Abstract
Skin diseases have caused a heavy burden on the infected population worldwide. This study aimed to examine the health-related quality of life (HRQOL) among patients with different skin diseases and identify associated factors. A cross-sectional study with 430 participants was conducted at the Vietnam National Hospital of Dermatology and Venereology (NHD) from September to November 2018. The EuroQol-5 Dimensions-5 Levels (EQ-5D-5L) instrument was employed, which measures the EQ-5D index from five domains including mobility, self-care, usual activity, pain/discomfort, and anxiety/depression. Multivariate Tobit regression was adopted to determine factors that were associated with HRQOL (EQ-5D index). The rate of atopic dermatitis was the highest with 28.8%, following by contact dermatitis (17.0%) and skin fungal infections (13.0%). Regarding HRQOL, anxiety/depression was the most common health problem in patients with skin diseases (71.8%), following by pain/discomfort (63.6%). The mean EQ-5D index score was 0.73 (SD = 0.19). The lowest EQ-5D index scores were obtained for females with skin infections (mean = 0.52) and for males with psoriasis (mean = 0.59). Females had significantly lower scores compared to males (Coef. = −0.06; 95% CI = −0.11 to −0.01). Higher income and living in rural areas were also negatively correlated with the EQ-5D index. This study demonstrated the low HRQOL among patients with skin diseases in Vietnam and emphasized the vulnerability of patients with different socioeconomic statuses to their HRQOL.
1. Introduction
Skin diseases have been causing heavy burden all over the world regardless of age and gender, especially in tropical regions [1]. According to The Global Burden of Disease project, skin diseases were estimated to cause 41.6 million disability-adjusted life years (DALYs)—equivalent to 1.79% of the total burden of diseases [2], ranking the fourth among causes of non-fatal morbidity worldwide [3]. Dermatitis accounts for the highest burden compared to other skin diseases with 0.38% of total disease burdens globally, following by acne vulgaris (0.29%), psoriasis (0.19%), and urticaria (0.19%) [2]. Among people 65+ years old, Hahnel et al. in their systematic review indicated that the most common skin diseases were fungal infections (prevalence rate 14.3% to 64%), following by dermatitis (1% to 58.7%), xerosis (5.4% to 85.5%), and benign skin tumors (1.7% to 74.5%) [4].
Skin diseases cause a wide range of detrimental effects on all aspects of a patient’s life. They may suffer from physical impairment, psychological distress, and even mortality [5]. Skin diseases, in many cases, are the potentially surface presentation of more serious illnesses such as HIV/AIDS or many neglected tropical diseases [2,6]. Regarding financial burden, patients with skin diseases are also more likely to suffer high medical cost and lost work productivity [7]. Moreover, severe skin-related symptoms on the face and body can deteriorate self-esteem and self-confidence of patients, which significantly affect their involvement in social activities [8,9,10].
Due to the complicated consequences of skin diseases in patients’ lives, instead of focusing on medical outcomes alone, physicians are encouraged to pay attention to improving the overall health and well-being of these patients. One indicator that can reflect these aspects is the health-related quality of life (HRQOL) [11]. Previous studies indicated that the perception of the patient regarding their physical, mental, and emotional conditions as well as how they function socially would determine their state of wellness and burden of disease [11,12]. Moreover, the HRQOL evaluation provides a homogeneous outcome to compare the impacts of different skin diseases, as well as the effectiveness of different treatment options for each disease. There have been a number of studies attempting to measure the HRQOL of people with specific skin diseases [8,9,13,14,15]. A multicenter study was conducted in Europe in 2013 across 13 countries covering 26 categories of disease, which reported the highest HRQOL impairment in people with hidradenitis suppurativa, blistering conditions, leg ulcers, psoriasis, and eczemas [16]. However, the results of these studies varied significantly, requiring contextualized evidence for each country in order to optimize the treatment outcomes in each population.
Despite being in a region that favors the development of many skin conditions, the literature looking into prevalence of skin diseases in Vietnam as well as the HRQOL of patients have been limited. It can be argued that, especially in resource-poor settings, knowledge regarding the HRQOL of people with skin diseases would be a reference point for developing contextualized, individual-focus interventions that potentially deliver results more efficiently. Thus, this study aimed to explore the HRQOL impairments of people with different skin diseases. Moreover, we determined socioeconomic inequalities in HRQOL among these patients in order to identify the most socially vulnerable populations for the HRQOL reduction due to skin diseases in Vietnam. The results will be helpful in drawing implications for the development and implementation of appropriate care/treatment.
2. Materials and Methods
2.1. Study Design and Participants
The protocol of the study was approved by the Institutional Review Board of the Vietnam National Hospital of Dermatology and Venereology (code 855/HDDDDBVDLTU). We conducted a cross-sectional study at the outpatient clinic in the Vietnam National Hospital of Dermatology and Venereology (NHD) during the period of September–November 2018. The NHD is one of the main centers for dermatology and venereology diagnosis and treatment in Vietnam, providing services for a broad range of patients with varying illness severity. Many of the patients being treated at the NHD were previously transferred from health facilities at provincial and communal levels due to the level of severity of their conditions. At the outpatient clinic, 1500–2000 patients are examined per day.
We used a convenient sampling technique to select participants for our study among patients who were diagnosed and treated at the NHD at the time of study. Eligibility criteria for participating in our study were: (1) being 18 years old or above; (2) being able to coherently answer the questions asked by our interviewers; and (3) giving written consent expressing agreement to be involved in the study. To estimate the appropriate sample size, we used confidence level = 95%; expected mean = 0.70; expected standard deviation = 0.20 (according to a previous study in 13 European countries [16]), and absolute precision required = 0.02. The essential sample size was 385. After adding 15% of the sample size to prevent those who did not agree to participate or did not complete the interview, the final sample size was 443 patients. Finally, we successfully recruited a total of 430 participants for the study (97.1%).
2.2. Measurements and Instruments
Face-to-face interviews were conducted by trained medical students from Hanoi Medical University with 15–20 min per interview using a structured questionnaire in Vietnamese language. Selected participants were invited to a private room at the hospital in which interviews took place to ensure the confidentiality and quality of the answers. Data regarding the socioeconomic status of participants as well as their health status and HRQOL were collected, and are detailed below.
2.2.1. Socioeconomic Characteristics and Alcohol Use
Data about gender (“What is your gender?”), age (“How old are you?”), education (“Which education level have you completed?”), marital status (What is your current marital status?”), occupation (“What is your current occupation that you spend most of the time on?”), living location (“Do you live in rural or urban area?”), and possession of health insurance (“Do you have any type of health insurance?”) were collected. We also obtained information about household monthly income (“Could you please estimate your average household monthly income from all possible sources?”), and then we divided participants into five income quintiles: lowest income, low income, middle income, high income, and highest income. All of these questions were open-ended questions, and patients were asked these questions without suggestions.
Moreover, we asked patients to report the frequency of alcohol consumption (“How often do you drink alcohol?”).
2.2.2. Dermatology Conditions and Health-Related Quality of Life (HRQOL)
The information on the type and severity of dermatology diseases respondents was collected by extracting these data from patients’ medical records. The HRQOL of the patients was assessed using the EuroQOl-5 dimensions-5 levels (EQ-5D-5L) instrument. The version used in our study was translated into Vietnamese and validated in another HRQOL study in Vietnam [17,18]. The Vietnamese EQ-5D-5L has good psychometric properties with a good convergent validity, discrimination validity, and Cronbach’s alpha = 0.85 [17]. The EQ-5D-5L measured HRQOL through five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each domain had five different respond options to choose, ranging from no problem to extreme problem/impossible to do. The combination of responses yielded 3125 unique health statuses [19]. By using a cross-walk value set developed for Vietnam, 3125 health statuses were converted into 3125 single indexes within the score range of –0.566 to 1.000 [19,20].
2.3. Statistical Analysis
Stata version 15.0 (Stata Corp. LP, College Station, TX, USA) was used to analyze the data. We used Mann–Whitney and Chi-squared tests to determine differences between genders. Multivariate Tobit regression, along with stepwise selection strategies (p < 0.2 as the threshold for selecting variables), was adopted to identify factors that were associated with the HRQOL of respondents. A p-value < 0.05 was considered statistically significant.
3. Results
Of the 430 dermatology patients in this study, the majority were female (54.7%). The mean age of participants was 36.5 (SD = 14.1) years, in which the highest proportion was the age group of 18–30 years (45.6%). Most of the patients had completed more than a high school education (66.5%) and had partners or were married (62.2%). About one third of the patients (32.1%) were freelancers, while 2.8% were unemployed. Patients were predominantly living in urban areas (62.4%) and had health insurances (83.2%). There were 44.3% of patients not drinking alcohol. Differences between male and female patients were found in age, education, marital status, occupation, and frequency of drinking alcohol (p < 0.05) (Table 1).

Table 1.
Demographic characteristics of dermatology patients.
Table 2 depicts the health conditions and HRQOL of dermatology patients. The rate of atopic dermatitis was the highest with 28.8%, following by contact dermatitis (17.0%) and skin fungal infections (13.0%). Regarding HRQOL, anxiety/depression was the most common health problem in patients with skin diseases (71.8%), followed by pain/discomfort (63.6%). The mean EQ-5D index score was 0.73 (SD = 0.19).

Table 2.
Health-related quality of life (HRQOL) and health status of respondents.
Figure 1 reveals the proportion of patients suffering problems in each EQ-5D dimension according to different dermatology diseases. The percentage of patients with skin infections having mobility problems was the highest (61.5%). Meanwhile, the rates of psoriasis patients with problems in the other four dimensions including self-care, usual activities, pain/discomfort, and anxiety/depression were the highest compared to those with other diseases (31.0%, 38.5%, 82.8%, and 82.1%, respectively).
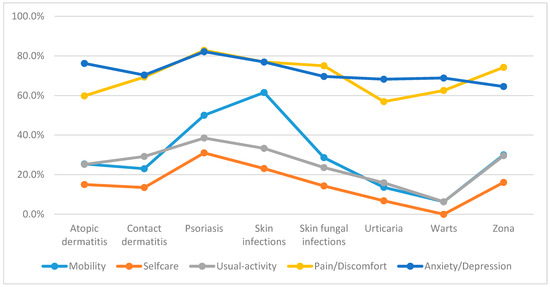
Figure 1.
Percentage of patients reporting any problems in EuroQol-5 Dimensions-5 Levels (EQ-5D-5L) dimensions according to different dermatology disorders.
Regarding EQ-5D index score, warts patients had the highest score at 0.80 while psoriasis patients had the lowest score at 0.63. In terms of gender, the EQ-5D index score was the lowest in female patients with skin infections (mean = 0.52) and in male patients with psoriasis (mean = 0.59) (Figure 2).
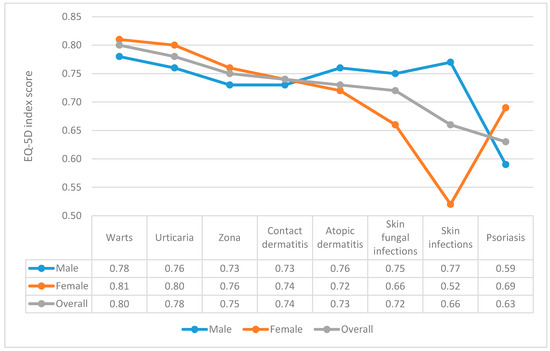
Figure 2.
EQ-5D index according to gender and different dermatology disorders.
Table 3 reveals that among dermatology patients, being female and living in rural areas were positively associated with having problems in anxiety/depression (OR = 2.35; 95% CI = 1.21–4.56 and OR = 1.94; 95% CI = 1.03–3.65, respectively). Patients drinking alcohol weekly were 3.5 times more likely to suffer anxiety/depression (OR = 3.50; 95% CI = 1.23; 9.97) than those not drinking alcohol. Those in the highest income group (OR = 3.11; 95% CI = 1.45–6.68) or living in rural areas (OR = 2.38; 95% CI = 1.40–4.03) were more likely to experience pain/discomfort compared to patients in the lowest income group or living in urban areas, respectively.

Table 3.
Socioeconomic factors associated with the HRQOL of dermatology patients.
Regarding the EQ-5D index, female patients had a significantly lower score compared to males (Coef. = −0.06; 95% CI = −0.11–−0.01). Higher income (compared to the lowest income) and living in rural areas (compared to urban areas) were also negatively correlated with the EQ-5D index score. Patients who were students had markedly higher EQ-5D index scores than unemployed patients (Coef. = 0.21; 95% CI = 0.05–0.37).
In terms of dermatology illnesses, patients having skin infections or psoriasis were more likely to suffer pain/discomfort. Patients with psoriasis also had a significantly lower EQ-5D index score compared to those not having this disease.
4. Discussion
The current study explored the HRQOL in patients with skin diseases as well as their socioeconomic determinants. Overall, we found a low HRQOL in both the entire sample as well as in patients with specific dermatology diseases. We also underlined that people who were female, unemployed, and living in rural areas were the populations most vulnerable to the decrement of the HRQOL if experiencing dermatology diseases. Notably, contrary to our expectation, high income was a significant predictor of poor HRQOL among dermatology patients.
In this study, we observed a low EQ-5D index with the mean value of 0.73 among dermatology patients, which was significantly lower than that in the Vietnamese general population [18], even in disadvantaged populations such as elderly, rural, or mountainous people [21,22,23]. By subgroup analysis, we confirmed the robustness of the HRQOL for each disease when compared to previous studies. For instance, the mean EQ-5D index score of urticaria patients in our study was 0.78, which was equivalent to the index score of patients experiencing moderate urticaria in three randomized clinical trials [24]. The EQ-5D index observed in our psoriasis patients (mean = 0.65) was similar to the mean score of patients with moderate-to-severe psoriasis in Europe [25], while the score in atopic dermatitis (eczema) patients (mean = 0.73) was approximately equal to this population in the United States [26]. Therefore, we believe that our results could be partly used as a vital component to compute quality-adjusted life years (QALYs), which serves as an indicator of health economic evaluation and aids in decision-making in dermatology care [27].
Our finding showed a particularly high rate of patients suffering physical and psychological impartments across dermatology diseases. The clinical impacts of dermatology diseases on depression, anxiety, and the physical health of patients have been documented [28,29,30], which were major drivers of the deterioration of the HRQOL [29,30]. Along with painful or itching conditions that patients have to suffer during the course of diseases [13,31], depression/anxiety conditions might be developed that can be explained by the onset of immunity disorders and increased proinflammatory cytokine concentrations [32]. Moreover, some previous studies indicated that patients with skin diseases might feel socially stigmatized due to their abnormal skin [33,34]. In our study, more than 70% of our respondents reported anxiety/depression, which was more severe than that of populations with other chronic conditions such as respiratory and cardiovascular diseases [29,33].
Females were found to be more greatly influenced by the dermatology illnesses compared to their male counterparts since they had a significantly lower HRQOL and a higher likelihood of having anxiety/depression. This finding was consistent with previous works [35,36,37]. The common reason for this was that physical appearance was a more sensitive issue in women than men, and dermatology disorders could develop more psychological distress among women [35]. Another study argued the differences of genetic and other molecular factors such as abnormalities in genes, metabolism, or histamin between the two genders contributed to the higher risk of depression among females [38].
Being unemployed and living in rural areas were considered significant predictors of lower HRQOL among dermatology patients. Prior studies highlighted a higher HRQOL in employed people compared to unemployed individuals due to a better life standard and earlier dermatological care access [15,18,39]. These reasons can be applied when explaining the differences in the HRQOL between rural and urban patients [9,40,41]. Interestingly, in multivariate models, we found that patients who had a higher financial status were more likely to have a poorer HRQOL and experience pain/discomfort, which was different from previous studies conducted worldwide [14,42,43]. The role of disease severity might be potential reason for these phenomena. A study in India found similar results that income was negatively correlated with HRQOL [42]. We suppose that those with a higher income also have greater concern regarding their self-esteem and appearance compared to those with a low income [44,45]. Skin diseases have been well-documented to remarkably affect the appearance and comfort of patients. In a regression model, we also found that those in the highest income group were three times more likely to suffer pain/discomfort than patients in the lowest income group. Collectively, patients with a high income possibly had a lower HRQOL than those with a low income. However, the reason for this is not clear; further studies are required to elucidate this gap.
Several suggestions could be drawn from the findings of this study. First, proper pain management and psychological counselling services should be provided to patients with skin diseases given the particularly high prevalence of pain and anxiety/depression in this population. Second, gender, living location, and occupation disparities in HRQOL suggest that more attention should be paid to female, rural, and unemployed patients, who are disadvantaged groups, in developing dermatology care services. Third, monitoring HRQOL should be performed regularly by using a short, simple instrument such as the EQ-5D-5L in order to track the progress in addressing the inequalities between different socioeconomic groups among skin disease patients.
There are a number of methodological issues that should be acknowledged in this study. First, we were unable to detect the causal relationships between socioeconomic status and HRQOL due to the nature of the cross-sectional design. Thus, further longitudinal studies are required. Second, information about HRQOL and socioeconomic status was subjectively self-reported, which could lead to measurement error. Third, using the convenient sampling technique in one hospital with a small sample size might constrain our generalizability to other dermatology populations. More studies on a large scale with different settings are warranted to confirm the effects of socioeconomic status on the HRQOL of patients with skin diseases.
5. Conclusions
In conclusion, this cross-section study demonstrated the low HRQOL among patients with skin diseases in Vietnam, of which warts patients had the highest HRQOL and psoriasis patients had the lowest HRQOL. This study also emphasized the impacts of socioeconomic status on the HRQOL, particularly among patients who were female, unemployed, living rural areas, and having a high household income.
Author Contributions
Conceptualization, S.H.N., L.H.N. and C.A.L.; Data curation, C.T.N., T.H.T.L., B.X.T., C.S.H.H. and R.C.M.H.; Formal analysis, T.H.T.L. and R.C.M.H.; Methodology, S.H.N., L.H.N., B.X.T. and R.C.M.H.; Project administration, S.H.N.; Supervision, T.H.T.L.; Visualization, L.H.N. and C.S.H.H.; Writing—original draft, S.H.N., L.H.N., G.T.V., C.T.N. and C.A.L.; Writing—review & editing, S.H.N., L.H.N., G.T.V., C.T.N., B.X.T., C.A.L., C.S.H.H. and R.C.M.H.
Funding
This research received no external funding.
Acknowledgments
We would thank all patients who provide their information for this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hay, R.; Bendeck, S.E.; Chen, S.; Estrada, R.; Haddix, A.; McLeod, T.; Mahe, A. Skin Diseases. In Disease Control Priorities in Developing Countries; Jamison, D.T., Breman, J.G., Measham, A.R., Alleyne, G., Claeson, M., Evans, D.B., Jha, P., Mills, A., Musgrove, P., Eds.; The World Bank: Washington, DC, USA, 2006. [Google Scholar]
- Karimkhani, C.; Dellavalle, R.P.; Coffeng, L.E.; Flohr, C.; Hay, R.J.; Langan, S.M.; Nsoesie, E.O.; Ferrari, A.J.; Erskine, H.E.; Silverberg, J.I.; et al. Global Skin Disease Morbidity and Mortality: An Update From the Global Burden of Disease Study 2013. JAMA Dermatol. 2017, 153, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Seth, D.; Cheldize, K.; Brown, D.; Freeman, E.F. Global Burden of Skin Disease: Inequities and Innovations. Curr. Dermatol. Rep. 2017, 6, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Hahnel, E.; Lichterfeld, A.; Blume-Peytavi, U.; Kottner, J. The epidemiology of skin conditions in the aged: A systematic review. J. Tissue Viability 2017, 26, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Basra, M.K.; Shahrukh, M. Burden of skin diseases. Expert Rev. Pharmacoecon. Outcomes Res. 2009, 9, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Engelman, D.; Fuller, L.C.; Solomon, A.W.; McCarthy, J.S.; Hay, R.J.; Lammie, P.J.; Steer, A.C. Opportunities for Integrated Control of Neglected Tropical Diseases That Affect the Skin. Trends Parasitol. 2016, 32, 843–854. [Google Scholar] [CrossRef] [PubMed]
- Tun, K.; Shurko, J.F.; Ryan, L.; Lee, G.C. Age-based health and economic burden of skin and soft tissue infections in the United States, 2000 and 2012. PLoS ONE 2018, 13, e0206893. [Google Scholar] [CrossRef] [PubMed]
- Jankowiak, B.; Sekmistrz, S.; Kowalewska, B.; Niczyporuk, W.; Krajewska-Kulak, E. Satisfaction with life in a group of psoriasis patients. Postepy Dermatol. Alergol. 2013, 30, 85–90. [Google Scholar] [CrossRef]
- Abolfotouh, M.A.; Al-Khowailed, M.S.; Suliman, W.E.; Al-Turaif, D.A.; Al-Bluwi, E.; Al-Kahtani, H.S. Quality of life in patients with skin diseases in central Saudi Arabia. Int. J. Gen. Med. 2012, 5, 633–642. [Google Scholar] [CrossRef]
- De Korte, J.; Sprangers, M.A.; Mombers, F.M.; Bos, J.D. Quality of life in patients with psoriasis: A systematic literature review. J. Investig. Dermatol. Symp. Proc. 2004, 9, 140–147. [Google Scholar] [CrossRef]
- Megari, K. Quality of Life in Chronic Disease Patients. Health Psychol. Res. 2013, 1, e27. [Google Scholar] [CrossRef]
- Kim, J.-H.; Park, E.-C. Impact of socioeconomic status and subjective social class on overall and health-related quality of life. BMC Public Health 2015, 15, 783. [Google Scholar] [CrossRef]
- Lasek, R.J.; Chren, M.M. Acne vulgaris and the quality of life of adult dermatology patients. Arch. Dermatol. 1998, 134, 454–458. [Google Scholar] [CrossRef]
- Vasquez, R.; Wang, D.; Tran, Q.P.; Adams-Huet, B.; Chren, M.M.; Costner, M.I.; Cohen, J.B.; Werth, V.P.; Chong, B.F. A multicentre, cross-sectional study on quality of life in patients with cutaneous lupus erythematosus. Br. J. Dermatol. 2013, 168, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Pack, T.G.; Szirony, G.M.; Kushner, J.D.; Bellaw, J.R. Quality of life and employment in persons with multiple sclerosis. Work 2014, 49, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Balieva, F.; Kupfer, J.; Lien, L.; Gieler, U.; Finlay, A.Y.; Tomás-Aragonés, L.; Poot, F.; Misery, L.; Sampogna, F.; Middendorp, H.; et al. The burden of common skin diseases assessed with the EQ5D™: A European multicentre study in 13 countries. Br. J. Dermatol. 2017, 176, 1170–1178. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Ohinmaa, A.; Nguyen, L.T. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. Health Qual. Life Outcomes 2012, 10, 132. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Tran, B.X.; Hoang Le, Q.N.; Tran, T.T.; Latkin, C.A. Quality of life profile of general Vietnamese population using EQ-5D-5L. Health Qual. Life Outcomes 2017, 15, 199. [Google Scholar] [CrossRef] [PubMed]
- Reenen, M.v.; Janssen, B. EQ-5D-5L User Guide—Basic Information on How to Use the EQ-5D-5L Instrument; EuroQOL: Rotterdam, The Netherlands, 2015. [Google Scholar]
- Mai, V.Q.; Minh, H.V.; Sun, S.; Giang, K.B.; Sahlen, K.G. Valuing Health—Related Quality of Life: An EQ-5D-5L Value Set for Vietnam; Hanoi University of Public Health: Hanoi, Vietnam, 2018. [Google Scholar]
- Huong, N.T.; Ha, L.T.H.; Tien, T.Q. Determinants of Health-Related Quality of Life Among Elderly: Evidence From Chi Linh Town, Vietnam. Asia Pac. J. Public Health 2017, 29, 84s–93s. [Google Scholar] [CrossRef]
- Hoi le, V.; Chuc, N.T.; Lindholm, L. Health-related quality of life, and its determinants, among older people in rural Vietnam. BMC Public Health 2010, 10, 549. [Google Scholar] [CrossRef]
- Tran, B.X.; Moir, M.P.; Thai, T.P.T.; Nguyen, L.H.; Ha, G.H.; Nguyen, T.H.T.; Truong, N.T.; Latkin, C.A. Socioeconomic Inequalities in Health-Related Quality of Life among Patients with Cardiovascular Diseases in Vietnam. BioMed Res. Int. 2018, 2018, 2643814. [Google Scholar] [CrossRef]
- Hawe, E.; McBride, D.; Balp, M.M.; Tian, H.; Halliday, A.; Stull, D.E. EQ-5D Utilities in Chronic Spontaneous/Idiopathic Urticaria. PharmacoEconomics 2016, 34, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Dauden, E.; Griffiths, C.E.; Ortonne, J.P.; Kragballe, K.; Molta, C.T.; Robertson, D.; Pedersen, R.; Estojak, J.; Boggs, R. Improvements in patient-reported outcomes in moderate-to-severe psoriasis patients receiving continuous or paused etanercept treatment over 54 weeks: The CRYSTEL study. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Dibenedetti, D.; Baranowski, E.; Zelt, S.; Reynolds, M.; Sherrill, B. Assessing United States Patient and Dermatologist Experiences with Severe Chronic Hand Eczema. J. Clin. Aesthetic Dermatol. 2015, 8, 19–27. [Google Scholar]
- Glick, H.A.; Doshi, J.A.; Sonnad, S.S.; Polsky, D. Economic Evaluation in Clinical Trials; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Balp, M.M.; Vietri, J.; Tian, H.; Isherwood, G. The Impact of Chronic Urticaria from the Patient’s Perspective: A Survey in Five European Countries. Patient 2015, 8, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Møller, A.H.; Erntoft, S.; Vinding, G.R.; Jemec, G.B. A systematic literature review to compare quality of life in psoriasis with other chronic diseases using EQ-5D-derived utility values. Patient Relat. Outcome Meas. 2015, 6, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Brazier, J.; Longworth, L. EQ-5D in skin conditions: An assessment of validity and responsiveness. Eur. J. Health Econ. 2015, 16, 927–939. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, B.F.; Lawlor, F.; Simpson, J.; Morgan, M.; Greaves, M.W. The impact of chronic urticaria on the quality of life. Br. J. Dermatol. 1997, 136, 197–201. [Google Scholar] [CrossRef]
- Filakovic, P.; Biljan, D.; Petek, A. Depression in dermatology: An integrative perspective. Psychiatr. Danub. 2008, 20, 419–425. [Google Scholar]
- Reich, K.; Segaert, S.; Van de Kerkhof, P.; Durian, C.; Boussuge, M.P.; Paolozzi, L.; Wajdula, J.; Boggs, R. Once-weekly administration of etanercept 50 mg improves patient-reported outcomes in patients with moderate-to-severe plaque psoriasis. Dermatology 2009, 219, 239–249. [Google Scholar] [CrossRef]
- Hrehorow, E.; Salomon, J.; Matusiak, L.; Reich, A.; Szepietowski, J.C. Patients with psoriasis feel stigmatized. Acta Derm. Venereol. 2012, 92, 67–72. [Google Scholar] [CrossRef]
- Mina, S.; Jabeen, M.; Singh, S.; Verma, R. Gender differences in depression and anxiety among atopic dermatitis patients. Indian J. Dermatol. 2015, 60, 211. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, X.; Lai, W.; Long, E.; Zhang, X.; Li, W.; Zhu, Y.; Chen, C.; Zhong, X.; Liu, Z.; et al. Prevalence of depression and depressive symptoms among outpatients: A systematic review and meta-analysis. BMJ Open 2017, 7, e017173. [Google Scholar] [CrossRef] [PubMed]
- Sampogna, F.; Chren, M.M.; Melchi, C.F.; Pasquini, P.; Tabolli, S.; Abeni, D. Age, gender, quality of life and psychological distress in patients hospitalized with psoriasis. Br. J. Dermatol. 2006, 154, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Timonen, M.; Jokelainen, J.; Hakko, H.; Silvennoinen-Kassinen, S.; Meyer-Rochow, V.B.; Herva, A.; Rasanen, P. Atopy and depression: Results from the Northern Finland 1966 Birth Cohort Study. Mol. Psychiatry 2003, 8, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Hultman, B.; Hemlin, S.; Hornquist, J.O. Quality of life among unemployed and employed people in northern Sweden. Are there any differences? Work 2006, 26, 47–56. [Google Scholar] [PubMed]
- McCaffrey, N.; Kaambwa, B.; Currow, D.C.; Ratcliffe, J. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual. Life Outcomes 2016, 14, 133. [Google Scholar] [CrossRef]
- Vaidya, T.; Zubritsky, L.; Alikhan, A.; Housholder, A. Socioeconomic and geographic barriers to dermatology care in urban and rural US populations. J. Am. Acad. Dermatol. 2018, 78, 406–408. [Google Scholar] [CrossRef]
- Nayak, P.B.; Girisha, B.S.; Noronha, T.M. Correlation between Disease Severity, Family Income, and Quality of Life in Psoriasis: A Study from South India. Indian Dermatol. Online J. 2018, 9, 165–169. [Google Scholar] [CrossRef]
- Thakolwiboon, S.; Upala, S.; Geeratragool, T.; Benjatikul, N.; Uathaya, M.; Tripipitsiriwat, A.; Jiranapakul, S.; Chutinimitkul, B.; Wongpraparut, C.; Kulthanan, K.; et al. The factors affecting quality of life in Thai psoriasis patients. J. Med. Assoc. Thai 2013, 96, 1344–1349. [Google Scholar]
- Bannink, R.; Pearce, A.; Hope, S. Family income and young adolescents’ perceived social position: Associations with self-esteem and life satisfaction in the UK Millennium Cohort Study. Arch. Dis. Child. 2016, 101, 917–921. [Google Scholar] [CrossRef]
- Von Soest, T.; Wichstrom, L.; Kvalem, I.L. The development of global and domain-specific self-esteem from age 13 to 31. J. Personal. Soc. Psychol. 2016, 110, 592–608. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).