Bacterial Contamination on Latrine Surfaces in Community and Household Latrines in Kathmandu, Nepal
Abstract
1. Introduction
2. Materials and Methods
2.1. Site Selection
2.2. Community Toilet Site Swabbing
2.3. Household Toilet Swabbing
2.4. Swabbing Methods
2.5. Lab Methods
2.6. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization/UNICEF. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines; World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF): Geneva, Switzerland, 2017; ISBN 978-92-4-151289-3. [Google Scholar]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet Lond. Engl. 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Prüss-Üstün, A.; Bos, R.; Gore, F.; Bartram, J. Safer Water, Better Health: Costs, Benefits and Sustainability of Interventions to Protect and Promote Health; World Health Organization: Geneva, Switzerland, 2008; ISBN 978-92-4-159643-5. [Google Scholar]
- Flores, G.E.; Bates, S.T.; Knights, D.; Lauber, C.L.; Stombaugh, J.; Knight, R.; Fierer, N. Microbial biogeography of public restroom surfaces. PLoS ONE 2011, 6, e28132. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, M.A.; Elimelech, M. Water and sanitation in developing countries: Including health in the equation. Environ. Sci. Technol. 2007, 41, 17–24. [Google Scholar] [CrossRef] [PubMed]
- WHO/UNICEF. Progress on Sanitation and Drinking Water—2015 update and MDG assessment; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Progress on Drinking Water and Sanitation: 2014 Update; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-92-4-150724-0.
- Heijnen, M.; Cumming, O.; Peletz, R.; Chan, G.K.-S.; Brown, J.; Baker, K.; Clasen, T. Shared Sanitation versus Individual Household Latrines: A systematic review of health outcomes. PLoS ONE 2014, 9, e93300. [Google Scholar] [CrossRef] [PubMed]
- Exley, J.L.R.; Liseka, B.; Cumming, O.; Ensink, J.H.J. The sanitation ladder, what constitutes an improved form of sanitation? Environ. Sci. Technol. 2015, 49, 1086–1094. [Google Scholar] [CrossRef] [PubMed]
- Least Developed Country Category: Nepal Profile|Economic Analysis & Policy Division. Available online: https://www.un.org/development/desa/dpad/least-developed-country-category-nepal.html (accessed on 9 October 2018).
- World Urbanization Prospects: The 2014 Revision; The United Nations: New York, NY, USA, 2014; ISBN 978-92-1-151517-6.
- Regmi, L.K. An Overview of Population Growth Trends of Nepal. J. Inst. Sci. Technol. 2015, 19, 57–61. [Google Scholar] [CrossRef]
- 2.6 Million Nepalis Still Lack Toilet—General—The Kathmandu Post. Available online: http://kathmandupost.ekantipur.com/news/2017-11-21/26-million-nepalis-still-lack-toilet.html (accessed on 9 October 2018).
- Nepal: Annual Household Survey 2015/16—Nepal. Available online: https://reliefweb.int/report/nepal/ nepal-annual-household-survey-201516 (accessed on 9 October 2018).
- Sinclair, R.G.; Gerba, C.P. Microbial contamination in kitchens and bathrooms of rural Cambodian village households. Lett. Appl. Microbiol. 2011, 52, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Progress on Drinking Water and Sanitation: 2012 Update|UNICEF Publications|UNICEF. Available online: https://www.unicef.org/publications/index_69025.html (accessed on 15 October 2018).
- Kwiringira, J.; Atekyereza, P.; Niwagaba, C.; Kabumbuli, R.; Rwabukwali, C.; Kulabako, R.; Günther, I. Seasonal variations and shared latrine cleaning practices in the slums of Kampala city, Uganda. BMC Public Health 2016, 16, 361. [Google Scholar] [CrossRef] [PubMed]
- Tumwebaze, I.K.; Mosler, H.-J. Shared toilet users’ collective cleaning and determinant factors in Kampala slums, Uganda. BMC Public Health 2014, 14, 1260. [Google Scholar] [CrossRef] [PubMed]
- Sonego, I.L.; Mosler, H.-J. Why are some latrines cleaner than others? Determining the factors of habitual cleaning behaviour and latrine cleanliness in rural Burundi. J. Water Sanit. Hyg. Dev. 2014, 4, 257–267. [Google Scholar] [CrossRef]
- Kwiringira, J.; Atekyereza, P.; Niwagaba, C.; Günther, I. Gender variations in access, choice to use and cleaning of shared latrines; experiences from Kampala Slums, Uganda. BMC Public Health 2014, 14, 1180. [Google Scholar] [CrossRef] [PubMed]
- Biran, A.; Schmidt, W.-P.; Wright, R.; Jones, T.; Seshadri, M.; Isaac, P.; Nathan, N.A.; Hall, P.; McKenna, J.; Granger, S.; et al. The effect of a soap promotion and hygiene education campaign on handwashing behaviour in rural India: A cluster randomised trial. Trop. Med. Int. Health 2009, 14, 1303–1314. [Google Scholar] [CrossRef] [PubMed]
- Fewtrell, L.; Kaufmann, R.B.; Kay, D.; Enanoria, W.; Haller, L.; Colford, J.M. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: A systematic review and meta-analysis. Lancet Infect. Dis. 2005, 5, 42–52. [Google Scholar] [CrossRef]
- Briscoe, C.; Aboud, F. Behaviour change communication targeting four health behaviours in developing countries: A review of change techniques. Soc. Sci. Med. 2012, 75, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Rusin, P.; Maxwell, S.; Gerba, C. Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria, and phage. J. Appl. Microbiol. 2002, 93, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Tiimub, B.M.; Forson, M.A.; Obiri-Danso, K.; Rahaman, I.A. Pointed gaps in the provision, quality, patronage and management of toilet facilities in Bawku East District. In Water, Sanitation and Hygiene: Sustainable Development and Multisectoral Approaches, Proceedings of the 34th WEDC International Conference, United Nations Conference Centre, Addis Ababa, Ethiopia, 18–22 May 2009; Water, Engineering and Development Centre (WEDC), Loughborough University of Technology: Loughborough, UK, 2009; pp. 715–720. [Google Scholar]
- Monsell, L.; Dullaghan, N.; Krastev, S.; Pilat, D. Applying Behavior Change to Promote Gender—Symmetrical Public Toilet Usage in Nepal; Aerosan Behavioral Diagnostic Report; The Decision Lab: Montreal, QC, Canada, 2018. [Google Scholar]
- Patterns and Determinants of Communal Latrine Usage in Urban Poverty Pockets in Bhopal, India. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21414114 (accessed on 15 October 2018).
- Savichtcheva, O.; Okabe, S. Alternative indicators of fecal pollution: Relations with pathogens and conventional indicators, current methodologies for direct pathogen monitoring and future application perspectives. Water Res. 2006, 40, 2463–2476. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.; Griffith, C. Problems associated with traditional hygiene swabbing: The need for in-house standardization. J. Appl. Microbiol. 2007, 103, 1090–1103. [Google Scholar] [CrossRef] [PubMed]
- Wigger, C.; Morris, P.S.; Stevens, M.; Smith-Vaughan, H.; Hare, K.; Beissbarth, J.; Leach, A.J. A comparison of flocked nylon swabs and non-flocked rayon swabs for detection of respiratory bacteria in nasopharyngeal carriage in Australian Indigenous children. J. Microbiol. Methods 2019, 157, 47–49. [Google Scholar] [CrossRef] [PubMed]
- Chavda, K.D.; Satlin, M.J.; Chen, L.; Manca, C.; Jenkins, S.G.; Walsh, T.J.; Kreiswirth, B.N. Evaluation of a Multiplex PCR Assay to Rapidly Detect Enterobacteriaceae with a Broad Range of β-Lactamases Directly from Perianal Swabs. Antimicrob. Agents Chemother. 2016, 60, 6957–6961. [Google Scholar] [CrossRef] [PubMed]
| Surface ID | Household Latrines | Community Latrines | |||||
|---|---|---|---|---|---|---|---|
| Surface Type | Average Area Swabbed | N | Surface Type | Average Area Swabbed | N (Dirty) | N (Clean) | |
| TS | Toilet seat for cistern flush toilets or latrine slab for pit latrines | 76 cm2 | 5 | Latrine slab | 55 cm2 | 16 | 11 |
| AC | Spray handle/bucket for anal cleansing | 23 cm2 | 5 | Tap used for anal cleansing | 140 cm2 | 16 | 11 |
| DH | Door Handle | 82 cm2 | 5 | Door Handle | 30 cm2 | 16 | 11 |
| W | Wall (Pit latrines only) | 100 cm2 | 2 | Wall | 100 cm2 | 16 | 11 |
| SH | Sink handle at handwashing station | 424 cm2 | 3 | Sink handle at handwashing station | 218 cm2 | 6 | 3 |
| F | Flush (cistern flush toilets only) | 10 cm2 | 3 | Flush (United States control site only) | 28 cm2 | 6 | 1 |
| Fl | Floor (United States control site only) | 100 cm2 | 5 | ||||
| M | Money (collected from latrine operator at community site 1) * | 45 cm2 | 2 | ||||
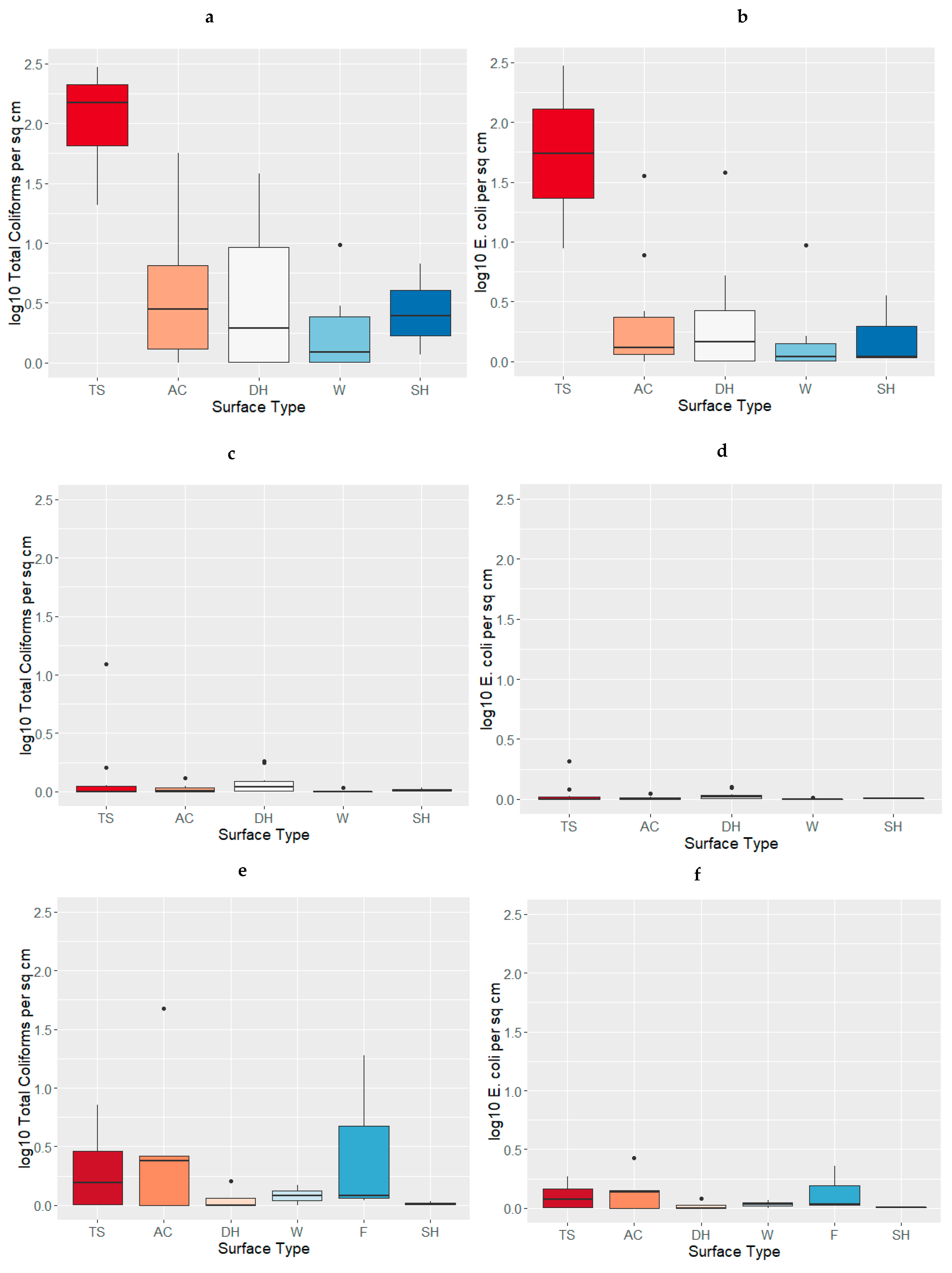
| Site-Types | Surface Type | Sample N | Total Coliforms Median cfu/cm2 | Total Coliforms Range | E. coli Median cfu/cm2 | E. coli Range |
|---|---|---|---|---|---|---|
| Community-Dirty | TS | 10 | 214 | (20–1060) | 56 | (8–295) |
| AC | 10 | 2 | (0–56) | 0.3 | (0–34) | |
| DH | 10 | 1 | (0–37) | 0.5 | (0–37) | |
| W | 10 | 0.2 | (0–9) | 0.1 | (0–8) | |
| SH | 3 | 1 | (0.2–6) | 0.1 | (0.07–3) | |
| Community–Clean | TS | 10 | 0.03 | (0–11) | 0 | (0–1) |
| AC | 10 | 0.02 | (0–0.3) | 0.01 | (0–0.1) | |
| DH | 10 | 0.1 | (0–0.8) | 0.04 | (0–0.3) | |
| W | 10 | 0 | (0–0.01) | 0 | (0–0.03) | |
| SH | 3 | 0.02 | (0.02–0.1) | 0.01 | (0–0.05) | |
| Households | TS | 5 | 0.5 | (0–6) | 0.2 | (0–0.9) |
| AC | 5 | 1 | (0–47) | 0.4 | (0–23) | |
| DH | 5 | 0 | (0–0.6) | 0 | (0–0.2) | |
| W | 2 | 0.2 | (0–0.5) | 0.1 | (0–0.2) | |
| F | 3 | 0.2 | (0.1–18) | 0.08 | (0.04–1) | |
| SH | 3 | 0.03 | (0–0.7) | 0.01 | (0–0.03) | |
| Control Site (USA) | TS | 5 | 0 | NA | 0 | NA |
| DH | 5 | 0 | (0–0.01) | 0 | NA | |
| F | 5 | 0 | NA | 0 | NA | |
| Fl | 5 | 0 | (0–0.1) | 0 | NA | |
| SH | 3 | 0 | NA | 0 | NA | |
| Money * | M | 2 | 0.2 | (0–0.3) | 0.03 | (0–0.06) |
| Surface Type | Total Coliforms | E. coli | ||||
|---|---|---|---|---|---|---|
| Median (cfu/cm2) Before Cleaning | Median (cfu/cm2) After Cleaning | p-Value | Median (cfu/cm2) Before Cleaning | Median (cfu/cm2) After Cleaning | p-Value | |
| TS | 214.77 | 0 | <0.01 | 56.25 | 0.003 | <0.01 |
| AC | 1.90 | 0.02 | 0.01 | 0.30 | 0.01 | 0.01 |
| DH | 0.99 | 0.10 | 0.06 | 0.47 | 0.04 | 0.06 |
| W | 0.24 | 0 | 0.01 | 0.1 | 0 | 0.02 |
| SH | 1.46 | 0.24 | 0.25 | 0.09 | 0.01 | 0.25 |
| Surface Type | Total Coliforms | E. coli | ||||
|---|---|---|---|---|---|---|
| Household Median (cfu/cm2) | Community Median (cfu/cm2) Before Cleaning | p-Value | Household Median (cfu/cm2) | Community Median (cfu/cm2) Before Cleaning | p-Value | |
| TS | 0.55 | 214.77 | <0.01 | 0.19 | 56.25 | <0.01 |
| AC | 1.39 | 1.90 | 0.67 | 0.38 | 0.30 | 0.67 |
| DH | 0 | 0.99 | 0.16 | 0 | 0.47 | 0.10 |
| W | 0.24 | 0.24 | 0.59 | 0.08 | 0.10 | 0.66 |
| F | 0.08 | NA | NA | 0.08 | NA | NA |
| SH | 0.03 | 1.46 | 0.10 | 0.01 | 0.09 | 0.10 |
| Surface Type | Total Coliforms | E. coli | ||||
|---|---|---|---|---|---|---|
| Household Median (cfu/cm2) | Community Median (cfu/cm2) After Cleaning | p-Value | Household Median (cfu/cm2) | Community Median (cfu/cm2) After Cleaning | p-Value | |
| TS | 0.58 | 0 | 0.22 | 0.19 | 0.004 | 0.28 |
| AC | 1.39 | 0.02 | 0.50 | 0.38 | 0.01 | 0.50 |
| DH | 0 | 0.10 | 0.45 | 0 | 0.04 | 0.45 |
| W | 0.24 | 0 | 0.19 | 0.08 | 0 | 0.19 |
| F | 0.29 | NA | NA | 0.08 | NA | NA |
| SH | 0.03 | 0.02 | 1 | 0.01 | 0.01 | 1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGinnis, S.; Marini, D.; Amatya, P.; Murphy, H.M. Bacterial Contamination on Latrine Surfaces in Community and Household Latrines in Kathmandu, Nepal. Int. J. Environ. Res. Public Health 2019, 16, 257. https://doi.org/10.3390/ijerph16020257
McGinnis S, Marini D, Amatya P, Murphy HM. Bacterial Contamination on Latrine Surfaces in Community and Household Latrines in Kathmandu, Nepal. International Journal of Environmental Research and Public Health. 2019; 16(2):257. https://doi.org/10.3390/ijerph16020257
Chicago/Turabian StyleMcGinnis, Shannon, Dianna Marini, Prakash Amatya, and Heather M. Murphy. 2019. "Bacterial Contamination on Latrine Surfaces in Community and Household Latrines in Kathmandu, Nepal" International Journal of Environmental Research and Public Health 16, no. 2: 257. https://doi.org/10.3390/ijerph16020257
APA StyleMcGinnis, S., Marini, D., Amatya, P., & Murphy, H. M. (2019). Bacterial Contamination on Latrine Surfaces in Community and Household Latrines in Kathmandu, Nepal. International Journal of Environmental Research and Public Health, 16(2), 257. https://doi.org/10.3390/ijerph16020257




