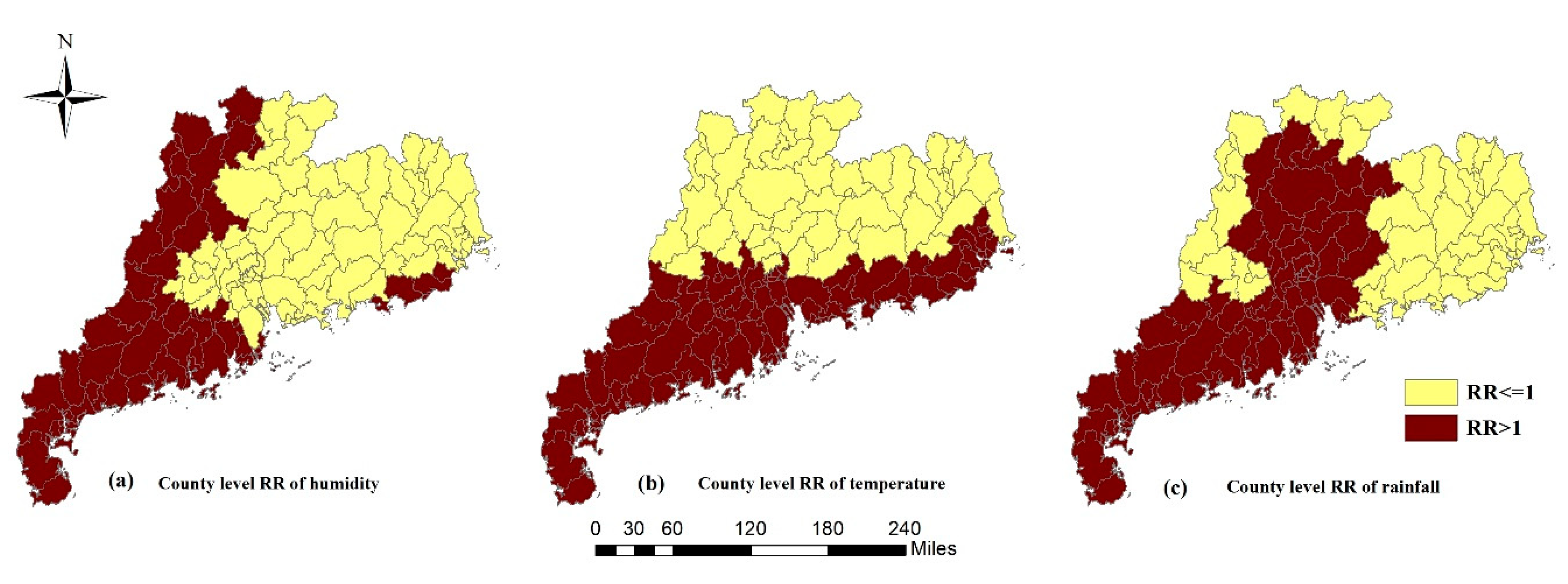
3.6. Potential Predictors
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Goksugur, N.; Goksugur, S. Images in clinical medicine. Hand, foot, and mouth disease. N. Engl. J. Med. 2010, 362, e49. [Google Scholar] [CrossRef]
- Wang, Y.; Feng, Z.; Yang, Y.; Self, S.; Gao, Y.; Longini, I.M.; Wakefield, J.; Zhang, J.; Wang, L.; Chen, X.; et al. Hand, foot, and mouth disease in China: Patterns of spread and transmissibility. Epidemiology 2011, 22, 781–792. [Google Scholar] [CrossRef]
- Qi, L.; Tang, W.; Zhao, H.; Ling, H.; Su, K.; Zhao, H.; Li, Q.; Shen, T. Epidemiological Characteristics and Spatial-Temporal Distribution of Hand, Foot, and Mouth Disease in Chongqing, China, 2009–2016. Int. J. Environ. Res. Public Health 2018, 15, 270. [Google Scholar] [CrossRef] [PubMed]
- Chew, S.P.; Chong, S.L.; Barbier, S.; Matthew, A.; Lee, J.H.; Chan, Y.H. Risk factors for severe hand foot mouth disease in Singapore: A case control study. BMC Infect. Dis. 2015, 15, 486. [Google Scholar] [CrossRef] [PubMed]
- Phung, D.; Nguyen, H.X.; Nguyen, H.; Do, C.M.; Tran, Q.D.; Chu, C. Spatiotemporal variation of hand-foot-mouth disease in relation to socioecological factors: A multiple-province analysis in Vietnam. Sci. Total Environ. 2018, 610–611, 983–991. [Google Scholar] [CrossRef]
- Wang, P.; Goggins, W.B.; Chan, E.Y. Hand, Foot and Mouth Disease in Hong Kong: A Time-Series Analysis on Its Relationship with Weather. PLoS ONE 2016, 11, e161006. [Google Scholar] [CrossRef] [PubMed]
- Sumi, A.; Toyoda, S.; Kanou, K.; Fujimoto, T.; Mise, K.; Kohei, Y.; Koyama, A.; Kobayashi, N. Association between meteorological factors and reported cases of hand, foot, and mouth disease from 2000 to 2015 in Japan. Epidemiol. Infect. 2017, 145, 2896–2911. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China. Overview of the National Notifiable Infectious Disease Epidemic in 2017 [EB/OL]. Available online: http://www.nhfpc.gov.cn/jkj/s3578/201802/de926bdb046749abb7b0a8e23d929104.shtml (accessed on 26 February 2018).
- Zeng, M.; Pu, D.; Mo, X.; Zhu, C.; Gong, S.; Xu, Y.; Lin, G.; Wu, B.; He, S.; Jiao, X.; et al. Children of rural-to-urban migrant workers in China are at a higher risk of contracting severe hand, foot and mouth disease and EV71 infection: A hospital-based study. Emerg. Microbes. Infect. 2013, 2, e72. [Google Scholar] [CrossRef]
- Deng, T.; Huang, Y.; Yu, S.; Gu, J.; Huang, C.; Xiao, G.; Hao, Y. Spatial-temporal clusters and risk factors of hand, foot, and mouth disease at the district level in Guangdong Province, China. PLoS ONE 2013, 8, e56943. [Google Scholar] [CrossRef]
- Zhang, W.; Du, Z.; Zhang, D.; Yu, S.; Hao, Y. Boosted regression tree model-based assessment of the impacts of meteorological drivers of hand, foot and mouth disease in Guangdong, China. Sci. Total Environ. 2016, 553, 366–371. [Google Scholar] [CrossRef]
- Liao, J.; Qin, Z.; Zuo, Z.; Yu, S.; Zhang, J. Spatial-temporal mapping of hand foot and mouth disease and the long-term effects associated with climate and socio-economic variables in Sichuan Province, China from 2009 to 2013. Sci. Total Environ. 2016, 563–564, 152–159. [Google Scholar] [CrossRef]
- Tian, L.; Liang, F.; Xu, M.; Jia, L.; Pan, X.; Clements, A. Spatio-temporal analysis of the relationship between meteorological factors and hand-foot-mouth disease in Beijing, China. BMC Infect. Dis. 2018, 18, 158. [Google Scholar] [CrossRef]
- Liu, J.; Xiang, X.; Pu, Z.; Long, Y.; Xiao, D.; Zhang, W.; Li, Q.; Li, X.; Li, S.; Shao, Z.; et al. Epidemic pattern of hand-foot-and-mouth disease in Xi’an, China from 2008 through 2015. BMC Infect. Dis. 2019, 19, 19. [Google Scholar] [CrossRef]
- Ma, E.; Lam, T.; Chan, K.C.; Wong, C.; Chuang, S.K. Changing epidemiology of hand, foot, and mouth disease in Hong Kong, 2001–2009. Jpn. J. Infect. Dis. 2010, 63, 422–426. [Google Scholar] [PubMed]
- Song, C.; Shi, X.; Bo, Y.; Wang, J.; Wang, Y.; Huang, D. Exploring spatiotemporal nonstationary effects of climate factors on hand, foot, and mouth disease using Bayesian Spatiotemporally Varying Coefficients (STVC) model in Sichuan, China. Sci. Total Environ. 2019, 648, 550–560. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.D.; Xiao, G.X. Spatiotemporal risk mapping of hand, foot and mouth disease and its association with meteorological variables in children under 5 years. Epidemiol. Infect. 2017, 145, 2912–2920. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Du, Z.; Zhang, D.; Yu, S.; Huang, Y.; Hao, Y. Assessing the impact of humidex on HFMD in Guangdong Province and its variability across social-economic status and age groups. Sci. Rep. 2016, 6, 18965. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Du, Z.; Zhang, D.; Yu, S.; Hao, Y. Quantifying the adverse effect of excessive heat on children: An elevated risk of hand, foot and mouth disease in hot days. Sci. Total Environ. 2016, 541, 194–199. [Google Scholar] [CrossRef]
- Liu, L.; Zhao, X.; Yin, F.; Lv, Q. Spatio-temporal clustering of hand, foot and mouth disease at the county level in Sichuan province, China, 2008-2013. Epidemiol. Infect. 2015, 143, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Marta, B.; Michela, C. Spatial and Spatio-Temporal Bayesian Models with R-INLA; John Wiley & Sons: Hoboken, NJ, USA, 2015; pp. 236–246. [Google Scholar]
- The Ministry of Health of The People’s Republic of China. Guide for the Preparedness and Control Measures of Hand, Foot, and Mouth Disease in China; 2008 version; Cap J Public Health: Beijing, China, 2008; pp. 146–148. (In Chinese)
- Studenmund, A.H. Using Econometrics: A Practical Guide, 5th ed.; Pearson International Edition: London, UK, 2006; pp. 258–259. [Google Scholar]
- Besag, J.; York, J.; Mollié, A. Bayesian image restoration, with two applications in spatial statistics. Ann. Inst. Stat. Math. 1991, 43, 1–20. [Google Scholar] [CrossRef]
- Thway, A.M.; Rotejanaprasert, C.; Sattabongkot, J.; Lawawirojwong, S.; Thi, A.; Hlaing, T.M.; Soe, T.M.; Kaewkungwal, J. Bayesian spatiotemporal analysis of malaria infection along an international border: Hlaingbwe Township in Myanmar and Tha-Song-Yang District in Thailand. Malar. J. 2018, 17, 428. [Google Scholar] [CrossRef]
- Lau, S.Y.; Chen, E.; Wang, M.; Cheng, W.; Zee, B.C.; Han, X.; Yu, Z.; Sun, R.; Chong, K.C.; Wang, X. Association between meteorological factors, spatiotemporal effects, and prevalence of influenza A subtype H7 in environmental samples in Zhejiang province, China. Sci. Total Environ. 2019, 663, 793–803. [Google Scholar] [CrossRef]
- Zhang, X.; Xu, C.; Xiao, G. Space-time heterogeneity of hand, foot and mouth disease in children and its potential driving factors in Henan, China. BMC Infect. Dis. 2018, 18, 638. [Google Scholar] [CrossRef] [PubMed]
- Raghavan, R.K.; Hanlon, C.A.; Goodin, D.G.; Davis, R.; Moore, M.; Moore, S.; Anderson, G.A. Bayesian Spatiotemporal Pattern and Eco-climatological Drivers of Striped Skunk Rabies in the North Central Plains. PLoS Negl. Trop. Dis. 2016, 10, e4632. [Google Scholar] [CrossRef]
- Dedefo, M.; Mwambi, H.; Fanta, S.; Assefa, N. Spatiotemporal mapping and detection of mortality cluster due to cardiovascular disease with Bayesian hierarchical framework using integrated nested Laplace approximation: A discussion of suitable statistic applications in Kersa, Oromia, Ethiopia. Geospat. Health 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, T.; Fu, B. A measure of spatial stratified heterogeneity. Ecol. Indic. 2016, 67, 250–256. [Google Scholar] [CrossRef]
- Wang, J.F.; Li, X.H.; Christakos, G.; Liao, Y.L.; Zhang, T.; Gu, X.; Zheng, X.Y. Geographical Detectors-Based Health Risk Assessment and its Application in the Neural Tube Defects Study of the Heshun Region, China. Int. J. Geogr. Inf. Sci. 2010, 24, 107–127. [Google Scholar] [CrossRef]
- Richardson, S.; Thomson, A.; Best, N.; Elliott, P. Interpreting posterior relative risk estimates in disease-mapping studies. Environ. Health Perspect. 2004, 112, 1016–1025. [Google Scholar] [CrossRef]
- Liu, W.; Ji, H.; Shan, J.; Bao, J.; Sun, Y.; Li, J.; Bao, C.; Tang, F.; Yang, K.; Bergquist, R.; et al. Spatiotemporal Dynamics of Hand-Foot-Mouth Disease and Its Relationship with Meteorological Factors in Jiangsu Province, China. PLoS ONE 2015, 10, e131311. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, X.; Pang, C.; Yuan, Z.; Li, H.; Xue, F. Spatio-temporal analysis of the relationship between climate and hand, foot, and mouth disease in Shandong province, China, 2008–2012. BMC Infect. Dis. 2015, 15, 146. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Deng, T.; Yu, S.; Gu, J.; Huang, C.; Xiao, G.; Hao, Y. Effect of meteorological variables on the incidence of hand, foot, and mouth disease in children: A time-series analysis in Guangzhou, China. BMC Infect. Dis. 2013, 13, 134. [Google Scholar] [CrossRef] [PubMed]
- Ma, E.; Lam, T.; Wong, C.; Chuang, S.K. Is hand, foot and mouth disease associated with meteorological parameters? Epidemiol. Infect. 2010, 138, 1779–1788. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Drossinos, Y.; Stilianakis, N.I. Indirect transmission and the effect of seasonal pathogen inactivation on infectious disease periodicity. Epidemics 2013, 5, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Kulldorff, M. A spatial scan statistic. Commun. Stat.-Theory Methods 1997, 26, 1481–1496. [Google Scholar] [CrossRef]

| Covariates | Minimum | 2.5% Percentile | Median | 97.5% Percentile | Maximum |
|---|---|---|---|---|---|
| Average relative humidity (%) | 54.10 | 59.25 | 76.53 | 85.83 | 91.56 |
| Average temperature (°C) | 4.79 | 10.47 | 23.01 | 29.18 | 29.65 |
| Average rainfall (mm) | 0 | 1.66 | 98.76 | 410.11 | 645.50 |
| Sunshine duration (hour) | 18.91 | 38.05 | 149.18 | 253.48 | 303.47 |
| Average wind speed (m/s) | 1.25 | 1.53 | 2.10 | 3.38 | 5.33 |
| Average GDP (yuan) | 5717 | 9981 | 26,370 | 110,421 | 123,247 |
| Covariates | VIF | Covariates | VIF |
|---|---|---|---|
| Average relative humidity (%) | 2.305 | Sunshine duration (hour) | 3.126 |
| Average temperature (°C) | 3.827 | Average wind speed (m/s) | 1.091 |
| Average rainfall (mm) | 2.129 | Average GDP (yuan) | 1.025 |
| Model | Component | DIC | |
|---|---|---|---|
| 1 | Non-spatiotemporal model | 1,083,638.0 | |
| 2 | Spatial model | 422,115.3 | |
| 3 | Temporal model | 816,474.6 | |
| 4 | Spatiotemporal model | 202,885.9 | |
| 5 | Spatiotemporal interaction model | 45,036.5 |
| Data | q | p | Data | q | p | Data | q | p | Data | q | p |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009-01 | 0.122 | 0.856 | 2010-01 | 0.179 | 0.663 | 2011-01 | 0.145 | 0.771 | 2012-01 | 0.321 | 0.013 * |
| 2009-02 | 0.292 | 0.095 | 2010-02 | 0.296 | 0.221 | 2011-02 | 0.238 | 0.302 | 2011-02 | 0.191 | 0.507 |
| 2009-03 | 0.336 | 0.022 * | 2010-03 | 0.366 | 0.058 | 2011-03 | 0.089 | 0.980 | 2011-03 | 0.409 | <0.001 * |
| 2009-04 | 0.301 | 0.038 * | 2010-04 | 0.251 | 0.184 | 2011-04 | 0.215 | 0.534 | 2011-04 | 0.379 | 0.004 * |
| 2009-05 | 0.229 | 0.257 | 2010-05 | 0.190 | 0.507 | 2011-05 | 0.292 | 0.207 | 2011-05 | 0.465 | <0.001 * |
| 2009-06 | 0.265 | 0.362 | 2010-06 | 0.315 | 0.038 * | 2011-06 | 0.274 | 0.112 | 2011-06 | 0.341 | 0.019 * |
| 2009-07 | 0.287 | 0.202 | 2010-07 | 0.403 | 0.002 * | 2011-07 | 0.498 | <0.001 * | 2011-07 | 0.325 | 0.033 * |
| 2009-08 | 0.402 | 0.013 * | 2010-08 | 0.458 | <0.001 * | 2011-08 | 0.299 | 0.069 | 2011-08 | 0.319 | 0.037 * |
| 2009-09 | 0.254 | 0.198 | 2010-09 | 0.221 | 0.541 | 2011-09 | 0.260 | 0.203 | 2011-09 | 0.573 | <0.001 * |
| 2009-10 | 0.246 | 0.243 | 2010-10 | 0.281 | 0.265 | 2011-10 | 0.259 | 0.267 | 2011-10 | 0.290 | 0.101 |
| 2009-11 | 0.266 | 0.264 | 2010-11 | 0.179 | 0.710 | 2011-11 | 0.153 | 0.763 | 2011-11 | 0.158 | 0.715 |
| 2009-12 | 0.129 | 0.916 | 2010-12 | 0.174 | 0.589 | 2011-12 | 0.239 | 0.149 | 2011-12 | 0.264 | 0.096 |
| Covariates | Unstandardized Coefficients (95% CI) | Standardized Coefficients (95% CI) |
|---|---|---|
| Intercept | 0.054 (0.021, 0.138) | 0.397 (0.359, 0.439) |
| Average relative humidity (%) | 1.015 (1.006, 1.024) | 1.102 (1.042, 1.166) |
| Average temperature (°C) | 1.045 (1.021, 1.069) | 1.291 (1.128, 1.476) |
| Average rainfall (cm) | 1.004 (1.001, 1.008) | 1.050 (1.008, 1.094) |
| Sunshine duration (10 h) | 0.997 (0.985, 1.009) | 0.982 (0.915, 1.054) |
| Average wind speed (dm/s) | 0.998 (0.990, 1.007) | 0.991 (0.951, 1.032) |
| Average GDP (1000 yuan) | 0.999 (0.994, 1.003) | 0.961 (0.835, 1.105) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Lai, Y.; Du, Z.; Zhang, W.; Feng, C.; Li, R.; Hao, Y. Spatiotemporal Distribution of Hand, Foot, and Mouth Disease in Guangdong Province, China and Potential Predictors, 2009–2012. Int. J. Environ. Res. Public Health 2019, 16, 1191. https://doi.org/10.3390/ijerph16071191
Wang Y, Lai Y, Du Z, Zhang W, Feng C, Li R, Hao Y. Spatiotemporal Distribution of Hand, Foot, and Mouth Disease in Guangdong Province, China and Potential Predictors, 2009–2012. International Journal of Environmental Research and Public Health. 2019; 16(7):1191. https://doi.org/10.3390/ijerph16071191
Chicago/Turabian StyleWang, Yijing, Yingsi Lai, Zhicheng Du, Wangjian Zhang, Chenyang Feng, Ruixue Li, and Yuantao Hao. 2019. "Spatiotemporal Distribution of Hand, Foot, and Mouth Disease in Guangdong Province, China and Potential Predictors, 2009–2012" International Journal of Environmental Research and Public Health 16, no. 7: 1191. https://doi.org/10.3390/ijerph16071191
APA StyleWang, Y., Lai, Y., Du, Z., Zhang, W., Feng, C., Li, R., & Hao, Y. (2019). Spatiotemporal Distribution of Hand, Foot, and Mouth Disease in Guangdong Province, China and Potential Predictors, 2009–2012. International Journal of Environmental Research and Public Health, 16(7), 1191. https://doi.org/10.3390/ijerph16071191





