Impact of an 8-Week Exercise and Sport Intervention on Post-Traumatic Stress Disorder Symptoms, Mental Health, and Physical Fitness among Male Refugees Living in a Greek Refugee Camp
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Procedures
2.3. Exercise and Sport Program
2.4. Measures
2.5. Statistical Analyses
2.6. Data Availability
3. Results
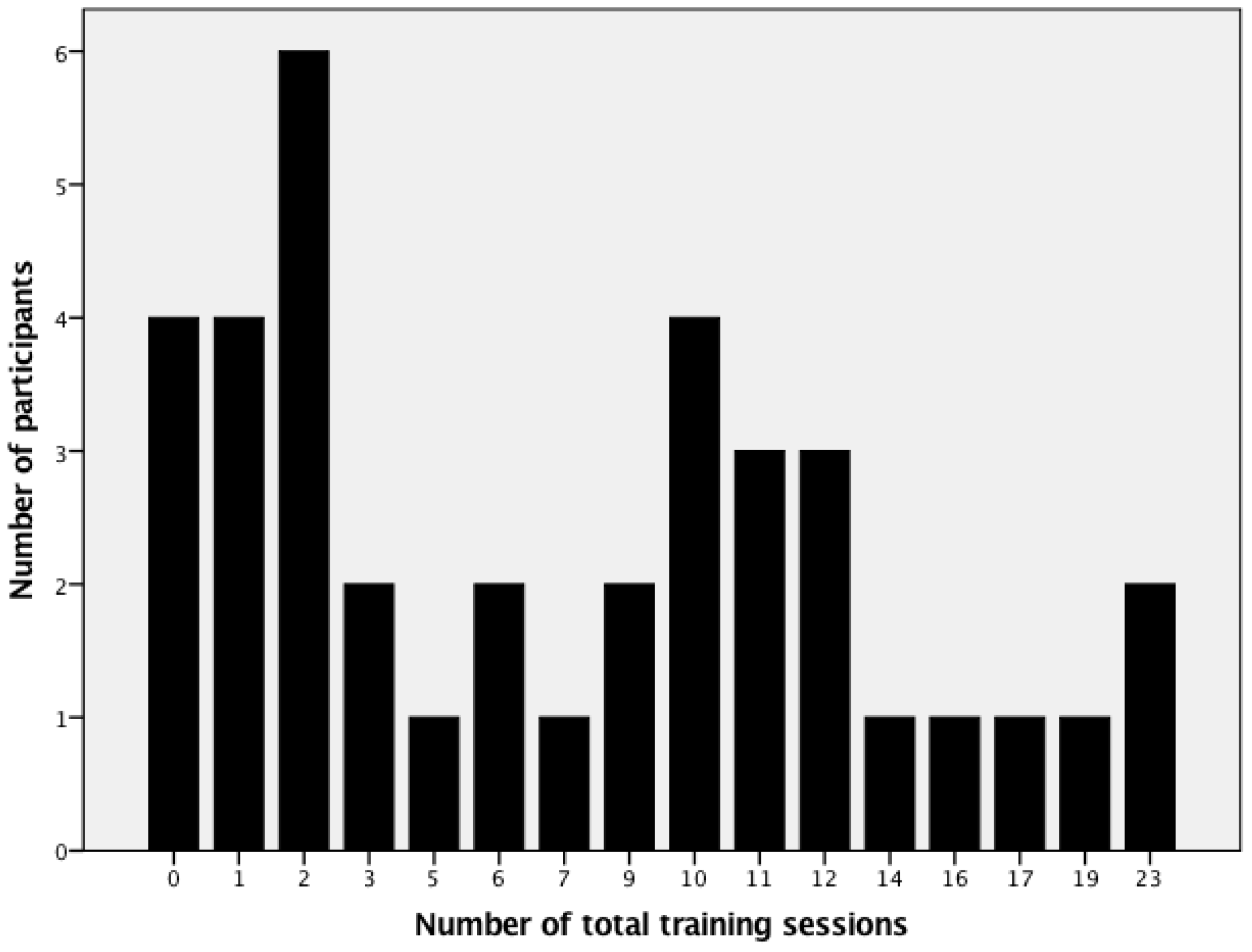
3.1. Descriptive Statistics and Dropout Analyses
3.2. Associations between Confounders and Outcomes at Baseline and Follow-Up
3.3. Changes from Baseline to Post-Intervention
3.4. Prediction of Post-Intervention Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- UNHCR. Global Trends. Forced Displacement. 2016. Available online: http://www.unhcr.org/576408cd7.pdf (accessed on 20 May 2018).
- Xin, H.; Karamehic-Muratovic, A.; Aydt Klein, N. Examining the effectiveness of physical activity on mental health among Bosnian refugees: A pilot study. Univ. J. Public Health 2017, 5, 76–84. [Google Scholar] [CrossRef]
- Madsen, T.S.; Carlsson, J.; Nordbrandt, M.S.; Jensen, J.A. Refugee experiences of individual basic body awareness therapy and the level of transference into daily life. An interview study. J. Bodyw. Mov. Ther. 2016, 20, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Gerritsen, A. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc. Psychiatry Epidemiol. 2006, 41, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Sharp, T.J.; Harvey, A.G. Chronic pain and posttraumatic stress disorder: Mutual maintenance? Clin. Psychol. Rev. 2001, 21, 857–877. [Google Scholar] [CrossRef]
- Hetrick, S.E.; Purcell, R.; Garner, B.; Parslow, R. Combined pharmacotherapy and psychologcial therapies for post traumatic stress disorder (PTSD). Cochrane Database Syst. Rev. 2010, 7, CD007316. [Google Scholar] [CrossRef]
- Korsik, A.; Ivarsson, V.; Nakitanda, O.A.; Perez Rosas, L.R. Implementing Sports in Refugee Camps; AISTS: Lausanne, Switzerland, 2013. [Google Scholar]
- Lawrence, S.; De Silva, M.; Henley, R. Sports and games for post-traumatic stress disorders (PTSD). Cochrane Database Syst. Rev. 2010, 20, CD007171. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Vancampfort, D.; Steel, Z.; Newby, J.; Ward, P.B.; Stubbs, B. Physical activity in the treatment of post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Res. 2015, 230, 130–136. [Google Scholar] [CrossRef]
- Fazel, M.; Wheeler, J.; Danesh, J. Prevalence of serious mental disorders in 7000 refugees resettled in Western countries: A systematic review. Lancet 2005, 365, 1309–1314. [Google Scholar] [CrossRef]
- Heeren, M.; Wittmann, L.; Ehlert, U.; Schnyder, U.; Maier, T.; Müller, J. Psychopathology and resident status—Comparing asylum seekers, refugees, illegal migrants, labor migrants, and residents. Compr. Psychiatry 2014, 55, 818–825. [Google Scholar] [CrossRef]
- Gerber, M.; Barker, D.; Pühse, U. Acculturation and physical activity among ethnic minorities: A systematic review. J. Public Health 2012, 20, 313–341. [Google Scholar] [CrossRef]
- Gadd, M.; Sundquist, J.; Johansson, S.E.; Wändell, P. Do immigrants have an increased prevalence of unhealthy behaviours and risk factors for coronary heart disease? Eur. J. Cardiovasc. Prev. Rehabil. 2005, 12, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Sandalio, R.N. Life after Trauma: The Mental Health Needs of Asylum Seekers in Europe; Migration Policy Institute: Washington, DC, USA, 2018. [Google Scholar]
- Liedl, A.; Müller, J.; Morina, N.; Karl, A.; Denke, C.; Knaevelsrud, C. Physical activity within a CBT intervention improves coping with pain in traumatized refugees: Results of randomized controlled design. Pain Med. 2011, 12, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Wieland, M.L.; Jiedje, K.; Meiers, S.J.; Mohamed, A.A.; Formea, C.M.; Ridgeway, J.L.; Asiedu, G.B.; Boyum, G.; Weis, J.A.; Nigon, J.A.; et al. Perspectives on physical activity among immigrants and refugees to a small urban community in Minnesota. J. Immigr. Minority Health 2015, 17, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Goel, M.S.; McCarthy, E.P.; Phillips, R.S.; Wee, C.C. Obesity among US immigrant subgroups by duration of residence. JAMA 2004, 292, 2860–2867. [Google Scholar] [CrossRef]
- Buhmann, C.B. Traumatized refugees: Morbidity, treatment and predictors of outcome. Dan. Med. J. 2014, 61, B4871. [Google Scholar]
- Walker, E.R.; McGee, R.E.; Druss, B.G. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 2015, 72, 334–341. [Google Scholar] [CrossRef]
- Horyniak, D.; Melo, J.S.; Farrell, R.M.; Oieda, V.D.; Strathdee, S.A. Epidemiology of substance use among forced migrants: A global systematic review. PLoS ONE 2016, 11, e0159134. [Google Scholar] [CrossRef]
- Abou-Saleh, M.T.; Hughes, P. Mental health of Syrian refugees: Looking backwards and forwards. Insight 2015, 2, 870–871. [Google Scholar] [CrossRef]
- Médecins Sans Frontières. EU Border Policies Fuel Mental Health Crisis for Asylum Seekers. 2017. Available online: https://www.msf.org/greece-eu-border-policies-fuel-mental-health-crisis-asylum-seekers (accessed on 4 March 2019).
- Brucks, U. Der blinde Fleck der medizinsichen Versorgung in Deutschland. Migration und psychische Erkrankung (The blind spot of medical care in Germany. Migration and mental illness). PsychoNeuro 2004, 30, 228–231. [Google Scholar]
- Nordbrandt, M.S.; Carlsson, J.; Glahder Lindberg, L.; Sandahl, H.; Mortensen, E.L. Treatment of traumatised refugees with basic body awareness therapy versus mixed physical activity as add-on treatment: Study protocol of a randomised controlled trial. Trials 2015, 16, 477. [Google Scholar] [CrossRef][Green Version]
- Stade, K.; Skammeritz, S.; Hjortkjaer, C.; Carlsson, J. “After all the traumas my body has been through, it feels good that it is still working.”—Basic body awareness therapy for traumatised refugees. Torture 2015, 25, 33–50. [Google Scholar] [PubMed]
- Nebiker, L.; Lichtenstein, E.; Minghetti, A.; Zahner, L.; Gerber, M.; Faude, O.; Donath, L. Moderating effects of exercise duration and intensity in neuromuscular versus endurance exercise interventions for the treatment of depression: A meta-analytical review with meta-regression and sensitivity analyses. Front. Psychiatry 2018, 9, 305. [Google Scholar] [CrossRef] [PubMed]
- Klavestrand, J.; Vingard, E. The relationship between physical activity and health-related quality of life: A systematic review of current evidence. Scand. J. Med. Sci. Sports 2009, 19, 300–312. [Google Scholar] [CrossRef] [PubMed]
- Danish Refugee Council. Code of Conduct. 2007. Available online: https://drc.ngo/media/1214238/drc-code-of-conduct.pdf (accessed on 29 July 2018).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Erlbaum: Mahwah, NJ, USA, 1988. [Google Scholar]
- Thomas, S.; Reading, J.; Shephard, R.J. Revision of the physical activity readiness questionnaire (PAR-Q). Can. J. Sport Sci. 1992, 17, 338–345. [Google Scholar] [PubMed]
- Weiss, D.S.; Marmar, C.R. The impact of event scale—Revised. In Assessing Psychological Trauma and PTSD; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar]
- Davey, C.; Heard, R.; Lennings, C. Development of the Arabic versions of the impact of events scale-revised and the posttraumatic growth inventory to assess trauma and growth in Middle Eastern refugees in Australia. Clin. Psychol. 2015, 19, 131–139. [Google Scholar] [CrossRef]
- Morina, N.; Ehring, T.; Priebe, S. Diagnostic utility of the impact of event scale—Revised in two sample of survivors of war. PLoS ONE 2013, 8, e83916. [Google Scholar] [CrossRef]
- Creamer, M.; Bell, R.; Falilla, S. Psychometric properties of the impact of event scale—Revised. Behav. Res. Ther. 2002, 41, 1489–1496. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. Validity of a brief depression severity measure. J. Gen. Int. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Feyera, F.; Mihretie, G.; Bedaso, A.; Gedle, D.; Kumera, G. Prevalence of depression and associated factors among Somali refugee at Melkadida camp, southeast Ethiopia: A cross-sectional study. BMC Psychiatry 2015, 15, 171. [Google Scholar] [CrossRef]
- Alhadi, A.N.; Alateeq, D.A.; Al-Sharif, E.; Bawazeer, H.M.; Alanazi, H.; Alahomrani, A.T.; Shuqdar, R.M.; Alowaybil, R. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann. Gen. Psychiatry 2017, 16, 32. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the hospital anxiety and depression scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Herrmann, C. International experiences with the hospital anxiety and depression scale: A review of validation data and clinical results. J. Psychosom. Res. 1997, 42, 17–41. [Google Scholar] [CrossRef]
- Huskisson, E.C. Measurement of pain. Lancet 1974, 2, 1127–1131. [Google Scholar] [CrossRef]
- Blom, E.H.; Bech, P.; Högberg, G.; Larsson, J.O.; Serlachius, E. Screening for depressed mood in an adolescent psychiatric context by brief self- assessment scales—Testing psychometric validity of WHO-5 and BDI-6 indices by latent trait analyses. Health Qual. Life Outcomes 2012, 10, 149. [Google Scholar] [CrossRef] [PubMed]
- Bech, P.; Olsen, L.R.; Kjoller, M.; Rasmussen, N.K. Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 mental health subscale and the WHO-five well-being scale. Int. J. Mehthods Psychiatr. Res. 2003, 12, 85–91. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 well-being index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Plante, T.G.; LeCaptain, S.E.; McLain, H.C. Perceived fitness predicts daily coping better than physical activity. J. Appl. Biobehav. Res. 2000, 5, 66–79. [Google Scholar] [CrossRef]
- Plante, T.G.; Lantis, A.; Checa, G. The influence of perceived versus aerobic fitness on psychological health and physiological stress responsitivity. Int. J. Stress Manag. 1998, 5, 141–156. [Google Scholar] [CrossRef]
- Lang, C.; Brand, S.; Colledge, F.; Ludyga, S.; Pühse, U.; Gerber, M. Adolescents’ personal beliefs about sufficient physical activity are more closely related to sleep and psychological functioning than self-reported physical activity: A prospective study. J. Sport Health Sci. 2019, 8, 280–288. [Google Scholar] [CrossRef]
- Leger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Mayorga-Vega, D.; Aguilar-Soto, P.; Viciana, J. Criterion-related validity of the 20-m shuttle run test for estimating cardiorespiratory fitness: A meta-analysis. J. Sports Sci. Med. 2015, 14, 536–547. [Google Scholar] [PubMed]
- Council of Europe. Testing Physical Fitness: Eurofit Experimental Battery; Council of Europe: Strasbourg, France, 1983. [Google Scholar]
- Fukumori, N.; Yamamoto, Y.; Takegami, M.; Yamazaki, S.; Onishi, Y.; Sekiguchi, M.; Otani, K.; Konno, S.; Kikuchi, S.; Fukuhara, S. Association between hand-grip strength and depressive symptoms: Locomotive syndrome and health outcomes in Aizu cohort study (LOHAS). Age Ageing 2015, 44, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Haith-Cooper, M. Exercise and physical activity in asylum seekers in Northern England. BMC Public Health 2018, 18, 762. [Google Scholar] [CrossRef] [PubMed]
- Morres, I.D.; Hatzigeorgiadis, A.; Stathi, A.; Comoutos, N.; Arpin-Cribbie, C.; Krommidas, C.; Theodorakis, Y. Aerobic exercise for adult patients with major depressive disorder in mental health services: A systematic review and meta-analysis. Depress. Anxiety 2019, 36, 39–53. [Google Scholar] [CrossRef] [PubMed]
- Azevedo Da Silva, M.; Singh-Manoux, A.; Brunner, E.J.; Kaffashian, S.; Shipley, M.J.; Kivimäki, M.; Nabi, H. Bidirectional association between physical activity and symptoms of anxiety and depression: The Whitehall II study. Eur. J. Epidemiol. 2012, 27, 537–546. [Google Scholar] [CrossRef]
- Long, A.C.; Palermo, T.M.; Manees, A.M. Brief report: Using actigraphy to compare physical activity levels in adolescents with chronic pain and healthy adolescents. J. Pediatr. Psychol. 2008, 33, 660–665. [Google Scholar] [CrossRef]
- Acevedo, E.O.; Ekkekakis, P. Psychobiology of Physical Activity; Human Kinetics: Champaign, IL, USA, 2006. [Google Scholar]
- Ekkekakis, P.; Acevedo, E.O. Affective responses to acute exercise: Toward a psychobiological dose-response model. In Psychobiology of Physical Activity; Acevedo, E.O., Ekkekakis, P., Eds.; Human Kinetics: Champaign, IL, USA, 2006; pp. 91–110. [Google Scholar]
- Mücke, M.; Ludyga, S.; Colledge, F.; Gerber, M. Influence of regular physical activity and fitness on stress reactivity as measured with the trier social stress test protocol: A systematic review. Sports Med. 2018, 48, 2607–2622. [Google Scholar] [CrossRef]
- Gerber, M.; Isoard-Gautheur, S.; Schilling, R.; Ludyga, S.; Brand, S.; Colledge, F. When low leisure-time physical activity meets unsatisfied psychological needs: Insights from a stress-buffer perspective. Front. Psychiatry 2018, 9, 2097. [Google Scholar] [CrossRef]
- Lindwall, M.; Lindgren, E.-C. The effects of a 6-month exercise intervention programme on physical self-perceptions and social physique anxiety in non-physically active adolescent Swedish girls. Psychol. Sport Exerc. 2005, 6, 643–658. [Google Scholar] [CrossRef]
- Myers, J.; McAuley, P.; Lavie, C.J.; Despres, J.P.; Arena, R.; Kokkinos, P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: Their independent and interwoven importance to health status. Prog. Cariovasc. Dis. 2015, 57, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Börjesson, M.; Ljung, T.; Lindwall, M.; Jonsdottir, I. Fitness moderates the relationship between stress and cardiovascular risk factors. Med. Sci. Sports Exerc. 2016, 48, 2075–2081. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, B.; Rosenbaum, S.; Vancampfort, D.; Ward, P.B.; Schuch, F.B. Exercise improves cardiorespiratory fitness in people with depression: A meta-analysis of randomized controlled trials. J. Affect. Disord. 2016, 190, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Brien, S.E.; Katzmarzyk, P.T.; Craig, C.L.; Gauvin, L. Physical activity, cardiorespiratory fitness and body mass index as predictors of substantial weight gain and obesity: The Canadian physical activity longitudinal study. Can. J. Public Health 2007, 98, 121–124. [Google Scholar] [CrossRef]
- Chase, N.L.; Sui, X.; Lee, D.C.; Blair, S.N. The association of cardiorespiratory fitness and physical activity with incidence of hypertension in men. Am. J. Hypertens. 2009, 22, 417–424. [Google Scholar] [CrossRef]
- Leite, S.A.; Monk, A.M.; Upham, P.A.; Bergenstal, R.M. Low cardiorespiratory fitness in people at risk for type 2 diabetes: Early marker for insulin resistance. Diabetol. Metab. Syndr. 2009, 1, 8. [Google Scholar] [CrossRef]
- Arseneault, B.J.; Lachance, D.; Lemieux, I.; Almeras, N.; Tremblay, A.; Bouchard, C.; Pérusse, L.; Desprès, J.P. Visceral adipose tissue accumulation, cardiorespiratory fitness, and features of the metabolic syndrome. Arch. Int. Med. 2007, 167, 1518–1525. [Google Scholar] [CrossRef]
- Wainstein, H.M.; Feldman, M.; Shen, C.L.; Leonard, D.; Willis, B.L.; Finley, C.E.; Gruntmanis, U.; DeFina, L.F. The relationship betweeen cardiorespiratory fitness and bone mineral density in men: A cross-sectional study. Mayo Clin. Proc. 2016, 91, 726–734. [Google Scholar] [CrossRef]
- Pour, M.S.; Kumble, S.; Hanieh, S.; Biggs, B.-A. Prevalence of dyslipidaemia and micronutrient deficiencies among newly arrived Afghan refugees in rural Australia: A cross-sectional study. BMC Public Health 2014, 14, 896. [Google Scholar] [CrossRef][Green Version]
- Kinzie, J.D.; Riley, C.; McFarland, B.; Hayes, M.; Boehnlein, J.; Leaung, P.; Adams, G. High prevalence rates of diabetes and hypertension among refugee psychiatric patients. J. Nerv. Ment. Dis. 2008, 196, 108–112. [Google Scholar] [CrossRef]
- Ashdown-Franks, G.; Stubbs, B.; Koyanagi, A.; Schuch, F.B.; Firth, J.; Veronese, N.; Vancampfort, D. Handgrip strength and depression among 34,129 adults aged 50 years and older in six low- and middle-income countries. J. Affect. Disord. 2019, 243, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.W.; Perry, A.C. Perception of physical fitness and exercise self-efficacy and its contribution to the relationship between body dissatisfaction and physical fitness in female minority children. Int. J. Environ. Res. Public Health 2018, 15, 1187. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Holsboer-Trachsler, E.; Pühse, U.; Brand, S. Exercise is medicine for patients with major depressive disorders. But only if the “pill” is taken! Neuropsychiatr. Dis. Treat. 2016, 12, 1977–1981. [Google Scholar] [CrossRef] [PubMed]
- Wieland, M.L. Physical activity and nutrition among immigrant and refugee women. Womens Helath Issues 2012, 22, e225–e232. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 compendium of physical activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Dunn, A.L.; Trivedi, M.H.; Kampert, J.B.; Clark, C.G.; Chambliss, H.O. Exercise treatment for depression. Efficacy and dose response. Am. J. Prev. Med. 2005, 28, 1–8. [Google Scholar] [CrossRef] [PubMed]
| Baseline: Total Sample (n = 45) | Baseline: Dropouts (n = 7) | Baseline: Participants (n = 38) | Test of Group Differences at Baseline | Post: Participants (n = 38) | Test of Changes from Baseline to Post-Test | ||||
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | F | η2 | M (SD) | t | d | 95% Confidence Intervals | |
| Social and demographic background | |||||||||
| Age | 25.3 (6.8) | 23.5 (4.0) | 25.5 (7.1) | 0.47 | 0.011 | --- | --- | --- | |
| BMI | 22.2 (3.5) | 24.9 (4.6) | 21.8 (3.2) | 4.12 * | 0.089 | --- | --- | --- | |
| Years of education | 9.5 (3.2) | 10.0 (1.8) | 9.6 (3.3) | 0.10 | 0.002 | --- | --- | --- | |
| Months since fleeing home country | 34.0 (40.9) | 22.5 (25.0) | 32.9 (39.4) | 0.40 | 0.009 | --- | --- | --- | |
| Weeks in camp | 20.8 (18.1) | 26.4 (20.3) | 20.0 (18.2) | 0.47 | 0.013 | --- | --- | --- | |
| Primary and secondary outcomes | |||||||||
| PTSD symptoms | 48.1 (21.2) | 60.7 (16.2) | 45.7 (21.5) | 2.65 | 0.059 | 35.4 (25.5) | 3.53 ** | 0.57 | (0.23 to 0.91) |
| Depressive symptoms | 11.9 (6.3) | 16.3 (7.3) | 11.1 (6.0) | 3.80 + | 0.083 | 9.2 (6.2) | 2.48 * | 0.40 | (0.07 to 0.73) |
| Anxiety symptoms | 9.6 (4.2) | 12.2 (4.0) | 9.1 (4.2) | 2.76 | 0.062 | 8.2 (5.0) | 1.53 | 0.25 | (−0.08 to 0.57) |
| Sleep complaints | 14.1 (6.0) | 17.8 (5.9) | 13.4 (6.0) | 2.88 + | 0.064 | 11.1 (7.6) | 2.11 * | 0.34 | (0.01 to 0.67) |
| Pain | 128.3 (94.6) | 216.8 (130.4) | 109.0 (74.9) | 8.64 ** | 0.171 | 91.9 (72.6) | 1.55 | 0.25 | (−0.07 to 0.57) |
| Health-related quality of life | 8.1 (5.9) | 5.3 (4.7) | 8.6 (6.0) | 1.61 | 0.037 | 10.6 (6.8) | −1.72 + | −0.28 | (−0.60 to 0.15) |
| Self-perceived fitness | 5.0 (2.2) | 4.8 (3.3) | 5.1 (2.1) | 0.05 | 0.001 | 5.3 (2.0) | −1.07 + | −0.17 | (−0.49 to 0.15) |
| Handgrip strength test | 41.0 (6.7) | 42.4 (9.2) | 41.0 (6.2) | 0.24 | 0.006 | 44.9 (6.7) | −5.61 *** | −0.91 | (−0.53 to −1.28) |
| 20 m shuttle run test | 46.6 (16.1) | 37.8 (4.4) | 48.3 (16.9) | 2.24 | 0.051 | 50.7 (19.0) | −1.34 | −0.21 | (−0.54 to 0.11) |
| PTSD Symptoms | Depressive Symptoms | Anxiety Symptoms | Sleep Complaints | Pain | ||||||
| β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | |
| Step 1 | 0.533 *** | 0.536 *** | 0.415 *** | 0.298 *** | 0.334 *** | |||||
| Age | 0.14 | --- | --- | --- | --- | |||||
| Weeks in camp | --- | 0.07 | --- | --- | --- | |||||
| Baseline score | 0.67 *** | 0.73 *** | 0.65 | 0.51 *** | 0.56 *** | |||||
| Step 2 | 0.036 + | 0.042 + | 0.036 + | 0.040 | 0.041 | |||||
| Participation | −0.19 + | −0.29 + | −0.27 * | −0.21 | −0.20 | |||||
| Step 3 | 0.001 | 0.002 | 0.002 | 0.022 | 0.022 | |||||
| Baseline score × Participation | 0.03 | 0.04 | −0.05 | −0.15 | −0.18 | |||||
| R2 = 0.570 *** | R2 = 0.580 *** | R2 = 0.487 *** | R2 = 0.360 *** | R2 = 0.397 ** | ||||||
| Health-Related Quality of Life | Self-Perceived Fitness | Handgrip Strength Test | 20 m Shuttle Run Test | |||||||
| β | ΔR2 | β | ΔR2 | β | ΔR2 | β | ΔR2 | |||
| Step 1 | 0.155 * | 0.444 *** | 0.612 *** | 0.676 *** | ||||||
| Age | --- | --- | --- | −0.05 | ||||||
| Baseline score | 0.40 ** | 0.62 *** | 0.76 *** | 0.75 *** | ||||||
| Step 2 | 0.083 + | 0.098 ** | 0.048 * | 0.043 * | ||||||
| Participation | 0.32 * | 0.32 ** | 0.23* | 0.22 * | ||||||
| Step 3 | 0.034 | 0.001 | 0.002 | 0.002 | ||||||
| Baseline score × Participation | −0.19 | −0.04 | −0.04 | −0.04 | ||||||
| R2 | R2 = 0.272 * | R2 = 0.543 *** | R2 = 0.662 *** | R2 = 0.721 *** | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knappe, F.; Colledge, F.; Gerber, M. Impact of an 8-Week Exercise and Sport Intervention on Post-Traumatic Stress Disorder Symptoms, Mental Health, and Physical Fitness among Male Refugees Living in a Greek Refugee Camp. Int. J. Environ. Res. Public Health 2019, 16, 3904. https://doi.org/10.3390/ijerph16203904
Knappe F, Colledge F, Gerber M. Impact of an 8-Week Exercise and Sport Intervention on Post-Traumatic Stress Disorder Symptoms, Mental Health, and Physical Fitness among Male Refugees Living in a Greek Refugee Camp. International Journal of Environmental Research and Public Health. 2019; 16(20):3904. https://doi.org/10.3390/ijerph16203904
Chicago/Turabian StyleKnappe, Florian, Flora Colledge, and Markus Gerber. 2019. "Impact of an 8-Week Exercise and Sport Intervention on Post-Traumatic Stress Disorder Symptoms, Mental Health, and Physical Fitness among Male Refugees Living in a Greek Refugee Camp" International Journal of Environmental Research and Public Health 16, no. 20: 3904. https://doi.org/10.3390/ijerph16203904
APA StyleKnappe, F., Colledge, F., & Gerber, M. (2019). Impact of an 8-Week Exercise and Sport Intervention on Post-Traumatic Stress Disorder Symptoms, Mental Health, and Physical Fitness among Male Refugees Living in a Greek Refugee Camp. International Journal of Environmental Research and Public Health, 16(20), 3904. https://doi.org/10.3390/ijerph16203904





