Towards a People’s Social Epidemiology: Envisioning a More Inclusive and Equitable Future for Social Epi Research and Practice in the 21st Century
Abstract
1. Introduction: Social Epidemiology and Its (Dis)Contents
“Do epidemiologists and other public health professionals have a responsibility to ask whether the ways we think and work reflect or contribute to social inequality? Proponents of socially responsible science would answer yes. What say you?”[1] (p.1152)
2. The Makings of a People’s Social Epi
2.1. The People + Social Epidemiology: Reconnecting with “Demos”
2.2. Participation + Social Epidemiology: Integrating CBPR
“More than other subfields, social epidemiology is uniquely placed to benefit from partnerships to help generate new questions and to ensure findings are used to inform population health interventions”.[12] (p.855)
2.3. Socializing Social Epidemiology: Incorporating ICTs
“a practice owned and directed by those who are contributing the data… The essence of Small Data is that such communities may not just participate in, but can actually initiate and drive such data investigations towards the better understanding of an important local issue”.(p.116)
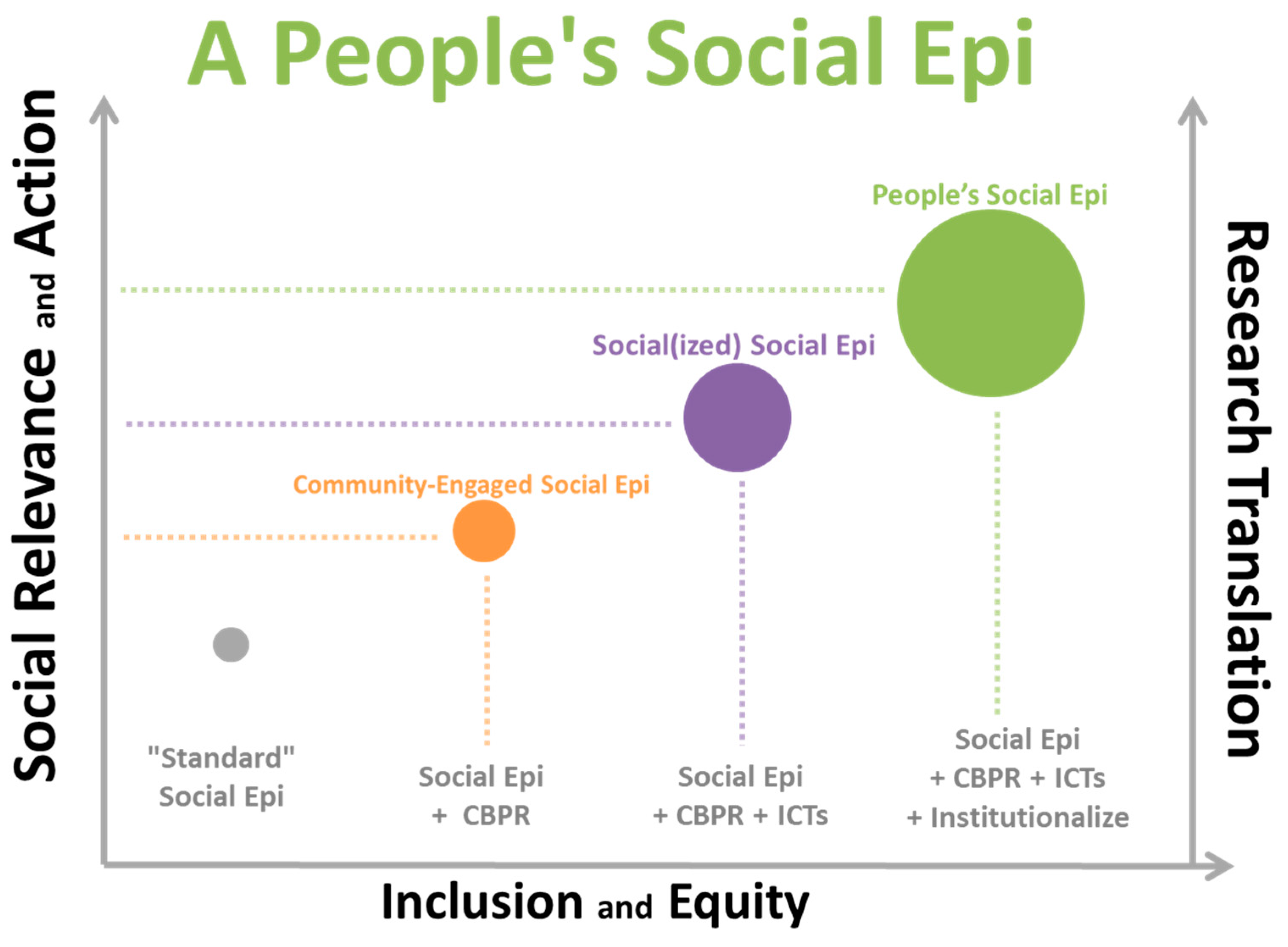
3. A People’s Social Epidemiology: An Introductory Framework
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Declaration
References
- Krieger, N. Questioning epidemiology: Objectivity, advocacy, and socially responsible science. Am. J. Public Health 1999, 89, 1151–1153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Krieger, N. Epidemiology emerges: Early theories and debating determinants of disease distribution—Poison, filth, class, & race 1600–1900. In Epidemiology and the People’s Health: Theory and Context; Oxford University Press: New York, NY, USA, 2011; pp. 58–94. [Google Scholar]
- Cassel, J. The contribution of the social environment to host resistance. Am. J. Epidemiol. 1976, 104, 107–123. [Google Scholar] [CrossRef] [PubMed]
- Syme, S.L.; Berkman, L. Social class, susceptibility, and sickness. Am. J. Epidemiol. 1976, 104, 1–8. [Google Scholar] [CrossRef]
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 2001, 30, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.G.; Shipley, M.J.; Rose, G. Inequalities in death—Specific explanations of a general pattern? Lancet 1984, 323, 1003–1006. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 35, 80. [Google Scholar] [CrossRef]
- Geronimus, A.T. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethn. Dis. 1992, 2, 207–221. [Google Scholar]
- Galea, S.; Link, B.G. Six paths for the future of social epidemiology. Am. J. Epidemiol. 2013, 178, 843–849. [Google Scholar] [CrossRef]
- Kaplan, G.A. What’s wrong with social epidemiology, and how can we make it better? Epidemiol. Rev. 2004, 26, 124–135. [Google Scholar] [CrossRef]
- Glymour, M.M.; Osypuk, T.L.; Rehkopf, D.H. Invited commentary: Off-roading with social epidemiology—Exploration, causation, translation. Am. J. Epidemiol. 2013, 178, 858–863. [Google Scholar] [CrossRef]
- Muntaner, C. Invited commentary: On the future of social epidemiology—A case for scientific realism. Am. J. Epidemiol. 2013, 178, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Oakes, J.M. Invited commentary: Paths and pathologies of social epidemiology. Am. J. Epidemiol. 2013, 178, 850–851. [Google Scholar] [CrossRef] [PubMed]
- O’Campo, P.; Dunn, J.R. Introduction. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 1–19. [Google Scholar] [CrossRef]
- Shankardass, K. Place-based stress and chronic disease: A systems view of environmental determinants. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 113–136. [Google Scholar] [CrossRef]
- Shankardass, K.; Dunn, J.R. How goes the neighbourhood? Rethinking neighbourhoods and health research in social epidemiology. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 137–156. [Google Scholar] [CrossRef]
- Yen, I.H.; Shim, J.K.; Martínez, A.D. Application of two schools of social theory to neighbourhood, place and health research. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 157–174. [Google Scholar] [CrossRef]
- Bayoumi, A.M.; Guta, A. Values and social epidemiologic research. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 43–65. [Google Scholar] [CrossRef]
- Muntaner, C.; Borrell, C.; Ng, E.; Chung, H.; Espelt, A.; Rodriguez-Sanz, M.; Benach, J.; O’Campo, P. Locating politics in social epidemiology. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 175–202. [Google Scholar] [CrossRef]
- Murphy, K.; Fafard, P. Knowledge translation and social epidemiology: Taking power, politics and values seriously. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 267–283. [Google Scholar] [CrossRef]
- Mowat, D.; Chambers, C. Producing more relevant evidence: App.lying a social epidemiology research agenda to public health practice. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 305–325. [Google Scholar] [CrossRef]
- Smylie, J.; Lofters, A.; Firestone, M.; O’Campo, P. Population-based data and community empowerment. In Rethinking Social Epidemiology; O’Campo, P., Dunn, J.R., Eds.; Springer: Dordrecht, The Netherlands, 2012; pp. 67–92. [Google Scholar] [CrossRef]
- Lantz, P.; Israel, B.A.; Schulz, A.J.; Reyes, A.G. Community-based participatory research: Rationale and relevance for social epidemiology. In Methods in Social Epidemiology; Oakes, J.M., Kaufman, J., Eds.; Jossey-Bass: San Francisco, CA, USA, 2006; pp. 229–266. [Google Scholar]
- Leung, M.W. Community based participatory research: A promising approach for increasing epidemiology’s relevance in the 21st century. Int. J. Epidemiol. 2004, 3, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Schwab, M.; Syme, S.L. On paradigms, community participation, and the future of public health. Am. J. Public Health 1997, 87, 2049–2052. [Google Scholar] [CrossRef]
- Syme, S.L. Social determinants of health: The community as an empowered partner. Prev. Chron. Dis. 2004, 1, 5. [Google Scholar]
- Wallerstein, N.B.; Yen, I.H.; Syme, S.L. Integration of social epidemiology and community-engaged interventions to improve health equity. Am. J. Public Health 2011, 101, 822–830. [Google Scholar] [CrossRef]
- Kawachi, I.; Subramanian, S.V. Social epidemiology for the 21st century. Soc. Sci. Med. 2018, 196, 240–245. [Google Scholar] [CrossRef]
- Krieger, N. Epidemiology and the web of causation: Has anyone seen the spider? Soc. Sci. Med. 1994, 39, 887–903. [Google Scholar] [CrossRef]
- Krieger, N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef]
- McMichael, A.J. Prisoners of the proximate: Loosening the constraints on epidemiology in an age of change. Am. J. Epidemiol. 1999, 14, 11. [Google Scholar] [CrossRef]
- Muntaner, C. Invited commentary: Social mechanisms, race, and social epidemiology. Am. J. Epidemiol. 1999, 150, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Israel, B.A.; Schurman, S.J.; Hugentobler, M.K. Conducting action research: Relationships between organization members and researchers. J. Appl. Behav. Sci. 1992, 28, 74–101. [Google Scholar] [CrossRef]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing partnership approaches to improve public health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [PubMed]
- Minkler, M. Using participatory action research to build healthy communities. Public Health Rep. 2000, 115, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Wallerstein, N.; Duran, B. The theoretical, historical, and practice roots of CBPR. In Community-Based Participatory Research for Health: Advancing Social and Health Equity; Wallerstein, N., Duran, B., Oetzel, J., Minkler, M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2017. [Google Scholar]
- Cashman, S.B.; Adeky, S.; Allen, A.J.; Corburn, J.; Israel, B.A.; Montaño, J.; Rafelito, A.; Rhodes, S.D.; Swanston, S.; Wallerstein, N.; et al. The power and the promise: Working with communities to analyze data, interpret findings, and get to outcomes. Am. J. Public Health 2008, 98, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.; Green, L. Federal funding and support for participatory research in public health and health care. In Community Based Participatory Research for Health: Process to Outcomes; Minkler, M., Wallerstein, N., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 399–406. [Google Scholar]
- Wallerstein, N.; Duran, B. Community-based participatory research contributions to intervention research: The intersection of science and practice to improve health equity. Am. J. Public Health 2010, 100, S40–S46. [Google Scholar] [CrossRef] [PubMed]
- Israel, B.A.; Coombe, C.M.; Cheezum, R.R.; Schulz, A.J.; McGranaghan, R.J.; Lichtenstein, R.; Reyes, A.G.; Clement, J.; Burris, A. Community-based participatory research: A capacity-building approach for policy advocacy aimed at eliminating health disparities. Am. J. Public Health 2010, 100, 2094–2102. [Google Scholar] [CrossRef]
- Minkler, M. Linking science and policy through community-based participatory Research to study and address health disparities. Am. J. Public Health 2010, 100, S81–S87. [Google Scholar] [CrossRef]
- Atwood, K.; Colditz, G.A.; Kawachi, I. From public health science to prevention policy: Placing science in its social and political contexts. Am. J. Public Health 1997, 87, 1603–1606. [Google Scholar] [CrossRef]
- Liverani, M.; Hawkins, B.; Parkhurst, J.O. Political and institutional influences on the use of evidence in public health policy. A systematic review. PLoS ONE 2013, 8, e77404. [Google Scholar] [CrossRef]
- Morgan-Trimmer, S. Policy is political; our ideas about knowledge translation must be too. J. Epidemiol. Commun. Health 2014, 68, 1010–1011. [Google Scholar] [CrossRef]
- Muntaner, C.; Chung, H.; Murphy, K.; Ng, E. Barriers to knowledge production, knowledge translation, and urban health policy change: Ideological, economic, and political considerations. J. Urban Health 2012, 89, 915–924. [Google Scholar] [CrossRef] [PubMed]
- Oliver, T.R. The politics of public health policy. Annu. Rev. Public Health 2006, 27, 195–233. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.E. The politics of ideas: The complex interplay of health inequalities research and policy. Sci. Public Policy 2014, 41, 561–574. [Google Scholar] [CrossRef]
- Balazs, C.L.; Morello-Frosch, R. The three rs: How community-based participatory research strengthens the rigor, relevance, and reach of science. Environ. Justice 2013, 6, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Cargo, M.; Mercer, S.L. The value and challenges of participatory research: Strengthening its practice. Annu. Rev. Public Health 2008, 29, 325–350. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, C.R.; Robinson, M.; Seifer, S. Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation 2009, 119, 2633–2642. [Google Scholar] [CrossRef]
- Cook, W.K. Integrating research and action: A Systematic review of community-based participatory research to address health disparities in environmental and occupational health in the USA. J. Epidemiol. Commun. Health 2008, 62, 668–676. [Google Scholar] [CrossRef]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health: Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef]
- Ellen, I.G.; Mijanovich, T.; Dillman, K.-N. Neighborhood effects on health: Exploring the links and assessing the evidence. J. Urban Aff. 2001, 23, 391–408. [Google Scholar] [CrossRef]
- Pickett, K.E.; Pearl, M. Multilevel analyses of neighbourhood socioeconomic context and health Outcomes: A critical review. J. Epidemiol. Commun. Health 2001, 55, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Arcaya, M.C.; Tucker-Seeley, R.D.; Kim, R.; Schnake-Mahl, A.; So, M.; Subramanian, S.V. Research on neighborhood effects on health in the United States: A systematic review of study characteristics. Soc. Sci. Med. 2016, 168, 16–29. [Google Scholar] [CrossRef] [PubMed]
- Chaix, B.; Merlo, J.; Evans, D.; Leal, C.; Havard, S. Neighbourhoods in eco-epidemiologic research: Delimiting personal exposure areas. A response to Riva, Gauvin, Apparicio and Brodeur. Soc. Sci. Med. 2009, 69, 1306–1310. [Google Scholar] [CrossRef] [PubMed]
- Leal, C.; Chaix, B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a methodological assessment and a research agenda: Geographic life environments and cardiometabolic risk factors. Obes. Rev. 2011, 12, 217–230. [Google Scholar] [CrossRef]
- Wilson, E.; Kenny, A.; Dickson-Swift, V. Ethical challenges in community-based participatory research: A scoping review. Qual. Health Res. 2018, 28, 189–199. [Google Scholar] [CrossRef]
- Stoecker, R. Are we talking the walk of community-based research? Action Res. 2009, 7, 385–404. [Google Scholar] [CrossRef]
- Minkler, M. Community-based research partnerships: Challenges and opportunities. J. Urban Health Bull. N. Y. Acad. Med. 2005, 82 (Suppl. S2), ii3–ii12. [Google Scholar] [CrossRef]
- Minkler, M. Ethical challenges for the “Outside” researcher in community-based participatory research. Health Educ. Behav. 2004, 31, 684–697. [Google Scholar] [CrossRef]
- Chávez, V.; Duran, B.; Baker, Q.E.; Avila, M.M.; Wallerstein, N. The dance of race and privilege in cbpr. In Community-Based Participatory Research for Health: From Process to Outcomes; Minkler, M., Wallerstein, N., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 91–106. [Google Scholar]
- Muhammad, M.; Garzón, C.; Reyes, A.; West Oakland Environmental Indicators Project. Understanding Contemporary Racism, Power, and Privilege and Their Impacts on CBPR. In Community-Based Participatory Research for Health: Advancing Social and Health Equity; Wallerstein, N., Duran, B., Oetzel, J., Minkler, M., Eds.; Jossey-Bass: San Francisco, CA, USA, 2017; pp. 47–59. [Google Scholar]
- Stanton, C.R. Crossing methodological borders: Decolonizing community-based participatory research. Qual. Inq. 2014, 20, 573–583. [Google Scholar] [CrossRef]
- Janes, J.E. Democratic encounters? Epistemic privilege, power, and community-based participatory action research. Action Res. 2016, 14, 72–87. [Google Scholar] [CrossRef]
- Schulz, A.J.; Kannan, S.; Dvonch, J.T.; Israel, B.A.; Allen, A.; James, S.A.; House, J.S.; Lepkowski, J. Social and physical environments and disparities in risk for cardiovascular disease: The healthy environments partnership conceptual model. Environ. Health Perspect. 2005, 113, 1817–1825. [Google Scholar] [CrossRef]
- Schultz, A.; Zenk, S.; Kannan, S.; Koch, M.; Israel, B.; Stokes, C. Community-based participatory approach to survey design and implementation: The healthy environments community survey. In Methods for Conducting Community-Based Participatory Research for Health; Israel, B., Parker, E.A., Eng, E., Schulz, A., Eds.; Jossey-Bass: San Francisco, CA, USA, 2005; pp. 107–127. [Google Scholar]
- Palaniappan, M. Ditching diesel: Community-driven research reduces pollution in West Oakland. Race Poverty Env. 2004, 11, 31–34. [Google Scholar]
- Gonzalez, P.A.; Minkler, M.; Garcia, A.P.; Gordon, M.; Garzón, C.; Palaniappan, M.; Prakash, S.; Beveridge, B. Community-based participatory research and policy advocacy to reduce diesel exposure in West Oakland, California. Am. J. Public Health 2011, 101 (Suppl. S1), S166–S175. [Google Scholar] [CrossRef]
- Garzón, C.; Beveridge, B.; Gordon, M.; Martin, C.; Matalon, E.; Moore, E. Power, privilege, and the process of community-based participatory research: Critical reflections on forging an empowered partnership for environmental justice in West Oakland, California. Environ. Justice 2013, 6, 71–78. [Google Scholar] [CrossRef]
- Imara, N.; Lazerow, S.; Lee, A.Y.; Malloy, N.; Orozco, A.; Pérez, C. East Oakland Particulate Matter 2.5 Community-Based Air Monitoring Research Report; Communities for a Better Environment (CBE): Oakland, CA, USA, 2010. [Google Scholar]
- Brown, P.; Brody, J.G.; Morello-Frosch, R.; Tovar, J.; Zota, A.R.; Rudel, R.A. Measuring the success of community science: The Northern California household exposure study. Environ. Health Perspect. 2012, 120, 326–331. [Google Scholar] [CrossRef]
- Cohen, A.; Lopez, A.; Malloy, N.; Morello-Frosch, R. Our environment, our health: A community-based participatory environmental health survey in Richmond, California. Health Educ. Behav. 2012, 39, 198–209. [Google Scholar] [CrossRef]
- Commodore, A.; Wilson, S.; Muhammad, O.; Svendsen, E.; Pearce, J. Community-based participatory research for the study of air pollution: A review of motivations, approaches, and outcomes. Environ. Monit. Assess. 2017, 189. [Google Scholar] [CrossRef]
- Heeks, R. Theorizing ICT4D research. Inf. Technol. Int. Dev. 2007, 3, 1–4. [Google Scholar] [CrossRef]
- Karanasios, S. Framing ICT4D research using activity theory: A match between the ICT4D field and theory? Inf. Technol. 2014, 10, 18. [Google Scholar]
- Parmar, V. A multidisciplinary approach to ICT development. Inf. Technol. Int. Dev. 2009, 5, 8. [Google Scholar]
- Avgerou, C. Discourses on ICT and Development. Inf. Technol. Int. Dev. 2010, 6, 1–18. [Google Scholar]
- Burrell, J.; Toyama, K. What constitutes good ICTD research? Inf. Technol. Int. Dev. 2009, 5, 13. [Google Scholar]
- Dearden, A. See No Evil? Ethics in an Interventionist ICTD. Inf. Technol. Int. Dev. 2012, 9, 1–17. [Google Scholar]
- D’Ignazio, C.; Warren, J.; Blair, D. The role of small data for governance in the 21st century. In Governança Digital; Universidade Federal Rio Grande do Sul: Porto Alegre, Brazil, 2014; pp. 115–129. [Google Scholar]
- Brown, P. Popular epidemiology revisited. Curr. Soc. 1997, 45, 137–156. [Google Scholar] [CrossRef]
- Brown, P. Popular epidemiology and toxic waste contamination: Lay and professional ways of knowing. J. Health Soc. Behav. 1992, 33, 267. [Google Scholar] [CrossRef]
- Conrad, C.C.; Hilchey, K.G. A review of citizen science and community-based environmental monitoring: issues and opportunities. Environ. Monit. Assess. 2011, 176, 273–291. [Google Scholar] [CrossRef]
- Den Broeder, L.; Devilee, J.; Van Oers, H.; Schuit, A.J.; Wagemakers, A. Citizen science for public health. Health Promot. Int. 2016. [Google Scholar] [CrossRef]
- Pfister, D.S.; Godana, G.D. Deliberation technology. J. Public Delib. 2012, 8, 1–7. [Google Scholar]
- Kamel Boulos, M.N.; Resch, B.; Crowley, D.N.; Breslin, J.G.; Sohn, G.; Burtner, R.; Pike, W.A.; Jezierski, E.; Chuang, K.-Y. Crowdsourcing, citizen sensing and sensor web technologies for public and environmental health surveillance and crisis management: Trends, OGC standards and application examples. Int. J. Health Geogr. 2011, 10, 67. [Google Scholar] [CrossRef]
- Lupton, D. Health promotion in the digital era: A Critical commentary. Health Promot. Int. 2015, 30, 174–183. [Google Scholar] [CrossRef]
- Lupton, D. Beyond techno-utopia: Critical approaches to digital health technologies. Societies 2014, 4, 706–711. [Google Scholar] [CrossRef]
- Lupton, D. M-Health and health promotion: The digital cyborg and surveillance society. Soc. Theor. Health 2012, 10, 229–244. [Google Scholar] [CrossRef]
- NACCHO. YouTube, Facebook, MySpace, Blogs, and More: Innovative Ways Local Health Departments Are Reaching Adolescents; Issue Brief; NACCHO: Washington, DC, USA, 2008. [Google Scholar]
- NACCHO. The Use of Public Health Informatics to Identify and Address Inequities; Issue Brief; NACCHO: Washington, DC, USA, 2009. [Google Scholar]
- Brabham, D.C.; Ribisl, K.M.; Kirchner, T.R.; Bernhardt, J.M. Crowdsourcing applications for public health. Am. J. Prev. Med. 2014, 46, 179–187. [Google Scholar] [CrossRef]
- Ozdalga, E.; Ozdalga, A.; Ahuja, N. The smartphone in medicine: A review of current and potential use among physicians and students. J. Med. Internet Res. 2012, 14. [Google Scholar] [CrossRef]
- Patrick, K.; Griswold, W.G.; Raab, F.; Intille, S.S. Health and the mobile phone. Am. J. Prev. Med. 2008, 35, 177–181. [Google Scholar] [CrossRef]
- DHHS. Healthy People 2020. 2012. Available online: http://www.hhs.gov/open/initiatives/mhealth/recommendations.html (accessed on 10 September 2012).
- Lemay, N.V.; Sullivan, T.; Jumbe, B.; Perry, C.P. Reaching remote health workers in Malawi: Baseline assessment of a pilot mhealth intervention. J. Health Commun. 2012, 17 (Suppl. S1), 105–117. [Google Scholar] [CrossRef]
- Lester, R.T.; Ritvo, P.; Mills, E.J.; Kariri, A.; Karanja, S.; Chung, M.H.; Jack, W.; Habyarimana, J.; Sadatsafavi, M.; Najafzadeh, M.; et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet 2010, 376, 1838–1845. [Google Scholar] [CrossRef]
- Redfern, J.; Thiagalingam, A.; Jan, S.; Whittaker, R.; Hackett, M.; Mooney, J.; Keizer, L.D.; Hillis, G.; Chow, C. Development of a set of mobile phone text messages designed for prevention of recurrent cardiovascular events. Eur. J. Prev. Cardiol. 2014, 21, 492–499. [Google Scholar] [CrossRef]
- Stenner, S.P.; Johnson, K.B.; Denny, J.C. PASTE: Patient-centered SMS text tagging in a medication management system. J. Am. Med. Inf. Assoc. 2012, 19, 368–374. [Google Scholar] [CrossRef]
- Bravo, S.; Valero, M.A.; Pau, I. A Tele-Health communication and information system for underserved children in rural areas of Nicaragua. Inf. Technol. 2012, 8, 18. [Google Scholar]
- Tamrat, T.; Kachnowski, S. Special delivery: An analysis of mhealth in maternal and newborn health programs and their outcomes around the world. Matern. Child Health J. 2012, 16, 1092–1101. [Google Scholar] [CrossRef] [PubMed]
- Brownstein, J.S.; Freifeld, C.C.; Madoff, L.C. Digital disease detection—Harnessing the web for public health surveillance. N. Engl. J. Med. 2009, 360, 2153–2157. [Google Scholar] [CrossRef] [PubMed]
- Freifeld, C.C.; Chunara, R.; Mekaru, S.R.; Chan, E.H.; Kass-Hout, T.; Ayala Iacucci, A.; Brownstein, J.S. Participatory epidemiology: Use of mobile phones for community-based health reporting. PLoS Med. 2010, 7, e1000376. [Google Scholar] [CrossRef] [PubMed]
- Ranard, B.L.; Ha, Y.P.; Meisel, Z.F.; Asch, D.A.; Hill, S.S.; Becker, L.B.; Seymour, A.K.; Merchant, R.M. Crowdsourcing—Harnessing the masses to advance health and medicine, a systematic review. J. Gen. Intern. Med. 2014, 29, 187–203. [Google Scholar] [CrossRef]
- Chaix, B.; Kestens, Y.; Perchoux, C.; Karusisi, N.; Merlo, J.; Labadi, K. An interactive mapping tool to assess individual mobility patterns in neighborhood studies. Am. J. Prev. Med. 2012, 43, 440–450. [Google Scholar] [CrossRef]
- Gorely, T.; Biddle, S.J.H.; Marshall, S.J.; Cameron, N. The prevalence of leisure time sedentary behaviour and physical activity in adolescent boys: An ecological momentary assessment approach. Int. J. Pediatr. Obes. 2009, 4, 289–298. [Google Scholar] [CrossRef]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef]
- Zenk, S.N.; Schulz, A.J.; Matthews, S.A.; Odoms-Young, A.; Wilbur, J.; Wegrzyn, L.; Gibbs, K.; Braunschweig, C.; Stokes, C. Activity space environment and dietary and physical activity behaviors: A pilot study. Health Place 2011, 17, 1150–1161. [Google Scholar] [CrossRef]
- WHO. MHealth: New Horizons for Health through Mobile Technologies; Global Observatory for eHealth; World Health Organization: Geneva, Switzerland, 2011; Volume 3. [Google Scholar]
- APHA. The New Public Health: Rewiring for the Future; Mid Year Meeting; APHA: Washington, DC, USA, 2012. [Google Scholar]
- NACCHO. Local Health Departments and MHealth; Issue Brief; NACCHO: Washington, DC, USA, 2012. [Google Scholar]
- NIH. Office of Behavior and Social Science Research. 2014. Available online: http://obssr.od.nih.gov/scientific_areas/methodology/mhealth/index.aspx (accessed on 10 September 2014).
- CDC. CDC Mobile. 2014. Available online: http://www.cdc.gov/mobile/index.html (accessed on 10 September 2014).
- HRSA. HRSA MHealth. 2013. Available online: http://www.hrsa.gov/healthit/healthitgranteespotlight/mhealth2013/ (accessed on 10 September 2014).
- NIH. Wireless Health 2014. 2014. Available online: http://www.wirelesshealth2014.org/ (accessed on 10 September 2014).
- Lupton, D. Digitized Health Promotion: Personal Responsibility for Health in the Web 2.0 Era; The Sydney Health & Society Group: Sydney, Australia, 2013. [Google Scholar]
- Petteway, R.J.; Mujahid, M.; Allen, A.; Morello-Frosch, R. The body language of place: A new method for mapping intergenerational “Geographies of Embodiment” in place-Health research. Soc. Sci. Med. 2019, 223, 51–63. [Google Scholar] [CrossRef]
- Petteway, R.J. Intergenerational photovoice perspectives of place and health in public housing: participatory coding, theming, and mapping in/of the “Structure Struggle”. Health Place 2019. in Press. [Google Scholar]
- Van Wart, S.; Tsai, K.; Parikh, T. Local ground: A paper-based toolkit for documenting local geospatial knowledge. In Proceedings of the ACM Symposium on Computing for Development (DEV), London, UK, 2010. [Google Scholar]
- Campos-Castillo, C. Revisiting the first-level digital divide in the United States: Gender and race/ethnicity patterns, 2007–2012. Soc. Sci. Comput. Rev. 2015, 33, 423–439. [Google Scholar] [CrossRef]
- Chen, W.; Wellman, B. The global digital divide—Within and between countries. IT Soc. 2004, 1, 39–45. [Google Scholar]
- Tsatsou, P. Digital Divides Revisited: What is new about divides and their research? Media Cult. Soc. 2011, 33, 317–331. [Google Scholar] [CrossRef]
- Borg, K.; Boulet, M.; Smith, L.; Bragge, P. Digital inclusion & health communication: A rapid review of literature. Health Commun. 2019, 34, 1320–1328. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.; Schaffer, G.; Wolfson, T. Digital human capital: Developing a framework for understanding the economic impact of digital exclusion in low-income communities. J. Inf. Policy 2013, 3, 247. [Google Scholar] [CrossRef]
- Bambra, C.; Smith, K.E.; Pearce, J. Scaling up: The politics of health and place. Soc. Sci. Med. 2019, 232, 36–42. [Google Scholar] [CrossRef]
| ICT Name | Features | |
|---|---|---|
| 1 | Magpi | Survey instrument design, data collection & analysis; real-time assessment; SMS, photo, and audio capabilities; geolocation and mapping capability; smartphone deployment; built-in data analysis & visualization tools; collaborative use options; online/offline use |
| 2 | Fulcrum | Survey instrument design, data collection & analysis; real-time assessment; photo capability; geolocation and mapping capability; smartphone deployment; built-in data analysis & visualization tools; collaborative use options; online/offline use |
| 3 | Kobo ToolBox | Survey instrument design, data collection & analysis; real-time assessment; geolocation and mapping capability; smartphone deployment; built-in data analysis & visualization tools; online/offline use; open source |
| 4 | EthnoCorder | Survey instrument design, data collection & analysis; real-time assessment; Text, photo, video, and audio capabilities; geolocation and mapping capability; smartphone deployment; built-in data analysis & visualization tools; collaborative use options |
| 5 | MyInsights (MyPanel) | Qualitative and mixed-methods research platform for survey design, data collection and analysis; real-time assessment; Text, photo, video, and audio capabilities; geolocation capability; smartphone deployment; built-in data analysis & visualization tools; collaborative use options |
| 6 | QuickTapSurvey | Survey instrument design, data collection & analysis; real-time assessment; text and photo capabilities; geolocation capability; smartphone deployment; built-in data visualization tools; collaborative use options; online/offline use |
| 7 | FieldNotes | GPS location-based note taking and data collection & platform; real-time assessment; Text, photo, video, and audio capabilities; geolocation capability; smartphone deployment |
| 8 | LiveTrekker | GPS location-based tool for documenting geographic travel and spatial movement patterns; real-time assessment; Text, photo, video, and audio capabilities; geolocation and mapping capability; smartphone deployment; built-in data visualization tools; social media sharing tools |
| 9 | Capture365 Journal | Multimedia-enabled journaling platform; Text, photo, video, and audio capabilities; geolocation and weather tracking capability; smartphone deployment; built-in data visualization and social media sharing tools |
| 10 | MapYourWorld | Suite of mapping-focused tools geared towards youth participatory research; geolocation and mapping capabilities; built-in data visualization tools; built-in social media sharing tools |
| Activity Description | Core Local Collaborators | Objectives | |
|---|---|---|---|
| 1 | Use local social epi research study data in local health department (LHD) and city planning practice
| University Researchers; Health and Planning Agencies; Other social determinants of health (SDH)-related Agencies; Community Organizations | Facilitate research translation and action based on local research; Facilitate collaboration between researchers and local agencies; Promote social value and relevance of social epidemiology |
| 2 | Create Social Epidemiology/Health Equity programs within LHDs where social epi research projects are being conducted
| University Researchers; LHDs | Increase LHD capacity to do social epidemiology; Facilitate collaboration between researchers and LHDs; Create opportunities for collaborative grant writing for social epidemiology research and translation activities |
| 3 | Develop local social epi Research & Practice Training Institutes
| University Researchers; LHDs; Community Organizations | Increase LHD capacity to do social epidemiology; Facilitate collaboration between researchers and LHDs; Promote social value and relevance of social epidemiology; Promote broader community understanding and knowledge of social epidemiology |
| 4 | Develop social epi “exchange program” for faculty/researchers of local universities conducting social epi research to give guest lectures at local high schools | University Researchers; High Schools | Promote social value and relevance of social epidemiology; Encourage pursuit of future public health education opportunities; Promote meaningful opportunities for researchers to connect/contribute to local communities beyond research |
| 5 | Support opportunities for local high school students to openly and freely attend courses taught by social epi researchers who are conducting research in the local community | University Researchers; Universities; High Schools | Promote social value and relevance of social epidemiology; Encourage pursuit of future public health education opportunities; Promote meaningful opportunities for researchers to connect/contribute to local communities beyond research |
| 6 | Co-Develop social epi and health equity-oriented school curricula for local high schools
| University Researchers; High Schools; LHDs | Promote social value and relevance of social epidemiology; Encourage pursuit of future public health education opportunities; Provide unique education, training, and professional development opportunities for students; Promote student connectivity to local health equity issues and facilitate their development as local change agents and future scientists |
| 7 | Develop social epi/public health college pipeline programs and/or summer institutes for local high school students
| Universities; High Schools | Promote social value and relevance of social epidemiology; Encourage pursuit of future public health education opportunities; Promote meaningful opportunities for researchers to connect/contribute to local communities beyond research |
| 8 | Create local media linkages for regular reporting/distribution of info/results/knowledge based on local social epi research projects
| University Researchers; Media Outlets | Promote social value and relevance of social epidemiology; Facilitate research translation and action based on local research; Promote meaningful opportunities for researchers to connect/contribute to local communities beyond research; Promote broader community understanding and knowledge of social epidemiology |
| 9 | Develop collaborations with local artists to creatively frame, represent/re-present, and disseminate social epi research findings
| University Researchers; Arts Colleges; Artists and Art Groups | Promote social value and relevance of social epidemiology; Facilitate research translation and action based on local research; Promote meaningful opportunities for researchers to connect/contribute to local communities beyond research; Promote broader community understanding and knowledge of social epidemiology |
| 10 | Support formation of standing Social Determinants Assessment and Action bodies within local government
| University Researchers; Health, Planning, Housing, Transportation, Education, and Recreation Agencies; Community Organizations; High Schools | Facilitate research translation and action based on local research; Facilitate collaboration between researchers and local agencies; Promote social value and relevance of social epidemiology |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petteway, R.; Mujahid, M.; Allen, A.; Morello-Frosch, R. Towards a People’s Social Epidemiology: Envisioning a More Inclusive and Equitable Future for Social Epi Research and Practice in the 21st Century. Int. J. Environ. Res. Public Health 2019, 16, 3983. https://doi.org/10.3390/ijerph16203983
Petteway R, Mujahid M, Allen A, Morello-Frosch R. Towards a People’s Social Epidemiology: Envisioning a More Inclusive and Equitable Future for Social Epi Research and Practice in the 21st Century. International Journal of Environmental Research and Public Health. 2019; 16(20):3983. https://doi.org/10.3390/ijerph16203983
Chicago/Turabian StylePetteway, Ryan, Mahasin Mujahid, Amani Allen, and Rachel Morello-Frosch. 2019. "Towards a People’s Social Epidemiology: Envisioning a More Inclusive and Equitable Future for Social Epi Research and Practice in the 21st Century" International Journal of Environmental Research and Public Health 16, no. 20: 3983. https://doi.org/10.3390/ijerph16203983
APA StylePetteway, R., Mujahid, M., Allen, A., & Morello-Frosch, R. (2019). Towards a People’s Social Epidemiology: Envisioning a More Inclusive and Equitable Future for Social Epi Research and Practice in the 21st Century. International Journal of Environmental Research and Public Health, 16(20), 3983. https://doi.org/10.3390/ijerph16203983





