Effects of Fall Training Program on Automatization of Safe Motor Responses during Backwards Falls in School-Age Children
Abstract
:1. Introduction
2. Materials and Methods
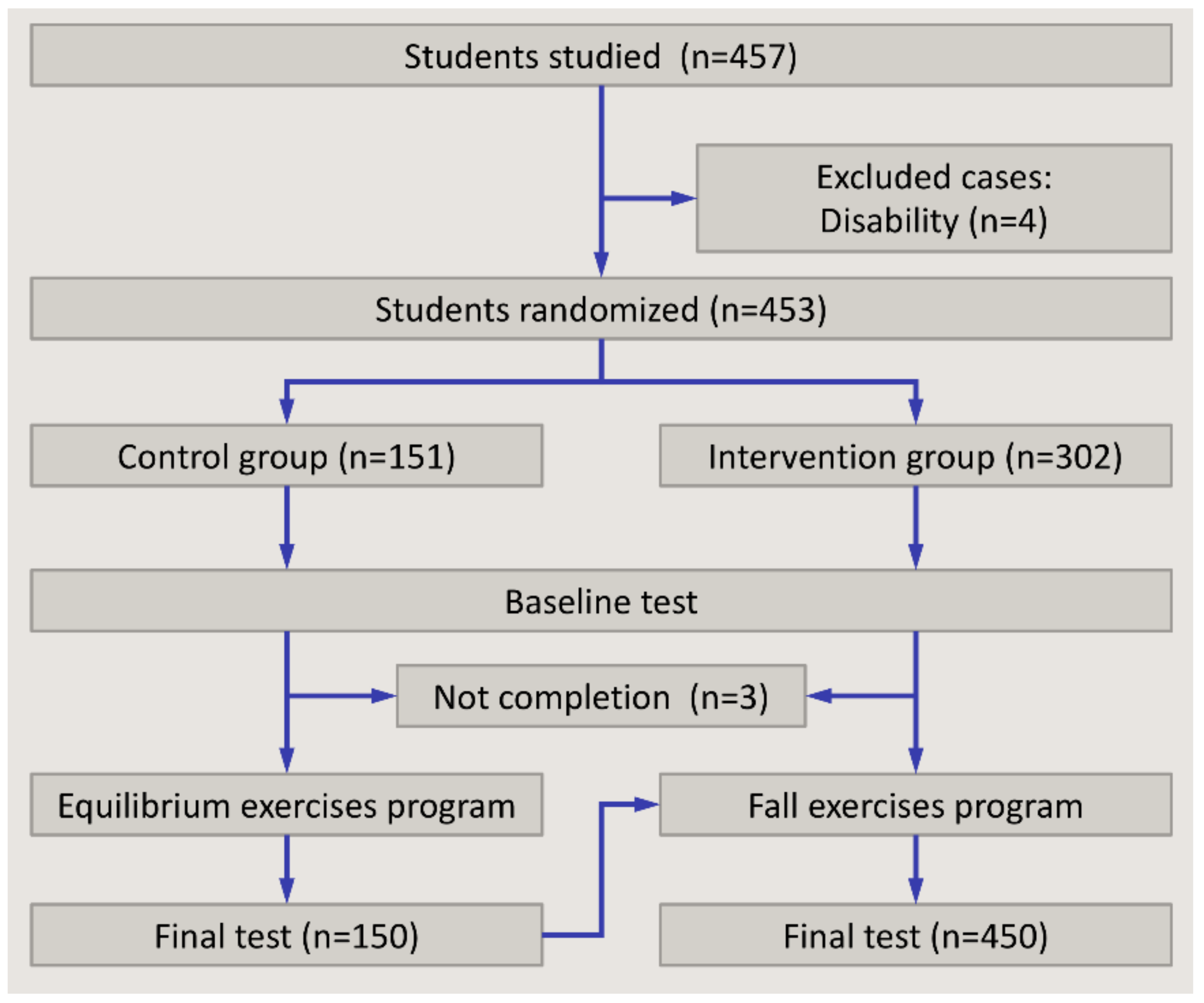
2.1. Sample
2.2. Structure
2.3. Blinding
2.4. Ethics Approval
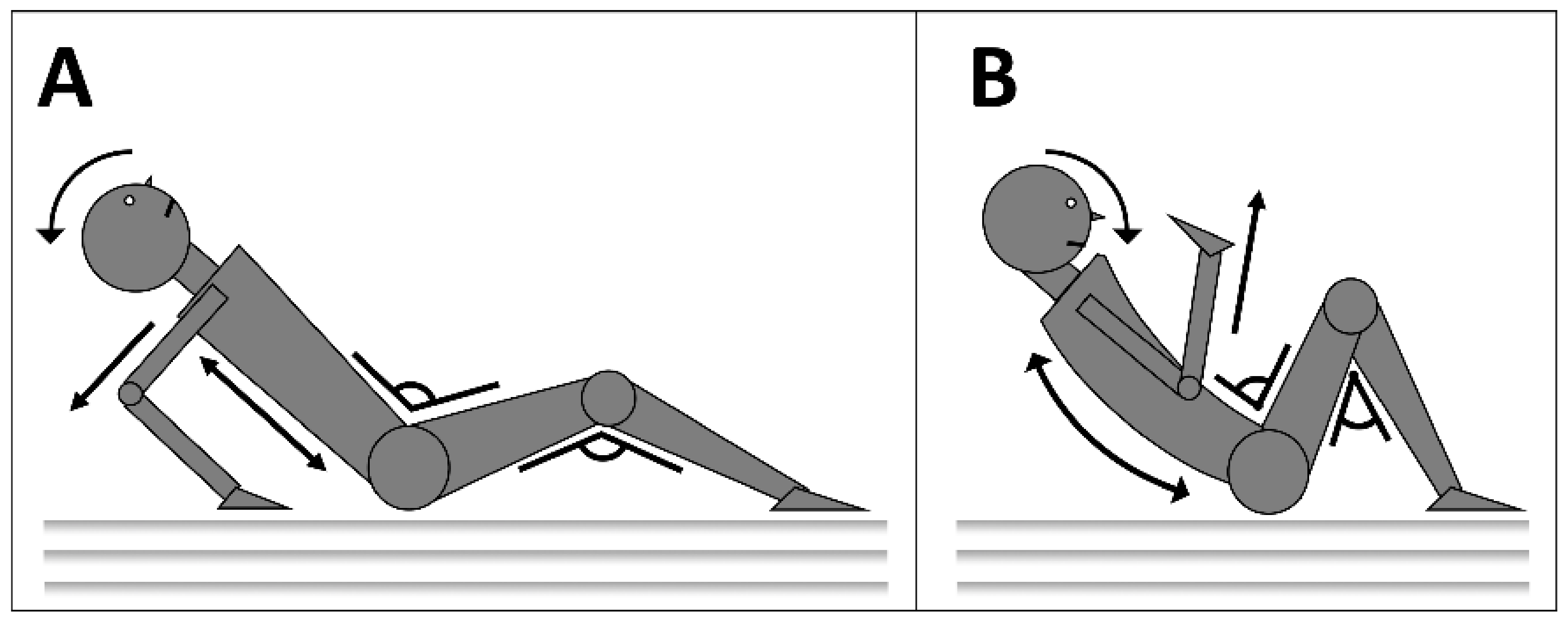
2.5. Implementation of the Safe Fall Program and Assessments
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
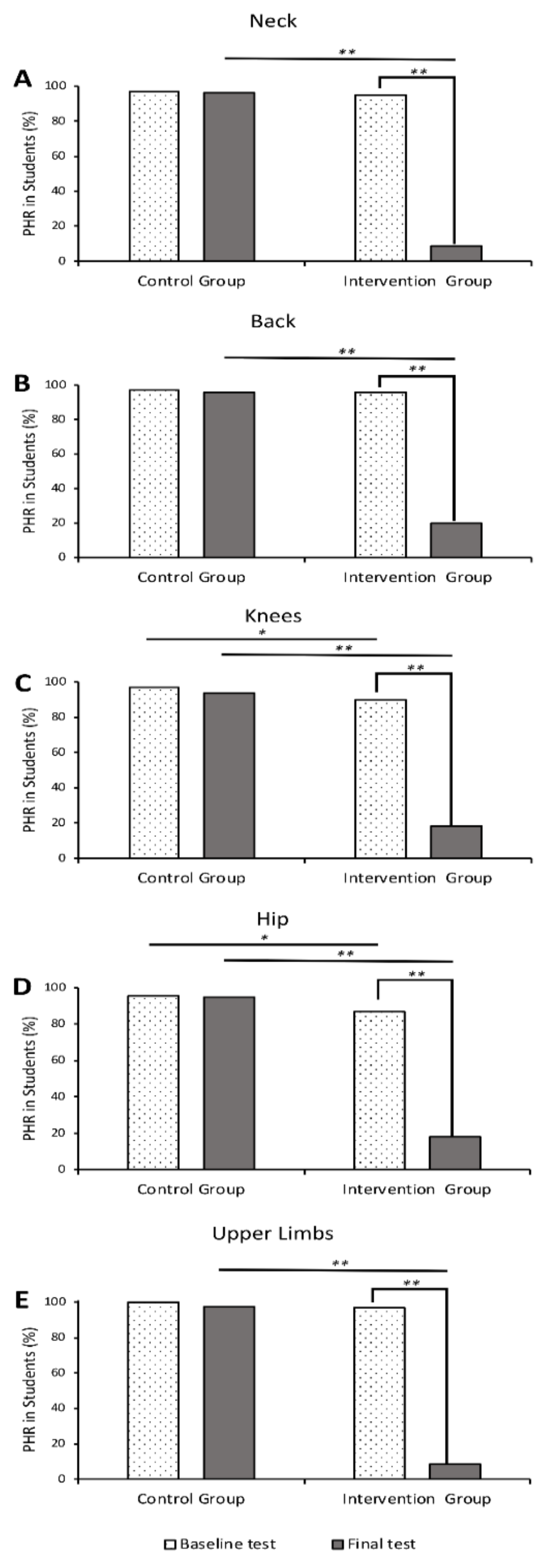
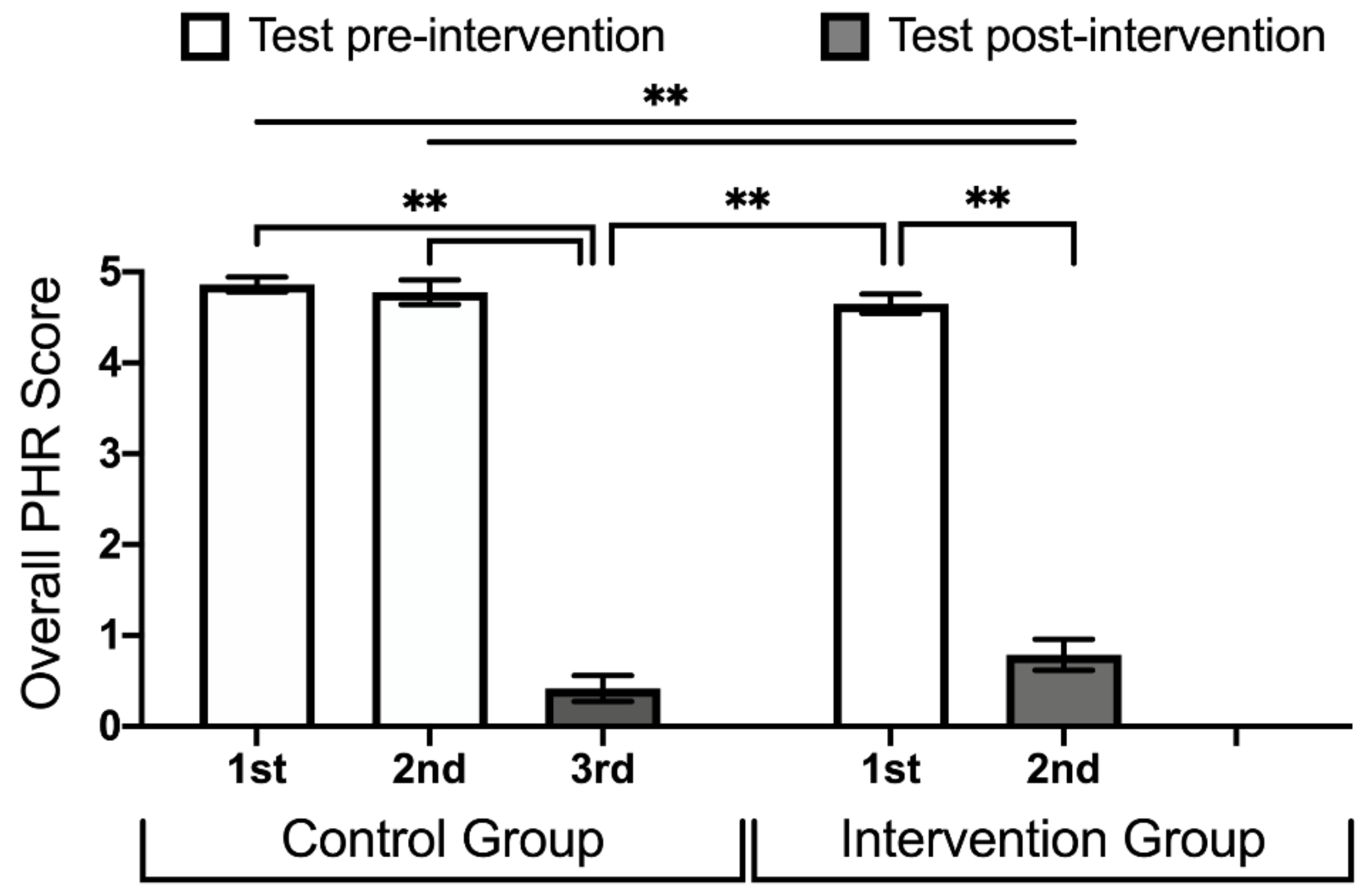
3.2. Effect of the Safe Fall Program on PHR
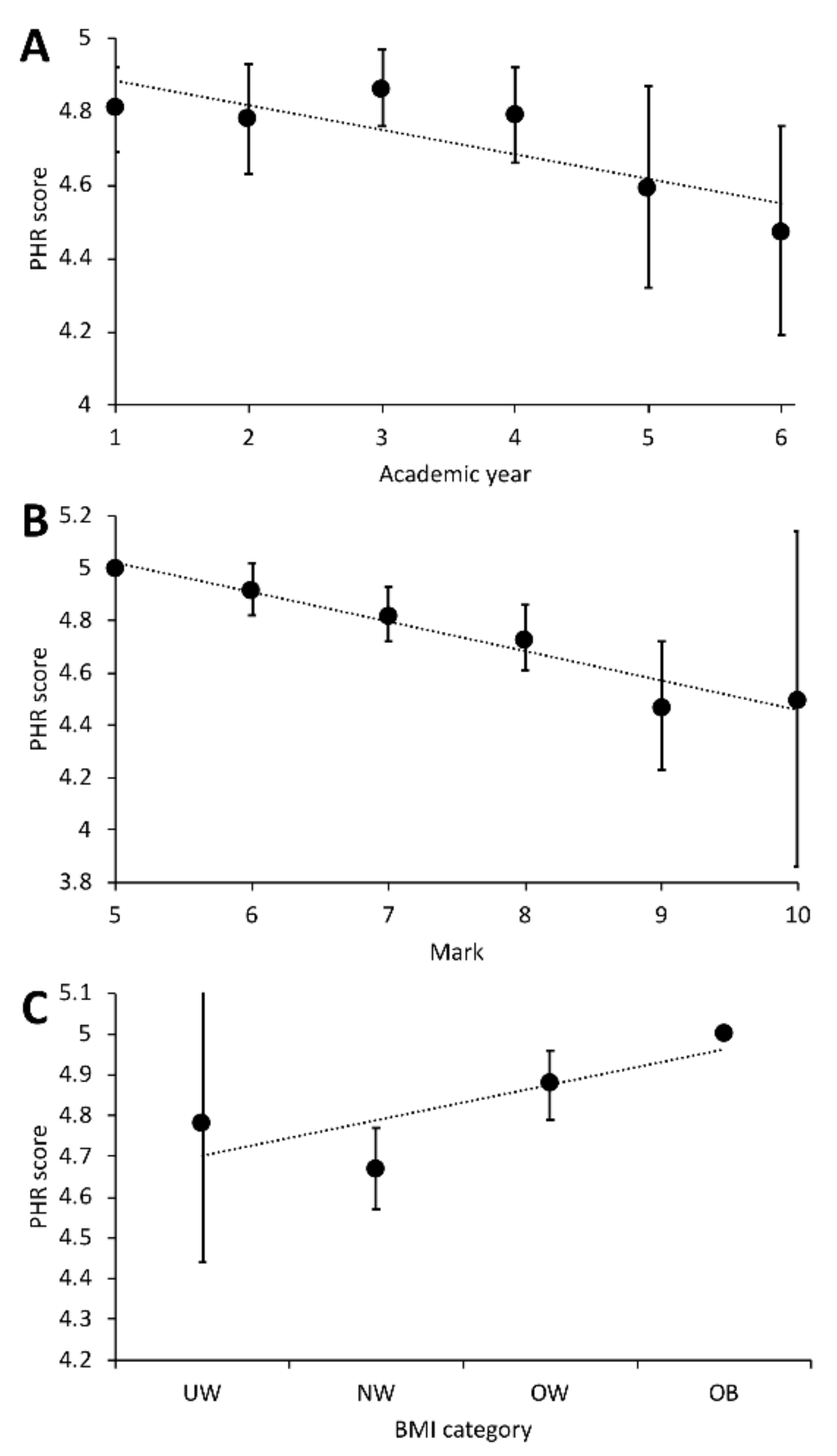
3.3. Effects of Different Variables on the Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- MacKay, M.; Vincente, J. Child Safety Report Card 2012 Europe Summary for 31 Countries. Eur. Child Saf. Alliance 2012. Available online: https://www.childsafetyeurope.org/publications/info/child-safety-report-cards-europe-summary-2012.pdf (accessed on 10 September 2019).
- Anderson, V.A.; Anderson, P.; Northam, E.; Jacobs, R.; Catroppa, C. Development of Executive Functions Through Late Childhood and Adolescence in an Australian Sample. Dev. Neuropsychol. 2001, 20, 385–406. [Google Scholar] [CrossRef]
- Frick, A.; Möhring, W. A Matter of Balance: Motor Control is Related to Children’s Spatial and Proportional Reasoning Skills. Front. Physiol. 2016, 6, 2049. [Google Scholar] [CrossRef]
- Bahr, R.; Clarsen, B.; Ekstrand, J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br. J. Sports Med. 2018, 52, 14–17. [Google Scholar] [CrossRef]
- Ishikawa, T.; Mâsse, L.C.; Brussoni, M. Changes in parents’ perceived injury risk after a medically-attended injury to their child. Prev. Med. Rep. 2019, 13, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Beck, B.; Teague, W.; Cameron, P.; Gabbe, B.J. Causes and characteristics of injury in paediatric major trauma and trends over time. Arch. Dis. Child. 2019, 104, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Eager, D.; Hayati, H. Additional Injury Prevention Criteria for Impact Attenuation Surfacing Within Children’s Playgrounds. J. Risk Uncertain. Eng. Syst. Part B Mech. Eng. 2019, 5, 011002. [Google Scholar] [CrossRef]
- Bierbaum, M.; Curtis, K.; Mitchell, R. Incidence and cost of hospitalisation of children with injuries from playground equipment falls in New South Wales, Australia. J. Paediatr. Child Health 2018, 54, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Mroczkowski, A.; Sikorski, M.M. The susceptibility to body injuries during a fall and abilities related to motor coordination of children aged 10 to 12. Arch. Judo Sci. Martial Arts Extrem. Sport 2015, 11, 65–71. [Google Scholar]
- Rössler, R.; Verhagen, E.; Rommers, N.; Dvorak, J.; Junge, A.; Lichtenstein, E.; Donath, L.; Faude, O. Comparison of the ‘ 11 + Kids ’ injury prevention programme and a regular warmup in children’s football (soccer ): A cost effectiveness analysis. Br. J. Sports Med. 2019, 53, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Nauta, J.; Knol, D.L.; Adriaensens, L.; Wolt, K.K.; Van Mechelen, W.; Verhagen, E.A. Prevention of fall-related injuries in 7-year-old to 12-year-old children: A cluster randomised controlled trial. Br. J. Sports Med. 2013, 47, 909–913. [Google Scholar] [CrossRef] [PubMed]
- DelCastillo-Andrés, Ó.; Toronjo-Hornillo, L.; Rodríguez-López, M.; Castañeda-Vázquez, C.; Campos-Mesa, M. Children’s Improvement of a Motor Response during Backward Falls through the Implementation of a Safe Fall Program. Int. J. Environ. Res. Publich Health 2018, 15, 2669. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.Y.; Davids, K.; Button, C.; Shuttleworth, R.; Renshaw, I.; Araújo, D. The role of nonlinear pedagogy in physical education. Rev. Educ. Res 2007, 77, 251–278. [Google Scholar] [CrossRef]
- De Domingo, A.J.; García, E.R.; Pardillo, R.M.; Constanti, V.A.; Haiek, L.A.; Arola, M.S.; Oliveras, F.R.; García, C.R.; Ferrer, G.E.; Romero, J.L. Epidemiología y factores de riesgo de las lesiones por caídas en niños menores de un año. Pediatría 2017, 86, 337–343. [Google Scholar] [CrossRef]
- Pacheco, N.G.; Pardillo, R.M.; De Gracia Calvo, P.S.; Calleja, C.C.; Muñoz, E.M.; Sáez, M.R.; Rupérez, E.C.; Occhiuzzo, F.P.; Sáez, C.D.; Martínez-Páis, V.B.; et al. Accidentes de bicicleta atendidos en los Servicios de Urgencias. Estudio multicéntrico. Pediatría 2014, 80, 242–248. [Google Scholar]
- Gelfman, D.M.G.; Ledesma, J.; Hauier, F.; Volonté, P.; Orbe, G.; Fiorentino, J.A. Trauma por caída de altura en pediatría. Arch. Argent. Pediatr. 2005, 103, 414–419. [Google Scholar]
- Moon, Y.; Sosnoff, J.J. Safe Landing Strategies During a Fall: Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 783–794. [Google Scholar] [CrossRef] [PubMed]
- Bloemers, F.; Collard, D.; Paw, M.C.A.; Van Mechelen, W.; Twisk, J.; Verhagen, E. Physical inactivity is a risk factor for physical activity-related injuries in children. Br. J. Sports Med. 2012, 46, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Kalina, R.M.; Mosler, D. Risk of Injuries Caused by Fall of People Differing in Age, Sex, Health and Motor Experience. In Proceedings of the AHFE 2017 International Conference on Human Factors in Sports, Injury Prevention and Outdoor Recreation, Los Angeles, CA, USA, 17–21 July 2017; Volume 603. [Google Scholar]
- Morrongiello, B.A.; Corbett, M. Parents’ perspectives on preschool children’s in-home falls: Implications for injury prevention. Vulnerable Child. Youth Stud. 2016, 11, 136–145. [Google Scholar] [CrossRef]
- Shi, X.; Wang, T.; Nie, C.; Wang, H.; Luo, L.; Qi, Y.; Jiang, Z. Epidemiologic features and intervention effect of fall injury among rural school-aged children in southwest China: A short-term cohort study. Int. J. Inj. Contr. Saf. Promot. 2018, 25, 439–442. [Google Scholar] [CrossRef]
- Olsen, L.; Brussoni, M.; Ishikawa, T.; Mâsse, L.; Chan, G. Development and validation of a survey on fathers’ attitudes towards child injury prevention. Inj. Prev. 2016, 22, A330. [Google Scholar] [CrossRef]
- Nilsen, P.; Yorkston, E. Uncovering evidence on community-based injury prevention: A review of programme effectiveness and factors influencing effectiveness. Int. J. Inj. Contr. Saf. Promot. 2007, 14, 241–250. [Google Scholar] [CrossRef] [PubMed]
| Control | Intervention | p-Value | |
|---|---|---|---|
| Participants 3 | 151 (33) | 302 (67) | |
| Sex (Females) 3 | 77 (51.0) | 151 (50.0) | 0.921 a |
| Academic year 3 | 0.955 b | ||
| 1st | 25 (16.6) | 49 (16.2) | |
| 2nd | 26 (17.2) | 52 (17.2) | |
| 3rd | 26 (17.2) | 50 (16.6) | |
| 4th | 24 (15.9) | 53 (17.5) | |
| 5th | 25 (16.6) | 50 (16.6) | |
| 6th | 26 (17.2) | 48 (15.9) | |
| PE mark 1 | 7.72 (1.00) | 7.77 (1.06) | 0.529 c |
| BMI (kg/m2) 2 | 18.71 (18.15, 19.28) | 18.44 (18.02, 18.86) | 0.252 b |
| Categories 3 | 0.711 d | ||
| Underweight | 4 (2.7) | 6 (2.0) | |
| Normal | 114 (76.0) | 232 (77.3) | |
| Overweight | 29 (19.3) | 51 (17.0) | |
| Obese | 3 (2) | 11 (3.7) | |
| Sport participation 3 | 0.196 a | ||
| Low | 102 (67.5) | 180 (59.8) | |
| Moderate | 32 (21.2) | 87 (28.9) | |
| High | 16 (10.6) | 34 (11.3) |
| Variables | Baseline Test | Final Test |
|---|---|---|
| Sex | 0.739 | 0.296 |
| Academic year | 0.002 | 0.145 |
| PE mark | 0.025 | 0.747 |
| BMI | 0.015 | 0.233 |
| Sport participation | 0.617 | 0.607 |
| Intervention | 0.153 | <0.001 |
| Baseline | --- | 0.055 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
DelCastillo-Andrés, Ó.; Toronjo-Hornillo, L.; Toronjo-Urquiza, L. Effects of Fall Training Program on Automatization of Safe Motor Responses during Backwards Falls in School-Age Children. Int. J. Environ. Res. Public Health 2019, 16, 4078. https://doi.org/10.3390/ijerph16214078
DelCastillo-Andrés Ó, Toronjo-Hornillo L, Toronjo-Urquiza L. Effects of Fall Training Program on Automatization of Safe Motor Responses during Backwards Falls in School-Age Children. International Journal of Environmental Research and Public Health. 2019; 16(21):4078. https://doi.org/10.3390/ijerph16214078
Chicago/Turabian StyleDelCastillo-Andrés, Óscar, Luis Toronjo-Hornillo, and Luis Toronjo-Urquiza. 2019. "Effects of Fall Training Program on Automatization of Safe Motor Responses during Backwards Falls in School-Age Children" International Journal of Environmental Research and Public Health 16, no. 21: 4078. https://doi.org/10.3390/ijerph16214078
APA StyleDelCastillo-Andrés, Ó., Toronjo-Hornillo, L., & Toronjo-Urquiza, L. (2019). Effects of Fall Training Program on Automatization of Safe Motor Responses during Backwards Falls in School-Age Children. International Journal of Environmental Research and Public Health, 16(21), 4078. https://doi.org/10.3390/ijerph16214078





