Determinants and Sources of Iron Intakes of Australian Toddlers: Findings from the SMILE Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Recruitment
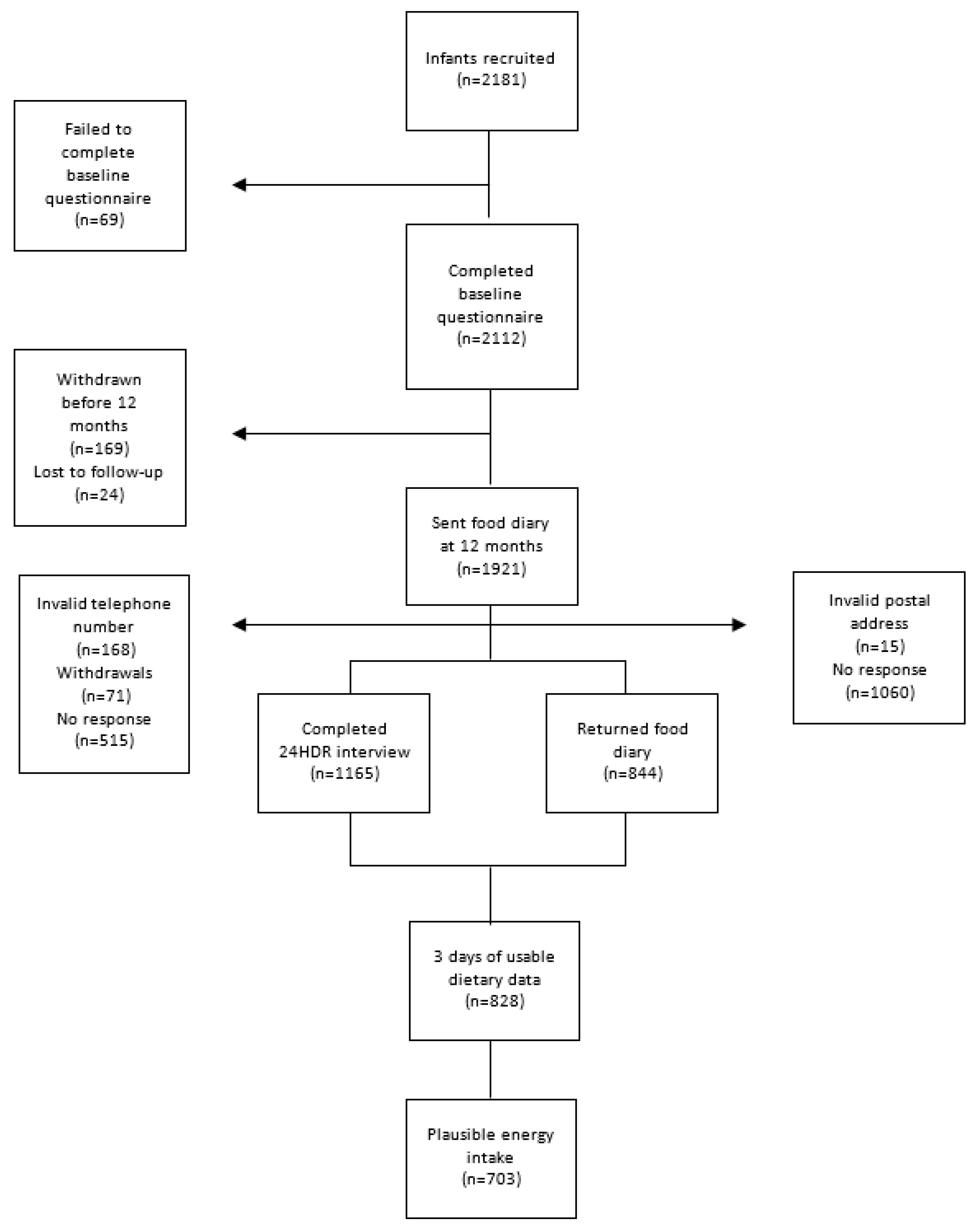
2.2. Collection and Handling of Dietary Data
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Iron Intake
3.3. Sources of Iron Intake
3.4. Determinants of Iron Intake
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| CI | Confidence interval |
| EAR | Estimated average requirement |
| FITS | Feeding Infants and Toddlers Study |
| GLM | General linear model |
| ID | Iron deficiency |
| IDA | Iron deficiency anemia |
| IFG | Infant Feeding Guidelines |
| IRSAD | Index of Relative Socio-Economic Advantage and Disadvantage |
| MSM | Multiple source method |
| NRV | Nutrient reference value |
| RDI | Recommended dietary intake |
| SD | Standard deviation |
| SE | Standard error |
| SMILE | Study of Mothers’ and Infants’ Life Events affecting oral health |
Appendix A
References
- Martorell, R. Improved nutrition in the first 1000 days and adult human capital and health. Am. J. Hum. Biol. 2017, 29, e22952. [Google Scholar] [CrossRef] [PubMed]
- Schwarzenberg, S.J.; Georgieff, M.K.; Committee on Nutrition. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics 2018, 141. [Google Scholar] [CrossRef]
- Burke, R.M.; Leon, J.S.; Suchdev, P.S. Identification, prevention and treatment of iron deficiency during the first 1000 days. Nutrients 2014, 6, 4093–4114. [Google Scholar] [CrossRef]
- Cerami, C. Iron nutriture of the fetus, neonate, infant, and child. Ann. Nutr. Metab. 2017, 71 (Suppl. 3), 8–14. [Google Scholar] [CrossRef] [PubMed]
- Eussen, S.; Alles, M.; Uijterschout, L.; Brus, F.; van der Horst-Graat, J. Iron intake and status of children aged 6–36 months in Europe: A systematic review. Ann. Nutr. Metab. 2015, 66, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, E.E. Consumption of cow’s milk as a cause of iron deficiency in infants and toddlers. Nutr. Rev. 2011, 69 (Suppl. 1), S37–S42. [Google Scholar] [CrossRef] [PubMed]
- Paoletti, G.; Bogen, D.L.; Ritchey, A.K. Severe iron-deficiency anemia still an issue in toddlers. Clin. Pediatr. 2014, 53, 1352–1358. [Google Scholar] [CrossRef] [PubMed]
- Commonwealth Scientific Industrial Research Organisation (CSIRO) Preventative Health National Research Flagship; The University of South Australia. 2007 Australian National Children’s Nutrition and Physical Activity Survey: Main Findings; Commonwealth of Australia: Canberra, Australia, 2008.
- Australian Bureau of Statistics. 4364.0.55.007—Australian Health Survey: Nutrition First Results—Foods and Nutrients, 2011-12. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4364.0.55.007Main+Features12011-12?OpenDocument (accessed on 23 March 2015).
- Conn, J.A.; Davies, M.J.; Walker, R.B.; Moore, V.M. Food and nutrient intakes of 9-month-old infants in Adelaide, Australia. Public Health Nutr. 2009, 12, 2448–2456. [Google Scholar] [CrossRef]
- Byrne, R.; Magarey, A.; Daniels, L. Food and beverage intake in Australian children aged 12–16 months participating in the NOURISH and SAIDI studies. Aust. N. Z. J. Public Health 2014, 38, 326–331. [Google Scholar] [CrossRef]
- Webb, K.; Rutishauser, I.; Knezevic, N. Foods, nutrients and portions consumed by a sample of Australian children aged 16–24months. Nutr. Diet. 2008, 65, 56–65. [Google Scholar] [CrossRef]
- Scott, J.; Davey, K.; Ahwong, E.; Devenish, G.; Ha, D.; Do, L. A comparison by milk feeding method of the nutrient intake of a cohort of Australian toddlers. Nutrients 2016, 8, 501. [Google Scholar] [CrossRef] [PubMed]
- Atkins, L.A.; McNaughton, S.A.; Campbell, K.J.; Szymlek-Gay, E.A. Iron intakes of Australian infants and toddlers: Findings from the Melbourne Infant Feeding, Activity and Nutrition Trial (InFANT) Program. Br. J. Nutr. 2016, 115, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Finn, K.; Callen, C.; Bhatia, J.; Reidy, K.; Bechard, L.J.; Carvalho, R. Importance of dietary sources of iron in infants and toddlers: Lessons from the FITS study. Nutrients 2017, 9, 733. [Google Scholar] [CrossRef] [PubMed]
- Lennox, A.; Sommerville, J.; Ong, K.K.; Henderson, H.; Allen, R. Diet and Nutrition Survey of Infants and Young Children. 2011. Available online: http://webarchive.nationalarchives.gov.uk/20130402145952/http://transparency.dh.gov.uk/2013/03/13/dnsiyc-2011/ (accessed on 23 July 2018).
- McCarthy, E.K.; Ni Chaoimh, C.; Hourihane, J.O.; Kenny, L.C.; Irvine, A.D.; Murray, D.M.; Kiely, M. Iron intakes and status of 2-year-old children in the Cork BASELINE Birth Cohort Study. Matern. Child Nutr. 2017, 13, e12320. [Google Scholar] [CrossRef] [PubMed]
- Do, L.; Scott, J.; Thomson, W.; Stamm, J.; Rugg-Gunn, A.; Levy, S.; Wong, C.; Devenish, G.; Ha, D.; Spencer, A. Common risk factor approach to address socioeconomic inequality in the oral health of preschool children—A prospective cohort study. BMC Public Health 2014, 14, 429. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 4363.0.55.001—Australian Health Survey: Users’ Guide, 2011-13. 24-Hour Dietary Recall. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/0D6B1FE95EAB8FF3CA257CD2001CA113?opendocument (accessed on 18 March 2016).
- Food Standards Australia and New Zealand. AUSNUT 2011–2013. Australian Food, Supplement and Nutrient Database. Available online: http://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/pages/default.aspx (accessed on 5 November 2018).
- Kent, J.C.; Mitoulas, L.; Cox, D.B.; Owens, R.A.; Hartmann, P.E. Breast volume and milk production during extended lactation in women. Exp. Physiol. 1999, 84, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Harttig, U.; Haubrock, J.; Knuppel, S.; Boeing, H.; Consortium, E. The MSM program: Web-based statistics package for estimating usual dietary intake using the Multiple Source Method. Eur. J. Clin. Nutr. 2011, 65 (Suppl. 1), S87–S91. [Google Scholar] [CrossRef]
- Haubrock, J.; Nothlings, U.; Volatier, J.L.; Dekkers, A.; Ocke, M.; Harttig, U.; Illner, A.K.; Knuppel, S.; Andersen, L.F.; Boeing, H.; et al. Estimating usual food intake distributions by using the multiple source method in the EPIC-Potsdam Calibration Study. J. Nutr. 2011, 141, 914–920. [Google Scholar] [CrossRef]
- Souverein, O.W.; Dekkers, A.L.; Geelen, A.; Haubrock, J.; de Vries, J.H.; Ocke, M.C.; Harttig, U.; Boeing, H.; van ‘t Veer, P.; EFCOVAL Consortium. Comparing four methods to estimate usual intake distributions. Eur. J. Clin. Nutr. 2011, 65 (Suppl. 1), S92–S101. [Google Scholar] [CrossRef]
- National Health and Medical Research Council and Ministry of Health. Nutrient Reference Values for Australia and New Zealand; NHMRC: Canberra, Australia, 2005.
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas. Available online: http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa (accessed on 15 January 2017).
- Magarey, A.; Watson, J.; Golley, R.K.; Burrows, T.; Sutherland, R.; McNaughton, S.A.; Denney-Wilson, E.; Campbell, K.; Collins, C. Assessing dietary intake in children and adolescents: Considerations and recommendations for obesity research. Int. J. Pediatr. Obes. 2011, 6, 2–11. [Google Scholar] [CrossRef]
- World Health Organization/UNICEF. Global Strategy for Infant and Young Child Feeding; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Solomons, N.W.; Vossenaar, M. Nutrient density in complementary feeding of infants and toddlers. Eur. J. Clin. Nutr. 2013, 67, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Catellier, D.J.; Jun, S.; Dwyer, J.T.; Jacquier, E.F.; Anater, A.S.; Eldridge, A.L. Total usual nutrient intakes of US children (under 48 months): Findings from the Feeding Infants and Toddlers Study (FITS) 2016. J. Nutr. 2018, 148, 1557S–1566S. [Google Scholar] [CrossRef] [PubMed]
- Panel on Micronutrients Food and Nutrition Board Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; National Academy of Sciences: Washington, DC, USA, 2001. [Google Scholar]
- Committee on Medical Aspects of Food Policy. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom; Department of Health: London, UK, 1991.
- Food Standards Australia and New Zealand. Standard 2.9.1—Infant Formula Products. Available online: https://www.legislation.gov.au/Details/F2017C00332 (accessed on 25 October 2018).
- Fox, M.K.; Pac, S.; Devaney, B.; Jankowski, L. Feeding infants and toddlers study: What foods are infants and toddlers eating? J. Am. Diet. Assoc. 2004, 104, 22–30. [Google Scholar] [CrossRef]
- Grimes, C.A.; Szymlek-Gay, E.A.; Campbell, K.J.; Nicklas, T.A. Food sources of total energy and nutrients among U.S. infants and toddlers: National Health and Nutrition Examination Survey 2005–2012. Nutrients 2015, 7, 6797–6836. [Google Scholar] [CrossRef] [PubMed]
- Berry, N.J.; Jones, S.C.; Iverson, D. Toddler milk advertising in Australia: Infant formula advertising in disguise? Australas. Mark. J. (AMJ) 2012, 20, 24–27. [Google Scholar] [CrossRef]
- Baker, P.; Smith, J.; Salmon, L.; Friel, S.; Kent, G.; Iellamo, A.; Dadhich, J.P.; Renfrew, M.J. Global trends and patterns of commercial milk-based formula sales: Is an unprecedented infant and young child feeding transition underway? Public Health Nutr. 2016, 19, 2540–2550. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Infant Feeding Guidelines; National Health and Medical Research Council: Canberra, Australia, 2012. [Google Scholar]
- Szymlek-Gay, E.A.; Ferguson, E.L.; Heath, A.-L.M.; Fleming, E.A. Quantities of foods consumed by 12- to 24-month-old New Zealand children. Nutr. Diet. 2010, 67, 244–250. [Google Scholar] [CrossRef]
- Abbaspour, N.; Hurrell, R.; Kelishadi, R. Review on iron and its importance for human health. J. Res. Med. Sci. 2014, 19, 164–174. [Google Scholar]
- Koh, G.A.; Scott, J.A.; Oddy, W.H.; Graham, K.I.; Binns, C.W. Exposure to non-core foods and beverages in the first year of life: Results from a cohort study. Nutr. Diet. 2010, 67, 137–142. [Google Scholar] [CrossRef]
- North, K.; Emmett, P. Multivariate analysis of diet among three-year-old children and associations with socio-demographic characteristics. The Avon Longitudinal Study of Pregnancy and Childhood (ALSPAC) Study Team. Eur. J. Clin. Nutr. 2000, 54, 73–80. [Google Scholar] [CrossRef]
- Victora, C.G.; Bahl, R.; Barros, A.J.D.; França, G.V.A.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 96–113. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, J.T. The Feeding Infants and Toddlers Study (FITS) 2016: Moving forward. J. Nutr. 2018, 148, 1575S–1580S. [Google Scholar] [CrossRef] [PubMed]
- Beaton, E.; Wright, J.; Devenish, G.; Do, L.; Scott, J. Relative validity of a 24-h Recall in assessing intake of key nutrients in a cohort of Australian toddlers. Nutrients 2018, 10, 80. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n | % |
|---|---|---|
| Maternal characteristics | ||
| Maternal age at recruitment (years) | ||
| <25 | 73 | 8.8 |
| 25–34 | 574 | 69.3 |
| ≥35 | 179 | 21.6 |
| Not reported | 2 | 0.2 |
| Maternal education completed | ||
| High school/vocational | 356 | 43.0 |
| Some university and above | 468 | 56.5 |
| Not reported | 4 | 0.5 |
| IRSAD score (a) | ||
| Deciles 1–2 | 120 | 14.5 |
| Deciles 3–4 | 173 | 20.9 |
| Deciles 5–6 | 174 | 21.0 |
| Deciles 7–8 | 160 | 19.3 |
| Deciles 9–10 | 195 | 23.6 |
| Not reported | 6 | 0.7 |
| Maternal country of birth | ||
| Australia and New Zealand | 610 | 73.7 |
| India | 50 | 6.0 |
| UK | 31 | 3.7 |
| China | 37 | 4.5 |
| Asia-Other | 52 | 6.3 |
| All other countries | 43 | 5.2 |
| Not reported | 5 | 0.6 |
| Maternal BMI (b) (kg/m2) | ||
| <25 | 477 | 57.6 |
| 25–29.99 | 167 | 20.2 |
| ≥30 | 140 | 16.9 |
| Not reported | 44 | 5.3 |
| Parity | ||
| Primiparous | 389 | 47.0 |
| Multiparous | 412 | 49.8 |
| Not reported | 27 | 3.3 |
| Child characteristics | ||
| Child sex | ||
| Male | 452 | 54.6 |
| Female | 376 | 45.4 |
| Not reported | 0 | 0 |
| Primary milk feeding method at 12 months | ||
| Breast milk | 218 | 26.3 |
| Mixed-breast milk and formula | 68 | 8.2 |
| Formula | 309 | 37.3 |
| Neither breast milk nor formula | 226 | 27.5 |
| Not reported | 7 | 0.8 |
| Food Group | All Participants | Consumers Only | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) (mg/day) | Median (mg/day) | 25% | 75% | % Iron Intake | % Total group | Mean (SD) (mg/day) | Median (mg/day) | 25% | 75% | % RDI | ||
| Total | 6.96 (3.32) | 6.40 | 4.45 | 8.89 | - | - | - | - | - | - | - | |
| Breast milk | 0.03 (0.06) | 0.00 | 0.00 | 0.06 | 0.5 | 34.6 | 0.10 (0.06) | 0.09 | 0.06 | 0.13 | 1.1 | |
| Infant/toddler formula | 2.03 (2.81) | 0.00 | 0.00 | 4.13 | 29.6 | 46.0 | 4.43 (2.56) | 4.28 | 2.49 | 6.01 | 49.3 | |
| Infant/toddler commercial products | 1.12 (2.48) | 0.18 | 0.02 | 0.92 | 16.3 | 78.0 | 1.44 (2.73) | 0.43 | 0.09 | 1.28 | 16.0 | |
| Infant/toddler cereals | 0.78 (2.37) | 0.00 | 0.00 | 0.00 | 11.3 | 23.1 | 3.38 (3.95) | 2.11 | 0.46 | 4.77 | 37.6 | |
| Infant/toddler snack food (a) | 0.21 (0.47) | 0.05 | 0.00 | 0.17 | 3.1 | 70.0 | 0.31 (0.54) | 0.10 | 0.05 | 0.28 | 3.4 | |
| Infant/toddler savory dishes | 0.12 (0.26) | 0.00 | 0.00 | 0.14 | 1.8 | 28.1 | 0.44 (0.33) | 0.35 | 0.21 | 0.58 | 4.9 | |
| Cereals and cereal products | 1.75 (1.44) | 1.45 | 0.60 | 2.57 | 25.4 | 98.1 | 1.79 (1.43) | 1.50 | 0.67 | 2.59 | 19.9 | |
| Flours, grains | 0.07 (0.19) | 0.00 | 0.00 | 0.03 | 1.1 | 48.2 | 0.15 (0.25) | 0.03 | 0.01 | 0.18 | 1.7 | |
| Regular bread, bread rolls | 0.38 (0.40) | 0.27 | 0.06 | 0.58 | 5.6 | 79.7 | 0.48 (0.39) | 0.39 | 0.18 | 0.66 | 5.3 | |
| English muffins, flat breads, savory or sweet breads | 0.08 (0.21) | 0.00 | 0.00 | 0.03 | 1.2 | 26.4 | 0.31 (0.31) | 0.22 | 0.12 | 0.43 | 3.4 | |
| Pasta (without sauce) | 0.07 (0.14) | 0.00 | 0.00 | 0.08 | 1.0 | 40.1 | 0.17 (0.17) | 0.12 | 0.06 | 0.23 | 1.9 | |
| Breakfast cereals–ready-to-eat | 1.09 (1.35) | 0.75 | 0.00 | 1.79 | 15.9 | 59.9 | 1.83 (1.31) | 1.59 | 0.79 | 2.38 | 20.4 | |
| Breakfast cereals-porridge style | 0.05 (0.17) | 0.00 | 0.00 | 0.00 | 0.7 | 15.7 | 0.32 (0.33) | 0.26 | 0.10 | 0.41 | 3.6 | |
| Other cereal-based products and dishes (b) | 0.26 (0.34) | 0.14 | 0.03 | 0.36 | 3.8 | 81.6 | 0.32 (0.35) | 0.20 | 0.09 | 0.44 | 3.6 | |
| Meat | 0.40 (0.44) | 0.28 | 0.06 | 0.59 | 5.8 | 82.6 | 0.49 (0.44) | 0.37 | 0.18 | 0.67 | 5.4 | |
| Red meat (c) | 0.21 (0.34) | 0.02 | 0.00 | 0.31 | 3.1 | 51.5 | 0.41 (0.38) | 0.31 | 0.15 | 0.56 | 4.6 | |
| Poultry (d) | 0.09 (0.15) | 0.03 | 0.00 | 0.12 | 1.3 | 56.5 | 0.16 (0.18) | 0.10 | 0.05 | 0.22 | 1.8 | |
| Fish and seafood (e) | 0.08 (0.20) | 0.00 | 0.00 | 0.07 | 1.2 | 32.8 | 0.26 (0.28) | 0.16 | 0.07 | 0.33 | 2.9 | |
| Processed meats (f) | 0.10 (0.22) | 0.00 | 0.00 | 0.08 | 1.4 | 39.4 | 0.25 (0.28) | 0.17 | 0.05 | 0.37 | 2.8 | |
| Dairy | 0.12 (0.14) | 0.09 | 0.03 | 0.17 | 1.8 | 91.9 | 0.13 (0.15) | 0.10 | 0.04 | 0.18 | 1.5 | |
| Cow’s milk | 0.07 (0.08) | 0.03 | 0.00 | 0.11 | 1.0 | 77.4 | 0.09 (0.08) | 0.06 | 0.02 | 0.13 | 1.0 | |
| Yoghurt | 0.02 (0.05) | 0.00 | 0.00 | 0.03 | 0.4 | 45.2 | 0.05 (0.06) | 0.04 | 0.02 | 0.07 | 0.6 | |
| Other dairy products (g) | 0.03 (0.10) | 0.01 | 0.00 | 0.03 | 0.4 | 70.9 | 0.04 (0.12) | 0.02 | 0.01 | 0.04 | 0.5 | |
| Dairy and meat substitutes | 0.02 (0.17) | 0.00 | 0.00 | 0.00 | 0.4 | 6.2 | 0.40 (0.58) | 0.14 | 0.06 | 0.55 | 4.4 | |
| Dairy substitutes (h) | 0.02 (0.13) | 0.03 | 0.00 | 0.00 | 0.2 | 4.6 | 0.33 (0.53) | 0.10 | 0.03 | 0.49 | 3.6 | |
| Meat substitutes | 0.01 (0.11) | 0.00 | 0.00 | 0.00 | 0.1 | 1.7 | 0.55 (0.67) | 0.43 | 0.12 | 0.68 | 6.2 | |
| Fruit | 0.33 (0.27) | 0.26 | 0.13 | 0.47 | 4.8 | 95.3 | 0.35 (0.26) | 0.28 | 0.15 | 0.49 | 3.9 | |
| Vegetables | 0.42 (0.39) | 0.33 | 0.15 | 0.59 | 6.2 | 94.3 | 0.45 (0.38) | 0.36 | 0.18 | 0.61 | 5.0 | |
| Legumes and pulses | 0.09 (0.26) | 0.00 | 0.00 | 0.00 | 1.3 | 20.1 | 0.45 (0.43) | 0.31 | 0.15 | 0.61 | 5.0 | |
| Eggs | 0.13 (0.26) | 0.00 | 0.00 | 0.15 | 1.9 | 35.2 | 0.37 (0.32) | 0.27 | 0.13 | 0.52 | 4.1 | |
| Nuts and seeds | 0.02 (0.09) | 0.00 | 0.00 | 0.00 | 0.4 | 24.6 | 0.10 (0.15) | 0.05 | 0.03 | 0.11 | 1.1 | |
| Other (i) | 0.14 (0.24) | 0.06 | 0.01 | 0.18 | 2.0 | 88.7 | 0.16 (0.25) | 0.08 | 0.03 | 0.20 | 1.7 | |
| Variables | % Below EAR (a) | Unadjusted Mean (mg/day) | 95% CI | p | Adjusted Mean (mg/day) | 95% CI | p |
|---|---|---|---|---|---|---|---|
| Total sample | 18.2 | 7.0 | 6.7–7.2 | ||||
| Maternal characteristics | |||||||
| Maternal age at recruitment (years) | 0.689 | ||||||
| <25 | 16.4 | 6.7 | 5.9–7.4 | ||||
| 25–34 | 17.8 | 7.0 | 6.8–7.3 | ||||
| ≥35 | 20.1 | 6.9 | 6.5–7.4 | ||||
| Maternal education-highest level completed | 0.489 | ||||||
| High school/vocational | 16.9 | 7.1 | 6.7–7.4 | ||||
| Some university and above | 19.2 | 6.9 | 6.6–7.2 | ||||
| IRSAD (b) score | 0.924 | ||||||
| Deciles 1–2 | 19.2 | 6.9 | 6.3–7.4 | ||||
| Deciles 3–4 | 19.1 | 6.8 | 6.3–7.3 | ||||
| Deciles 5–6 | 18.4 | 7.0 | 6.5–7.5 | ||||
| Deciles 7–8 | 19.4 | 7.1 | 6.6–7.6 | ||||
| Deciles 9–10 | 15.4 | 7.1 | 6.6–7.5 | ||||
| Maternal country of birth | 0.005 | 0.249 | |||||
| Australia and New Zealand | 17.2 | 6.9 | 6.6–7.1 | 6.4 | 6.1–6.7 | ||
| India | 22.0 | 6.8 | 5.9–7.7 | 6.6 | 5.9–7.4 | ||
| China | 8.1 | 8.2 | 7.1–9.3 | 6.4 | 5.5–7.4 | ||
| UK | 16.1 | 6.7 | 5.6–7.9 | 6.1 | 5.0–7.2 | ||
| Asia Other | 28.8 | 8.4 | 7.5–9.3 | 7.7 | 6.9–8.5 | ||
| Other | 20.9 | 6.5 | 5.6–7.5 | 6.9 | 6.0–7.8 | ||
| Maternal BMI (c) (kg/m2) | 0.765 | ||||||
| <25 | 19.1 | 6.9 | 6.6–7.2 | ||||
| 25–29.99 | 19.8 | 7.0 | 6.4–7.5 | ||||
| ≥30 | 15.0 | 7.1 | 6.6–7.7 | ||||
| Parity | 0.002 | 0.096 | |||||
| Primiparous | 14.7 | 7.4 | 7.0–7.7 | 6.9 | 5.6–7.3 | ||
| Multiparous | 21.1 | 6.6 | 6.3–6.9 | 6.4 | 6.0–6.9 | ||
| Child characteristics | |||||||
| Sex | 0.481 | ||||||
| Male | 17.3 | 7.0 | 6.7–7.4 | ||||
| Female | 19.4 | 6.9 | 6.5–7.2 | ||||
| Primary milk feeding method at 12 months | <0.001 | <0.001 | |||||
| Breast milk | 41.3 | 4.8 | 4.5–5.2 | 4.4 | 4.0–5.0 | ||
| Mixed-breast milk and formula | 11.8 | 8.0 | 7.3–8.7 | 7.5 | 6.7–8.2 | ||
| Formula | 2.3 | 9.2 | 8.9–9.5 | 9.2 | 8.8–9.6 | ||
| Neither breast milk nor formula | 20.1 | 5.6 | 5.3–6.0 | 5.6 | 5.1–6.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scott, J.A.; Gee, G.; Devenish, G.; Ha, D.; Do, L. Determinants and Sources of Iron Intakes of Australian Toddlers: Findings from the SMILE Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 181. https://doi.org/10.3390/ijerph16020181
Scott JA, Gee G, Devenish G, Ha D, Do L. Determinants and Sources of Iron Intakes of Australian Toddlers: Findings from the SMILE Cohort Study. International Journal of Environmental Research and Public Health. 2019; 16(2):181. https://doi.org/10.3390/ijerph16020181
Chicago/Turabian StyleScott, Jane A, Georgina Gee, Gemma Devenish, Diep Ha, and Loc Do. 2019. "Determinants and Sources of Iron Intakes of Australian Toddlers: Findings from the SMILE Cohort Study" International Journal of Environmental Research and Public Health 16, no. 2: 181. https://doi.org/10.3390/ijerph16020181
APA StyleScott, J. A., Gee, G., Devenish, G., Ha, D., & Do, L. (2019). Determinants and Sources of Iron Intakes of Australian Toddlers: Findings from the SMILE Cohort Study. International Journal of Environmental Research and Public Health, 16(2), 181. https://doi.org/10.3390/ijerph16020181






