Comparing Quality of Life in Breast Cancer Patients Who Underwent Mastectomy Versus Breast-Conserving Surgery: A Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection and Extracted Information
2.4. Statistical Analysis
3. Results
3.1. Cohort Characteristics
3.2. Outcome Analysis
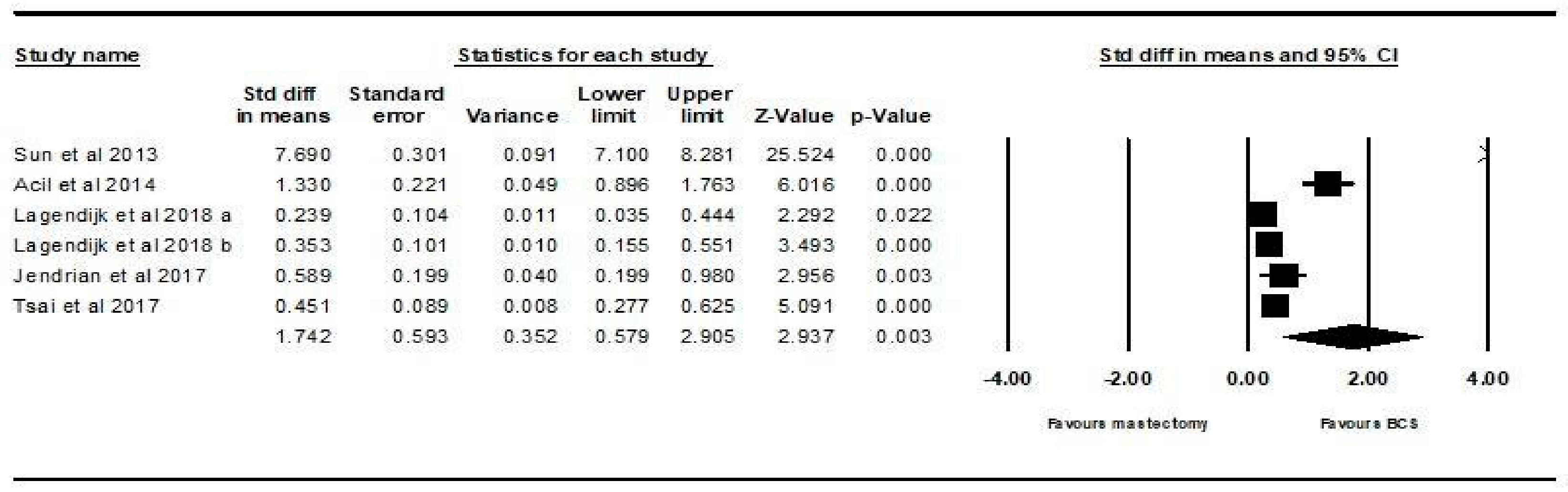
3.2.1. Body Image Outcome
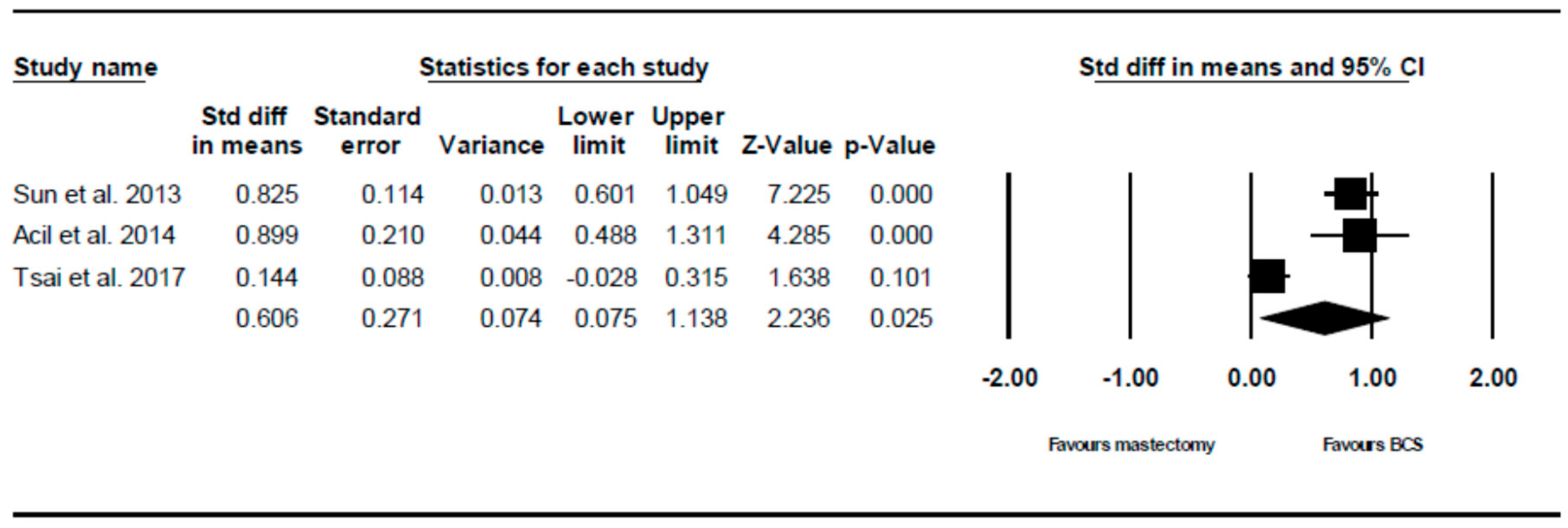
3.2.2. Future Perspective Outcome
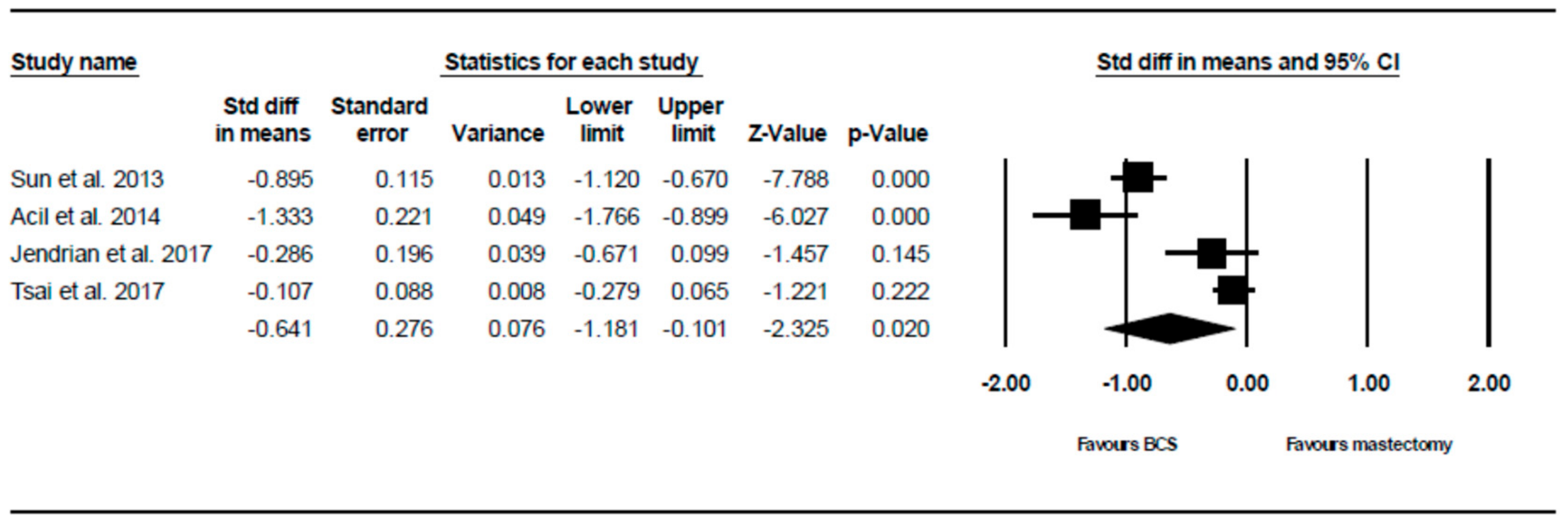
3.2.3. Systemic Therapy Side Effects Outcome
3.3. Meta-Regression and Publication Bias
3.3.1. Body Image
3.3.2. Systemic Therapy Side Effects
4. Discussion
4.1. Significant Results
4.2. Nonsignificant Results
4.3. Limitations
4.4. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA A Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [Green Version]
- Christiansen, P.; Carstensen, S.L.; Ejlertsen, B.; Kroman, N.; Offersen, B.; Bodilsen, A.; Jensen, M.B. Breast conserving surgery versus mastectomy: Overall and relative survival—A population based study by the Danish Breast Cancer Cooperative Group (DBCG). Acta Oncol. 2017, 57, 19–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vila, J.; Gandini, S.; Gentilini, O. Overall survival according to type of surgery in young (≤40 years) early breast cancer patients: A systematic meta-analysis comparing breast-conserving surgery versus mastectomy. Breast 2015, 24, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Sinnadurai, S.; Kwong, A.; Hartman, M.; Hartman Tan, E.Y.; Bhoo-Pathy, N.T.; Dahlui, M.; See, M.H.; Yip, C.H.; Taib, N.A.; Bhoo-Pathy, N.; et al. Breast-conserving surgery versus mastectomy in young women with breast cancer in Asian settings. BJS Open 2018, 3, 48–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, C.; Hu, G.; Biskup, E.; Qiu, X.; Zhang, H.; Zhang, H. Depression Induced by Total Mastectomy, Breast Conserving Surgery and Breast Reconstruction: A Systematic Review and Meta-analysis. World J. Surg. 2018, 42, 2076–2085. [Google Scholar] [CrossRef] [PubMed]
- Tralongo, P.; Surbone, A.; Serraino, D.; Maso, L.D. Major patterns of cancer cure: Clinical implications. Eur. J. Cancer Care 2019, 28, 13139. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHOQOL: Measuring Quality of Life. Available online: https://www.who.int/healthinfo/survey/whoqol-qualityoflife/en/ (accessed on 20 April 2019).
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.J.M.; et al. The European Organisation for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Sprangers, M.A.G.; Groenvold, M.; Arraras, J.I.; Franklin, J.; te Velde, A.; Muller, M.; Franzini, L.; Williams, A.; de Haes, C.H.; Hopwood, P.; et al. The EORTC breast cancer-specific quality-of-life questionnaire module: First results from a three-country field study. J. Clin. Oncol. 1996, 14, 2756–2768. [Google Scholar] [CrossRef]
- Clinical Trials Database. EORTC. Available online: https://www.eortc.org/research_field/clinical-detail/15931/ (accessed on 20 April 2019).
- Leng, T.; Ching, S.; Idris, D.B.; Teo, L.W.; Loh, S.Y.; Seow, G.C.; Chia, Y.Y.; Tin, A.S. Validation of EORTC QLQ-C30 and QLQ-BR23 questionnaires in the measurement of quality of life of breast cancer patients in Singapore. Asia-Pac. J. Oncol. Nurs. 2014, 1, 22. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Cheung, M.W.L.; Ho, R.C.M.; Lim, Y.; Mak, A. Conducting a meta-analysis: Basics and Good Practices. Int. J. Rheum. Dis. 2012, 15, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Mak, A.; Cheung, M.W.; Fu, E.H.; Ho, R.C. Meta-analysis in medicine: An introduction. Int. J. Rheum. Dis. 2010, 13, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Ho, R.C.; Ong, H.S.; Kudva, K.G.; Cheung, M.W.; Mak, A. How to critically appraise and apply meta-analyses in clinical practice. Int. J. Rheum. Dis. 2010, 13, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Liang, E.F.; Lim, S.Z.; Tam, W.W.; Ho, C.S.; Zhang, M.W.; McIntyre, R.S.; Ho, R.C. The Effect of Methylphenidate and Atomoxetine on Heart Rate and Systolic Blood Pressure in Young People and Adults with Attention-Deficit Hyperactivity Disorder (ADHD): Systematic Review, Meta-Analysis, and Meta-Regression. Int. J. Environ. Res. Public Health 2018, 15, 1789. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Kim, S.W.; Heo, C.Y.; Kim, D.; Hwang, Y.; Yom, C.K.; Kang, E. Comparison of Quality of Life Based on Surgical Technique in Patients with Breast Cancer. Jpn. J. Clin. Oncol. 2013, 44, 22–27. [Google Scholar] [CrossRef] [Green Version]
- Acil, H.; Cavdar, I. Comparison of Quality of Life of Turkish Breast Cancer Patients Receiving Breast Conserving Surgery or Modified Radical Mastectomy. Asian Pac. J. Cancer Prev. 2014, 15, 5377–5381. [Google Scholar] [CrossRef] [Green Version]
- Lagendijk, M.; Egdom, L.V.; Richel, C.; van Leeuwen, N.; Verhoef, C.; Lingsma, H.F.; Koppert, L.B. Patient reported outcome measures in breast cancer patients. Eur. J. Surg. Oncol. 2018, 44, 963–968. [Google Scholar] [CrossRef]
- Lagendijk, M.; Egdom, L.S.E.; Vos, E.L.; Mureau, M.A.M.; van Leeuwen, N.; Hazelzet, J.A.; Lingsma, H.F.; Koppert, L.B.; Veen, F.E.E.V. Patient-Reported Outcome Measures May Add Value in Breast Cancer Surgery. Ann. Surg. Oncol. 2018, 25, 3563–3571. [Google Scholar] [CrossRef]
- Jendrian, S.; Steffens, K.; Schmalfeldt, B.; Laakmann, E.; Bergelt, C.; Witzel, I. Quality of life in patients with recurrent breast cancer after second breast-conserving therapy in comparison with mastectomy: The German experience. Breast Cancer Res. Treat. 2017, 163, 517–526. [Google Scholar] [CrossRef]
- Tsai, H.Y.; Kuo, R.N.C.; Chung, K.P. Quality of life of breast cancer survivors following breast-conserving therapy versus mastectomy: A multicenter study in Taiwan. Jpn. J. Clin. Oncol. 2017, 47, 909–918. [Google Scholar] [CrossRef] [Green Version]
- Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. Mean Variance Estimation. Available online: http://www.comp.hkbu.edu.hk/~xwan/median2mean.html (accessed on 29 May 2019).
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2016, 27, 1785–1805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arndt, V.; Stegmaier, C.; Ziegler, H.; Brenner, H. Quality of life over 5 years in women with breast cancer after breast-conserving therapy versus mastectomy: A population-based study. J. Cancer Res. Clin. Oncol. 2008, 134, 1311–1318. [Google Scholar] [CrossRef] [PubMed]
- Kiebert, G.M.; Haes, J.C.; Velde, C.J. The impact of breast-conserving treatment and mastectomy on the quality of life of early-stage breast cancer patients: A review. J. Clin. Oncol. 2008, 9, 1059–1070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganz, P.A.; Schag, C.C.; Lee, J.J.; Polinsky, M.L.; Tan, S. Breast conservation versus mastectomy. Is there a difference in psychological adjustment or quality of life in the year after surgery? Cancer 1992, 69, 1729–1738. [Google Scholar] [CrossRef] [Green Version]
- Ghodusi, M.; Heidari, M. The relationship between body esteem and hope and mental health in breast cancer patients after mastectomy. Indian J. Palliat. Care 2015, 21, 198. [Google Scholar] [CrossRef] [PubMed]
- Fisher, B.; Anderson, S.; Bryant, J.; Margolese, R.G.; Deutsch, M.; Fisher, E.R.; Wolmark, N. Twenty-Year Follow-up of a Randomized Trial Comparing Total Mastectomy, Lumpectomy, and Lumpectomy plus Irradiation for the Treatment of Invasive Breast Cancer. N. Engl. J. Med. 2002, 347, 1233–1241. [Google Scholar] [CrossRef] [Green Version]
- Veronesi, U.; Cascinelli, N.; Mariani, L.; Greco, M.; Saccozzi, R.; Luini, A.; Marubini, E. Twenty-Year Follow-up of a Randomized Study Comparing Breast-Conserving Surgery with Radical Mastectomy for Early Breast Cancer. N. Engl. J. Med. 2002, 347, 1227–1232. [Google Scholar] [CrossRef]
- Jeffe, D.B.; Pérez, M.; Cole, E.F.; Liu, Y.; Schootman, M. The Effects of Surgery Type and Chemotherapy on Early-Stage Breast Cancer Patients’ Quality of Life Over 2-Year Follow-up. Ann. Surg. Oncol. 2015, 23, 735–743. [Google Scholar] [CrossRef] [Green Version]
- Nowicki, A.; Licznerska, B.; Rhone, P. Evaluation of the quality of life of women treated due to breast cancer using amputation or breast conserving surgery in the early postoperative period. Pol. J. Surg. 2015, 87, 174–180. [Google Scholar] [CrossRef] [Green Version]
- Cortés-Flores, A.O.; Vargas-Meza, A.; Morgan-Villela, G.; Jiménez-Tornero, J.; Valle, C.J.; Solano-Genesta, M.; González-Ojeda, A. Sexuality Among Women Treated for Breast Cancer: A Survey of Three Surgical Procedures. Aesthetic Plast. Surg. 2017, 41, 1275–1279. [Google Scholar] [CrossRef]
- Shahhosseini, Z.; Gardeshi, Z.; Pourasghar, M.; Salehi, F. A Review of Affecting Factors on Sexual Satisfaction in Women. Mater. Socio Med. 2014, 26, 378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spivey, T.L.; Gutowski, E.D.; Zinboonyahgoon, N.; King, T.A.; Dominici, L.; Edwards, R.R.; Schreiber, K.L. Chronic Pain After Breast Surgery: A Prospective, Observational Study. Ann. Surg. Oncol. 2018, 25, 2917–2924. [Google Scholar] [CrossRef] [PubMed]
- Freitas-Silva, R.; Conde, D.M.; Freitas-Júnior, R.D.; Martinez, E.Z. Comparison of quality of life, satisfaction with surgery and shoulder-arm morbidity in breast cancer survivors submitted to breast-conserving therapy or mastectomy followed by immediate breast reconstruction. Clinics 2010, 65, 781–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sprangers, M.A.; Groenvold, M.; Arraras, J.I. The European Organization for Research and Treatment of. Cancer breast cancer-specific quality-of-life questionnaire module: First results from a three-country field study. J. Clin. Oncol. 1996, 14, 2756–2768. [Google Scholar] [CrossRef] [PubMed]
- Sprangers, M.A.G.; Groenvold, M.; Veldete, A. The Construction of a Breast Cancer Module; Internal Report of the EORTC Study Group on Quality of Life: Edinburgh, UK, 1992. [Google Scholar]
- Groenvold, M. Quality of Life in Breast Cancer Adjuvant Therapy: What Should be Measured? Content Validation of a Questionnaire Using Qualitative Interviews. Presented at the 6th European Conference on Clinical Oncology and Cancer Nursing, Florence, Italy, 27–31 October 1991. [Google Scholar]
- Zawisza, K.; Tobiasz-Adamczyk, B.; Nowak, W.; Kulig, J.; Jedrys, J. Validity and reliability of the quality of life questionnaire (EORTC QLQ C30) and its breast cancer module (EORTC QLQ BR23). Ginekol. Pol. 2010, 81, 262–267. [Google Scholar] [PubMed]
- Agnieszka, J.; Słowik Marcin, J.; Jabłoński Anna, M.; Michałowska-Kaczmarczyk, A.M.; Jach, R. Evaluation of quality of life in women with breast cancer, with particular emphasis on sexual satisfaction, future perspectives and body image, depending on the method of surgery. Psychiatr. Pol. 2017, 56, 1–18. [Google Scholar] [CrossRef]
- Golubnitschaja, O.; Polivka, J.; Yeghiazaryan, K., Jr.; Berliner, L. Liquid biopsy and multiparametric analysis in management of liver malignancies: New concepts of the patient stratification and prognostic approach. EPMA J. 2018, 9, 271–285. [Google Scholar] [CrossRef]
- Zubor, P.; Kubatka, P.; Kajo, K.; Dankova, Z.; Polacek, H.; Bielik, T.; Kudela, E.; Samec, M.; Liskova, A.; Vlcakova, D.; et al. Why the Gold Standard Approach by Mammography Demands Extension by Multiomics? Application of Liquid Biopsy miRNA Profiles to Breast Cancer Disease Management. Int. J. Mol. Sci. 2019, 20, 2878. [Google Scholar] [CrossRef] [Green Version]
- Fröhlich, H.; Patjoshi, S.; Yeghiazaryan, K.; Kehrer, C.; Kuhn, W.; Golubnitschaja, O. Premenopausal breast cancer: Potential clinical utility of a multi-omics based machine learning approach for patient stratification. EPMA J. 2018, 9, 175–186. [Google Scholar] [CrossRef]
- Polivka, J.; Altun, I., Jr.; Golubnitschaja, O. Pregnancy-associated breast cancer: The risky status quo and new concepts of predictive medicine. EPMA J. 2018, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Bubnov, R.; Polivka, J.; Zubor, P., Jr.; Konieczka, K.; Golubnitschaja, O. “Pre-metastatic niches” in breast cancer: Are they created by or prior to the tumour onset? Flammer Syndrome" relevance to address the question. EPMA J. 2017, 8, 141–157. [Google Scholar] [CrossRef] [PubMed]

| Study | Year | Country | Total n | Age, Mean ± SD (Range) | Mean Time from Surgery to Survey (Range) |
|---|---|---|---|---|---|
| Sun [17] | 2013 | Korea | 376 | 51.6 (28–70) | 4.08 (2–8.67) years |
| Acil [18] | 2014 | Turkey | 100 | 51.83 ± 9.26 (34–76) | NA |
| Lagendijk (a) [19] | 2018 | Netherlands | 385 | 54.93 ± 8.77 a | 5 a years |
| Lagendijk (b) [20] | 2018 | Netherlands | 419 | 51.35 ± 12.65 a | 6.34 a years |
| Jendrian [21] | 2017 | Germany | 107 | 67.33 ± 9.40 a (36.4–83.8) | 4.44 a (0.2–16) years |
| Tsai [22] | 2017 | Taiwan | 544 | 52.8 ± 9.4 | NA |
| Predictor | No. of Studies Used | Univariate Coefficient | Z-Value | p-Value | Estimated Tau2 |
|---|---|---|---|---|---|
| Mean age | 6 | −0.128 | −1.14 | 0.253 | 2.38 |
| Mean time since surgery (years) | 4 | −2.23 | −1.49 | 0.136 | 6.57 |
| Predictor | No. of Studies Used | Univariate Coefficient | Z-Value | p-Value | Estimated Tau2 |
|---|---|---|---|---|---|
| Mean age | 4 | 0.0348 | 0.760 | 0.448 | 0.334 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, E.T.; Ang, R.Z.; Tran, B.X.; Ho, C.S.; Zhang, Z.; Tan, W.; Bai, Y.; Zhang, M.; Tam, W.W.; Ho, R.C. Comparing Quality of Life in Breast Cancer Patients Who Underwent Mastectomy Versus Breast-Conserving Surgery: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4970. https://doi.org/10.3390/ijerph16244970
Ng ET, Ang RZ, Tran BX, Ho CS, Zhang Z, Tan W, Bai Y, Zhang M, Tam WW, Ho RC. Comparing Quality of Life in Breast Cancer Patients Who Underwent Mastectomy Versus Breast-Conserving Surgery: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2019; 16(24):4970. https://doi.org/10.3390/ijerph16244970
Chicago/Turabian StyleNg, Elvin T., Russell Z. Ang, Bach X. Tran, Cyrus S. Ho, Zhisong Zhang, Wanqiu Tan, Yu Bai, Min Zhang, Wilson W. Tam, and Roger C. Ho. 2019. "Comparing Quality of Life in Breast Cancer Patients Who Underwent Mastectomy Versus Breast-Conserving Surgery: A Meta-Analysis" International Journal of Environmental Research and Public Health 16, no. 24: 4970. https://doi.org/10.3390/ijerph16244970
APA StyleNg, E. T., Ang, R. Z., Tran, B. X., Ho, C. S., Zhang, Z., Tan, W., Bai, Y., Zhang, M., Tam, W. W., & Ho, R. C. (2019). Comparing Quality of Life in Breast Cancer Patients Who Underwent Mastectomy Versus Breast-Conserving Surgery: A Meta-Analysis. International Journal of Environmental Research and Public Health, 16(24), 4970. https://doi.org/10.3390/ijerph16244970






