How Do Nurses Cope with Shift Work? A Qualitative Analysis of Open-Ended Responses from a Survey of Nurses
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Recruitment
2.2. Participant Characteristics
2.3. Data Collection
2.4. Data Analysis
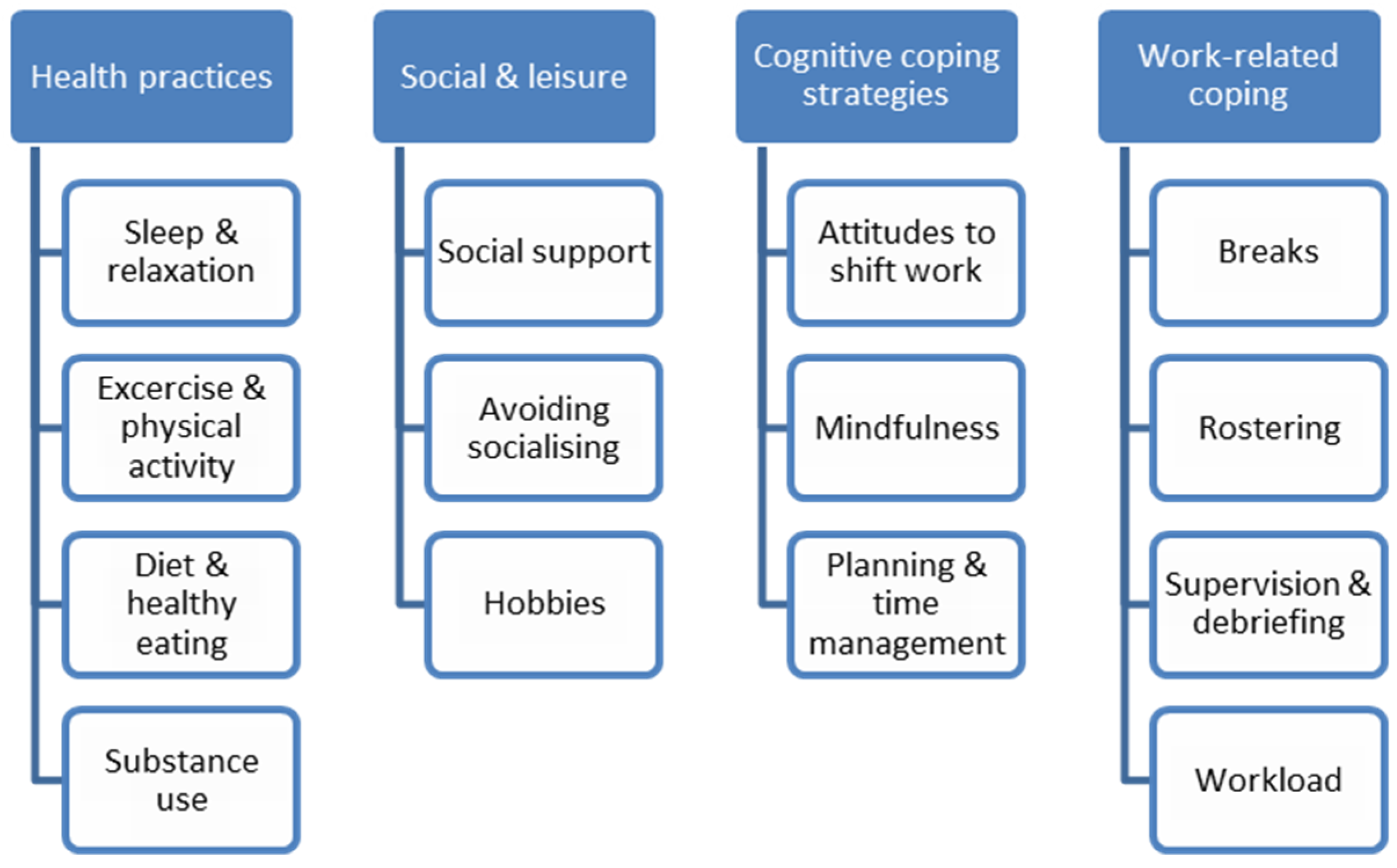
3. Results
3.1. Health Practices
3.1.1. Sleep and Relaxation
“Try and get as much sleep as I can to allow me to be less tired.”.(Participant 102, female, age 25)
“I try to ensure I get rest after work but resting/sleeping affects my ability to socialise with people.”.(Participant 13, female, age 24)
“I try to relax when I have days off. However, this impacts on the other activities which promote a healthy life, such as exercise and healthy eating.”.(Participant 253, male, age 31)
3.1.2. Exercise and Physical Activity
“I de-stress through physical activity. However, when exhausted I cannot do this and this has a negative impact on my wellbeing.”.(Participant 307, female, age 33)
“I struggle but try and participate in exercise every day.”.(Participant 267, female, age 28)
3.1.3. Diet and Healthy Eating
“Learning to adapt. Eat healthy. Eat minimal on night shift and only light things such as cut up carrot.”.(Participant 221, female, age not specified)
“Eat well at work. Take a full dinner break and not talk at dinner.”.(Participant 350, female, age 34)
“I pre-prepare food and shopping before my nights in order to minimise tasks and improve eating when tired.”.(Participant 13, female, age 24)
3.1.4. Substance Use
“Unfortunately falling into the quick fixes of caffeine drinks to stay awake and having to see a doctor about sleep and prescribed melatonin and temazepam.”.(Participant 231, female, age 34)
“Take a lot of sleeping tablets to at least get some sleep during the day.”.(Participant 435, male, age 49)
“Take non-prescription medication and sleep.”.(Participant 403, male, age not specified)
“Plan nice days off and drink alcohol.”.(Participant 188, female, age 27)
3.2. Social and Leisure
3.2.1. Social Support
“I am a very social person and find that taking solace in my large community of friends keeps me going. We spend what time we can together, and I like to go out dancing etc. to blow off steam.”.(Participant 326, non-binary/third gender, age 25)
“I try to spend a lot of my free time socialising with friends and debriefing about anything stressful.”.(Participant 274, female, age 28)
3.2.2. Avoiding Socialising
“I like to get up as late as possible (after a shift). Withdraw to myself to get emotional/psychological recharge from a reduction in the social stimulus. I need wind down time after shifts of 2+ hours to stop mind racing and allow for some sleep.”.(Participant 353, male, age 43)
“Try to engage in activities that I think are important and avoid others.”.(Participant 67, female, age 62)
“I cope by being disengaged from activities requiring regular commitment. I prepare all significant others in my world for the likelihood of being tired and unable to participate in some events.”.(Participant 319, female, age 54)
3.2.3. Hobbies
“I ride my horse 3 to 4 times a week. I book annual leave so that I can participate in clinics and competitions with my horse.”.(Participant 271, female, age 37)
“Try to enjoy things that provide some emotional wellbeing like gardening for me, walking dog, enjoying family, and grandchildren.”.(Participant 68, female, age 55)
3.3. Cognitive Coping Strategies
3.3.1. Mindfulness
“Practice mindfulness meditation daily.”.(Participant 184, female, age 46)
“Making sure l attend church, pray on the way to work, and outside activities.”.(Participant 211, male, age 58)
3.3.2. Attitudes to Shift Work
“I like shift work as it allows me to do more activity than a regular 9–5 worker.”.(Participant 279, female, age 53)
“Acknowledge I have a stable job with sustainable income, I get more time with my young family.”.(Participant 446, male, age 26)
“I don’t feel I have any coping mechanisms, I don’t believe I need any, work is work.”.(Participant 306, female, age 22)
“I have to accept it and survive.”.(Participant 282, female, age 62)
“I have got used to feeling like this as done shift work for 30 years.”.(Participant 451, female, age 50)
3.3.3. Planning and Time Management
“I set alarms and have my roster written on the fridge. Keep a diary also and have my roster on my phone.”.(Participant 102, female, age 25)
“Making sure time is allocated to enjoy yourself.”.(Participant 375, female, age 30)
3.4. Work-Related Coping
3.4.1. Breaks
“I will utilise sick leave if exhaustion becomes overwhelming, or if my mental health feels unstable.”.(Participant 277, female, age not specified)
“Try to take short A/L (annual leave) breaks to rest and recover every 3 months”.(Participant 436, male, age 46)
“When I am on day shift I tend to break up my shifts to not work long stretches, if possible.”.(Participant 16, female, age 56)
“Take a full dinner break.”.(Participant 350, female, age 34)
3.4.2. Rostering
“I ask to have my days off together because I need the break to recover.”.(Participant 152, female, age 60)
“I rely on good rostering so I can have at least two days off in a row after Night shift and minimal number of Late/Early short changeover occasions, work no more than 32 hours per week for past 20 years.”.(Participant 185, female, age 60)
“I try to ensure I put in roster requests that suit my lifestyle to try and have as much as a normal work life balance as I can.”.(Participant 259, female, age 28)
3.4.3. Workload
“I have reduced my hours to a 0.7 EFT [equivalent full time] commitment in one location, and add to those hours casually elsewhere (on days I am not tired). The past 12 months this has been a significant improvement in my energy levels, and I have joined a gym and trained more.”.(Participant 13, female, age 24)
“Dropped my work hours to 48 hours for fortnight, trying to look after myself first rather than earning more money.”.(Participant 404, female, age 32)
“I stress less now I have become a casual worker and have the choice of where and when to work. No worries about getting holiday leave approved.”.(Participant 320, female, age 59)
3.4.4. Supervision and Debriefing
“I engage in clinical supervision.”.(Participant 117, male, age 27)
“I tend to debrief at work if required before I go home, even if it means staying late, I always relax more quickly after work when I do this.”.(Participant 185, female, age 60)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- National Sleep Foundation. What Is Shift Work? Available online: https://sleepfoundation.org/shift-work/content/what-shift-work (accessed on 9 July 2019).
- Beers, T.M. Flexible schedules and shift work: Replacing the 9-to-5 workday. Mon. Labor Rev. 2000, 123, 33–40. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Australian Labour Market Statistics; Australian Bureau of Statistics: Canberra, Australia, 2010.
- McMenamin, T.M. A time to work: Recent trends in shift work and flexible schedules. Mon. Labor Rev. 2007, 130, 3–15. [Google Scholar]
- Steel, M. Changes in Shift Work Patterns over the Last Ten Years (1999 to 2009); Office for National Statistics for the Health and Safety Executive 2011: Newport, UK, 2011.
- Williams, C. Work-Life Balance of Shift Workers; Perspectives on Labour and Income: Ottawa, ON, Canada, 2008. [Google Scholar]
- Reppert, S.M.; Weaver, D.R. Coordination of circadian timing in mammals. Nature 2002, 418, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Pevet, P.; Challet, E. Melatonin: Both master clock output and internal time-giver in the circadian clocks network. J. Physiol. Paris 2011, 105, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, C.A.; Duffy, J.F.; Shanahan, T.L.; Brown, E.N.; Mitchell, J.F.; Rimmer, D.W.; Ronda, J.M.; Silva, E.J.; Allan, J.S.; Emens, J.S.; et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science 1999, 284, 2177–2181. [Google Scholar] [CrossRef] [PubMed]
- Rajaratnam, S.M.W.; Arendt, J. Health in a 24-h society. Lancet 2001, 358, 999–1005. [Google Scholar] [CrossRef]
- Carrier, J.; Monk, T.H. Circadian rhythms of performance: New trends. Chronobiol. Int. 2000, 17, 719–732. [Google Scholar] [CrossRef]
- Schmidt, C.; Collette, F.; Cajochen, C.; Peigneux, P. A time to think: Circadian rhythms in human cognition. Cogn. Neuropsychol. 2007, 24, 755–789. [Google Scholar] [CrossRef]
- Sallinen, M.; Kecklund, G. Shift work, sleep, and sleepiness—Differences between shift schedules and systems. Scand. J. Work Environ. Health 2010, 36, 121–133. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef]
- Vallières, A.; Azaiez, A.; Moreau, V.; LeBlanc, M.; Morin, C.M. Insomnia in shift work. Sleep Med. 2014, 15, 1440–1448. [Google Scholar] [CrossRef] [PubMed]
- Rajaratnam, S.M.W.; Barger, L.K.; Lockley, S.W.; Shea, S.A.; Wang, W.; Landrigan, C.P.; O’Brien, C.S.; Qadri, S.; Sullivan, J.P.; Cade, B.E.; et al. Sleep disorders, health, and safety in police officers. JAMA 2011, 306, 2567–2578. [Google Scholar] [CrossRef] [PubMed]
- Zhai, L.; Zhang, H.; Zhang, D. Sleep duration and depression among adults: A meta-analysis of prospective studies. Depress. Anxiety 2015, 32, 664–670. [Google Scholar] [CrossRef] [PubMed]
- Wright, K.P.; Bogan, R.K.; Wyatt, J.K. Shift work and the assessment and management of shift work disorder (SWD). Sleep Med. Rev. 2013, 17, 41–54. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic & Coding Manual; American Academy of Sleep Medicine: Westchester, IL, USA, 2005. [Google Scholar]
- Barger, L.K.; Ogeil, R.P.; Drake, C.L.; O’Brien, C.S.; Ng, K.T.; Rajaratnam, S.M.W. Validation of a questionnaire to screen for shift work disorder. Sleep 2012, 35, 1693–1703. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic review of shift work and nurses’ health. Occup. Med. 2019, 69, 237–243. [Google Scholar] [CrossRef]
- Erren, T.C.; Falaturi, P.; Morfeld, P.; Knauth, P.; Reiter, R.J.; Piekarski, C. Shift work and cancer: The evidence and the challenge. Dtsch. Arztebl. Int. 2010, 107, 657–662. [Google Scholar] [CrossRef]
- Grundy, A.; Sanchez, M.; Richardson, H.; Tranmer, J.; Borugian, M.; Graham, C.H.; Aronson, K.J. Light intensity exposure, sleep duration, physical activity, and biomarkers of melatonin among rotating shift nurses. Chronobiol. Int. 2009, 26, 1443–1461. [Google Scholar] [CrossRef]
- He, C.; Anand, S.T.; Ebell, M.H.; Vena, J.E.; Robb, S.W. Circadian disrupting exposures and breast cancer risk: A meta-analysis. Int. Arch. Occup. Environ. Health 2015, 88, 533–547. [Google Scholar] [CrossRef]
- Wang, F.; Yeung, K.L.; Chan, W.C.; Kwok, C.C.H.; Leung, S.L.; Wu, C.; Chan, E.Y.Y.; Yu, I.T.S.; Yang, X.R.; Tse, L.A. A meta-analysis on dose–response relationship between night shift work and the risk of breast cancer. Ann. Oncol. 2013, 24, 2724–2732. [Google Scholar] [CrossRef]
- Costa, G. Shift work and occupational medicine: An overview. Occup. Med. 2003, 53, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Caruso, C.C. Negative impacts of shiftwork and long work hours. Rehabil. Nurs. 2014, 39, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Fathi, A.; Hajizadeh, M.; Moradi, K.; Zandian, H.; Dezhkameh, M.; Kazemzadeh, S.; Rezaei, S. Medication errors among nurses in teaching hospitals in the west of Iran: What we need to know about prevalence, types, and barriers to reporting. Epidemiol. Health 2017, 39, e2017022. [Google Scholar] [CrossRef] [PubMed]
- Sprinks, J. Pinpointing the risks and benefits of shift patterns. Nurs. Stand. (2014+) 2015, 29, 12–13. [Google Scholar] [CrossRef] [PubMed]
- Gaudine, A.; Saks, A.M.; Dawe, D.; Beaton, M. Effects of absenteeism feedback and goal-setting interventions on nurses’ fairness perceptions, discomfort feelings and absenteeism. J. Nurs. Manag. 2013, 21, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Gifkins, J.; Johnston, A.; Loudoun, R. The impact of shift work on eating patterns and self-care strategies utilised by experienced and inexperienced nurses. Chronobiol. Int. 2018, 35, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Chang, E.M.; Daly, J.W.; Hancock, K.M.; Bidewell, J.; Johnson, A.; Lambert, V.A.; Lambert, C.E. The relationships among workplace stressors, coping methods, demographic characteristics, and health in Australian nurses. J. Prof. Nurs. 2006, 22, 30–38. [Google Scholar] [CrossRef]
- Samaha, E.; Lal, S.; Samaha, N.; Wyndham, J. Psychological, lifestyle and coping contributors to chronic fatigue in shift-worker nurses. J. Adv. Nurs. 2007, 59, 221–232. [Google Scholar] [CrossRef]
- Schluter, P.J.; Turner, C.; Benefer, C. Long working hours and alcohol risk among Australian and New Zealand nurses and midwives: A cross-sectional study. Int. J. Nurs. Stud. 2012, 49, 701–709. [Google Scholar] [CrossRef]
- Australian Government, Department of Health. National Health Workforce Dataset Summary Statistics. Available online: https://hwd.health.gov.au/summary.html (accessed on 26 August 2019).
- Novak, R.D.; Auvil-Novak, S.E. Focus group evaluation of night nurse shiftwork difficulties and coping strategies. Chronobiol. Int. 1996, 13, 457–463. [Google Scholar] [CrossRef]
- Akbar, R.E.; Elahi, N.; Mohammadi, E.; Khoshknab, M.F. What strategies do the nurses apply to cope with job stress? A qualitative study. Glob. J. Health Sci. 2015, 8, 55–64. [Google Scholar] [CrossRef]
- Burnard, P.; Edwards, D.; Fothergill, A.; Hannigan, B.; Coyle, D. Community mental health nurses in Wales: Self-reported stressors and coping strategies. J. Psychiatr. Ment. Health Nurs. 2000, 7, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Healy, C.M.; McKay, M.F. Nursing stress: The effects of coping strategies and job satisfaction in a sample of Australian nurses. J. Adv. Nurs. 2000, 31, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Bogossian, F.; Ahern, K. Stress and coping in Australian nurses: A systematic review. Int. Nurs. Rev. 2010, 57, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Tahghighi, M.; Rees, C.S.; Brown, J.A.; Breen, L.J.; Hegney, D. What is the impact of shift work on the psychological functioning and resilience of nurses? An integrative review. J. Adv. Nurs. 2017, 73, 2065–2083. [Google Scholar] [CrossRef] [PubMed]
- Persson, M.; Mårtensson, J. Situations influencing habits in diet and exercise among nurses working night shift. J. Nurs. Manag. 2006, 14, 414–423. [Google Scholar] [CrossRef]
- Happell, B.; Reid-Searl, K.; Dwyer, T.; Caperchione, C.M.; Gaskin, C.J.; Burke, K.J. How nurses cope with occupational stress outside their workplaces. Collegian 2013, 20, 195–199. [Google Scholar] [CrossRef]
- Dorrian, J.; Centofanti, S.; Colella, A.; Devine, L.; Dingle, C.; Galindo, H.; Pantelios, S.; Brkic, G.; Bull, C.; Almond, T.; et al. Coping with Shiftwork: Understanding and Communicating Resilience Strategies for Performance, Safety and Health; University of South Australia: Adelaide, Australia, 2017. [Google Scholar]
- Dorrian, J.; Lamond, N.; van den Heuvel, C.; Pincombe, J.; Rogers, A.E.; Dawson, D. A pilot study of the safety implications of Australian nurses’ sleep and work hours. Chronobiol. Int. 2006, 23, 1149–1163. [Google Scholar] [CrossRef]
- Centofanti, S.; Banks, S.; Colella, A.; Dingle, C.; Devine, L.; Galindo, H.; Pantelios, S.; Brkic, G.; Dorrian, J. Coping with shift work-related circadian disruption: A mixed-methods case study on napping and caffeine use in Australian nurses and midwives. Chronobiol. Int. 2018, 35, 853–864. [Google Scholar] [CrossRef]
- Ogeil, R.P.; Phillips, J.G. Commonly used stimulants: Sleep problems, dependence and psychological distress. Drug Alcohol Depend. 2015, 153, 145–151. [Google Scholar] [CrossRef]
- Ogeil, R.P.; Phillips, J.G.; Savic, M.; Lubman, D.I. Sleep- and wake-promoting drugs: Where are they being sourced, and what is their impact? Subst. Use Misuse 2019, 54, 1916–1928. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.-M.; Sun, N.; Hong, S.; Fan, Y.-Y.; Kong, F.-Y.; Li, Q.-J. Occupational stress and coping strategies among emergency department nurses of China. Arch. Psychiatr. Nurs. 2015, 29, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Pisarski, A.; Bohle, P.; Callan, V.J. Effects of coping strategies, social support and work-nonwork conflict on shift worker’s health. Scand. J. Work Environ. Health 1998, 24, 141–145. [Google Scholar] [PubMed]
- Lambert, V.A.; Lambert, C.E.; Ito, M. Workplace stressors, ways of coping and demographic characteristics as predictors of physical and mental health of Japanese hospital nurses. Int. J. Nurs. Stud. 2004, 41, 85–97. [Google Scholar] [CrossRef]
- Ritchie, J.; Spencer, L.; O’Connor, W. Carrying out qualitative analysis. In Qualitative Research Practice: A Guide for Social Science Students and Researchers; Ritchie, J., Lewis, J., Eds.; SAGE Publications: London, UK, 2003; pp. 219–262. [Google Scholar]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. 2013, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- O’Cathain, A.; Thomas, K.J. “Any other comments?” Open questions on questionnaires—A bane or a bonus to research? BMC Med. Res. Methodol. 2004, 4, 25. [Google Scholar] [CrossRef] [PubMed]
- Ainley, E.; King, J.; Käsbauer, S.; Cooper, R. A framework analysis of free-text data from the neonatal survey 2014. J. Neonatal Nurs. 2018, 24, 163–168. [Google Scholar] [CrossRef]
- Schirmann, A.; Boyle, F.M.; Horey, D.; Siassakos, D.; Ellwood, D.; Rowlands, I.; Flenady, V. Understanding mothers’ decision-making needs for autopsy consent after stillbirth: Framework analysis of a large survey. Birth 2018, 45, 255–262. [Google Scholar] [CrossRef]
- Harrington, J.M. Health effects of shift work and extended hours of work. Occup. Environ. Med. 2001, 58, 68–72. [Google Scholar] [CrossRef]
- Adams, R.; Appleton, S.; Taylor, A.; McEvoy, D.; Antic, N. Report to the Sleep Health Foundation 2016 Sleep Health Survey of Australian Adults; The University of Adelaide, The Adelaide Institute for Sleep Health: Adelaide, Australia, 2017. [Google Scholar]
- Geiger-Brown, J.; Rogers, V.E.; Trinkoff, A.M.; Kane, R.L.; Bausell, R.B.; Scharf, S.M. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol. Int. 2012, 29, 211–219. [Google Scholar] [CrossRef]
- Manomenidis, G.; Panagopoulou, E.; Montgomery, A. The ‘switch on–switch off model’: Strategies used by nurses to mentally prepare and disengage from work. Int. J. Nurs. Pract. 2016, 22, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Sleep Health Foundation. Caffeine and Sleep. Available online: https://www.sleephealthfoundation.org.au/caffeine-and-sleep.html (accessed on 23 August 2019).
- Lo, R. A longitudinal study of perceived level of stress, coping and self-esteem of undergraduate nursing students: An Australian case study. J. Adv. Nurs. 2002, 39, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Munro, L.; Rodwell, J.; Harding, L. Assessing occupational stress in psychiatric nurses using the full job strain model: The value of social support to nurses. Int. J. Nurs. Stud. 1998, 35, 339–345. [Google Scholar] [CrossRef]
- Henderson, N.J.; Burt, C.D.B. An evaluation of the effectiveness of shift work preparation strategies. N. Z. J. Psychol. 1998, 27, 13–20. [Google Scholar]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Jetten, J.; Haslam, C.; Haslam, S.A.; Dingle, G.; Jones, J.M. How groups affect our health and well-being: The path from theory to policy. Soc. Issues Policy Rev. 2014, 8, 103–130. [Google Scholar] [CrossRef]
- Jensen, H.I.; Larsen, J.W.; Thomsen, T.D. The impact of shift work on intensive care nurses’ lives outside work: A cross-sectional study. J. Clin. Nurs. 2018, 27, e703–e709. [Google Scholar] [CrossRef]
- Amirkhan, J.H.; Risinger, R.T.; Swickert, R.J. Extraversion: A “hidden” personality factor in coping? J. Personal. 1995, 63, 189–212. [Google Scholar] [CrossRef]
- Eastburg, M.C.; Williamson, M.; Gorsuch, R.; Ridley, C. Social support, personality, and burnout in nurses. J. Appl. Soc. Psychol. 1994, 24, 1233–1250. [Google Scholar] [CrossRef]
- Mahon, M.A.; Mee, L.; Brett, D.; Dowling, M. Nurses’ perceived stress and compassion following a mindfulness meditation and self compassion training. J. Res. Nurs. 2017, 22, 572–583. [Google Scholar] [CrossRef]
- Grover, S.L.; Teo, S.T.T.; Pick, D.; Roche, M. Mindfulness as a personal resource to reduce work stress in the job demands-resources model. Stress Health 2017, 33, 426–436. [Google Scholar] [CrossRef] [PubMed]
- Krausz, M.; Koslowsky, M. Impact of shift work and department type upon strain and attitudinal measures of hospital nurses. Work Stress 1995, 9, 88–94. [Google Scholar] [CrossRef]
- Smith, L.; Tanigawa, T.; Takahashi, M.; Mutou, K.; Tachibana, N.; Kage, Y.; Iso, H. Shiftwork locus of control, situational and behavioural effects on sleepiness and fatigue in shiftworkers. Ind. Health 2005, 43, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.; White, B.; Muncer, S. Nurses’ cognitive structural models of work-based stress. J. Adv. Nurs. 1999, 29, 974–983. [Google Scholar] [CrossRef] [PubMed]
- Bennett, P.; Lowe, R.; Matthews, V.; Dourali, M.; Tattersall, A. Stress in nurses: Coping, managerial support and work demand. Stress Health 2001, 17, 55–63. [Google Scholar] [CrossRef]
- Bartram, T.; Joiner, T.A.; Stanton, P. Factors affecting the job stress and job satisfaction of Australian nurses: Implications for recruitment and retention. Contemp. Nurse 2004, 17, 293–304. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | N (%) 1 |
|---|---|
| Gender | |
| Female | 394 (87.8) |
| Male | 53 (11.8) |
| Non-binary/third gender | 1 (0.2) |
| Prefer not to say | 1 (0.2) |
| Age | |
| ≤30 years | 110 (28.9) |
| 31–39 years | 70 (18.4) |
| 40–49 years | 80 (21.0) |
| 50–59 years | 98 (25.7) |
| ≥60 years | 23 (6.0) |
| Employment status | |
| Ongoing | 392 (87.3) |
| Fixed term | 31 (6.9) |
| Casual | 24 (5.3) |
| Executive contract | 2 (0.4) |
| Average hours worked (past month) | |
| 0 | 4 (0.9) |
| 1–40 | 392 (87.3) |
| >40 | 53 (11.8) |
| Years worked in current role | |
| ≤5 years | 207 (47.9) |
| 6–10 years | 107 (24.8) |
| 11–15 years | 50 (11.6) |
| 16–20 years | 28 (6.5) |
| >20 years | 40 (9.3) |
| Types of shift worked in past month | |
| Day (6:00am–7:00pm) | 385 (85.7) |
| Evening (3:00pm–12:00am) | 387 (86.2) |
| Night (10:00pm–8:00am) | 288 (64.1) |
| Frequency of night shifts (10:00pm–8:00am) | |
| Nearly every day | 12 (2.7) |
| 2–4 times per week | 107 (23.8) |
| 3–4 times per month | 108 (24.1) |
| 1–2 times per month | 68 (15.1) |
| Rarely/nearly never | 153 (34.1) |
| Frequency of rotating shifts | |
| Nearly every day | 188 (41.9) |
| 2–4 times per week | 110 (24.5) |
| 3–4 times per month | 41 (9.1) |
| 1–2 times per month | 42 (9.4) |
| Rarely/nearly never | 68 (15.1) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savic, M.; Ogeil, R.P.; Sechtig, M.J.; Lee-Tobin, P.; Ferguson, N.; Lubman, D.I. How Do Nurses Cope with Shift Work? A Qualitative Analysis of Open-Ended Responses from a Survey of Nurses. Int. J. Environ. Res. Public Health 2019, 16, 3821. https://doi.org/10.3390/ijerph16203821
Savic M, Ogeil RP, Sechtig MJ, Lee-Tobin P, Ferguson N, Lubman DI. How Do Nurses Cope with Shift Work? A Qualitative Analysis of Open-Ended Responses from a Survey of Nurses. International Journal of Environmental Research and Public Health. 2019; 16(20):3821. https://doi.org/10.3390/ijerph16203821
Chicago/Turabian StyleSavic, Michael, Rowan P. Ogeil, Megan J. Sechtig, Peta Lee-Tobin, Nyssa Ferguson, and Dan I. Lubman. 2019. "How Do Nurses Cope with Shift Work? A Qualitative Analysis of Open-Ended Responses from a Survey of Nurses" International Journal of Environmental Research and Public Health 16, no. 20: 3821. https://doi.org/10.3390/ijerph16203821
APA StyleSavic, M., Ogeil, R. P., Sechtig, M. J., Lee-Tobin, P., Ferguson, N., & Lubman, D. I. (2019). How Do Nurses Cope with Shift Work? A Qualitative Analysis of Open-Ended Responses from a Survey of Nurses. International Journal of Environmental Research and Public Health, 16(20), 3821. https://doi.org/10.3390/ijerph16203821





