Controversies in the Science of Sedentary Behaviour and Health: Insights, Perspectives and Future Directions from the 2018 Queensland Sedentary Behaviour Think Tank
Abstract
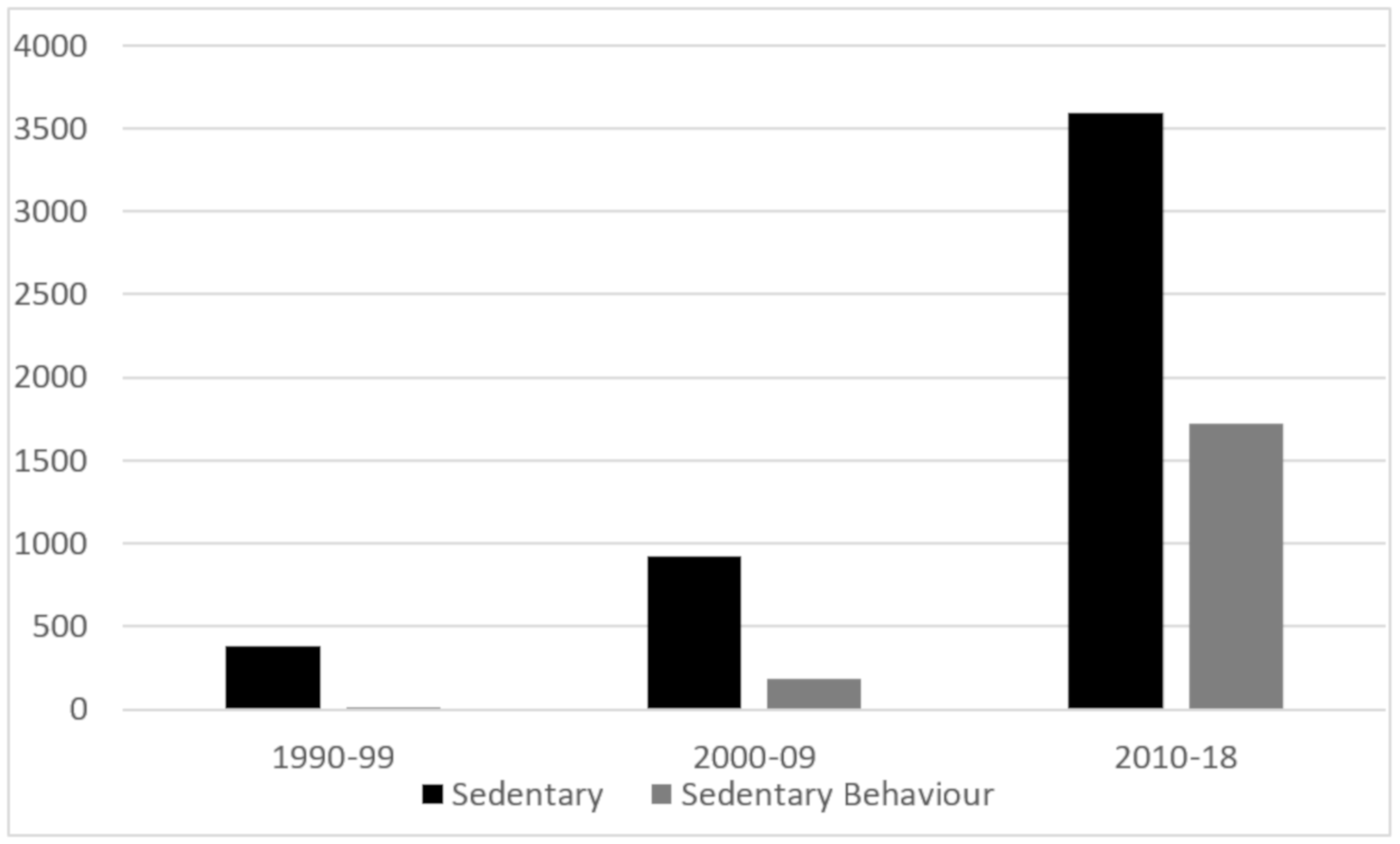
1. Introduction
2. Methods
2.1. Participants
2.2. Procedures
2.2.1. Stimulus Presentations
2.2.2. Topic-Focussed Discussions
- Sedentary behaviour has been shown to have differential effects on some health outcomes. For example, vascular and metabolic outcomes may show stronger effects than weight loss or mood and may vary by initial health status. However, despite being a comparatively weaker, albeit opposing, physiological stimulus (vs. moderate-vigorous physical activity), sedentary behaviour is often undertaken for long periods and is highly prevalent in many population groups. Regular exercise has clear effects on multiple aspects of health (i.e., can be a strong stimulus) but is undertaken for short periods and has low population prevalence.
- The behaviour itself—sedentary behaviour—is commonly assessed through self-reported methods or with wearable technology. Measures typical in the research literature include total sedentary time or time spent in individual domains of behaviour or settings, such as screen-viewing time or sitting at work.
- Assessment of health-related outcomes have included mortality, incident chronic disease (e.g., colon cancer, type II diabetes), cardio-metabolic biomarkers, adiposity, musculo-skeletal integrity, physical fitness, physical function, mental health and behavioural outcomes (e.g., work engagement).
- Combining all the above factors makes the area complex, and one should not necessarily expect simple or single answers or solutions.
3. Results
3.1. Topic 1: Is Standing a Sufficient Stimulus to Mitigate the Detrimental Health Effects of Prolonged Sitting?
3.1.1. Review-Level Evidence
3.1.2. Prospective Evidence
3.1.3. Isotemporal Substitution
3.1.4. Experimental Evidence
3.1.5. Sit-to-Stand Workstations
3.1.6. Research Summary
3.1.7. Think Tank Discussion
- Measurement of standing.
- Evidence to inform messages on standing.
- Key future research directions.
3.2. Topic 2: Are there Beneficial Effects for Breaking up Sedentary Time?
3.2.1. Observational and Isotemporal Substitution Studies
3.2.2. Experimental and Review-Level Evidence
3.2.3. Research Summary
3.2.4. Think Tank Discussion
- Frequency of breaks from sitting.
- Informing messages about breaks in sitting.
- Future research directions.
3.3. Topic 3: Does Moderate-to-Vigorous Physical Activity Attenuate the Adverse Health Effects of Sitting?
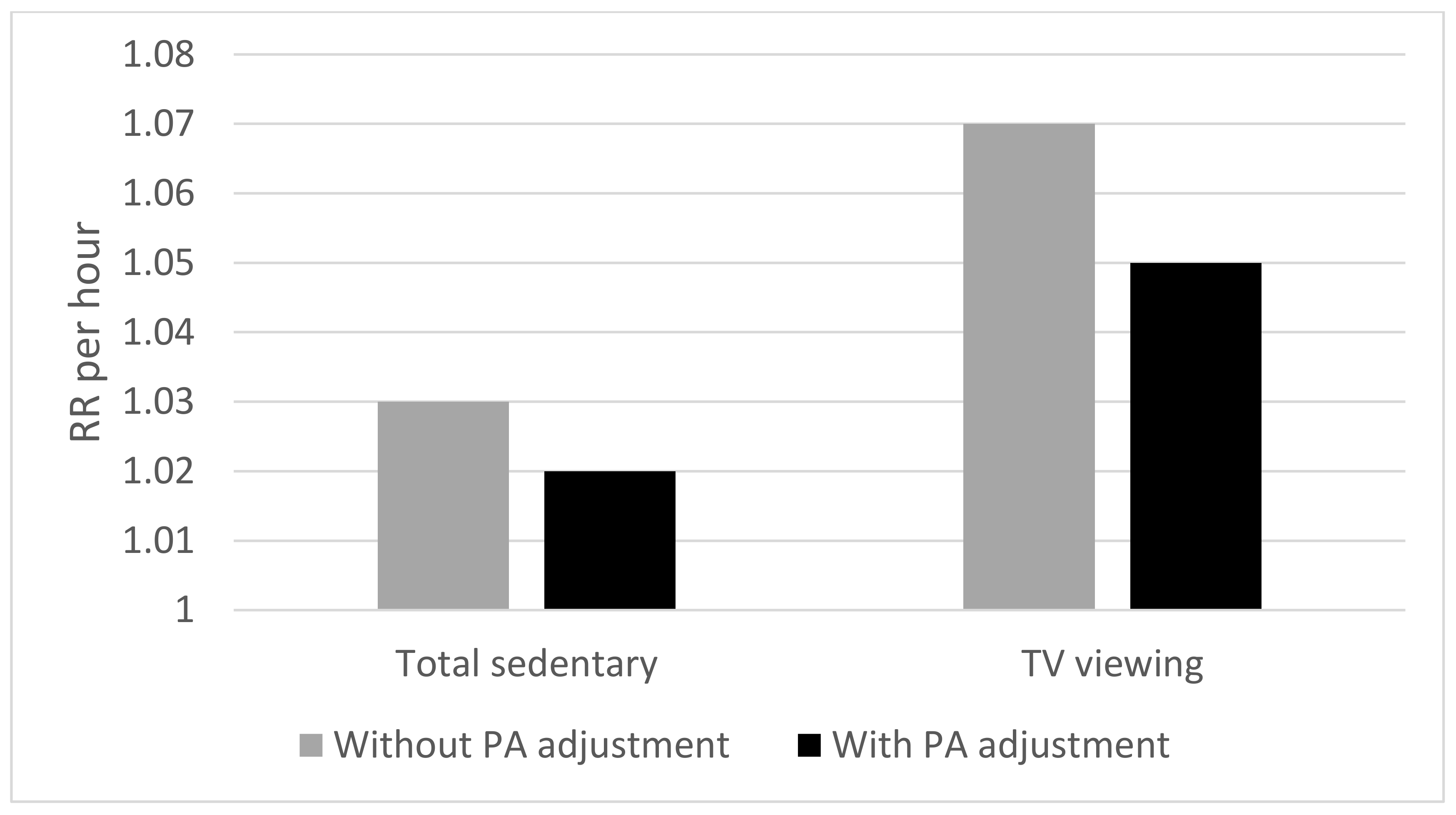
3.3.1. Effects of Sitting or Sedentary Behaviour after Adjusting for the Effects of Physical Activity
3.3.2. Moderation Effects of MVPA on Sedentary Behaviour and Health Relationships
3.3.3. Research Summary
3.3.4. Think Tank Discussion
- Methodological issues.
- Messaging concerning the role of MVPA in the health effects of sitting.
- Future research directions.
4. Conclusions and Recommendations
- Standing is important. Benefits may accrue from postural shifts and these include metabolic and cardiovascular adaptations with considerable health benefits and may or may not be related to energy expenditure.
- Prolonged (mainly static) standing and prolonged sitting are both bad for health.
- Postural transitions are vital—‘the best posture is the next posture’; regularly breaking up sitting time and replacing this with postural shifts and movement is important.
- Many health effects of sitting are evident even after controlling for levels of MVPA, but those undertaking high levels of MVPA are likely to have marked attenuation of deleterious effects of high levels of or prolonged sitting.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN): Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.H.; Valoski, A.M.; Vara, L.S.; McCurley, J.; Wisniewski, L.; Kalarchian, M.A.; Klein, K.R.; Shrager, L.R. Effects of decreasing sedentary behavior and increasing activity on weight change in obese children. Health Psychol. 1995, 14, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Leslie, E.; Salmon, J.; Fotheringham, M.J. Environmental determinants of physical activity and sedentary behavior. Exerc. Sport Sci. Rev. 2000, 28, 153–158. [Google Scholar] [PubMed]
- Salmon, J.; Bauman, A.; Crawford, D.; Timperio, A.; Owen, N. The association between television viewing and overweight among Australian adults participating in varying levels of leisure-time physical activity. Int. J. Obes. 2000, 24, 600–606. [Google Scholar] [CrossRef]
- Green, R.A.; Briggs, C.A. Effect of overuse injury and the importance of training on the use of adjustable workstation by keyboard operators. J. Occup. Med. 1989, 31, 557–561. [Google Scholar] [CrossRef]
- Shea, J.B.; Baute, K.J. Ergonomics of redesigning sitting. In Sedentary Behavior and Health: Concepts, Assessment, and Interventions; Zhu, W., Owen, N., Eds.; Human Kinetics: Champaign, IL, USA, 2017; pp. 321–331. [Google Scholar]
- Hughes, R.J.; Hopkins, R.J.; Hill, S.; Weatherall, M.; Van de Water, N.; Nowitz, M.; Milne, D.; Ayling, J.; Wisher, M.; Beasley, R. Frequency of venous thromboembolism in low to moderate risk long distance air travellers: The New Zealand Air Traveller’s Thrombosis (NZATT) study. Lancet 2003, 362, 2039–2044. [Google Scholar] [CrossRef]
- Kuipers, S.; Cannegieter, S.C.; Middeldorp, S.; Robyn, L.; Büller, H.R.; Rosendaal, F.R. The absolute risk of venous thrombosis after air travel: A cohort study of 8755 employees of international organisations. PLoS Med. 2007, 4, e290. [Google Scholar] [CrossRef]
- Dietz, W.H.; Gortmaker, S.L. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics 1985, 75, 807–812. [Google Scholar]
- Morris, J.N.; Heady, J.A.; Raffle, P.A.B.; Roberts, C.G.; Parks, J.W. Coronary heart disease and physical activity of work. Lancet 1953, 262, 1053–1057, 111–120. [Google Scholar] [CrossRef]
- Church, T.S.; Thomas, D.M.; Tudor-Locke, C.; Katzmarzyk, P.T.; Earnest, C.P.; Rodarte, R.Q.; Martin, C.K.; Blair, S.N.; Bouchard, C. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE 2011, 6, e19657. [Google Scholar] [CrossRef]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.K.; Sugiyama, T.; Healy, G.N.; Salmon, J.; Dunstan, D.W.; Owen, N. Validity and reliability of measures of television viewing time and other non-occupational sedentary behaviour of adults: A review. Obes. Rev. 2009, 10, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Marshall, A.L.; Miller, Y.D.; Burton, N.W.; Brown, W.J. Measuring total and domain-specific sitting: A study of reliability and validity. Med. Sci. Sports Exerc. 2010, 42, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Lynch, B.M.; Friedenreich, C.M.; Khandwala, F.; Liu, A.; Nicholas, J.; Csizmadi, I. Development and testing of a past year measure of sedentary behavior: The SIT-Q. BMC Public Health 2014, 14, 899. [Google Scholar] [CrossRef] [PubMed]
- Chau, J.Y.; Van der Ploeg, H.P.; Dunn, S.; Kurko, J.; Bauman, A.E. Validity of the occupational sitting and physical activity questionnaire. Med. Sci. Sports Exerc. 2012, 44, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Atkin, A.J.; Gorely, T.; Clemes, S.A.; Yates, T.; Edwardson, C.; Brage, S.; Salmon, J.; Marshall, S.J.; Biddle, S.J. Methods of measurement in epidemiology: Sedentary behaviour. Int. J. Epidemiol. 2012, 41, 1460–1471. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Church, T.S.; Craig, C.L.; Bouchard, C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med. Sci. Sports. Exerc. 2009, 41, 998–1005. [Google Scholar] [CrossRef]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Kunthi, K.; Yates, T.; Biddle, S.J. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily sitting time and all-cause mortality: A meta-analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef]
- Henson, J.; Davies, M.J.; Bodicoat, D.H.; Edwardson, C.L.; Gill, J.M.; Stensel, D.J.; Tolfrey, K.; Dunstan, D.W.; Khunti, K.; Yates, T. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: A randomized acute study. Diabetes Care 2016, 39, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Owen, N.; Yates, T.E.; Kingwell, B.A.; Dunstan, D.W. Sitting less and moving more: Improved glycaemic control for type 2 diabetes prevention and management. Curr. Diab. Rep. 2016, 16, 114. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; U.S. Department of Health and Human Services: Washington, DC, USA, 2018. [Google Scholar]
- Owen, N.; Sugiyama, T.; Eakin, E.E.; Gardiner, P.A.; Tremblay, M.S.; Sallis, J.F. Adults’ sedentary behavior: Determinants and interventions. Am. J. Prev. Med. 2011, 41, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Pronk, N.P.; Katz, A.S.; Lowry, M.; Payfer, J.R. Reducing occupational sitting time and improving worker health: The Take-a-Stand Project, 2011. Prev. Chronic Dis. 2012, 9, 110323. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Goode, A.; Schultz, D.; Lee, D.; Leahy, B.; Dunstan, D.; Gilson, N.; Eakin, E. The BeUpstanding Program: Scaling up the Stand Up Australia workplace intervention for translation into practice. AIMS Public Health 2016, 3, 341–347. [Google Scholar] [CrossRef]
- Zhu, W.; Owen, N. Sedentary Behavior and Health: Concepts, Assessments, and Interventions; Human Kinetics: Champaign, IL, USA, 2017. [Google Scholar]
- Leitzmann, M.; Jochem, C.; Schmid, D. Sedentary Behavior Epidemiology; Springer: Berlin, Germany, 2018. [Google Scholar]
- Van der Ploeg, H.P.; Hillsdon, M. Is sedentary behaviour just physical inactivity by another name? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 142. [Google Scholar] [CrossRef]
- De Bruin, A.; Della Salla, S. How biases inflate scientific evidence. Psychologist 2016, 29, 36–39. [Google Scholar]
- American College of Sports Medicine. Position statement on the recommended quantity and quality of exercise for developing and maintaining fitness in healthy adults. Med. Sci. Sports 1978, 10, vii–x. [Google Scholar]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C.; et al. Physical activity and public health: A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995, 273, 402–407. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Pearson, N.; Salmon, J. Sedentary behaviors and adiposity in young people: Causality and conceptual model. Exerc. Sport Sci. Rev. 2018, 46, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Ekelund, U.; Ding, D.; Hamer, M.; Bauman, A.E.; Lee, I.M. Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. Br. J. Sports Med. 2019, 53, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M. Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Gale, J.; Bauman, A.; Ekelund, U.; Hamer, M.; Ding, D. Sitting time, physical activity, and risk of mortality in adults. J. Am. Coll. Cardiol. 2019, 73, 2062–2072. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Waters, T.R.; Dick, R.B. Evidence of health risks associated with prolonged standing at work and intervention effectiveness. Rehabil. Nurs. 2015, 40, 148–165. [Google Scholar] [CrossRef]
- Coenen, P.; Willenberg, L.; Parry, S.; Shi, J.W.; Romero, L.; Blackwood, D.M.; Maher, C.G.; Healy, G.N.; Dunstan, D.; Straker, L.M. Associations of occupational standing with musculoskeletal symptoms: A systematic review with meta-analysis. Br. J. Sports Med. 2018, 52, 176–183. [Google Scholar] [CrossRef]
- Roffey, D.M.; Wai, E.K.; Bishop, P.; Kwon, B.K.; Dagenais, S. Causal assessment of occupational standing or walking and low back pain: Results of a systematic review. Spine J. 2010, 10, 262–272. [Google Scholar] [CrossRef]
- Coenen, P.; Parry, S.; Willenberg, L.; Shi, J.W.; Romero, L.; Blackwood, D.M.; Healy, G.N.; Dunstan, D.; Straker, L.M. Associations of prolonged standing with musculoskeletal symptoms—A systematic review of laboratory studies. Gait Posture 2017, 58, 310–318. [Google Scholar] [CrossRef]
- Saeidifard, F.; Medina-Inojosa, J.R.; Supervia, M.; Olson, T.P.; Somers, V.K.; Erwin, P.J.; Lopez-Jiminez, F. Differences of energy expenditure while sitting versus standing: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2018, 25, 522–538. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T. Standing and mortality in a prospective cohort of Canadian adults. Med. Sci. Sports Exerc. 2014, 46, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Van der Ploeg, H.P.; Chey, T.; Ding, D.; Chau, J.Y.; Stamatakis, E.; Bauman, A.E. Standing time and all-cause mortality in a large cohort of Australian adults. Prev. Med. 2014, 69, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; Ma, H.; Glazier, R.H.; Gilbert-Ouimet, M.; Mustard, C. The relationship between occupational standing and sitting and incident heart disease over a 12-year period in Ontario, Canada. Am. J. Epidemiol. 2018, 187, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Henson, J.; Bodicoat, D.H.; Bakrania, K.; Khunti, K.; Davies, M.J.; Yates, T. Associations of reallocating sitting time into standing or stepping with glucose, insulin and insulin sensitivity: A cross-sectional analysis of adults at risk of type 2 diabetes. BMJ Open 2017, 7, e014267. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Winkler, E.A.H.; Owen, N.; Anuradha, S.; Dunstan, D.W. Replacing sitting time, standing or stepping: Associations with cardio-metabolic risk biomarkers. Eur. Heart J. 2015, 36, 2643–2649. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.J.; Wullems, J.A.; Stebbings, G.K.; Morse, C.I.; Stewart, C.E.; Onambele-Pearson, G.L. Segregating the distinct effects of sedentary behavior and physical activity on older adults’ cardiovascular profile: Part 2—Isotemporal substitution approach. J. Phys. Act. Health 2018, 15, 537–542. [Google Scholar] [CrossRef]
- Van der Berg, J.D.; Van der Velde, J.H.P.M.; De Waard, E.A.C.; Bosma, H.; Savelberg, H.H.C.M.; Schaper, N.C.; Van Den Bergh, J.P.W.; Geusens, P.P.M.M.; Schram, M.T.; Sep, S.J.S.; et al. Replacement effects of sedentary time on metabolic outcomes: The Maastricht Study. Med. Sci. Sports Exerc. 2017, 49, 1351–1358. [Google Scholar] [CrossRef]
- Stamatakis, E.; Rogers, K.; Ding, D.; Berrigan, D.; Chau, J.; Hamer, M.; Bauman, A. All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: A prospective study of 201,129 mid-aged and older adults. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 121. [Google Scholar] [CrossRef]
- Henson, J.; Edwardson, C.L.; Bodicoat, D.H.; Bakrania, K.; Davies, M.J.; Khunti, K.; Talbot, D.C.S.; Yates, T. Reallocating sitting time to standing or stepping through isotemporal analysis: Associations with markers of chronic low-grade inflammation. J. Sports Sci. 2018, 36, 1586–1593. [Google Scholar] [CrossRef]
- Van Roekel, E.H.; Bours, M.J.; Breedveld-Peters, J.J.; Willems, P.J.; Meijer, K.; Kant, I.; van den Brandt, P.A.; Beets, G.L.; Sanduleanu, S.; Weijenberg, M.P. Modeling how substitution of sedentary behavior with standing or physical activity is associated with health-related quality of life in colorectal cancer survivors. Cancer Causes Control. 2016, 27, 513–525. [Google Scholar] [CrossRef]
- Van Der Velde, J.; Koster, A.; Van Der Berg, J.; Sep, S.J.S.; Van Der Kallen, C.J.H.; Dagnelie, P.C.; Schram, M.T.; Henry, R.M.A.; Eussen, S.J.P.M.; Van Dongen, M.C.J.M.; et al. Sedentary behavior, physical activity, and fitness—The Maastricht Study. Med. Sci. Sports Exerc. 2017, 49, 1583–1591. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Heiden, M.; Aadahl, M.; Korshøj, M.; Jørgensen, M.B.; Holtermann, A. What is the effect on obesity indicators from replacing prolonged sedentary time with brief sedentary bouts, standing and different types of physical activity during working days? A cross-sectional accelerometer-based study among blue-collar workers. PLoS ONE 2016, 11, e0154935. [Google Scholar] [CrossRef] [PubMed]
- Thorp, A.A.; Kingwell, B.A.; Sethi, P.; Hammond, L.; Owen, N.; Dunstan, D.W. Alternating bouts of sitting and standing attenuate postprandial glucose responses. Med. Sci. Sports Exerc. 2014, 46, 2053–2061. [Google Scholar] [CrossRef] [PubMed]
- Crespo, N.C.; Mullane, S.L.; Zeigler, Z.S.; Buman, M.P.; Gaesser, G.A. Effects of standing and light-intensity walking and cycling on 24-h glucose. Med. Sci. Sports Exerc. 2016, 48, 2503–2511. [Google Scholar] [CrossRef]
- Duvivier, B.M.F.M.; Schaper, N.C.; Koster, A.; van Kan, L.; Peters, H.P.F.; Adam, J.J.; Giesbrecht, T.; Kronips, E.; Hulsbosch, M.; Willems, P.; et al. Benefits of substituting sitting with standing and walking in free-living conditions for cardiometabolic risk markers, cognition and mood in overweight adults. Front. Physiol. 2017, 8. [Google Scholar] [CrossRef]
- Buckley, J.P.; Mellor, D.D.; Michael, M.; Franklin, J. Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion. Occup. Environ. Med. 2014, 71, 109–111. [Google Scholar] [CrossRef]
- Barone Gibbs, B.; Kowalsky, R.J.; Perdomo, S.J.; Taormina, J.M.; Balzer, J.R.; Jakicic, J.M. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J. Hypertens. 2017, 35, 2411–2418. [Google Scholar] [CrossRef]
- Zeigler, Z.S.; Mullane, S.L.; Crespo, N.C.; Buman, M.P.; Gaesser, G.A. Effects of standing and light-intensity activity on ambulatory blood pressure. Med. Sci. Sports Exerc. 2016, 48, 175–181. [Google Scholar] [CrossRef]
- Danquah, I.H.; Kloster, S.; Holtermann, A.; Aadahl, M.; Tolstrup, J.S. Effects on musculoskeletal pain from “Take a Stand!”—A cluster-randomized controlled trial reducing sitting time among office workers. Scand. J. Work Environ. Health 2017, 43, 350–357. [Google Scholar] [CrossRef]
- Lunde, L.K.; Koch, M.; Knardahl, S.; Veiersted, K.B. Associations of objectively measured sitting and standing with low-back pain intensity: A 6-month follow-up of construction and healthcare workers. Scand. J. Work Environ. Health 2017, 43, 269–278. [Google Scholar] [CrossRef]
- Thorp, A.A.; Kingwell, B.A.; Owen, N.; Dunstan, D.W. Breaking up workplace sitting time with intermittent standing bouts improves fatigue and musculoskeletal discomfort in overweight/obese office workers. Occup. Environ. Med. 2014, 71, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; Coenen, P.; Howie, E.; Lee, J.; Williamson, A.; Straker, L. A detailed description of the short-term musculoskeletal and cognitive effects of prolonged standing for office computer work. Ergonomics 2018, 61, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Mullane, S.L.; Buman, M.P.; Zeigler, Z.S.; Crespo, N.C.; Gaesser, G.A. Acute effects on cognitive performance following bouts of standing and light-intensity physical activity in a simulated workplace environment. J. Sci. Med. Sport 2017, 20, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Russell, B.A.; Summers, M.J.; Tranent, P.J.; Palmer, M.A.; Cooley, P.D.; Pedersen, S.J. A randomised control trial of the cognitive effects of working in a seated as opposed to a standing position in office workers. Ergonomics 2016, 59, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Karol, S.; Robertson, M.M. Implications of sit-stand and active workstations to counteract the adverse effects of sedentary work: A comprehensive review. Work 2015, 52, 255–267. [Google Scholar] [CrossRef]
- MacEwen, B.T.; MacDonald, D.J.; Burr, J.F. A systematic review of standing and treadmill desks in the workplace. Prev. Med. 2015, 70, 50–58. [Google Scholar] [CrossRef]
- Karakolis, T.; Callaghan, J.P. The impact of sit-stand office workstations on worker discomfort and productivity: A review. Appl. Ergon. 2014, 45, 799–806. [Google Scholar] [CrossRef]
- Agarwal, S.; Steinmaus, C.; Harris-Adamson, C. Sit-stand workstations and impact on low back discomfort: A systematic review and meta-analysis. Ergonomics 2018, 61, 538–552. [Google Scholar] [CrossRef]
- Shrestha, N.; Ijaz, S.; Kukkonen-Harjula, K.T.; Kumar, S.; Nwankwo, C.P. Workplace interventions for reducing sitting at work. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Schuna, J.M.; Frensham, L.J., Jr.; Proenca, M. Changing the way we work: Elevating energy expenditure with workstation alternatives. Int. J. Obes. 2014, 38, 755–765. [Google Scholar] [CrossRef]
- Ojo, S.O.; Bailey, D.P.; Chater, A.M.; Hewson, D.J. The impact of active workstations on workplace productivity and performance: A systematic review. Int. J. Environ. Res. Public Health 2018, 15. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, L.; Hall, J.; Smith, L.; Rasch, M.; Reeves, E.; Dewitt, S.; Gardner, B. “Could you sit down please?” A qualitative analysis of employees’ experiences of standing in normally-seated workplace meetings. PLoS ONE 2018, 13, e0198483. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.P.; Hedge, A.; Yates, T.; Copeland, R.J.; Loosemore, M.; Hamer, M.; Bradley, G.; Dunstan, D.W. The sedentary office: An expert statement on the growing case for change towards better health and productivity. Br. J. Sports Med. 2015, 49, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Vernikos, J. Gravity, sitting, and health. In Sedentary Behavior and Health: Concepts, Assessments, and Interventions; Zhu, W., Owen, N., Eds.; Human Kinetics: Champaign, IL, USA, 2017; pp. 13–29. [Google Scholar]
- Healy, G.N.; Dunstan, D.W.; Salmon, J.; Cerin, E.; Shaw, J.E.; Zimmet, P.Z.; Owen, N. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care 2008, 31. [Google Scholar] [CrossRef] [PubMed]
- Healy, G.N.; Matthews, C.E.; Dunstan, D.W.; Winkler, E.A.; Owen, N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur. Heart J. 2011, 32, 590–597. [Google Scholar] [CrossRef]
- Chastin, S.F.; Egerton, T.; Leask, C.; Stamatakis, E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity 2015, 23, 1800–1810. [Google Scholar] [CrossRef]
- Bellettiere, J.; Winkler, E.A.; Chastin, S.F.M.; Kerr, J.; Owen, N.; Dunstan, D.W.; Healy, G.N. Associations of sitting accumulation patterns with cardio-metabolic risk biomarkers in Australian adults. PLoS ONE 2017, 12, e0180119. [Google Scholar] [CrossRef]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: A national cohort study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef]
- Larsen, R.N.; Dempsey, P.C.; Dillon, F.; Grace, M.; Kingwell, B.A.; Owen, N.; Dunstan, D.W. Does the type of activity “break” from prolonged sitting differentially impact on postprandial blood glucose reductions? An exploratory analysis. Appl. Physiol. Nutr. Metab. 2017, 42, 897–900. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Larsen, R.N.; Winkler, E.A.H.; Owen, N.; Kingwell, B.A.; Dunstan, D.W. Prolonged uninterrupted sitting elevates postprandial hyperglycaemia proportional to degree of insulin resistance. Diabetes Obes. Metab. 2019, 20, 1526–1530. [Google Scholar] [CrossRef]
- Saunders, T.J.; Atkinson, H.F.; Burr, J.; MacEwen, B.; Skeaff, C.M.; Peddie, M.C. The acute metabolic and vascular impact of interrupting prolonged sitting: A systematic review and meta-analysis. Sports Med. 2018, 48, 2347–2366. [Google Scholar] [CrossRef] [PubMed]
- Duvivier, B.M.F.M.; Schaper, N.C.; Bremers, M.A.; van Crombrugge, G.; Menheere, P.P.; Kars, M.; Savelberg, H.H. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS ONE 2013, 82, e55542. [Google Scholar] [CrossRef] [PubMed]
- Alley, S.J.; Vandelanotte, C.; Duncan, M.J.; Short, C.E.; Maher, J.P.; Schoeppe, S.; Rebar, A. Should I sit or stand: Likelihood of adherence to messages about reducing sitting time. BMC Public Health 2019, 19, 871. [Google Scholar] [CrossRef] [PubMed]
- Wijndaele, K.; Brage, S.; Besson, H.; Khaw, K.T.; Sharp, S.J.; Luben, R.; Wareham, N.J.; Ekelund, U. Television viewing time independently predicts all-cause and cardiovascular mortality: The EPIC Norfolk Study. Int. J. Epidemiol. 2010, 40, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.H.; Bennie, J.; Bauman, A.; Chau, J.Y.; Dunstan, D.W.; Owen, N.; Stamatakis, E.; van Uffelen, J.G. Too much sitting and all-cause mortality: Is there a causal link? BMC Public Health 2016, 16, 635. [Google Scholar] [CrossRef]
- Hill, A.B. The environment and disease: Association or causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018. [Google Scholar] [CrossRef]
- Ku, P.W.; Steptoe, A.; Liao, Y.; Hsueh, M.C.; Chen, L.J. A cut-off of daily sedentary time and all-cause mortality in adults: A meta-regression analysis involving more than 1 million participants. BMC Med. 2018, 16, 74. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Evenson, K.R.; Kamada, M.; LaCroix, A.Z.; Buring, J.E. Accelerometer-measured physical activity and sedentary behavior in relation to all-cause mortality. Circulation 2018, 137, 203–205. [Google Scholar] [CrossRef]
- Bellettiere, J.; LaMonte, M.J.; Evenson, K.R.; Rillamas-Sun, R.; Kerr, J.; Lee, I.M.; Rosenberg, D.E.; Stefanick, M.; Buchner, D.; Hovell, M.F.; et al. Sedentary behavior and cardiovascular disease in older women. Circulation 2019, 139, 1036–1046. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Loenneke, J.P.; Ahmed, H.M.; Blaha, M.J. Joint effects of objectively-measured sedentary time and physical activity on all-cause mortality. Prev. Med. 2016, 90, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Powell, K.E.; Jakicic, J.M.; Troiano, R.P.; Piercy, K.; Tennant, B. Sedentary Behavior and Health: Update from the 2018 Physical Activity Guidelines Advisory Committee. Med. Sci. Sports Exerc. 2019, 51, 1227–1241. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.H.; García Bengoechea, E.; Bennie, J.; Pedisic, Z.; Vergeer, I.; Wiesner, G. Screen time, other sedentary behaviours, and obesity risk in adults: A review of reviews. Curr. Obes. Rep. 2017, 6, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Vallance, J.K.; Gardiner, P.A.; Lynch, B.M.; D’Silva, A.; Boyle, T.; Taylor, L.; Johnson, S.T.; Buman, M.P.; Owen, N. Evaluating the evidence on sitting, smoking, and health: Is sitting really the new smoking? Am. J. Public Health 2018, 108, 1478. [Google Scholar] [CrossRef]
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Barbara Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef]
| Source Type of Evidence | Standing Is in Favour of | Standing Is Detrimental for | Standing Is Not Associated with | Inconsistent Findings on the Link with Standing |
|---|---|---|---|---|
| Review studies (k = 5) | Energy expenditure (MA 1) (gender ≠) | Low back pain (MA 1) Lower extremity symptoms Vascular problems Fatigue & discomfort | Causality low back pain Upper extremity symptoms | |
| Review studies sit-stand desks (k = 6) | Performance/ productivity Sick leave | Musculoskeletal discomfort Mood states Energy expenditure | ||
| Prospective (k = 2) | All-cause mortality CVD 2 mortality Other mortality | Cancer mortality | ||
| Isotemporal substitutions (k = 9) | Cardio-metabolic health Mortality Metabolic syndrome Type 2 diabetes Inflammation Physical functioning Disability Fatigue | Cardiorespiratory fitness Quality of life Role functioning Social functioning Depression Anxiety | Adiposity | |
| Experiments (k = 13) | Energy expenditure | Cardio-metabolic health Blood pressure Musculoskeletal health Cognitive functions |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biddle, S.J.H.; Bennie, J.A.; De Cocker, K.; Dunstan, D.; Gardiner, P.A.; Healy, G.N.; Lynch, B.; Owen, N.; Brakenridge, C.; Brown, W.; et al. Controversies in the Science of Sedentary Behaviour and Health: Insights, Perspectives and Future Directions from the 2018 Queensland Sedentary Behaviour Think Tank. Int. J. Environ. Res. Public Health 2019, 16, 4762. https://doi.org/10.3390/ijerph16234762
Biddle SJH, Bennie JA, De Cocker K, Dunstan D, Gardiner PA, Healy GN, Lynch B, Owen N, Brakenridge C, Brown W, et al. Controversies in the Science of Sedentary Behaviour and Health: Insights, Perspectives and Future Directions from the 2018 Queensland Sedentary Behaviour Think Tank. International Journal of Environmental Research and Public Health. 2019; 16(23):4762. https://doi.org/10.3390/ijerph16234762
Chicago/Turabian StyleBiddle, Stuart J.H., Jason A. Bennie, Katrien De Cocker, David Dunstan, Paul A. Gardiner, Genevieve N. Healy, Brigid Lynch, Neville Owen, Charlotte Brakenridge, Wendy Brown, and et al. 2019. "Controversies in the Science of Sedentary Behaviour and Health: Insights, Perspectives and Future Directions from the 2018 Queensland Sedentary Behaviour Think Tank" International Journal of Environmental Research and Public Health 16, no. 23: 4762. https://doi.org/10.3390/ijerph16234762
APA StyleBiddle, S. J. H., Bennie, J. A., De Cocker, K., Dunstan, D., Gardiner, P. A., Healy, G. N., Lynch, B., Owen, N., Brakenridge, C., Brown, W., Buman, M., Clark, B., Dohrn, I.-M., Duncan, M., Gilson, N., Kolbe-Alexander, T., Pavey, T., Reid, N., Vandelanotte, C., ... Vincent, G. E. (2019). Controversies in the Science of Sedentary Behaviour and Health: Insights, Perspectives and Future Directions from the 2018 Queensland Sedentary Behaviour Think Tank. International Journal of Environmental Research and Public Health, 16(23), 4762. https://doi.org/10.3390/ijerph16234762










