A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
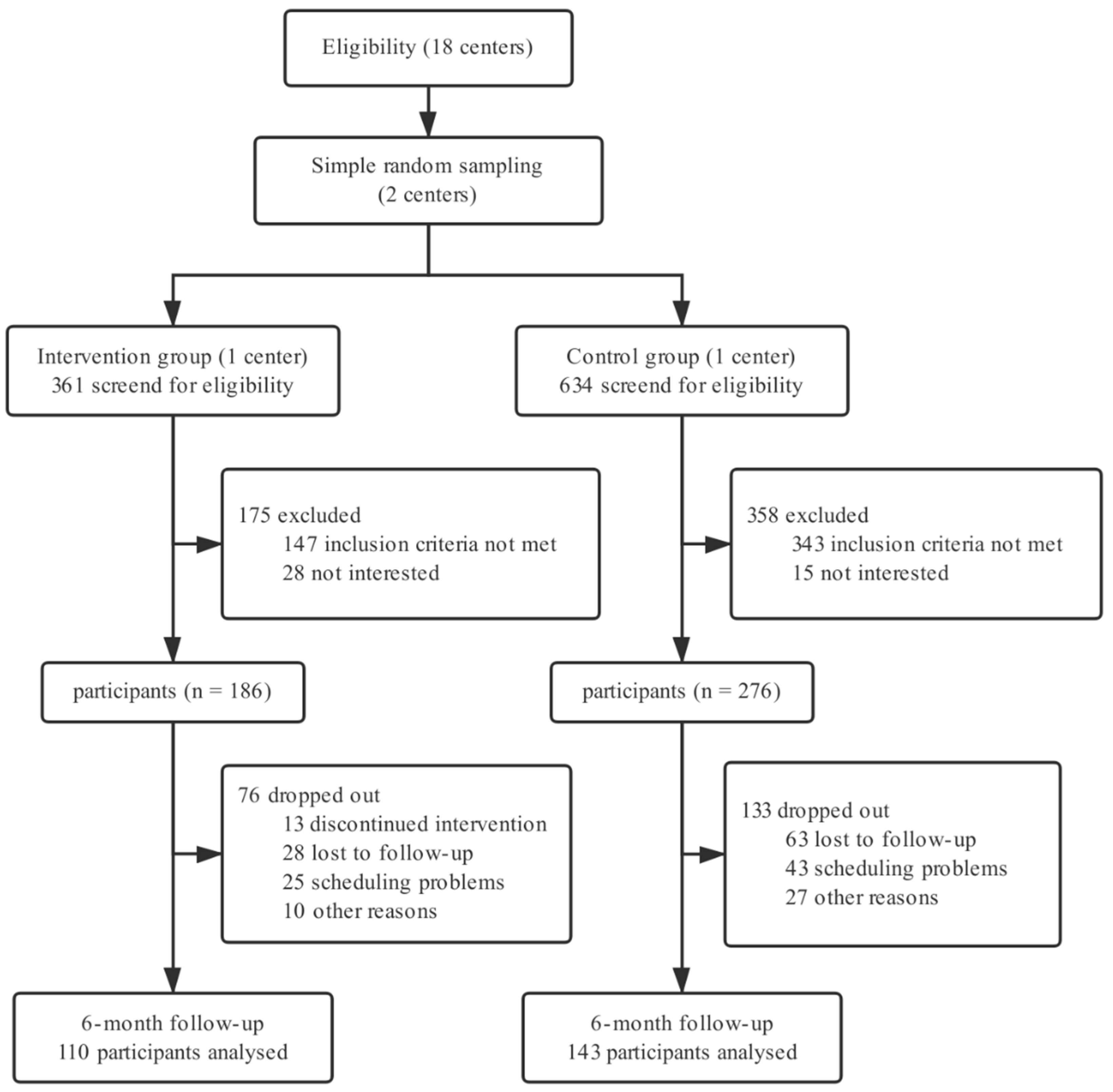
2.1. Study Design and Participants
2.2. Randomization
2.3. Intervention Program
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Follow-Up of Participants
3.3. Primary and Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of Hypertension in China: Results from the China Hypertension Survey, 2012–2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wu, S.; Wang, J.; Wang, W.; Bao, Y.; Cai, J.; Chen, L.; Chen, W.; Chu, S.; Feng, Y.; et al. 2018 Chinese guidelines for the management of hypertension. Chin. J. Cardiol. 2019, 24, 24–56. (In Chinese) [Google Scholar] [CrossRef]
- McManus, R.; Mant, J.; Bray, E.P.; Holder, R.; Jones, M.I.; Greenfield, S.; Kaambwa, B.; Banting, M.; Bryan, S.; Little, P.; et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): A randomised controlled trial. Lancet 2010, 376, 163–172. [Google Scholar] [CrossRef]
- Uhlig, K.; Patel, K.; Ip, S.; Kitsios, G.D.; Balk, E.M. Self-measured blood pressure monitoring in the management of hypertension: A systematic review and meta-analysis. Ann. Intern. Med. 2013, 159, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, N.N.; Hatcher, J.; Chaturvedi, N.; Jafar, T.H.; Hypertension Research, G. Effect of general practitioner education on adherence to antihypertensive drugs: Cluster randomised controlled trial. BMJ 2007, 335, 1030. [Google Scholar] [CrossRef]
- Tucker, K.L.; Sheppard, J.P.; Stevens, R.; Bosworth, H.B.; Bove, A.; Bray, E.P.; Earle, K.; George, J.; Godwin, M.; Green, B.B.; et al. Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis. PLoS Med. 2017, 14, e1002389. [Google Scholar] [CrossRef]
- Margolis, K.L.; Asche, S.E.; Bergdall, A.R.; Dehmer, S.P.; Groen, S.E.; Kadrmas, H.M.; Kerby, T.J.; Klotzle, K.J.; Maciosek, M.V.; Michels, R.D.; et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: A cluster randomized clinical trial. JAMA 2013, 310, 46–56. [Google Scholar] [CrossRef]
- McManus, R.J.; Mant, J.; Franssen, M.; Nickless, A.; Schwartz, C.; Hodgkinson, J.; Bradburn, P.; Farmer, A.; Grant, S.; Greenfield, S.M.; et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): An unmasked randomised controlled trial. Lancet 2018, 391, 949–959. [Google Scholar] [CrossRef]
- Watson, A.J.; Singh, K.; Myint, U.K.; Grant, R.W.; Jethwani, K.; Murachver, E.; Harris, K.; Lee, T.H.; Kvedar, J.C. Evaluating a web-based self-management program for employees with hypertension and prehypertension: A randomized clinical trial. Am. Heart J. 2012, 164, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Hui, C.Y.; Creamer, E.; Pinnock, H.; McKinstry, B. Apps to Support Self-Management for People with Hypertension: Content Analysis. JMIR Mhealth Uhealth 2019, 7, e13257. [Google Scholar] [CrossRef] [PubMed]
- Alessa, T.; Hawley, M.S.; Hock, E.S.; de Witte, L. Smartphone Apps to Support Self-Management of Hypertension: Review and Content Analysis. JMIR Mhealth Uhealth 2019, 7, e13645. [Google Scholar] [CrossRef] [PubMed]
- Number of Monthly Active WeChat Users from 2nd Quarter 2012 to 2nd Quarter 2019 (in Millions). Available online: https://www.statista.com/statistics/255778/number-of-active-wechat-messenger-accounts/ (accessed on 17 August 2019).
- Xia, J.; Hu, S.; Xu, J.; Hao, H.; Yin, C.; Xu, D. The correlation between glucose fluctuation from self-monitored blood glucose and the major adverse cardiac events in diabetic patients with acute coronary syndrome during a 6-month follow-up by WeChat application. Clin. Chem. Lab. Med. 2018, 56, 2119–2124. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Wu, S.; Zhao, Y.; Li, Z.; Zhang, Y.; Le, J.; Wang, L.; Wan, S.; Li, C.; Li, Y.; et al. Social Media-Promoted Weight Loss Among an Occupational Population: Cohort Study Using a WeChat Mobile Phone App-Based Campaign. J. Med. Internet Res. 2017, 19, e357. [Google Scholar] [CrossRef] [PubMed]
- Hou, L.; Jin, X.; Ma, J.; Qian, J.; Huo, Y.; Ge, J. Perception and self-management of hypertension in Chinese cardiologists (CCHS): A multicenter, large-scale cross-sectional study. BMJ Open 2019, 9, e029249. [Google Scholar] [CrossRef]
- Wang, J.G. Unique approaches to hypertension control in China. Ann. Transl. Med. 2018, 6, 296. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Li, T.; Ding, W.W.; Li, X.W.; Lin, A.H. Mobile health technology (WeChat) for the hierarchical management of community hypertension: Protocol for a cluster randomized controlled trial. Patient Prefer. Adher. 2019, 13, 1339–1352. [Google Scholar] [CrossRef]
- Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2018 Chinese guidelines for the management of hypertension. Chin. J. Cardiol. 2011, 39, 579–616. (In Chinese) [Google Scholar] [CrossRef]
- Wu, Z.; Huo, Y.; Wang, W.; Zhao, L.; Zhu, D. Chinese Guidelines for Patient Education of Hypertension. Chin. J. Front. Med. Sci. (Electron. Vers.) 2014, 3, 78–110. (In Chinese) [Google Scholar]
- Chen, J. Analysis and Intervention of Knowledge, Belief, Behavior in Elderly Patients with Primary Hypertension in Haizhu District of Guangzhou; Southern Medical University: Guangzhou, China, 2011. [Google Scholar]
- Zhao, Q.; Liu, X. Reliability and validity of the hypertension patients self-management behavior rating scale. Chin. Nurs. Manag. 2012, 12, 26–31. (In Chinese) [Google Scholar]
- Lan, G.; Yuan, Z.; Cook, A.; Xu, Q.; Jiang, H.; Zheng, H.; Wang, L.; Yuan, L.; Xie, X.; Lu, Y. The relationships among social support and quality of life in persons living with HIV/AIDS in Jiangxi and Zhejiang provinces, China. AIDS Care 2015, 27, 946–953. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Zhang, G.; Liu, Z.; Gu, J.; Chen, W.; Luo, F. Community-based lifestyle intervention for reducing blood pressure and glucose among middle-aged and older adults in China: A pilot study. Int. J. Environ. Res. Public Health 2014, 11, 11645–11663. [Google Scholar] [CrossRef]
- Collins, R.; Peto, R.; MacMahon, S.; Hebert, P.; Fiebach, N.H.; Eberlein, K.A.; Godwin, J.; Qizilbash, N.; Taylor, J.O.; Hennekens, C.H. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: Overview of randomised drug trials in their epidemiological context. Lancet 1990, 335, 827–838. [Google Scholar] [CrossRef]
- Staessen, J.A.; Gasowski, J.; Wang, J.G.; Thijs, L.; Den Hond, E.; Boissel, J.P.; Coope, J.; Ekbom, T.; Gueyffier, F.; Liu, L.; et al. Risks of untreated and treated isolated systolic hypertension in the elderly: Meta-analysis of outcome trials. Lancet 2000, 355, 865–872. [Google Scholar] [CrossRef]
- Law, M.R.; Morris, J.K.; Wald, N.J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009, 338, b1665. [Google Scholar] [CrossRef]
- Group, S.R.; Wright, J.T., Jr.; Williamson, J.D.; Whelton, P.K.; Snyder, J.K.; Sink, K.M.; Rocco, M.V.; Reboussin, D.M.; Rahman, M.; Oparil, S.; et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med. 2015, 373, 2103–2116. [Google Scholar] [CrossRef]
- Jung, H.; Lee, J.E. The impact of community-based eHealth self-management intervention among elderly living alone with hypertension. J. Telemed. Telecare 2017, 23, 167–173. [Google Scholar] [CrossRef]
- Zhang, X.; Liao, H.; Shi, D.; Li, X.; Chen, X.; He, S. Cost-effectiveness analysis of different hypertension management strategies in a community setting. Intern. Emerg. Med. 2019. [Google Scholar] [CrossRef]
- Huang, J.; Zhang, T.; Wang, L.; Guo, D.; Liu, S.; Lu, W.; Liang, H.; Zhang, Y.; Liu, C. The effect of family doctor-contracted services on noncommunicable disease self-management in Shanghai, China. Int. J. Health Plann. Manag. 2019, 34, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Esteva, A.; Robicquet, A.; Ramsundar, B.; Kuleshov, V.; DePristo, M.; Chou, K.; Cui, C.; Corrado, G.; Thrun, S.; Dean, J. A guide to deep learning in healthcare. Nat. Med. 2019, 25, 24–29. [Google Scholar] [CrossRef] [PubMed]

| Variables | Intervention (n = 186) | Control (n = 276) | p |
|---|---|---|---|
| Male | 75 (40.3%) | 94 (34.1%) | 0.170 |
| Age (years) | 61.7 (6.3) | 61.3 (6.4) | 0.531 |
| Education | <0.001 | ||
| Secondary school or below | 47 (25.3%) | 95 (34.4%) | |
| High school | 80 (43.0%) | 136 (49.3%) | |
| College or above | 59 (31.7%) | 45 (16.3%) | |
| Married | 163 (87.6%) | 235 (85.1%) | 0.447 |
| Employed | 31 (16.7%) | 38 (13.8%) | 0.391 |
| Low income (<¥3000/month) | 42 (22.6%) | 107 (38.8%) | <0.001 |
| Disease course (years) | 9.2 (7.2) | 9.0 (7.9) | 0.825 |
| Clinical complications | |||
| Heart disease | 28 (15.1%) | 37 (13.4%) | 0.617 |
| Cerebrovascular disease | 6 (3.2%) | 7 (2.5%) | 0.660 |
| Kidney disease | 8 (4.3%) | 7 (2.5%) | 0.294 |
| Diabetes | 34 (18.3%) | 59 (21.4%) | 0.416 |
| Family history of hypertension | 150 (80.6%) | 206 (74.6%) | 0.132 |
| Monitoring BP | 107 (57.5%) | 159 (57.6%) | 0.986 |
| SBP (mmHg) | 135.8 (15.9) | 135.2 (14.8) | 0.679 |
| DBP (mmHg) | 83.0 (10.1) | 81.1 (10.8) | 0.056 |
| Hypertension control | 113 (60.8%) | 187 (67.8%) | 0.148 |
| Disease knowledge | 22.9 (6.6) | 19.7 (6.6) | <0.001 |
| Self-efficacy | 66.1 (5.6) | 66.5 (6.4) | 0.551 |
| Self-management | 138.1 (14.9) | 142.3 (14.9) | 0.003 |
| Social support | 39.4 (6.1) | 37.0 (6.7) | <0.001 |
| Mean Difference from Baseline | Difference between Groups | p | |
|---|---|---|---|
| SBP (mmHg); unadjusted | |||
| Intervention | −5.5 (−8.3, −2.7) | −7.1(−11.4, −2.8) | 0.001 |
| Control | 1.6 (−1.2, 4.4) | ||
| SBP (mmHg); adjusted * | |||
| Intervention | −5.3 (−8.2, −2.4) | −6.9 (−11.2, −2.6) | 0.002 |
| Control | 1.6 (−1.2, 4.5) | ||
| DBP (mmHg); unadjusted | |||
| Intervention | −1.3 (−3.0, 0.4) | −3.4 (−5.9, −0.8) | 0.011 |
| Control | 2.1 (0.4, 3.8) | ||
| DBP (mmHg); adjusted * | |||
| Intervention | −1.1 (−2.7, 0.6) | −3.1 (−5.7, −0.6) | 0.016 |
| Control | 2.0 (0.6, 3.7) | ||
| Baseline | Follow-up | Adjusted Odds Ratio * | p | |
| Hypertension control (SBP < 140, DBP < 90 mmHg) | ||||
| Intervention | 67 (60.9%) | 92 (83.6%) | 5.0 (2.3, 11.3) | <0.001 |
| Control | 99 (69.2%) | 91 (63.6%) | ||
| Monitoring BP (≥1/week) | ||||
| Intervention | 63 (57.3%) | 86 (78.1%) | 4.2 (1.8, 10.1) | 0.001 |
| Control | 84 (58.7%) | 81 (56.6%) | ||
| Outcomes (Aggregate Score) | Intervention | Control | Adjusted Mean Difference * | p |
|---|---|---|---|---|
| Hypertension knowledge (35) | 2.3 (0.8, 3.8) | 0.8 (−0.4, 2.0) | 1.5 (−0.3, 3.3) | 0.110 |
| Diagnostic criteria (1) | 0.2 (0.1, 0.3) | 0.1 (0.0, 0.2) | 0.1 (−0.1, 0.2) | 0.218 |
| Salt intake (1) | 0.1 (0.0,0.2) | 0.1 (0.0, 0.2) | 0.0 (−0.1, 0.1) | 0.585 |
| Symptoms (9) | 0.6 (0.3, 1.0) | 0.7 (0.4, 1.1) | −0.1 (−0.7, 0.5) | 0.747 |
| Complications (7) | 0.6 (0.0, 1.1) | −0.2 (−0.8, 0.3) | 0.8 (0.0, 1.7) | 0.055 |
| Risk factors (8) | 0.6 (0.0, 1.2) | −0.3 (−0.8, 0.3) | 0.9 (0.1, 1.7) | 0.027 |
| Methods of self-management (8) | 0.5 (0.0, 1.0) | −0.3 (−0.7, 0.1) | 0.8 (0.2, 1.5) | 0.009 |
| Self-efficacy (75) | 0.8 (−0.4, 2.0) | −0.6 (−1.7, 0.4) | 1.4 (−0.2, 3.0) | 0.086 |
| Daily life (20) | 0.6 (0.1, 1.1) | −0.2 (−0.6, 0.3) | 0.8 (0.1, 1.5) | 0.025 |
| Health behavior (30) | 0.0 (−0.4, 0.5) | −0.5 (−0.9, 0.0) | 0.5 (−0.2, 1.3) | 0.153 |
| Medication adherence (15) | 0.0 (−0.4, 0.4) | 0.2 (−0.2, 0.6) | −0.2 (−0.8, 0.4) | 0.615 |
| Self-management (10) | 0.2 (−0.2, 0.5) | −0.1 (−0.5, 0.2) | 0.3 (−0.2, 0.8) | 0.242 |
| Self-management (165) | 7.3 (4.3, 10.3) | −1.4 (−4.0, 1.2) | 8.7 (4.7, 12.7) | <0.001 |
| Medication adherence (20) | 0.2 (−0.3, 0.7) | −0.2 (−0.7, 0.3) | 0.4 (−0.4, 1.2) | 0.355 |
| Condition monitoring (20) | 1.6 (1.0, 2.2) | 0.0 (−0.6, 0.6) | 1.6 (0.7, 2.5) | <0.001 |
| Diet management (50) | 1.7 (0.6, 2.8) | −2.5 (−3.5, −1.6) | 4.2 (2.7, 5.6) | <0.001 |
| Exercise management (15) | 1.3 (0.5, 2.0) | 0.8 (0.0, 1.5) | 0.5 (−0.7, 1.7) | 0.389 |
| Work–rest management (25) | 1.9 (0.7, 3.0) | 0.4 (−0.8, 1.5) | 1.5 (−0.2, 3.2) | 0.091 |
| Social support (64) | 0.4 (−0.1, 0.9) | 0.7 (0.3, 1.2) | −0.3 (−1.1, 0.3) | 0.309 |
| Subjective support (20) | 0.0 (−0.5, 0.5) | 0.2(−0.3, 0.7) | −0.2 (−0.8, 0.4) | 0.521 |
| Objective support (32) | −0.1 (−0.6, 0.4) | 0.1 (−0.4, −0.6) | −0.2 (−1.0, 0.7) | 0.647 |
| Use of social support (12) | 0.5 (0.0, 1.0) | 0.6 (0.1, 1.1) | −0.1 (−0.9, 0.7) | 0.785 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, X.; Li, T.; Chen, J.; Xie, Y.; An, X.; Lv, Y.; Lin, A. A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 4058. https://doi.org/10.3390/ijerph16214058
Li X, Li T, Chen J, Xie Y, An X, Lv Y, Lin A. A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2019; 16(21):4058. https://doi.org/10.3390/ijerph16214058
Chicago/Turabian StyleLi, Xiaowen, Tong Li, Jianying Chen, Yuanling Xie, Xia An, Yunhong Lv, and Aihua Lin. 2019. "A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial" International Journal of Environmental Research and Public Health 16, no. 21: 4058. https://doi.org/10.3390/ijerph16214058
APA StyleLi, X., Li, T., Chen, J., Xie, Y., An, X., Lv, Y., & Lin, A. (2019). A WeChat-Based Self-Management Intervention for Community Middle-Aged and Elderly Adults with Hypertension in Guangzhou, China: A Cluster-Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 16(21), 4058. https://doi.org/10.3390/ijerph16214058





