High-Intensity Interval Circuit Training Versus Moderate-Intensity Continuous Training on Functional Ability and Body Mass Index in Middle-Aged and Older Women: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
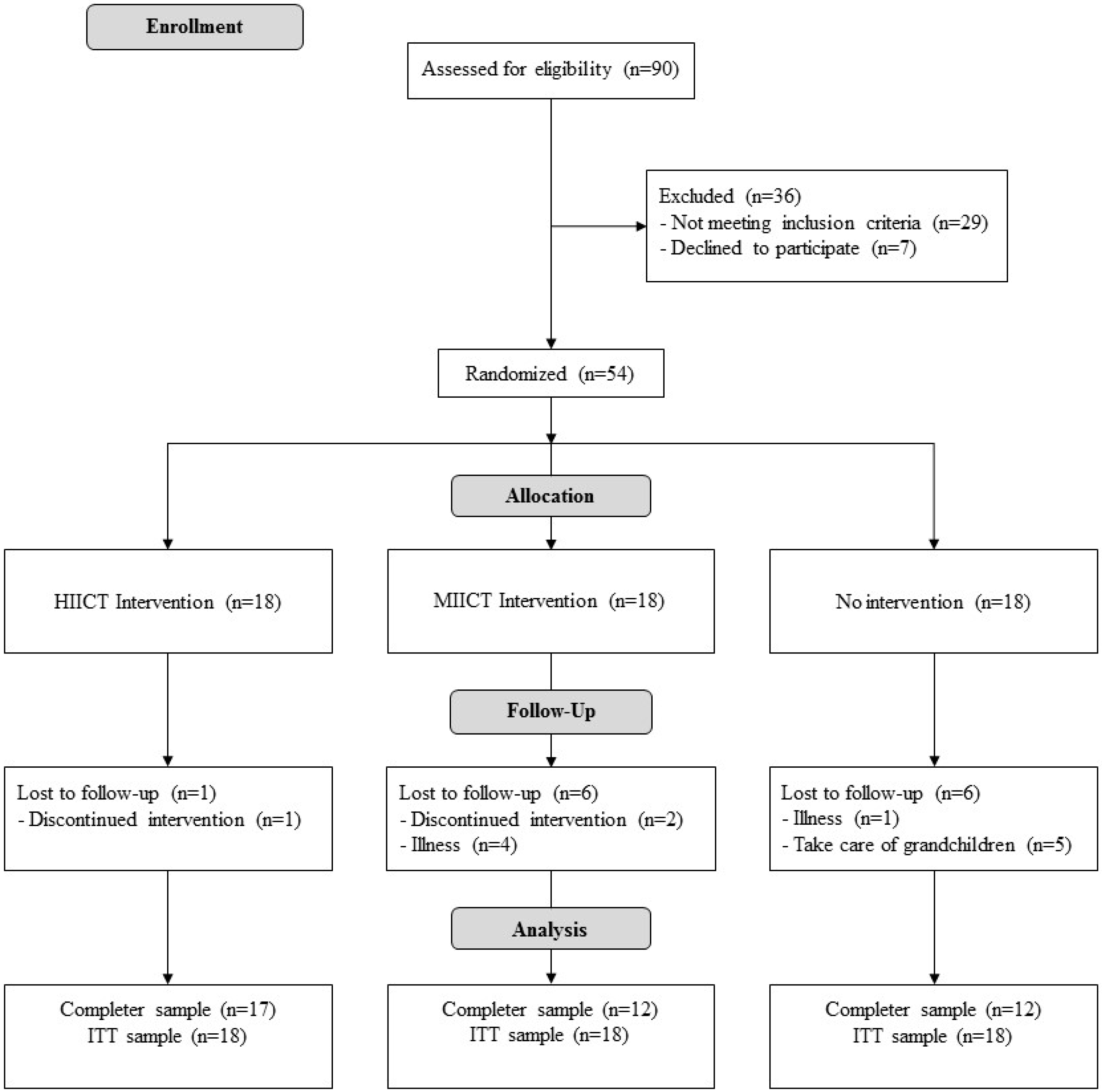
2.1. Design
2.2. Participants
2.3. Interventions
2.4. Outcomes
2.5. Sample Size and Power
2.6. Randomization and Blinding
2.7. Statistical methods
3. Results
3.1. Inter-group results
- In the ACT, HIICT was statistically better than MICT (dif = 6.6 rep, t = −3.905) and CG (dif = 9.3 rep, t = −2.986).
- In the 30-STS, HIICT was statistically better than CG (dif = 5.6 rep, t = −5.84) and MICT was also statistically better than CG (dif = 3.2 rep, t = −3.87).
- In the TUG, HIICT was statistically better than CG (dif = −0.78 sec, t = 4.03) and MICT was also statistically better than CG (dif = −0.23 sec, t = 4.244).
- In the 6MWT, HIICT was statistically better than CG (dif = 43 m, t = −3.631) and MICT was also statistically better than CG (dif = 55 m, t = −3.719).
- Regarding the BMI, HIICT was statistically better than CG (dif = −1.4 kg/m2, t = 3.58).
3.2. Intra-Group Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Blain, H.; Masud, T.; Dargent-Molina, P.; Martin, F.C.; Rosendahl, E.; van der Velde, N.; Bousquet, J.; Benetos, A.; Cooper, C.; Kanis, J.A.; et al. A comprehensive fracture prevention strategy in older adults: The European Union Geriatric Medicine Society (EUGMS) statement. Aging Clin. Exp. Res. 2016, 28, 797–803. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, E.D.; Valadares, A.L.R.; da Costa-Paiva, L.H.; Pedro, A.O.; Morais, S.S.; Pinto-Neto, A.M. Physical activity and quality of life in women aged 60 or older: Associated factors. Rev. Bras. Ginecol. E Obstet. 2010, 32, 433–440. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Bergman, H.; Ferrucci, L.; Guralnik, J.; Hogan, D.B.; Hummel, S.; Karunananthan, S.; Wolfson, C. Frailty: An emerging research and clinical paradigm—issues and controversies. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 731–737. [Google Scholar] [CrossRef]
- Guadalupe-Grau, A.; Carnicero, J.A.; Losa-Reyna, J.; Tresguerres, J.; Gómez-Cabrera, M.D.C.; Castillo, C.; Alfaro-Acha, A.; Rosado-Artalejo, C.; Rodríguez-Mañas, L.; García-García, F.J. Endocrinology of Aging from a Muscle Function Point of View: Results from the Toledo Study for Healthy Aging. J. Am. Med. Dir. Assoc. 2017, 18, 234–239. [Google Scholar] [CrossRef]
- Cesari, M.; Vellas, B.; Hsu, F.-C.; Newman, A.B.; Doss, H.; King, A.C.; Manini, T.M.; Church, T.; Gill, T.M.; Miller, M.E.; et al. A physical activity intervention to treat the frailty syndrome in older persons-results from the LIFE-P study. J. Gerontol. A Biol. Sci. Med. Sci. 2015, 70, 216–222. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 1059–1064. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health. Available online: https://population.un.org/wpp/ (accessed on 13 September 2019).
- Benítez-Porres, J.; Blanco, J.M.; Vázquez, R.F.; Alvero-Cruz, J.R. Sarcopenia y ejercicio físico. In Longevidad y Salud. Innovación en la Actividad Física, 1st ed.; Área de Cultura y Deportes de la Diputación de Málaga: Málaga, Spain, 2005; pp. 700–708. [Google Scholar]
- Bhaskaran, K.; dos-Santos-Silva, I.; Leon, D.A.; Douglas, I.A. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 2018, 6, 944–953. [Google Scholar] [CrossRef]
- Mazo, G.Z.; Liposcki, D.B.; Ananda, C.; Prevê, D. Health conditions, incidence of falls and physical activity levels among the elderly. Braz. J. Phys. Ther. 2007, 11, 437–442. [Google Scholar] [CrossRef]
- Arenas, S.R.; Gómez, J.P.; Ramón, P.E.A. Entrenamiento en circuitos. ¿Una herramienta útil para prevenir los efectos del envejecimiento? Cult. Cienc. Deporte 2011, 6, 185–192. [Google Scholar]
- Laredo-Aguilera, J.A.; Carmona-Torres, J.M.; García-Pinillos, F.; Latorre-Román, P.Á. Effects of a 10-week functional training programme on pain, mood state, depression, and sleep in healthy older adults. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2018, 18, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.; Paw, M.J.; van Poppel, M.N.; Twisk, J.W.; van Mechelen, W. Effects of resistance and all-round, functional training on quality of life, vitality and depression of older adults living in long-term care facilities: A ‘randomized’ controlled trial. BMC Geriatr. 2004, 4, 1–9. [Google Scholar] [CrossRef]
- Kaikkonen, H.; Yrjämä, M.; Siljander, E.; Byman, P.; Laukkanen, R. The effect of heart rate controlled low resistance circuit weight training and endurance training on maximal aerobic power in sedentary adults. Scand. J. Med. Sci. Sports 2000, 10, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Martínez, F.A.; Rubio-Arias, J.Á.; Ramos-Campo, D.J.; Alcaraz, P.E. Effectiveness of Resistance Circuit-Based Training for Maximum Oxygen Uptake and Upper-Body One-Repetition Maximum Improvements: A Systematic Review and Meta-Analysis. Sports Med. Auckl. NZ 2017, 47, 2553–2568. [Google Scholar] [CrossRef]
- Rosety, M.A.; Pery, M.T.; Rodriguez-Pareja, M.A.; Diaz, A.; Rosety, J.; Garcia, N.; Brenes-Martin, F.; Rosety-Rodríguez, M.; Toro, R.; Ordoñez, F.J.; et al. A Short-Term Circuit Resistance Programme Reduced Epicardial Fat in Obese Aged Women. Nutr. Hosp. 2015, 32, 2193–2197. [Google Scholar] [CrossRef]
- Romero-Arenas, S.; Blazevich, A.J.; Martínez-Pascual, M.; Pérez-Gómez, J.; Luque, A.J.; López-Román, F.J.; Alcaraz, P.E. Effects of high-resistance circuit training in an elderly population. Exp. Gerontol. 2013, 48, 334–340. [Google Scholar] [CrossRef]
- Giné-Garriga, M.; Guerra, M.; Unnithan, V.B. The effect of functional circuit training on self-reported fear of falling and health status in a group of physically frail older individuals: A randomized controlled trial. Aging Clin. Exp. Res. 2013, 25, 329–336. [Google Scholar] [CrossRef]
- Venturelli, M.; Cè, E.; Limonta, E.; Schena, F.; Caimi, B.; Carugo, S.; Veicteinas, A.; Esposito, F. Effects of endurance, circuit, and relaxing training on cardiovascular risk factors in hypertensive elderly patients. Age Dordr. Neth. 2015, 37, 101. [Google Scholar] [CrossRef]
- Whitehurst, M.A.; Johnson, B.L.; Parker, C.M.; Brown, L.E.; Ford, A.M. The benefits of a functional exercise circuit for older adults. J. Strength Cond. Res. 2005, 19, 647–651. [Google Scholar] [CrossRef]
- García, I.B.; Arias, J.Á.R.; Campo, D.J.R.; González-Moro, I.M.; Poyatos, M.C. High-intensity Interval Training Dosage for Heart Failure and Coronary Artery Disease Cardiac Rehabilitation. A Systematic Review and Meta-analysis. Rev. Espanola. Cardiol. Engl. Ed. 2019, 72, 233–243. [Google Scholar] [CrossRef]
- Wisløff, U.; Støylen, A.; Loennechen, J.P.; Bruvold, M.; Rognmo, Ø.; Haram, P.M.; Tjønna, A.E.; Helgerud, J.; Slørdahl, S.A.; Lee, S.J.; et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation 2007, 115, 3086–3094. [Google Scholar] [CrossRef] [PubMed]
- Moholdt, T.T.; Amundsen, B.H.; Rustad, L.A.; Wahba, A.; Løvø, K.T.; Gullikstad, L.R.; Bye, A.; Skogvoll, E.; Wisløff, U.; Slørdahl, S.A. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: A randomized study of cardiovascular effects and quality of life. Am. Heart J. 2009, 158, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Chicharro, J.L.; Campos, D.V. HIIT de la Teoría a la Práctica; Exercise Physiology & Training: Madrid, Spain, 2018. [Google Scholar]
- Adamson, S.; Lorimer, R.; Cobley, J.N.; Lloyd, R.; Babraj, J. High intensity training improves health and physical function in middle aged adults. Biology 2014, 3, 333–344. [Google Scholar] [CrossRef]
- Bruseghini, P.; Calabria, E.; Tam, E.; Milanese, C.; Oliboni, E.; Pezzato, A.; Pogliaghi, S.; Salvagno, G.L.; Schena, F.; Mucelli, R.P.; et al. Effects of eight weeks of aerobic interval training and of isoinertial resistance training on risk factors of cardiometabolic diseases and exercise capacity in healthy elderly subjects. Oncotarget 2015, 6, 16998–17015. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Van Bavel, D.; de Moraes, R.; Tibiriça, E.V. High-intensity interval training or continuous training, combined or not with fasting, in obese or overweight women with cardiometabolic risk factors: Study protocol for a randomised clinical trial. BMJ Open 2018, 8, e019304. [Google Scholar] [CrossRef]
- Coetsee, C.; Terblanche, E. The effect of three different exercise training modalities on cognitive and physical function in a healthy older population. Eur. Rev. Aging Phys. Act. 2017, 14, 13. [Google Scholar] [CrossRef]
- Alvarez, C.; Ramirez-Campillo, R.; Martinez-Salazar, C.; Mancilla, R.; Flores-Opazo, M.; Cano-Montoya, J.; Ciolac, E.G. Low-Volume High-Intensity Interval Training as a Therapy for Type 2 Diabetes. Int. J. Sports Med. 2016, 37, 723–729. [Google Scholar] [CrossRef]
- Hannan, A.L.; Hing, W.; Simas, V.; Climstein, M.; Coombes, J.S.; Jayasinghe, R.; Byrnes, J.; Furness, J. High-intensity interval training versis moderate-intensity continuous training within cardiac rehabilitation: A systematic review and meta-analysis. Open Access J. Sports Med. 2018, 9, 1–17. [Google Scholar] [CrossRef]
- Araujo, B.T.S.; Leite, J.C.; Furazo, H.K.B.; de Souza, R.J.P.; Remígio, M.I.; de Andrade, A.D.; Campos, S.L.; Brandāo, D.C. Influence of High-Intensity Interval Training Versus Continuous Training on Functional Capacity in Individuals with Heart Failure: A Systematic Review and Meta-analysis. J. Cardiopulm. Rehabil. Prev. 2019, 39, 293–298. [Google Scholar] [CrossRef]
- Liou, K.; Ho, S.; Fildes, J.; Ooi, S. High Intensity Interval versus Moderate Intensity Continuous Training in Patients with Coronary Artery Disease: A Meta-analysis of Physiological and Clinical Parameters. Heart Lung Circ. 2016, 25, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Aragão-Santos, J.C.; de Resende-Neto, A.G.; Nogueira, A.C.; Feitosa-Neta, M.L.; Brandão, L.H.; Chaves, L.M.; da Silva-Grogoletto, M.E. The effects of functional and traditional strength training on different strength parameters of elderly women: A randomized and controlled trial. J. Sports Med. Phys. Fit. 2019, 59, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA J. Am. Med. Assoc. 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Khalil, N.; Faulkner, K.A.; Greenspan, S.L.; Cauley, J.A. Osteoporotic Fractures in Men Research Group. Associations between bone mineral density, grip strength, and lead body burden in older men. J. Am. Geriatr. Soc. 2014, 62, 141–146. [Google Scholar] [CrossRef]
- Blain, H.; Jaussent, A.; Picot, M.-C.; Maimoun, L.; Coste, O.; Masud, T.; Bousquet, J.; Bernard, P.L. Effect of a 6-Month Brisk Walking Program on Walking Endurance in Sedentary and Physically Deconditioned Women Aged 60 or Older: A Randomized Trial. J. Nutr. Health Aging 2017, 21, 1183–1189. [Google Scholar] [CrossRef]
- Kim, J.; Shin, W. How to Do Random Allocation (Randomization). Clin. Orthop. Surg. 2014, 6, 103–109. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef]
- Boukabous, I.; Marcotte-Chénard, A.; Amamou, T.; Boulay, P.; Brochu, M.; Tessier, D.; Dionne, I.; Riesco, E. Low-Volume High-Intensity Interval Training (HIIT) versus Moderate-Intensity Continuous Training on Body Composition, Cardiometabolic Profile and Physical Capacity in Older Women. J. Aging Phys. Act. 2019, 29, 1–34. [Google Scholar] [CrossRef]
- García-Pinillos, F.; Laredo-Aguilera, J.A.; Muñoz-Jiménez, M.; Latorre-Román, P.A. Effects of 12-Week Concurrent High-Intensity Interval Strength and Endurance Training Program on Physical Performance in Healthy Older People. J. Strength Cond. Res. 2019, 33, 1445–1452. [Google Scholar] [CrossRef]
- Adamson, S.B.; Lorimer, R.; Cobley, J.N.; Babraj, J.A. Extremely Short-Duration High-Intensity Training Substantially Improves the Physical Function and Self-Reported Health Status of Elderly Adults. J. Am. Geriatr. Soc. 2014, 62, 1380–1381. [Google Scholar] [CrossRef] [PubMed]
- Correa, C.S.; LaRoche, D.P.; Cadore, E.L.; Reischak-Oliveira, A.; Bottaro, M.; Kruel, L.F.M.; Tartaruga, M.P.; RAdaelli, R.; Wilhelm, E.N.; Lacerda, F.C.; et al. 3 Different Types of Strength Training in Older Women. Int. J. Sports Med. 2012, 33, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Nawrocka, A.; Polechoński, J.; Garbaciak, W.; Mynarski, W. Functional Fitness and Quality of Life among Women over 60 Years of Age Depending on Their Level of Objectively Measured Physical Activity. Int. J. Environ. Res. Public Health 2019, 16, 972. [Google Scholar] [CrossRef] [PubMed]
- Sayers, S.P.; Gibson, K.; Mann, J.B. Improvement in functional performance with high-speed power training in older adults is optimized in those with the highest training velocity. Eur. J. Appl. Physiol. 2016, 116, 2327–2336. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-García, J.D.; Martínez-Amat, A.; De la Torre-Cruz, M.J.; Fábrega-Cuadros, R.; Cruz-Díaz, D.; Aibar-Almazán, A.; Achalandabaso-Ocho, A.; Hita-Contreras, F. Suspension Training HIIT Improves Gait Speed, Strength and Quality of Life in Older Adults. Int. J. Sports Med. 2019, 40, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Denison, H.J.; Syddall, H.E.; Dodds, R.; Martin, H.J.; Finucane, F.M.; Griffin, S.J.; Wareham, N.J.; Sayer, A.A. Effects of Aerobic Exercise on Muscle Strength and Physical Performance in Community-dwelling Older People from the Hertfordshire Cohort Study: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2013, 61, 1034–1036. [Google Scholar] [CrossRef] [PubMed]
- Sousa, N.; Mendes, R.; Silva, A.; Oliveira, J. Combined exercise is more effective than aerobic exercise in the improvement of fall risk factors: A randomized controlled trial in community-dwelling older men. Clin. Rehabil. 2017, 31, 478–486. [Google Scholar] [CrossRef]
- Shigematsu, R. Dance-based aerobic exercise may improve indices of falling risk in older women. Age Ageing 2002, 31, 261–266. [Google Scholar] [CrossRef]
- Carrasco-Poyatos, M.; Rubio-Arias, J.A.; Ballesta-García, I.; Ramos-Campo, D.J. Pilates vs. muscular training in older women. Effects in functional factors and the cognitive interaction: A randomized controlled trial. Physiol. Behav. 2019, 201, 157–164. [Google Scholar] [CrossRef]
- Charlton, K.; Batterham, M.; Langford, K.; Lateo, J.; Brock, E.; Walton, K.; Lyons-Wall, P.; Eisenhauer, K.; Green, N.; McLean, C. Lean Body Mass Associated with Upper Body Strength in Healthy Older Adults While Higher Body Fat Limits Lower Extremity Performance and Endurance. Nutrients 2015, 7, 7126–7142. [Google Scholar] [CrossRef]
- Granacher, U.; Muehlbauer, T.; Gruber, M. A qualitative review of balance and strength performance in healthy older adults: Impact for testing and training. J. Aging Res. 2012, 2012, 708905. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Lee, S.; Hotta, R.; Nakakubo, S.; Harada, K.; Lee, S.; Bae, S.; et al. Cognitive Functioning and Walking Speed in Older Adults as Predictors of Limitaitons in Self-Reported Instrumental Activity of Daily Libing-Prospective Fundings from the Obu Study of Helath Promotion for the Elderly. Int. J. Environ. Res. Public Health 2015, 12, 3002–3013. [Google Scholar] [CrossRef] [PubMed]
- Jaureguizar, K.V.; Vicente-Campos, D.; Bautista, L.R.; de la Peña, C.H.; Gómez, M.J.A.; Rueda, M.J.C.; Fernández-Maillo, I. Effect of High-Intensity Interval Versus Continuous Exercise Training on Functional Capacity and Quality of Life in Patients with Coronary Artery Disease: A Randomized Clinical Trial. J. Cardiopulm. Rehabil. Prev. 2016, 36, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Fleg, J.L. Aerobic exercise in the elderly: A key to successful aging. Discov. Med. 2012, 13, 223–228. [Google Scholar]
- Fraga, M.J.; Cader, S.A.; Ferreira, M.A.; Giani, T.S.; Dantas, E.H.M. Aerobic resistance, functional autonomy and quality of life (QoL) of elderly women impacted by a recreation and walking program. Arch. Gerontol. Geriatr. 2011, 52, e40–e43. [Google Scholar] [CrossRef]
- De Nardi, A.T.; Tolves, T.; Lenzi, T.L.; Signori, L.U.; Silva, A.M.V.D. High-intensity interval training versus continuous training on physiological and metabolic variables in prediabetes and type 2 diabetes: A meta-analysis. Diabetes Res. Clin. Pract. 2018, 137, 149–159. [Google Scholar] [CrossRef]
- Maillard, F.; Rousset, S.; Pereira, B.; Traore, A.; de Pradel, D.A.P.; Boirie, Y.; Duclos, M.; Boisseau, N. High-intensity interval training reduces abdominal fat mass in postmenopausal women with type 2 diabetes. Diabetes Metab. 2016, 42, 433–441. [Google Scholar] [CrossRef]
- Ramos, J.S.; Dalleck, L.C.; Borrani, F.; Beetham, K.S.; Wallen, M.P.; Mallard, A.R.; Clark, B.; Gomersall, S.; Keating, S.E.; Coombes, J.S. Low-Volume High-Intensity Interval Training Is Sufficient to Ameliorate the Severity of Metabolic Syndrome. Metab. Syndr. Relat. Disord. 2017, 15, 319–328. [Google Scholar] [CrossRef]
| Mesocycle | Group | Volume (min) | Work Effect (min) | Intensity (p) | Density (w/r) |
|---|---|---|---|---|---|
| Mesocycle 1 (weeks 3–6) | HIICT | 18–32 (6–8 intervals) | 6–12 | W: 14–15 Börg R: 7–8 Börg | 0.5–1 |
| MICT | 18–32 | 18–32 | 9–12 Börg | 1 | |
| Mesocycle 2 (weeks 7–10) | HIICT | 32–40 (9–10 intervals) | 12–15 | W: 15–16 Börg R: 7–8 Börg | 0.5–0.6 |
| MICT | 32–40 | 32–42 | 9–12 Börg | 1 | |
| Mesocycle 3 (weeks 11–14) | HIICT | 40 (8–10 intervals) | 10–15 | W: 16–18 Börg R: 9–10 Börg | 0.6 |
| MICT | 40 | 40 | 11–13 Börg | 1 | |
| Mesocycle 4 (weeks 15–18) | HIICT | 28–40 (8–12 intervals) | 15–18 | W: 16–18 Börg R: 10–11 Börg | 0.6–0.75 |
| MICT | 40–50 | 40–50 | 12–14 Börg | 1 |
| Mesocycle | HIICT | MICT |
|---|---|---|
| Mesocycle 1 (weeks 3–6) | work: grapevine; squat; step-touch; side step; swinging | grapevine; squat; gait; step-touch; side step; mambo cha-cha-cha; swinging |
| rest: gait; mambo cha-cha-cha | ||
| Mesocycle 2 (weeks 7–10) | work: grapevine with shoulder and elbow flexion; step-touch with shoulder and elbow flexion; knee-up; chasse; squats with shoulder-up | grapevine with shoulder and elbow flexion; step-touch with shoulder and elbow flexion; gait; knee-up; chasse; squats with shoulder-up; jogging |
| rest: gait; jogging | ||
| Mesocycle 3 (weeks 11–14) | work: grapevine with shoulder and elbow flexion and external load; jumping jack; step-touch with shoulder and elbow flexion and external load; chasse with shoulder-up. | grapevine with shoulder and elbow flexion and external load; chasse; jogging; step-touch with shoulder and elbow flexion and external load; chasse with shoulder-up; walking |
| rest: jogging; fast walking | ||
| Mesocycle 4 (weeks 15–18) | work: jumping jack with external load; grapevine with shoulder and elbow flexion and external load; knee-up with shoulder and elbow flexion and external load; hamstring curl with shoulder and elbow flexion and external load | step-touch with shoulder and elbow flexion and external load; grapevine with shoulder and elbow flexion and external load; knee-up with shoulder and elbow flexion and external load; hamstring curl with shoulder and elbow flexion and external load; walking; hops |
| rest: fast walking; hops |
| Group | n | Mean | SD | Min | Max | p |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| CG | 18 | 67.4 | 5.71 | 59 | 75 | 0.370 |
| MICT | 18 | 70 | 8.76 | 55 | 86 | |
| HIICT | 18 | 66.3 | 5.44 | 57 | 76 | |
| Body Mass Index (kg/m2) | ||||||
| CG | 18 | 31.2 | 4.89 | 20.9 | 38.4 | 0.689 |
| MICT | 18 | 30.1 | 3.08 | 24.3 | 35.9 | |
| HIICT | 18 | 30.4 | 4.13 | 35.2 | 37.7 | |
| Arm Curl Test (rep) | ||||||
| CG | 18 | 20.6 | 2.96 | 17.5 | 28.0 | 0.102 |
| MICT | 18 | 25.6 | 5.20 | 15.5 | 35.5 | |
| HIICT | 18 | 28.9 | 5.17 | 18.5 | 40.0 | |
| 30 Sit-To-Stand (rep) | ||||||
| CG | 18 | 16.8 | 2.90 | 11 | 22 | 0.140 |
| MICT | 18 | 13.7 | 3.38 | 6 | 18 | |
| HIICT | 18 | 15.1 | 2.69 | 10 | 19 | |
| Timed Up and Go test (s) | ||||||
| CG | 18 | 5.89 | 0.74 | 4.94 | 7.46 | 0.070 |
| MICT | 18 | 6.40 | 1.23 | 4.73 | 9.30 | |
| HIICT | 18 | 6.08 | 1.31 | 4.51 | 9.30 | |
| 6-Minute Walking Test (m) | ||||||
| CG | 18 | 510 | 59.0 | 410 | 590 | 0.135 |
| MICT | 18 | 502 | 72.3 | 355 | 636 | |
| HIICT | 18 | 564 | 41.0 | 455 | 625 | |
| One Leg Stand test with right leg (s) | ||||||
| CG | 18 | 19.6 | 9.09 | 5.89 | 30 | <0.001 |
| MICT | 18 | 21.6 | 11.20 | 3.00 | 30 | |
| HIICT | 18 | 26.9 | 7.75 | 2.00 | 30 | |
| One Leg Stand test with left leg (s) | ||||||
| CG | 18 | 15.1 | 9.10 | 1.98 | 30 | <0.001 |
| MICT | 18 | 19.9 | 10.00 | 2.00 | 30 | |
| HIICT | 18 | 27.4 | 6.87 | 2.00 | 30 | |
| Right Handgrip Strength (kg) | ||||||
| CG | 18 | 23.0 | 4.21 | 16.0 | 31.0 | 0.345 |
| MICT | 18 | 23.6 | 5.10 | 16.0 | 36.0 | |
| HIICT | 18 | 25.8 | 3.77 | 20.0 | 34.5 | |
| Left Handgrip Strength (kg) | ||||||
| CG | 18 | 21.4 | 4.06 | 14.0 | 29.0 | 0.904 |
| MICT | 18 | 22.3 | 4.01 | 16.5 | 31.0 | |
| HIICT | 18 | 25.0 | 3.49 | 20.0 | 32.5 | |
| Heart Rate during 6-Minute Walking Test (bpm) | ||||||
| CG | 18 | 34.9 | 14.8 | 15 | 57 | 0.684 |
| MICT | 18 | 26.7 | 14.7 | 5 | 59 | |
| HIICT | 18 | 34.8 | 17.1 | −15 | 65 | |
| Group | Increment | ANCOVA Interactions (F, p, ES η²) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (ITT) | n (Treated) | Mean | SD | Training × Group | Training × Baseline | Training × Age | |||||||
| F | p | ES η² | F | p | ES η² | F | p | ES η² | |||||
| Arm Curl Test (rep) | |||||||||||||
| CG | 18 | 12 | 1.80 | −0.10 | 8.1 | 8.99 × 10−4 2,3 | 0.192 | 18.3 | 8.51 × 10−5 | 0.217 | 9.85 × 10−3 | 0.921 | 0.000 |
| MICT | 18 | 12 | −0.50 | −1.14 | |||||||||
| HIICT | 18 | 17 | 2.80 | 0.28 | |||||||||
| 30 Sit-To-Stand (rep) | |||||||||||||
| CG | 18 | 12 | −1.90 | −0.05 | 17.42 | 1.81 × 10−6 1,2 | 0.381 | 6.54 | 1.36 × 10−2 | 0.072 | 0.353 | 0.555 | 0.004 |
| MICT | 18 | 12 | 3.80 | 1.47 | |||||||||
| HIICT | 18 | 17 | 5.60 | 0.47 | |||||||||
| Timed Up and Go Test (s) | |||||||||||||
| CG | 18 | 12 | 0.36 | 0.16 | 11.41 | 8.30 × 10−5 1,2 | 0.281 | 8.45 | 5.42 × 10−3 | 0.104 | 0.274 | 0.603 | 0.004 |
| MICT | 18 | 12 | −0.87 | 0.05 | |||||||||
| HIICT | 18 | 17 | −0.78 | −0.51 | |||||||||
| 6-Minute Walking Test (m) | |||||||||||||
| CG | 18 | 12 | −16 | −9.50 | 9.34 | 3.57 × 10−4 1,2 | 0.256 | 4.42 | 4.05 × 10−2 | 0.060 | 0.274 | 0.603 | 0.004 |
| MICT | 18 | 12 | 43 | 0.30 | |||||||||
| HIICT | 18 | 17 | 36 | 33.9 | |||||||||
| One Leg Stand Test with Right Leg (s) | |||||||||||||
| CG | 18 | 12 | 1.70 | 1.91 | 2.38 | 0.102 | 0.086 | 4.03 | 0.050 | 0.07 | 2.48 | 0.122 | 0.044 |
| MICT | 18 | 12 | 1.10 | −1.32 | |||||||||
| HIICT | 18 | 17 | −1.60 | 1.12 | |||||||||
| One Leg Stand Test with Left Leg (s) | |||||||||||||
| CG | 18 | 12 | −3.40 | 1.80 | 1.9 | 0.160 | 0.069 | 4.07 | 0.049 | 0.067 | 0.017 | 0.895 | 0.000 |
| MICT | 18 | 12 | 0.90 | 1.00 | |||||||||
| HIICT | 18 | 17 | −2.60 | 1.87 | |||||||||
| Group | n (ITT) | n (Treated) | Increment | ANCOVA Interactions (F, p, ES η²) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Training × Group | Training × Baseline | Training × Age | |||||||||
| F | p | ES η² | F | p | ES η² | F | p | ES η² | |||||
| Body Mass Index (kg/m2) | |||||||||||||
| CG | 18 | 12 | 0.30 | −0.05 | 6.99 | 0.002 2 | 0.215 | 3.02 | 0.088 | 0.046 | 0.217 | 0.643 | 0.003 |
| MICT | 18 | 12 | −0.10 | 1.47 | |||||||||
| HIICT | 18 | 17 | −0.30 | 0.47 | |||||||||
| Right Handgrip Strength (kg) | |||||||||||||
| CG | 18 | 12 | 0.60 | −0.86 | 0.881 | 0.420 | 0.033 | 9.72 | 3.02 × 10−3 | 0.155 | 1.45 | 0.233 | 0.028 |
| MICT | 18 | 12 | −0.40 | 0.49 | |||||||||
| HIICT | 18 | 17 | 0.60 | −0.68 | |||||||||
| Left Handgrip Strength (kg) | |||||||||||||
| CG | 18 | 12 | 0.90 | 0.04 | 1.46 | 0.243 | 0.054 | 1.39 | 0.244 | 0.026 | 1.13 | 0.293 | 0.021 |
| MICT | 18 | 12 | −0.20 | 0.74 | |||||||||
| HIICT | 18 | 17 | 0.60 | 0.87 | |||||||||
| Heart Rate during 6-Minute Walking Test (bpm) | |||||||||||||
| CG | 18 | 12 | −3 | −9.50 | 1 | 0.375 | 0.038 | 13.39 | 6.08 × 10−4 | 0.197 | 1.74 | 0.193 | 0.032 |
| MICT | 18 | 12 | 2 | 0.30 | |||||||||
| HIICT | 18 | 17 | 6 | 33.90 | |||||||||
| Group | Pre-Training | Post-Training | p | 95% CI for MD | Cohen’s d | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Lower | Upper | |||
| Arm Curl Test (rep) | ||||||||||
| CG | 18 | 20.6 | 2.96 | 12 | 22.4 | 2.86 | 2.04 × 10−4 | −2.61 | −0.99 | 0.57 |
| MICT | 18 | 25.6 | 5.20 | 12 | 25.1 | 4.06 | 0.575 | −1.34 | 2.34 | 0.09 |
| HIICT | 18 | 28.9 | 5.17 | 17 | 31.7 | 5.45 | 0.022 | −5.09 | −0.45 | 0.52 |
| 30 Sit-To-Stand (rep) | ||||||||||
| CG | 18 | 16.8 | 2.90 | 12 | 14.9 | 2.85 | 1.40 × 10−4 | 1.07 | 2.70 | 0.61 |
| MICT | 18 | 13.7 | 3.38 | 12 | 17.5 | 4.85 | 3.20 × 10−4 | −5.65 | −2.01 | 1.05 |
| HIICT | 18 | 15.1 | 2.69 | 17 | 20.7 | 3.16 | 1.00 × 10−6 | −7.13 | −4.08 | 1.98 |
| Timed Up and Go Test (s) | ||||||||||
| CG | 18 | 5.89 | 0.74 | 12 | 6.25 | 0.89 | 0.016 | −0.64 | −0.07 | 0.46 |
| MICT | 18 | 6.40 | 1.23 | 12 | 5.53 | 1.28 | 0.001 | 0.38 | 1.34 | 0.66 |
| HIICT | 18 | 6.08 | 1.31 | 17 | 5.30 | 0.80 | 0.009 | 0.21 | 1.35 | 0.57 |
| 6-Minute Walking Test (m) | ||||||||||
| CG | 18 | 510 | 59.0 | 12 | 494 | 49.5 | 0.058 | −0.60 | 33.39 | 0.25 |
| MICT | 18 | 502 | 72.3 | 12 | 545 | 72.6 | 3.09 × 10−4 | −61.94 | −22.46 | 0.55 |
| HIICT | 18 | 564 | 41.0 | 17 | 600 | 74.9 | 0.036 | −8.65 | −2.57 | 0.84 |
| One Leg Stand Test with Right Leg (s) | ||||||||||
| CG | 18 | 19.6 | 9.09 | 12 | 21.3 | 11.00 | 0.233 | −4.57 | 1.19 | 0.17 |
| MICT | 18 | 21.6 | 11.20 | 12 | 22.7 | 9.88 | 0.237 | −3.06 | 0.81 | 0.99 |
| HIICT | 18 | 26.9 | 7.75 | 17 | 25.3 | 8.87 | 0.024 | 0.24 | 3.10 | 0.20 |
| One Leg Stand Test with Left Leg (s) | ||||||||||
| CG | 18 | 15.1 | 9.1 | 12 | 11.7 | 10.90 | 0.129 | −1.08 | 7.79 | 0.35 |
| MICT | 18 | 19.9 | 10.0 | 12 | 20.80 | 11.00 | 0.486 | −3.54 | 1.75 | 0.08 |
| HIICT | 18 | 27.4 | 6.87 | 17 | 24.80 | 8.74 | 0.124 | −0.80 | 6.05 | 0.36 |
| Group | Pre-Training | Post-Training | p | 95% CI for MD | Cohen’s d | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Lower | Upper | |||
| Body Mass Index (kg/m2) | ||||||||||
| CG | 18 | 31.2 | 4.89 | 12 | 31.5 | 5.05 | 0.019 | −0.52 | −0.53 | 0.06 |
| MICT | 18 | 30.1 | 3.08 | 12 | 30.0 | 3.15 | 0.140 | −0.02 | 0.29 | 0.03 |
| HIICT | 18 | 30.4 | 4.13 | 17 | 30.1 | 4.24 | 0.035 | 0.02 | 0.60 | 0.07 |
| Right Handgrip Strength (kg) | ||||||||||
| CG | 18 | 23.0 | 4.21 | 12 | 23.6 | 3.35 | 0.155 | −1.54 | 0.26 | 0.13 |
| MICT | 18 | 23.6 | 5.1 | 12 | 23.2 | 5.59 | 0.650 | −1.38 | 2.16 | 0.07 |
| HIICT | 18 | 25.8 | 3.77 | 17 | 26.4 | 3.09 | 0.397 | −1.80 | 0.75 | 0.15 |
| Left Handgrip Strength (kg) | ||||||||||
| CG | 18 | 21.4 | 4.06 | 12 | 22.3 | 4.10 | 0.219 | −2.28 | 0.56 | 0.21 |
| MICT | 18 | 22.3 | 4.01 | 12 | 22.1 | 4.75 | 0.656 | −0.91 | 1.41 | 0.05 |
| HIICT | 18 | 25 | 3.49 | 17 | 25.6 | 4.36 | 0.229 | −1.64 | 0.42 | 0.16 |
| Heart Rate during 6-Minute Walking Test (bpm) | ||||||||||
| CG | 18 | 34.90 | 14.80 | 12 | 31.7 | 12.30 | 0.303 | −3.179 | 9.624 | 0.21 |
| MICT | 18 | 26.70 | 14.70 | 12 | 28.7 | 12.30 | 0.565 | −9.184 | 5.184 | 0.13 |
| HIICT | 18 | 34.80 | 17.10 | 17 | 40.6 | 14.20 | 0.137 | −13.582 | 2.027 | 0.32 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ballesta-García, I.; Martínez-González-Moro, I.; Rubio-Arias, J.Á.; Carrasco-Poyatos, M. High-Intensity Interval Circuit Training Versus Moderate-Intensity Continuous Training on Functional Ability and Body Mass Index in Middle-Aged and Older Women: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 4205. https://doi.org/10.3390/ijerph16214205
Ballesta-García I, Martínez-González-Moro I, Rubio-Arias JÁ, Carrasco-Poyatos M. High-Intensity Interval Circuit Training Versus Moderate-Intensity Continuous Training on Functional Ability and Body Mass Index in Middle-Aged and Older Women: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2019; 16(21):4205. https://doi.org/10.3390/ijerph16214205
Chicago/Turabian StyleBallesta-García, Ismael, Ignacio Martínez-González-Moro, Jacobo Á. Rubio-Arias, and María Carrasco-Poyatos. 2019. "High-Intensity Interval Circuit Training Versus Moderate-Intensity Continuous Training on Functional Ability and Body Mass Index in Middle-Aged and Older Women: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 16, no. 21: 4205. https://doi.org/10.3390/ijerph16214205
APA StyleBallesta-García, I., Martínez-González-Moro, I., Rubio-Arias, J. Á., & Carrasco-Poyatos, M. (2019). High-Intensity Interval Circuit Training Versus Moderate-Intensity Continuous Training on Functional Ability and Body Mass Index in Middle-Aged and Older Women: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 16(21), 4205. https://doi.org/10.3390/ijerph16214205







