Effect of a School-Based Anxiety Prevention Program among Primary School Children
Abstract
1. Introduction
2. Materials and Methods
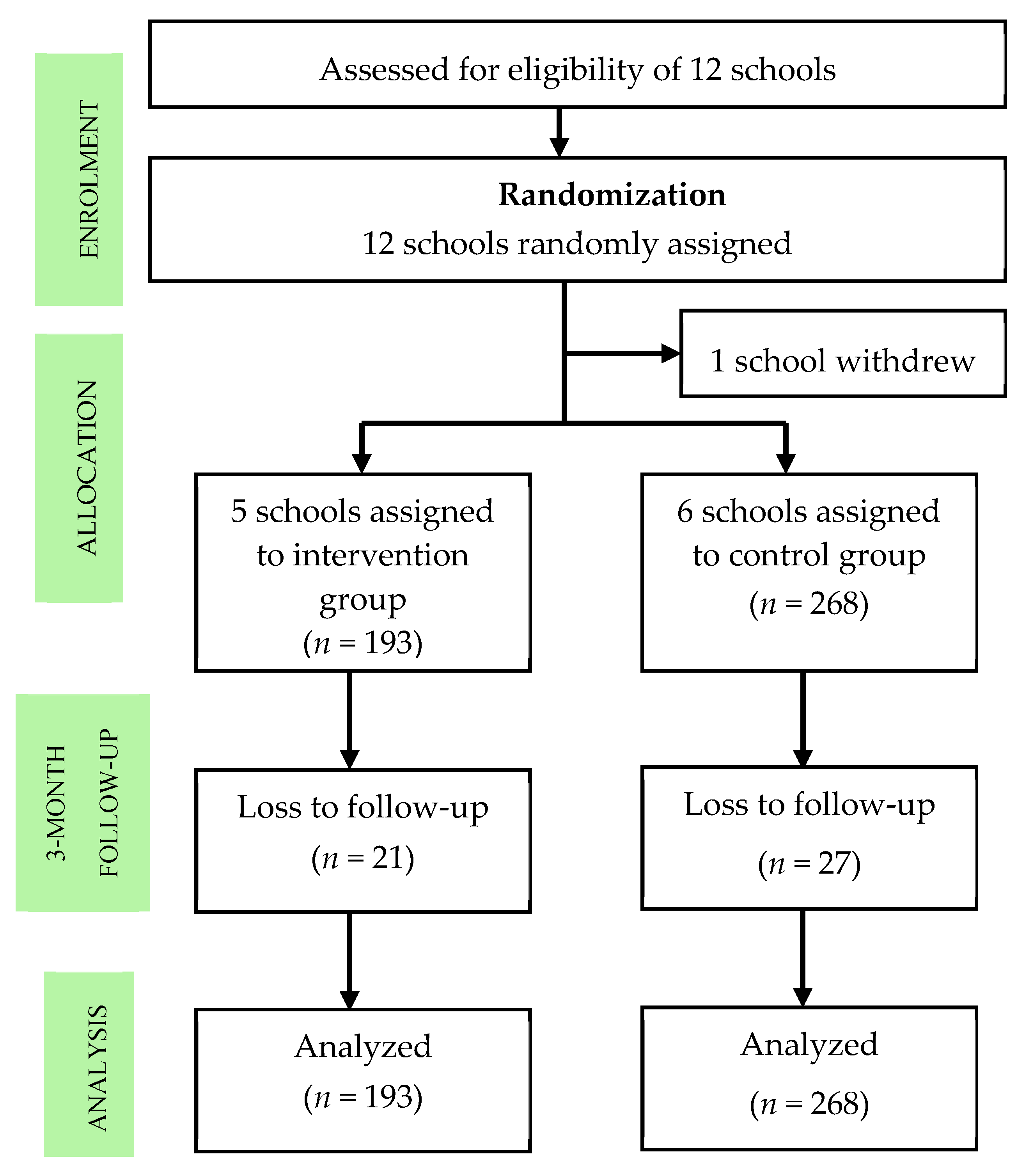
2.1. Study Design and Participants
2.2. Randomization and Masking
2.3. Intervention
2.4. Procedures
2.5. Measures
2.6. Data Analysis
2.7. Ethical Approval
3. Results
3.1. Participant Characteristics
3.2. Intervention Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yang, X.; Jiang, C.; Pan, W.; Xu, W.; Liang, F.; Li, N.; Mu, H.; Na, J.; Lv, M.; An, X.; et al. Prevalence of psychiatric disorders among children and adolescents in northeast China. PLoS ONE 2014, 9, e111223. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Study-Adolescent Supplement (NCS-A). J. Am. Acad. Child. Adolesc. Psychiatry 2011, 49, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Bittner, A.; Egger, H.L.; Erkanli, A.; Jane Costello, E.; Foley, D.L.; Angold, A. What do childhood anxiety disorders predict? J. Child Psychol. Psychiatry Allied Discip. 2007, 48, 1174–1183. [Google Scholar] [CrossRef] [PubMed]
- Essau, C.A.; Lewinsohn, P.M.; Olaya, B.; Seeley, J.R. Anxiety disorders in adolescents and psychosocial outcomes at age 30. J. Affect. Disord. 2014, 163, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.B.; Stein, D.J. Social Anxiety Disorder. Lancet 2008, 371, 1115–1125. [Google Scholar] [CrossRef]
- Bolton, J.M.; Cox, B.J.; Afifi, T.O.; Enns, M.W.; Bienvenu, O.J.; Sareen, J. Anxiety disorders and risk for suicide attempts: Findings from the Baltimore epidemiologic catchment area follow-up study. Depress. Anxiety 2008, 25, 477–481. [Google Scholar] [CrossRef]
- O’Neil Rodriguez, K.A.; Kendall, P.C. Suicidal ideation in anxiety-disordered youth: Identifying predictors of risk. J. Clin. Child Adolesc. Psychol. 2014, 43, 51–62. [Google Scholar] [CrossRef]
- Wolk, C.B.; Kendall, P.C.; Beidas, R.S. Cognitive-behavioral therapy for child anxiety confers long-term protection from suicidality. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 175–179. [Google Scholar] [CrossRef]
- James, A.C.; James, G.; Cowdrey, F.A.; Soler, A.; Choke, A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst. Rev. 2013, 6, CD004690. [Google Scholar]
- Kieling, C.; Baker-Henningham, H.; Belfer, M.; Conti, G.; Ertem, I.; Omigbodun, O.; Rahman, A. Child and adolescent mental health worldwide: Evidence for action. Lancet 2011, 378, 1515–1525. [Google Scholar] [CrossRef]
- Chavira, D.A.; Stein, M.B.; Bailey, K.; Stein, M.T. Child anxiety in primary care: Prevalent but untreated. Depress. Anxiety 2004, 20, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Moskos, M.A.; Olson, L.; Halbern, S.R. Utah youth suicide study: Barriers to mental health treatment for adolescents. Suicide Life-Threat. Behav. 2007, 37, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F.; Wright, A.; Morgan, A.J. Where to seek help for a mental disorder? National survey of the beliefs of Australian youth and their parents. Med. J. Aust. 2007, 187, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Barrett, P.M.; Pahl, K.M. School-based intervention: Examining a universal approach to anxiety management. Aust. J. Guid. Couns. 2006, 16, 55–75. [Google Scholar] [CrossRef]
- Mrazek, P.; Haggerty, R. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research; National Academy Press: Washington, DC, USA, 1994. [Google Scholar]
- Horowitz, J.; Garber, J.; Ciesla, J.; Young, J.; Mufson, L. Prevention of depressive symptoms in adolescents: A randomized trial of cognitive-behavioral and interpersonal prevention programs. J. Consult. Clin. Psychol. 2007, 75, 693–706. [Google Scholar] [CrossRef]
- Huggins, L.; Davis, M.C.; Rooney, R.; Kane, R. Socially prescribed and self-oriented perfectionism as predictors of depressive diagnosis in preadolescents. J. Psychol. Couns. Sch. 2008, 18, 182–194. [Google Scholar] [CrossRef]
- Diep, C.; Chen, T.; Davies, V.; Baranowski, J.; Baranowski, T. Influence of behavioral theory on fruit and vegetable intervention effectiveness among children: A meta-analysis. J. Nutr. Educ. Behav. 2014, 46, 506–546. [Google Scholar] [CrossRef]
- Watson, J. Behaviorism; Norton: New York, NY, USA, 1925. [Google Scholar]
- Lewin, K. The Nature of Field Theory. In Psychological Theory, Contemporary Readings; Mark, M.H., Ed.; Macmillan: New York, NY, USA, 1951. [Google Scholar]
- Skinner, B. The Behaviour of Organisms; Appleton-Century-Crofts: Englewood Cliffs, NJ, USA, 1938. [Google Scholar]
- Neil, A.; Christensen, H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin. Psychol. Rev. 2009, 29, 208–215. [Google Scholar] [CrossRef]
- Stallard, P. Think Good-Feel Good: A Cognitive Behaviour Therapy Workbook for Children and Young Children; John Wiley & Sons: Hoboken, NJ, USA, 2002. [Google Scholar]
- Piaget, J. The Psychology of Intelligence; Littlefield: Totowa, NJ, USA, 1972. [Google Scholar]
- Southam-Gerow, M.A. Emotion Regulation in Children and Adolescents: A Practitioner’s Guide; The Guilford Press: New York, NY, USA; London, UK, 2013. [Google Scholar]
- Suveg, C.; Zeman, J. Emotion regulation in children with anxiety disorders. J. Clin. Child Adolesc. Psychol. 2004, 33, 750–759. [Google Scholar] [CrossRef]
- Suveg, C.; Kendall, P.C.; Comer, J.S.; Robin, J. Emotion-focused cognitive-behavioral therapy for anxious youth: A multiple-baseline evaluation. J. Contemp. Psychother. 2006, 36, 77–85. [Google Scholar] [CrossRef]
- Rooney, R.; Morrison, D.; Hassan, S.; Kane, R.; Roberts, C.; Mancini, V. Prevention of internalizing disorders in 9–10 year old children: Efficacy of the Aussie optimism positive thinking skills program at 30-month follow-up. Front. Psychol. 2013, 4, 1–10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johnstone, J.; Rooney, R.; Hassan, S.; Kane, R. Prevention of depression and anxiety symptoms in adolescents: 42 and 54 months follow-up of the Aussie optimism program-positive thinking skills. Front. Psychol. 2014, 5, 364. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Fisher, W. Changing AIDS-risk behavior. Psychol. Bull. 1992, 111, 455–474. [Google Scholar] [CrossRef] [PubMed]
- Maideen, S.F.K.; Mohd-Sidik, S.; Rampal, L.; Mukhtar, F.; Ibrahim, N.; Phang, C.K.; Tan, K.A.; Ahmad, R. A web-based psychoeducational intervention program for depression and anxiety in an adult community in Selangor, Malaysia: Protocol of a randomized controlled trial. JMIR Res. Protoc. 2016, 5, e112. [Google Scholar] [CrossRef]
- Aday, L.; Cornelius, L.J. Designing and Conducting Health Surveys: A Comprehensive Guide, 3rd ed.; Jossey-Bass: San Francisco, CA, USA, 2006. [Google Scholar]
- Ebesutani, C.; Reise, S.P.; Chorpita, B.F.; Ale, C.; Regan, J.; Young, J.; Higa-McMillan, C. The revised child and depression scale-short version: Scale reduction via exploratory bifactor modeling of the broad anxiety factor. Psychol. Assess. 2012, 24, 833–845. [Google Scholar] [CrossRef]
- Zeman, J.L.; Cassano, M.; Suveg, C.; Shipman, K. Initial validation of the Children’s Worry Management Scale. J. Child Fam. Stud. 2010, 19, 381–392. [Google Scholar] [CrossRef]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Barrett, P.M.; Lock, S.; Farrell, L.J. Developmental differences in universal preventive intervention for child anxiety. Clin. Child Psychol. Psychiatry 2005, 10, 539–555. [Google Scholar] [CrossRef]
- Essau, C.; Conradt, J.; Sasagawa, S.; Ollendick, T. Prevention of anxiety symptoms in children: Results from a universal school-based trial. Behav. Ther. 2012, 43, 450–464. [Google Scholar] [CrossRef]
- Stallard, P.; Skryabina, E.; Taylor, G.; Phillips, R.; Daniels, H.; Anderson, R.; Simpson, N. Classroom-based cognitive behaviour therapy (FRIENDS): A cluster randomised controlled trial to Prevent Anxiety in Children through Education in Schools (PACES). Lancet Psychiatry 2014, 1, 185–192. [Google Scholar] [CrossRef]
- Stopa, J.E.; Barrett, P.M.; Golingi, F. The prevention of childhood anxiety in socioeconomically disadvantaged communities: A universal school-based trial. Adv. Sch. Ment. Health Promot. 2010, 3, 5–24. [Google Scholar] [CrossRef]
- Miller, L.; Lave-Gindhu, A.; Bennett, J.; Liu, Y.; Gold, S.; March, J.; Olson, B.F.; Weachtler, V. An effectiveness study of a culturally enriched school-based CBT anxiety prevention program. J. Clin. Child Adolesc. Psychol. 2011, 40, 618–629. [Google Scholar] [CrossRef]
- Manassis, K.; Wilansky-Traynor, P.; Farzan, N.; Kleiman, V.; Parker, K.; Sanford, M. The Feelings Club: Randomized controlled evaluation of school-based CBT for anxious or depressive symptoms. Depress. Anxiety 2010, 27, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Uroa, Y.; Yoshinaga, N.; Asano, K.; Ishikawa, R.; Tano, A.; Sato, Y.; Shimizu, E. Effectiveness of a cognitive behavioural therapy-based anxiety prevention programme for children: A preliminary quasi-experimental study in Japan. Child Adolesc. Psychiatry Ment. Health 2016, 10. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for Behavioural Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Teubert, D.; Pinquart, M. A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. J. Anxiety Disord. 2011, 25, 1046–1059. [Google Scholar]
- Fisak, B.; Richard, D.; Mann, A. The prevention of child and adolescent anxiety: A meta-analytic review. Prev. Sci. 2011, 12, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Ahlen, J.; Lenhard, F.; Ghaderi, A. Universal prevention for anxiety and depressive symptoms in children: A meta-analysis of randomized and cluster-randomized trials. J. Prim. Prev. 2015, 36, 387–403. [Google Scholar] [CrossRef] [PubMed]
- Werner-seidler, A.; Perry, Y.; Calear, A.L.; Newby, J.M.; Christensen, H. School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clin. Psychol. Rev. 2017, 51, 30–47. [Google Scholar] [CrossRef]
- Waldron, S.; Stallard, P.; Grist, R.; Hamilton-Giachritsis, C. The “long-term” effects of universal school-based anxiety prevention trials: A systematic review. Ment. Health Prev. 2018, 11, 8–15. [Google Scholar] [CrossRef]
- Bouchard, S.; Gagnier, N.; Loranger, C. Evaluation of a primary prevention program for anxiety disorders using story books with children aged 9-12 years. J. Prim. Prev. 2013, 34, 345–358. [Google Scholar] [CrossRef]
- Suveg, C.; Jones, A.; Jacob, M.; Morelen, D.; Thomassin, K.; Whitehead, M. Emotion-focused cognitive-behavioral therapy for youth with anxiety disorders: A randomized trial. J. Abnorm. Child Psychol. 2018, 46, 569–580. [Google Scholar] [CrossRef]
| Variables | Intervention (n = 193) | Control (n = 268) | p-Value |
|---|---|---|---|
| Age: n (%) | |||
| 10 | 98 (50.8) | 135 (50.4) | 0.932 a |
| 11 | 95 (49.2) | 133 (49.6) | |
| Gender: n (%) | |||
| Male | 77 (39.9) | 126 (47.0) | 0.129 a |
| Female | 116 (60.1) | 142 (53.0) | |
| Ethnicity: n (%) | |||
| Malay | 192 (99.5) | 268 (100.0) | 0.238 a |
| Non-Malay | 1 (0.5) | 0 (0.0) | |
| Anxiety score: Mean (SD) | 14.14 (6.194) | 15.06 (6.948) | 0.156 b |
| Worry coping skills score: Mean (SD) | 5.35 (1.409) | 5.54 (1.518) | 0.174 b |
| Self-esteem score: Mean (SD) | 37.43 (5.724) | 36.46 (6.127) | 0.089 b |
| Outcome Variable | Intervention | Control | ||||
|---|---|---|---|---|---|---|
| Baseline Mean (SD) | Immediately after Intervention Mean (SD) | 3 Months after Intervention Mean (SD) | Baseline Mean (SD) | Immediately after Intervention Mean (SD) | 3 Months after Intervention Mean (SD) | |
| Anxiety score | 14.14 (6.194) | 14.10 (6.421) | 12.95 (7.088) | 15.06 (6.948) | 15.14 (6.325) | 13.87 (7.178) |
| Worry coping skills score | 5.35 (1.409) | 5.28 (1.434) | 5.26 (1.382) | 5.54 (1.518) | 5.58 (1.487) | 5.50 (1.443) |
| Self-esteem score | 37.43 (5.724) | 36.41 (6.638) | 36.71 (7.106) | 36.46 (6.127) | 36.68 (6.710) | 35.52 (6.834) |
| Outcome Variable | Parameter | F | df1 | df2 | p-Value | Effect Size (Cohen’s d) |
|---|---|---|---|---|---|---|
| Anxiety score | Group | 1.213 | 1 | 1097 | 0.271 | |
| Group × time | 5.856 | 4 | 1097 | 0.001 * | 0.1026 | |
| Worry coping skills score | Group | 2.563 | 1 | 1098 | 0.110 | |
| Group × time | 0.484 | 4 | 1098 | 0.748 | ||
| Self-esteem score | Group | 0.058 | 1 | 1075 | 0.810 | |
| Group × time | 1.914 | 4 | 1075 | 0.106 |
| Outcome Variable | Parameter | F | df1 | df2 | p-Value | Effect Size (Cohen’s d) |
|---|---|---|---|---|---|---|
| Anxiety score | Group | 0.030 | 1 | 53 | 0.898 | |
| Group × time | 6.760 | 4 | 53 | 0.001 * | 0.3999 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ab Ghaffar, S.F.; Mohd Sidik, S.; Ibrahim, N.; Awang, H.; Gyanchand Rampal, L.R. Effect of a School-Based Anxiety Prevention Program among Primary School Children. Int. J. Environ. Res. Public Health 2019, 16, 4913. https://doi.org/10.3390/ijerph16244913
Ab Ghaffar SF, Mohd Sidik S, Ibrahim N, Awang H, Gyanchand Rampal LR. Effect of a School-Based Anxiety Prevention Program among Primary School Children. International Journal of Environmental Research and Public Health. 2019; 16(24):4913. https://doi.org/10.3390/ijerph16244913
Chicago/Turabian StyleAb Ghaffar, Siti Fatimah, Sherina Mohd Sidik, Normala Ibrahim, Hamidin Awang, and Lekhraj Rampal Gyanchand Rampal. 2019. "Effect of a School-Based Anxiety Prevention Program among Primary School Children" International Journal of Environmental Research and Public Health 16, no. 24: 4913. https://doi.org/10.3390/ijerph16244913
APA StyleAb Ghaffar, S. F., Mohd Sidik, S., Ibrahim, N., Awang, H., & Gyanchand Rampal, L. R. (2019). Effect of a School-Based Anxiety Prevention Program among Primary School Children. International Journal of Environmental Research and Public Health, 16(24), 4913. https://doi.org/10.3390/ijerph16244913





