Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia—A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sampling
2.2. Sample Size Calculation
2.3. Refractive Error Screening Procedure
2.4. Definition of Refractive Error
2.5. Statistical Analyses
3. Results
3.1. Demographic Data
3.2. Distribution of Refractive Error
3.3. Association of Refractive Error Group with Gender and Race.
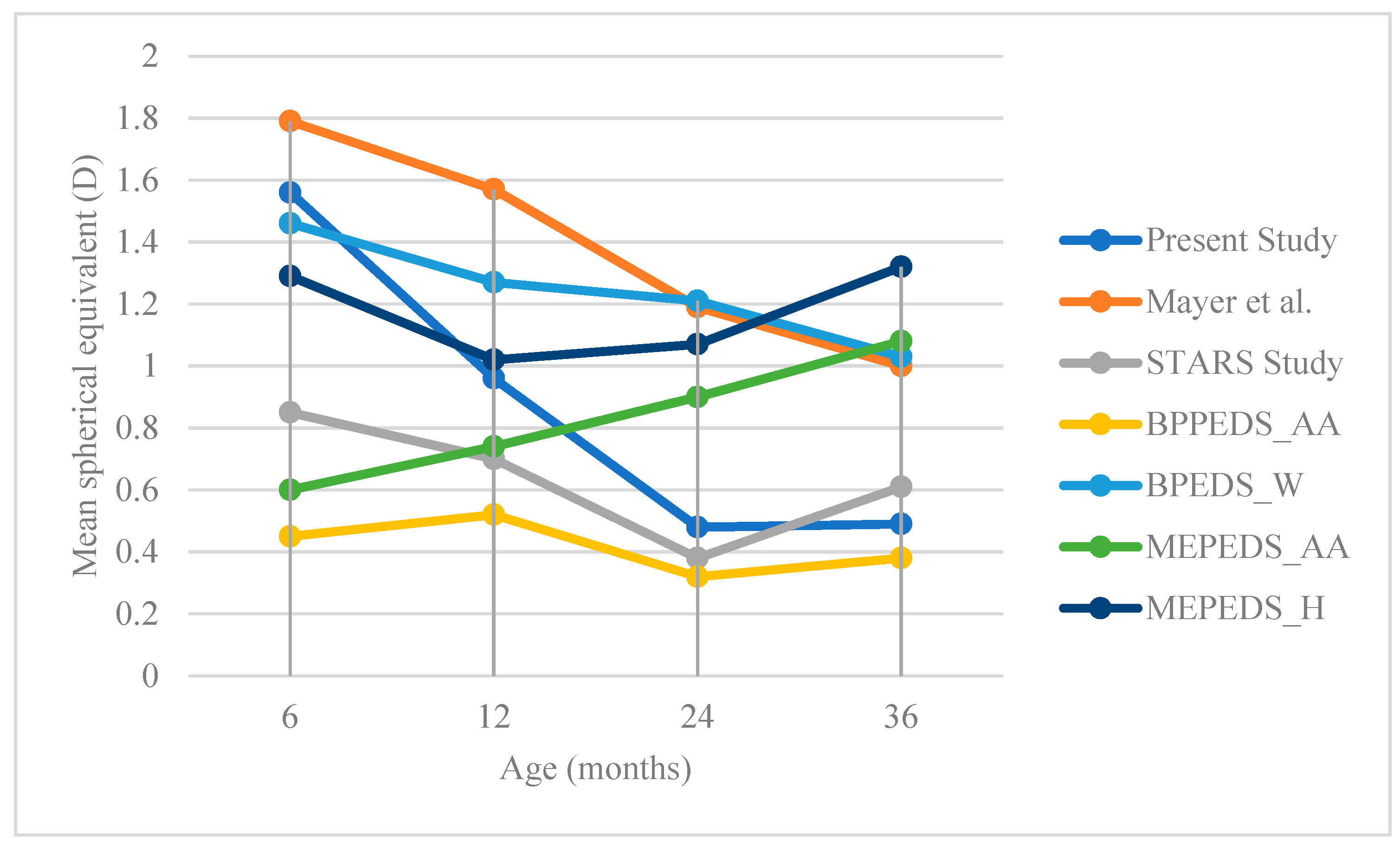
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hashemi, H.; Fotouhi, A.; Yekta, A.; Pakzad, R.; Ostadimoghaddam, H.; Khabazkhoob, M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J. Curr. Ophthalmol. 2018, 30, 3–22. [Google Scholar] [CrossRef] [PubMed]
- Ingram, R.M.; Traynar, M.J.; Walker, C. Screening for refractive errors at age 1 year: A pilot study. Br. J. Ophthalmol. 1979, 63, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Ingram, R.M.; Arnold, P.E.; Dally, S.; Lucas, J. Emmetropisation, squint, and reduced visual acuity after treatment. Br. J. Ophthalmol. 1991, 75, 414–416. [Google Scholar] [CrossRef] [PubMed]
- Dirani, M.; Chan, Y.; Gazzard, G.; Hornbeak, D.M.; Leo, S.; Selvaraj, P.; Zhou, B.; Young, T.L.; Mitchell, P.; Varma, R.; et al. Prevalence of Refractive Error in Singaporean Chinese Children: The Strabismus, Amblyopia, and Refractive Error in Young Singaporean Children (STARS) Study. Invest. Ophthalmol. Vis. Sci. 2010, 51, 1348–1355. [Google Scholar] [CrossRef] [PubMed]
- MEPED Study. Prevalence of Myopia and Hyperopia in 6 to 72 Months Old African American and Hispanic Children: The Multi-Ethnic Pediatric Eye Disease (MEPED) Study. Ophthalmology 2010, 117, 140–147. [Google Scholar] [CrossRef]
- Wen, G.; Tarczy-Hornoch, K.; Mckean-Cowdin, R.; Cotter, S.A.; Borchert, M.; Lin, J.; Kim, J.; Varma, R.; Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: Multi-ethnic pediatric eye disease study. Ophthalmology 2013, 120, 2109–2116. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Jones, L.A.; Friedman, N.E.; Frane, S.L.; Lin, W.K.; Moeschberger, M.L.; Zadnik, K. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest. Ophthalmol. Vis. Sci. 2005, 46, 3074–3080. [Google Scholar] [CrossRef]
- Read, S.A.; Collins, M.J.; Carney, L.G. A review of astigmatism and its possible genesis. Clin. Exp. Optom. 2007, 90, 5–19. [Google Scholar] [CrossRef]
- Dobson, V.; Harvey, E.M.; Miller, J.M. Spherical equivalent refractive error in preschool children from a population with a high prevalence of astigmatism. Optom. Vis. Sci. 2007, 84, 124–130. [Google Scholar] [CrossRef]
- Goss, D. Meridional analysis of with-the-rule astigmatism in Oklahoma Indians. Optom. Vis. Sci. 1989, 66, 281–287. [Google Scholar] [CrossRef]
- Mohindra, I.; Nagaraj, S. Astigmatism in Zuni and Navajo Indians. Am. J. Optom. Physiol. Opt. 1977, 54, 121–124. [Google Scholar] [CrossRef]
- Fan, D.S.P.; Rao, S.K.; Cheung, E.Y.Y.; Islam, M.; Chew, S.; Lam, D.S.C. Astigmatism in Chinese preschool children: Prevalence, change, and effect on refractive development. Br. J. Ophthalmol. 2004, 88, 938–941. [Google Scholar] [CrossRef] [PubMed]
- Kleinstein, R.N.; Jones, L.A.; Hullett, S.; Kwon, S.; Lee, R.J.; Friedman, N.E.; Manny, R.E.; Mutti, D.O.; Yu, J.A.; Zadnik, K.; et al. Refractive error and ethnicity in children. Arch. Ophthalmol. 2003, 121, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Thorn, F.; Cruz, A.A.V.; Machado, A.J.; Carvalho, R.A.C. Refractive status of indigenous people in the northwestern Amazon region of Brazil. Optom. Vis. Sci. 2005, 82, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Leat, S.J. To prescribe or not to prescribe? Guidelines for spectacle prescribing in infants and children. Cli. Exp. Optom. 2011, 94, 514–527. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.M.; Clarke, M.P. Amblyopia. Lancet 2006, 367, 1343–1351. [Google Scholar] [CrossRef]
- Ingram, R.M.; Barr, A. Changes in refraction between the ages of 1 and 3 1/2 years. Br. J. Ophthalmol. 1979, 63, 339–342. [Google Scholar] [CrossRef]
- Atkinson, J.; Braddick, O.; Robier, B.; Anker, S.; Ehrlich, D.; King, J.; Watson, P.; Moore, A. Two infant vision screening programmes: Prediction and prevention of strabismus and amblyopia from photo- and videorefractive screening. Eye (London, England). 1996, 10, 189–198. [Google Scholar] [CrossRef]
- Cochran, W. Sampling Techniques, 2nd ed.; John Wiley and Sons: New York, NY, USA, 1963. [Google Scholar]
- Mayer, D.L.; Hansen, R.M.; Moore, B.D.; Kim, S.; Fulton, A.B. Cycloplegic Refractions in Healthy Children Aged 1 Through 48 Months. Arch. Ophthalmol. 2001, 119, 1625–1628. [Google Scholar] [CrossRef]
- MEPED Study. Prevalence of Astigmatism in 6 to 72 Months Old African American and Hispanic Children: The Multi-Ethnic Pediatric Eye Disease Study 12,13. Ophthalmology 2011, 118, 284–293. [Google Scholar] [CrossRef]
- Gwiazda, J.; Scheiman, M.; Mohindra, I.; Held, R. Astigmatism in children: Changes in axis and amount from birth to six years. Invest. Ophthalmol. Vis. Sci. 1984, 25, 88–92. [Google Scholar] [PubMed]
- Mohindra, I.; Held, R.; Gwiazda, J.; Brill, J. Astigmatism in infants. Science (New York, N.Y.). 1978, 202, 329–331. [Google Scholar] [CrossRef] [PubMed]
- Giordano, L.; Friedman, D.S.; Repka, M.X.; Katz, J.; Ibironke, J.; Hawes, P.; Tielsch, J.M. Prevalence of Refractive Error among Preschool Children in an Urban Population: The Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009, 116, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Fan, D.S.P.; Lam, D.S.C.; Lam, R.F.; Lau, J.T.F.; Chong, K.S.; Cheung, E.Y.Y.; Lai, R.Y.K.; Chew, S.J. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest. Ophthalmol Vis. Sci. 2004, 45, 1071–1075. [Google Scholar] [CrossRef]
- Saw, S.M.; Nieto, F.J.; Katz, J.; Schein, O.D.; Levy, B.; Chew, S.J. Factors related to the progression of myopia in Singaporean children. Optom Vis. Sci. 2000, 77, 549–554. [Google Scholar] [CrossRef]
- Zhao, J.; Pan, X.; Sui, R.; Munoz, S.R.; Sperduto, R.D.; Ellwein, L.B. Refractive Error Study in Children: Results from Shunyi District, China. Am. J. Ophthalmol. 2000, 129, 427–435. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Jones, L.A.; Friedman, N.E.; Frane, S.L.; Lin, W.K.; Moeschberger, M.L.; Zednik, K. Refractive astigmatism and the toricity of ocular components in human infants. Opto. Vis. Sci. 2004, 81, 753–761. [Google Scholar] [CrossRef]
| WHO Regions | Astigmatism | Hyperopia | Myopia |
|---|---|---|---|
| %EPP (95% CI) | %EPP (95% CI) | %EPP (95% CI) | |
| South-East Asia | 9.8 (6.3−13.2) | 2.2 (1.2−3.3) | 4.9 (1.6−8.1) |
| Western Pacific | 12.1 (8.4−15.8) | 3.1 (1.9−4.3) | 18.2 (10.9−25.5) |
| Africa | 14.2 (9.9−18.5) | 3.0 (1.8−4.3) | 6.2 (4.8−7.6) |
| Americas | 27.2 (26−28.4) | 14.3 (13.4−15.2) | 8.4 (4.9−12) |
| Europe | 12.9 (4.1−21.8) | 9 (4.3−13.7) | 14.3 (10.5−18.2) |
| Eastern Mediterranean | 20.4 (14.5−26.3) | 6.8 (4.9−8.6) | 9.2 (8.1−10.4) |
| All | 14.9 (12.7−17.1) | 4.6 (3.9−5.2) | 11.7 (10.5−13.0) |
| Characteristics | Frequency (%) (Male:Female) (95% CI) | Mean ± SD | 95% Confidence Interval | Median (Interquartile range, IQR) |
|---|---|---|---|---|
| Age (months) | 18.09 (7.95) | 18.8–19.4 | 18.00 (12.00) | |
| Age (months) by group | ||||
| 6–11.9 | 33 (21.9) | |||
| (21:12) | ||||
| (15.3–28.5) | ||||
| 12–17.9 | 39 (25.8) | |||
| (21:18) | ||||
| (18.8–32.8) | ||||
| 18–23.9 | 38 (25.2) | |||
| (19:19) | ||||
| (18.3–32.1) | ||||
| 24–29.9 | 22 (14.6) | |||
| (13:9) | ||||
| (9.0–20.2) | ||||
| 30–36 | 19 (12.6) | |||
| (10:9) | ||||
| (7.3–17.9) | ||||
| Race/ethnicity | ||||
| Malay | 126 (83.4) | |||
| Chinese | 10 (6.6) | |||
| Indian | 14 (9.3) | |||
| Other | 1 (0.7) | |||
| Spherical equivalent, D | 0.85 (0.97) | 0.70–1.0 | 0.75 (1.38) | |
| Mothers age (years) | 30.42 (4.38) | 29.7–31.1 | 30.00 (5.00) | |
| Mother’s highest education level | ||||
| Primary school | 8 (5.3) | |||
| Secondary school | 82 (54.3) | |||
| Diploma | 35 (23.2) | |||
| Degree and above | 26 (17.2) | |||
| Mother’s occupation | ||||
| Housewife | 53 (35.1) | |||
| Government | 32 (21.2) | |||
| Private | 57 (37.7) | |||
| Self-employed | 9 (6.0) | |||
| Household income (RM) | ||||
| >5000 | 42 (27.8) | |||
| 3500–5000 | 49 (32.5) | |||
| 1500–3499 | 51 (33.8) | |||
| <1500 | 9 (6.0) | |||
| Mother’s smoking history | ||||
| None | 141 (93.4) | |||
| Current smoker | 5 (3.3) | |||
| Past smoker | 5 (3.3) | |||
| Father’s smoking history | ||||
| None | 53 (35.1) | |||
| Current smoker | 86 (57.0) | |||
| Past smoker | 12 (7.9) | |||
| Parental myopia | ||||
| None | 59 (39.1) | |||
| Mother | 60 (39.7) | |||
| Father | 13 (8.6) | |||
| Both | 19 (12.6) |
| Age, Month (N) | SE (D) | Cylinder (D) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard Deviation | 95% Confidence Interval | Median | IQR | Mean | Standard Deviation | 95% Confidence Interval | Median | IQR | |
| 6–11.9 (33) | 1.56 | 0.92 | 1.23–1.89 | 1.50 | 1.31 | −1.12 | 0.59 | −1.33 to −0.91 | −1.00 | 0.75 |
| 12–17.9 (39) | 0.96 | 1.10 | 0.65–1.34 | 0.88 | 1.50 | −0.99 | 0.61 | −1.19 to −0.80 | −1.00 | 0.75 |
| 18–23.9 (38) | 0.50 | 0.66 | 0.29–0.72 | 0.63 | 0.91 | −1.03 | 0.47 | −1.18 to −0.88 | −1.00 | 0.75 |
| 24–29.9 (22) | 0.48 | 0.78 | 0.13–0.82 | 0.50 | 1.25 | −0.82 | 0.53 | −1.05 to −0.58 | −0.75 | 1.00 |
| 30–36 (19) | 0.49 | 0.49 | 0.11–0.82 | 0.63 | 1.25 | −0.87 | 0.84 | −1.28 to −0.46 | −0.75 | 0.50 |
| Parameters | Hyperopia | Emmetropia | Myopia | Astigmatism | Anisometropia |
|---|---|---|---|---|---|
| Gender | |||||
| Male (n = 84) | 10 (11.9) | 72 (85.7) | 2 (2.4) | 22 (26.2) | 0 (0.0) |
| (5.9–20.8) | (76.4–92.4) | (0.3–8.3) | (17.2–36.9) | (0.0–4.3) | |
| Female (n = 67) | 9 (13.4) | 58 (86.6) | 0 (0.0) | 17 (25.4) | 1 (1.5) |
| (6.3–24) | (76.0–93.7) | (0.0–5.4) | (15.5–37.5) | (0.0–8.0) | |
| Age (months) | |||||
| 6–11.9 (n = 33) | 11 (33.3) | 22 (66.7) | 0 (0.0) | 17 (39.4) | 0 (0.0) |
| (18.0–51.8) | (48.2–82.0) | (0.00–10.6) | (22.9–57.9) | (0.0–10.6) | |
| 12–17.9 (n = 39) | 6 (15.4) | 33 (84.6) | 0 (0.0) | 8 (23.1) | 1 (2.6) |
| (5.9–30.5) | (69.5–94.1) | (0.0–9.0) | (0.11–0.39) | (0.1–13.5) | |
| 18–23.9 (n = 38) | 1 (2.6) | 37 (97.4) | 0 (0.0) | 8 (28.9) | 0 (0.0) |
| (0.1–13.8) | (86.2–99.9) | (0.0–9.3) | (15.4–45.9) | (0.0–9.3) | |
| 24–29.9 (n = 22) | 1 (4.5) | 20 (90.9) | 1 (4.5) | 4 (18.2) | 0 (0.0) |
| (0.1–22.8) | (70.8–98.9) | (0.1–22.8) | (5.2–40.3) | (0.0–15.4) | |
| 30–36 (n = 19) | 0 (0.0) | 18 (94.7) | 1 (5.3) | 2 (10.5) | 0 (0.0) |
| (0.0–17.6) | (74.0–99.9) | (0.1–0.26) | (1.3–33.1) | (0.0–17.6) | |
| Race | |||||
| Malay (n = 126) | 15 (11.9) | 109 (86.5) | 2 (1.6) | 32 (25.4) | 1 (0.8) |
| (6.8–18.9) | (79.3–91.9) | (0.2–5.6) | (18.1–33.9) | (0.0–4.3) | |
| Chinese (n = 10) | 0 (0.0) | 10 (100) | 0 (0.0) | 3 (30.0) | 0 (0.0) |
| (0.0–30.8) | (69.2–100) | (0.0–30.8) | (6.7–65.2) | (0.0–30.8) | |
| Indian (n = 14) | 5 (28.6) | 10 (71.4) | 0 (0.0) | 4 (28.6) | 0 (0.0) |
| (8.4–58.1) | (0.42–0.92) | (0.0–23.2) | (8.4–58.1) | (0.0–23.2) | |
| Others (n = 1) | 0 (0.0) | 1 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| (0.0–97.5) | (2.5–100) | (0.0–97.5) | (0.0–97.5) | (0.0–97.5) | |
| Total | 19 (12.6) | 130 (86.1) | 2 (1.3) | 39 (25.8) | 1 (0.7) |
| (7.7–19.0) | (79.5–91.2) | (0.2–4.7) | (19.1–33.6) | (0.0–3.6) |
| Characteristics | Cases | Number (%) of Subjects | p-Value | |
|---|---|---|---|---|
| With Refractive Error (n = 21) | Without Refractive Error (n = 130) | |||
| Race | ||||
| Malay | 126 | 17 (13.5) | 109 (86.5) | 0.23 |
| (8.1–20.7) | (79.3–91.9) | |||
| Chinese | 10 | 0 (0.0) | 10 (100.0) | |
| (0.0–30.8) | (69.2–100) | |||
| Indian | 14 | 4 (28.6) | 10 (71.4) | |
| (8.4–58.1) | (41.9–91.6) | |||
| Gender | ||||
| Male | 84 | 12 (14.3) | 72 (85.7) | 0.88 |
| (7.6–23.6) | (76.4–92.4) | |||
| Female | 67 | 9 (13.4) | 58 (86.6) | |
| (6.3–24.0) | (76.0–93.7) | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yahya, A.N.; Sharanjeet-Kaur, S.; Akhir, S.M. Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia—A Pilot Study. Int. J. Environ. Res. Public Health 2019, 16, 4730. https://doi.org/10.3390/ijerph16234730
Yahya AN, Sharanjeet-Kaur S, Akhir SM. Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia—A Pilot Study. International Journal of Environmental Research and Public Health. 2019; 16(23):4730. https://doi.org/10.3390/ijerph16234730
Chicago/Turabian StyleYahya, Arifah Nur, Sharanjeet Sharanjeet-Kaur, and Saadah Mohamed Akhir. 2019. "Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia—A Pilot Study" International Journal of Environmental Research and Public Health 16, no. 23: 4730. https://doi.org/10.3390/ijerph16234730
APA StyleYahya, A. N., Sharanjeet-Kaur, S., & Akhir, S. M. (2019). Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia—A Pilot Study. International Journal of Environmental Research and Public Health, 16(23), 4730. https://doi.org/10.3390/ijerph16234730




