Spatial Accessibility to Healthcare Services in Metropolitan Suburbs: The Case of Qingpu, Shanghai
Abstract
1. Introduction
2. Study Area, Data Sources, and Research Methods
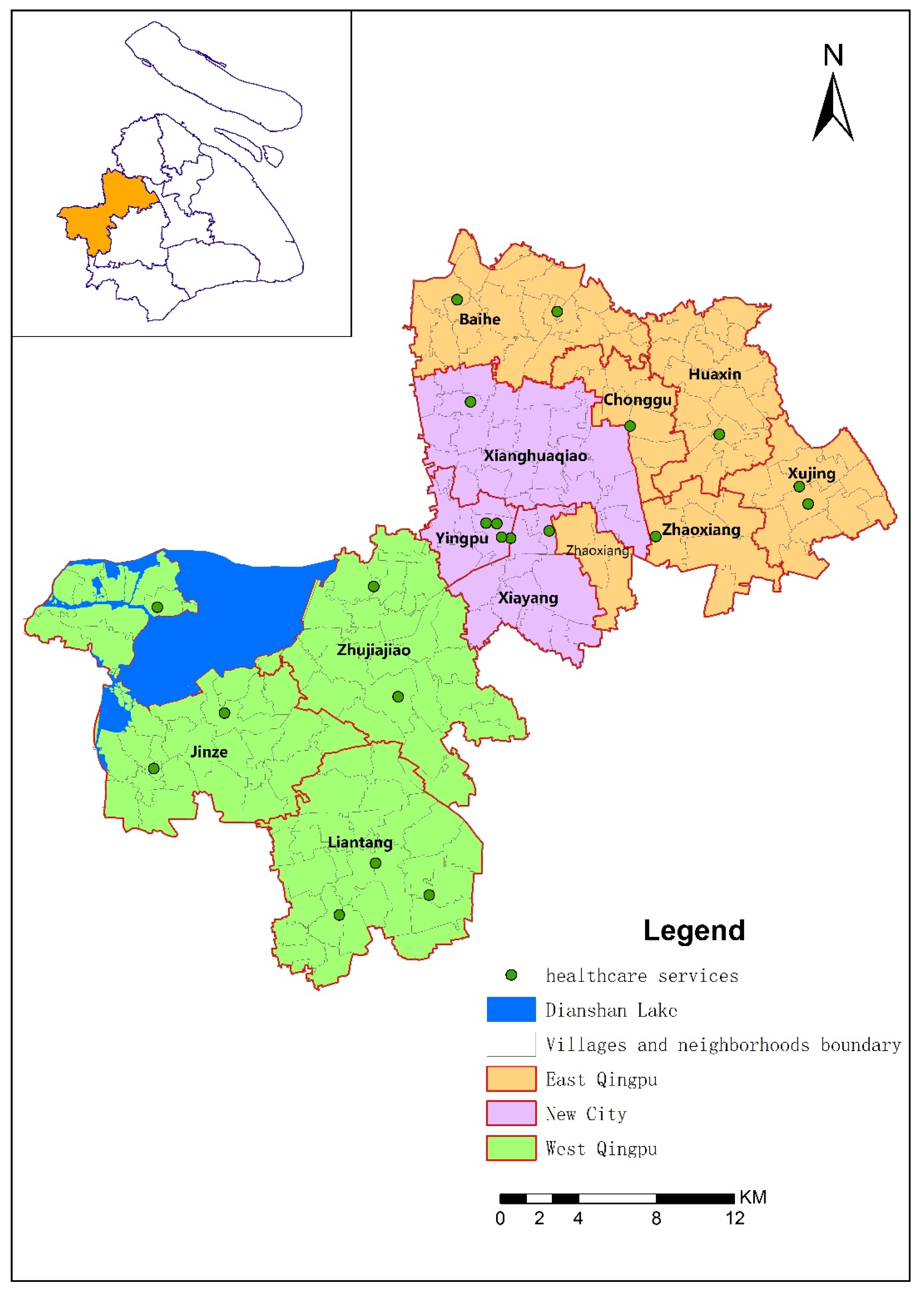
2.1. Study Area
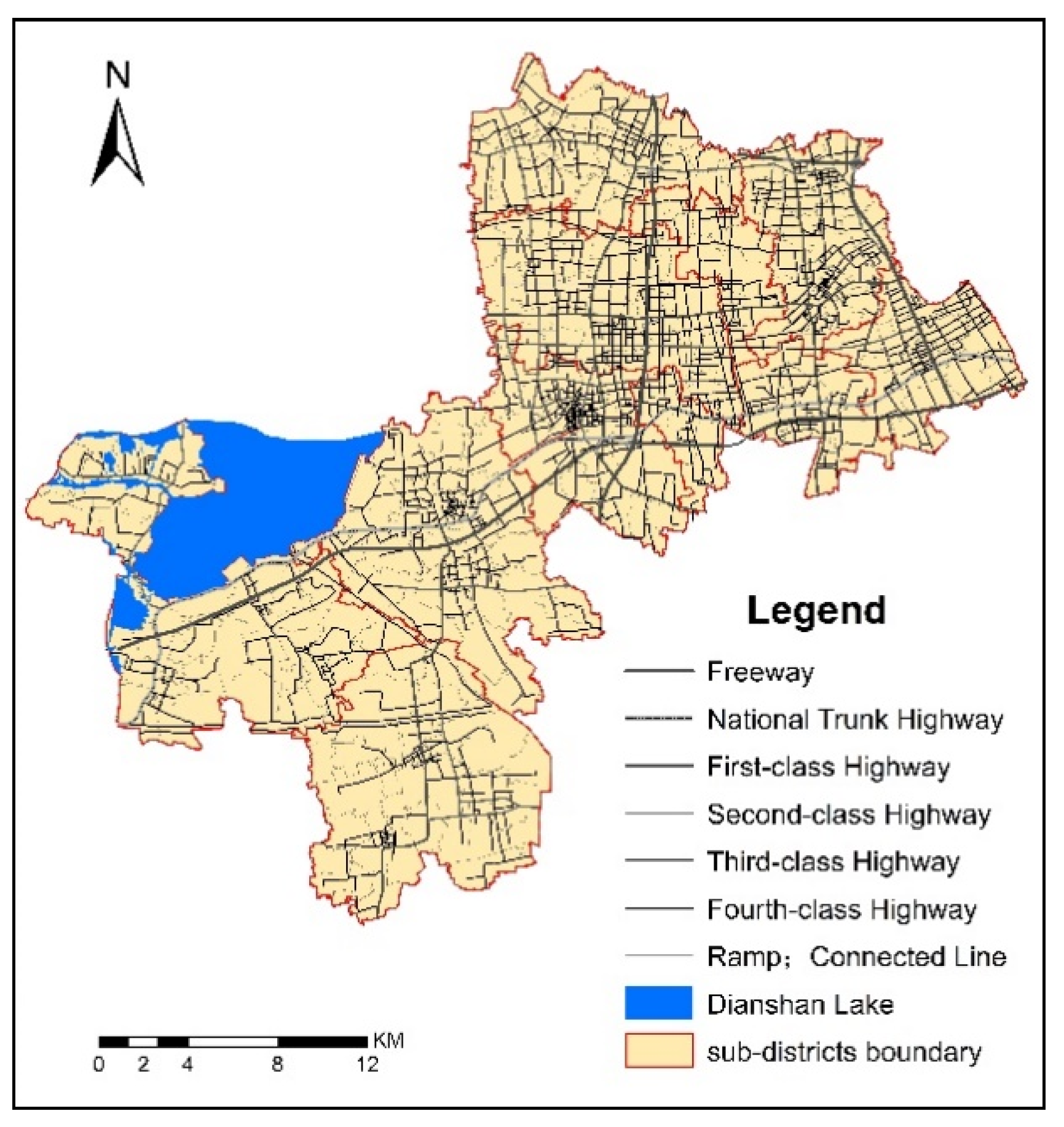
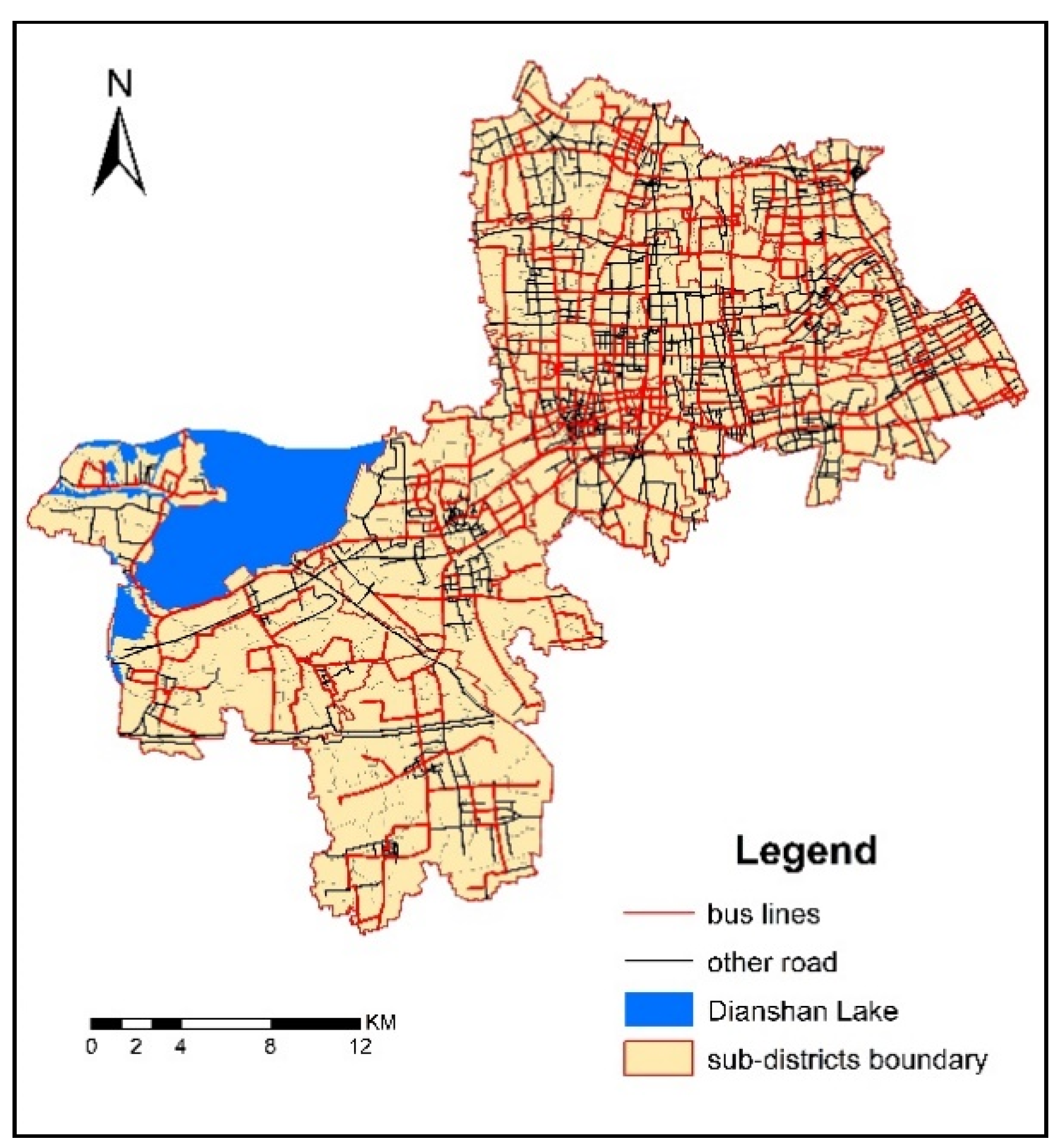
2.2. Data Sources
2.3. Research Methods
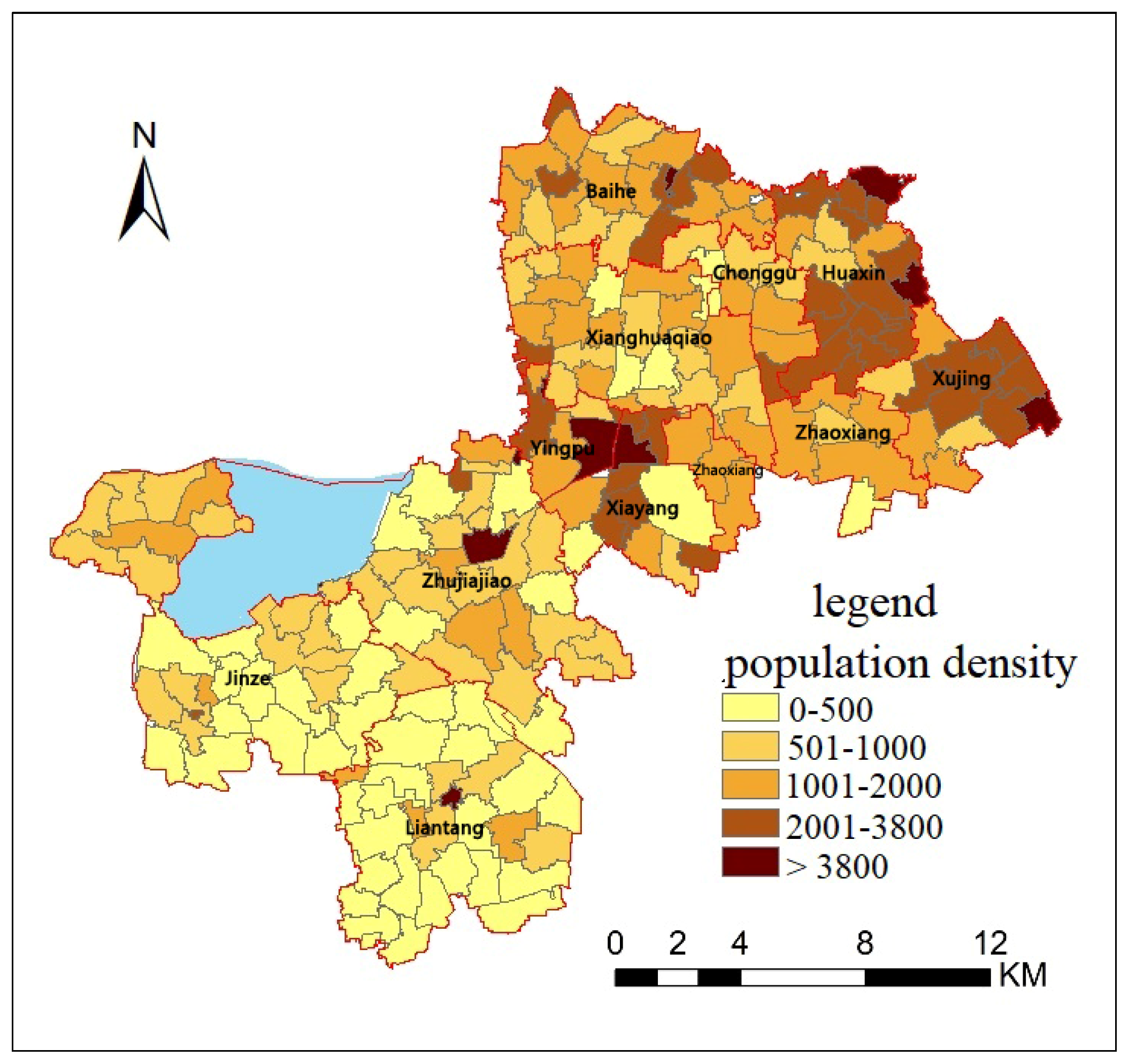
2.3.1. Population Distribution
2.3.2. Service Radius and Threshold
2.3.3. Healthcare Service Spatial Accessibility Index
3. Results
3.1. Spatial Accessibility to Healthcare Services by Public Transportation
3.2. Spatial Accessibility to Healthcare Services by Self-Driving
3.3. Sensitivity Analysis between the Different Transportation Mode and Travel Time
4. Discussion
4.1. Differences of Spatial Accessibility by Different Transportation Modes
4.2. Differences of Spatial Accessibility in the Qingpu
4.3. Influences of Planning and Policy
4.4. Potential Limitation and Directions for Further Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Li, Y.; Wei, Y.H.D. A Spatial-Temporal Analysis of Health Care and Mortality Inequalities in China. Eurasian Geogr. Econ. 2010, 51, 767–787. [Google Scholar] [CrossRef]
- WHO. The Declaration of Alma-Ata on Primary Health Care 1978. Available online: http://apps.who.int/iris/bitstream/10665/39228/1/9241800011.pdf (accessed on 20 December 2018).
- WHO. Sustainable Health Financing, Universal Coverage and Social Health Insurance 2005. Available online: http://apps.who.int/iris/bitstream/10665/20383/1/WHA58_33-en.pdf (accessed on 20 December 2018).
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Shan, L.; Wu, Q.; Liu, C.; Ye, L.; Yu, C.; Zi, L.; Hao, Y.; Liang, L.; Ning, N.; Ding, D. Perceived challenges to achieving universal health coverage: A cross-sectional survey of social health insurance managers/administrators in China. BMJ OPEN 2017, 7, e14425. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yang, H.; Duan, Z.; Pan, J. Spatial accessibility of primary health care in China: A case study in Sichuan Province. Soc. Sci. Med. 2018, 209, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Cutler, D.M.; Lleras-Muney, A.; Vogl, T. Socioeconomic Status and Health: Dimensions and Mechanisms; NBER Working Papers; National Bureau of Economic Research: Cambridge, MA, USA, 2008.
- Aday, L.A.; Andersen, R. A framework for the study of access to medical care. Health Serv. Res. 1974, 9, 208–220. [Google Scholar] [PubMed]
- Albert, D.P.; Butar, F.B. Estimating the de-designation of single-county HPSAs in the United States by counting naturopathic physicians as medical doctors. Appl. Geogr. 2005, 25, 271–285. [Google Scholar] [CrossRef]
- Wang, F.; Luo, W. Assessing spatial and nonspatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health Place 2005, 11, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Berke, E.M.; Xun, S. Computing travel time when the exact address is unknown: A comparison of point and polygon ZIP code approximation methods. Int. J. Health Geogr. 2009, 8, 23. [Google Scholar] [CrossRef] [PubMed]
- Luo, W. Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health Place 2004, 10, 1–11. [Google Scholar] [CrossRef]
- UN Habitat World Cities Report 2016: Urbanization and Development—Emerging Futures; UN: New York, NY, USA, 2016.
- Guang, S. Experience and inspiration on regional health planning in Germany and other eight developed countries. Health Econ. Res. 2009, 9, 22–25. [Google Scholar]
- Meng, T. Zhang J. Evaluation of Health Care Service Spatial Accessibility and the Analysis of the Spatial Distribution Characteristics in Beijing. Geospat. Inf. 2017, 15, 62–66. [Google Scholar]
- Liao, Z.Q.; Jiang, H.X. Urban Medical Facilities Spatial Accessibility Based on Improved Potential Model—A Case Study in Cangshan, Fuzhou. J. Fujian Norm. Univ. 2018, 1, 38–49. [Google Scholar]
- Tong, S.N.; Chen, H.H. Evaluation of accessibility of medical facilities based on street scale—A case study in Shenzhen city. Health Econ. Res. 2017, 2, 31–34. [Google Scholar]
- Wu, Q. Study on the Balanced Configurationof Public Health Resources under the Background of Shanghai Urban and Rural Integration. Master’s Thesis, Shanghai University of Engineering Science, Shanghai, China, 2015. [Google Scholar]
- Liu, J. The Evaluation on Equitable Distribution of Xi’an Health Service Facilities. Master’s Thesis, Xi’an International Studies University, Xi’an, China, 2015. [Google Scholar]
- Tao, Z.; Yao, Z.; Kong, H.; Duan, F.; Li, G. Spatial accessibility to healthcare services in Shenzhen, China: Improving the multi-modal two-step floating catchment area method by estimating travel time via online map APIs. BMC Health Serv. Res. 2018, 18, 345. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Li, M. Research on spatial accessibility of medical facilities based on improved 2SFCA. Inf. Rec. Mater. 2018, 19, 115–118. [Google Scholar]
- Tao, Z.; Cheng, Y.; Zheng, Q.; Li, G. Measuring spatial accessibility to healthcare services with constraint of administrative boundary: A case study of Yanqing District, Beijing, China. Int. J. Equity Health 2018, 17, 7. [Google Scholar] [CrossRef]
- Zheng, C. Analysis of Spatial Accessibility to Medical Institutions in County-level City Based on GIS: A Case Study of Shishi, Fujian. Trop. Geogr. 2011, 31, 598–603. [Google Scholar]
- Cheng, G.; Zeng, X.; Duan, L.; Lu, X.; Sun, H.; Jiang, T.; Li, Y. Spatial difference analysis for accessibility to high level hospitals based on travel time in Shenzhen, China. Habitat Int. 2016, 53, 485–494. [Google Scholar] [CrossRef]
- Pan, J.; Zhao, H.; Wang, X.; Shi, X. Assessing spatial access to public and private hospitals in Sichuan, China: The influence of the private sector on the healthcare geography in China. Soc. Sci. Med. 2016, 170, 35–45. [Google Scholar] [CrossRef]
- Gu, X.; Tao, S.; Dai, B. Spatial accessibility of country parks in Shanghai, China. Urban For. Urban Green. 2017, 27, 373–382. [Google Scholar] [CrossRef]
- Shanghai Statistical Bureau. Shanghai Statistical Yearbook 2016. Available online: http://www.stats-sh.gov.cn/tjnj/tjnj2016.htm# (accessed on 21 December 2018).
- Shanghai Municipal People’s Government. Shanghai Regional Health Planning (2001–2010). Available online: http://www.wsjsw.gov.cn/zhghjh/20180815/59004.html (accessed on 21 December 2018).
- Shanghai Municipal People’s Government. Recent Key Implementation Programs for Deepening the Reform of Medical and Health System in Shanghai. Available online: http://www.shanghai.gov.cn/nw2/nw2314/nw2319/nw2404/nw26256/nw26257/u26aw27894.html (accessed on 21 December 2018).
- Shanghai Municipal People’s Government. Opinions on Implementing the Opinions of the CPC Central Committee and the State Council on Deepening the Reform of the Medical and Health System. Available online: http://sh.eastday.com/qtmt/20110316/u1a864678.html (accessed on 19 December 2018).
- People’s Government of Qingpu District. Qingpu Yearbook 2001. Available online: http://qpsz.shqp.gov.cn/djs/qpnj-2001/index.html (accessed on 21 December 2018).
- People’s Government of Qingpu District. Qingpu Yearbook 2011. Available online: http://www.shqp.gov.cn/stat/dspkjwwtysy2011/20180807/238627.html (accessed on 20 December 2018).
- Statistics Bureau of Qingpu District. Statistical Bulletin on National Economic and Social Development of Qingpu District 2017. Available online: Available online: http://www.shqp.gov.cn/stat/tjgb/20180807/241311.html (accessed on 20 December 2018).
- Highway Bureau Ministry of Transport of The People’s Republic of China. Technical Standard of Highway Engineering (JTG B01-2014); People’s Communications Press: Beijing, China, 2014; p. 120.
- Shanghai Institute of Urban and Rural Construction and Transportation Development Research, Shanghai Urban Transport Development Report 2015. Available online: https://wenku.baidu.com/view/1de8b727b8f67c1cfad6b8d6.html (accessed on 20 December 2018).
- Radke, J.; Mu, L. Spatial Decompositions, Modeling and Mapping Service Regions to Predict Access to Social Programs. Geogr. Inf. Sci. 2000, 6, 105–112. [Google Scholar] [CrossRef]
- Luo, W.; Wang, F. Measures of Spatial Accessibility to Health Care in a GIS Environment: Synthesis and a Case Study in the Chicago Region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Flynn, T.N.; Louviere, J.J.; Peters, T.J.; Coast, J. Best-worst scaling: What it can do for health care research and how to do it. J. Health Econ. 2007, 26, 171–189. [Google Scholar] [CrossRef] [PubMed]
- Shanghai Municipal Commission of Health AND Family Planning, Directory of Healthcare Service Institutions. Available online: http://www.wsjsw.gov.cn/bmfw/ (accessed on 20 December 2018).
- People’s Government of Qingpu District. Qingpu Regional Health Planning (2014–2020). Available online: http://xxgk.shqp.gov.cn/xxgk/govinfopub/department/showinfo.aspx?infoid=7ad91d31-3f97-4ece-b7fc-c882627eea53&deptcode=004&showflag=1 (accessed on 20 December 2018).
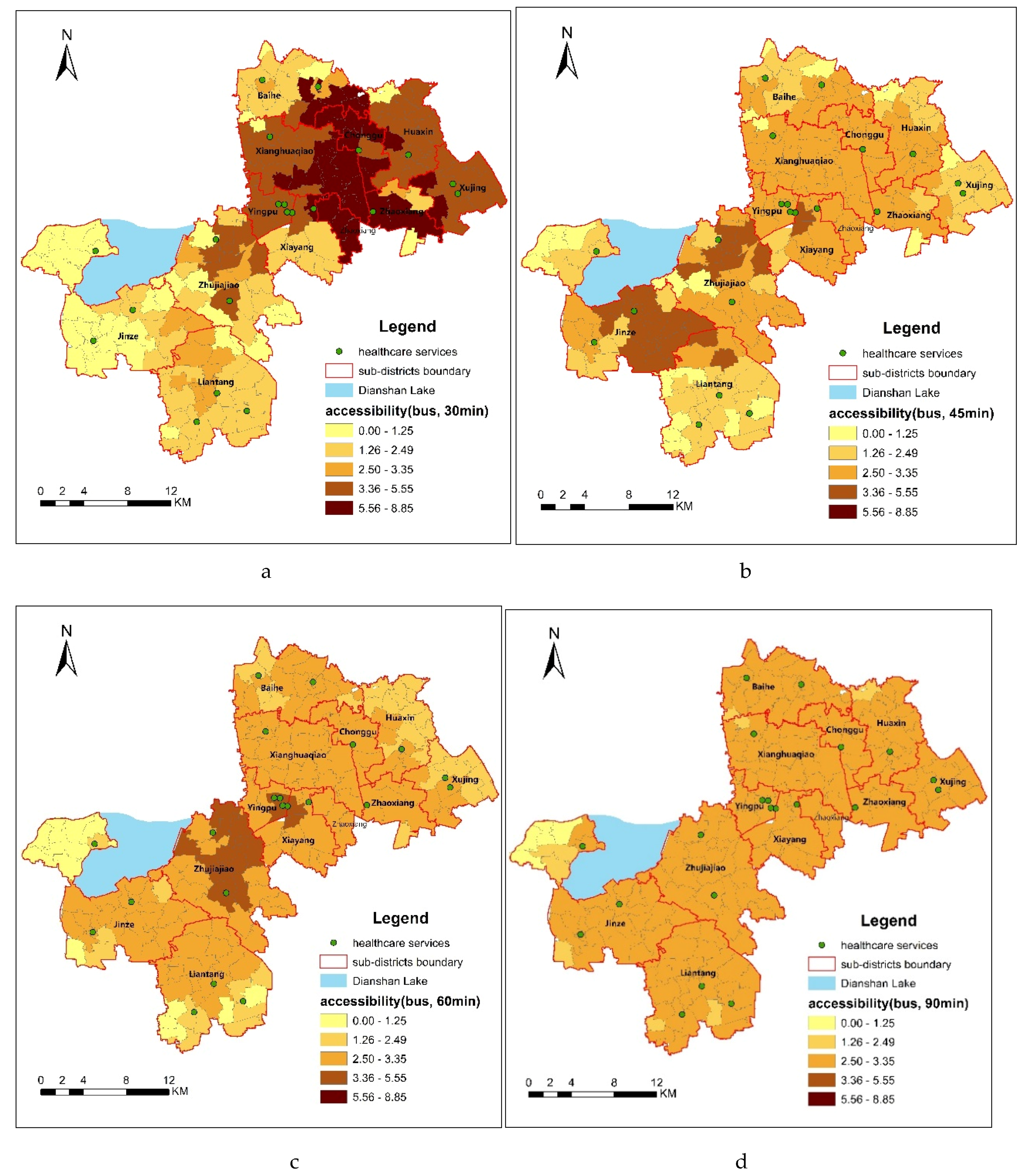
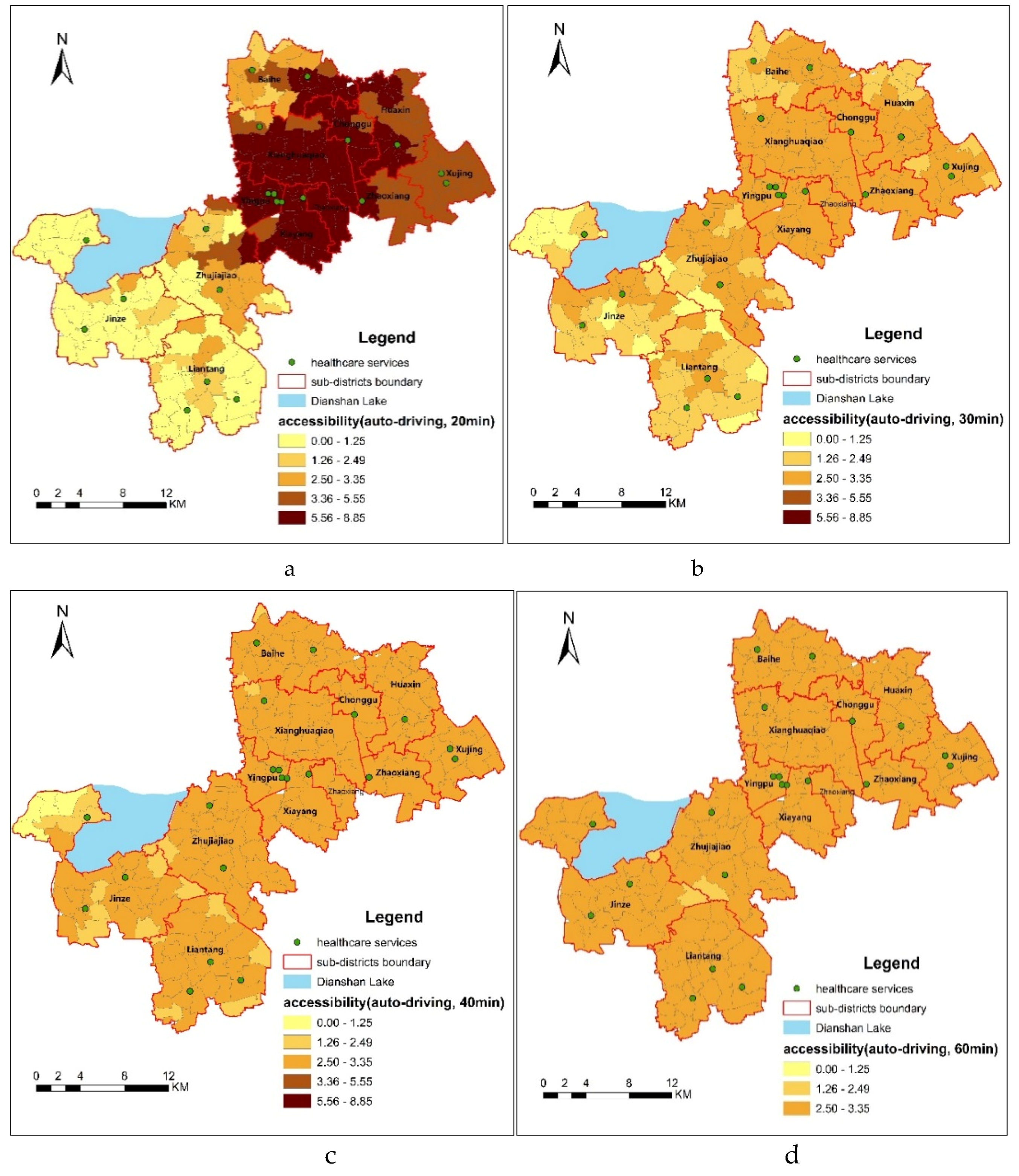
| Transportation Mode | Travel Time | Spatial Accessibility Grade | ||||
|---|---|---|---|---|---|---|
| 0–1.25 | 1.26–2.49 | 2.50–3.35 | 3.36–5.55 | 5.56–8.85 | ||
| Bus | 30 min | 40 | 51 | 25 | 56 | 31 |
| 45 min | 22 | 58 | 99 | 24 | 0 | |
| 60 min | 7 | 47 | 132 | 17 | 0 | |
| 90 min | 4 | 8 | 191 | 0 | 0 | |
| Self-driving | 20 min | 57 | 18 | 22 | 39 | 67 |
| 30 min | 15 | 59 | 129 | 0 | 0 | |
| 40 min | 4 | 21 | 178 | 0 | 0 | |
| 60 min | 0 | 2 | 201 | 0 | 0 | |
| Transportation Mode | Threshold | Minimum Value | Maximum Value | Standard Deviation | Average Value | Weighted Average | Weighted Average |
|---|---|---|---|---|---|---|---|
| Bus | 30 min | 0.00 | 8.86 | 2.21 | 3.36 | 2.84 | 2.84 |
| 45 min | 0.00 | 5.40 | 0.98 | 2.51 | |||
| 60 min | 0.59 | 3.65 | 0.58 | 2.65 | |||
| 90 min | 2.33 | 2.94 | 0.15 | 2.85 | |||
| Self-driving | 20 min | 0.00 | 7.30 | 2.24 | 3.52 | 2.85 | |
| 30 min | 0.00 | 3.34 | 0.74 | 2.51 | |||
| 40 min | 0.80 | 2.79 | 0.28 | 2.67 | |||
| 60 min | 2.48 | 2.70 | 0.00 | 2.70 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gu, X.; Zhang, L.; Tao, S.; Xie, B. Spatial Accessibility to Healthcare Services in Metropolitan Suburbs: The Case of Qingpu, Shanghai. Int. J. Environ. Res. Public Health 2019, 16, 225. https://doi.org/10.3390/ijerph16020225
Gu X, Zhang L, Tao S, Xie B. Spatial Accessibility to Healthcare Services in Metropolitan Suburbs: The Case of Qingpu, Shanghai. International Journal of Environmental Research and Public Health. 2019; 16(2):225. https://doi.org/10.3390/ijerph16020225
Chicago/Turabian StyleGu, Xiaokun, Lufa Zhang, Siyuan Tao, and Boming Xie. 2019. "Spatial Accessibility to Healthcare Services in Metropolitan Suburbs: The Case of Qingpu, Shanghai" International Journal of Environmental Research and Public Health 16, no. 2: 225. https://doi.org/10.3390/ijerph16020225
APA StyleGu, X., Zhang, L., Tao, S., & Xie, B. (2019). Spatial Accessibility to Healthcare Services in Metropolitan Suburbs: The Case of Qingpu, Shanghai. International Journal of Environmental Research and Public Health, 16(2), 225. https://doi.org/10.3390/ijerph16020225





