The Effect of Tai Chi Chuan on Negative Emotions in Non-Clinical Populations: A Meta-Analysis and Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion Criteria and Study Selection
2.3. Methodological Quality Assessment of Included Studies
2.4. Data Extraction and Analysis
3. Results
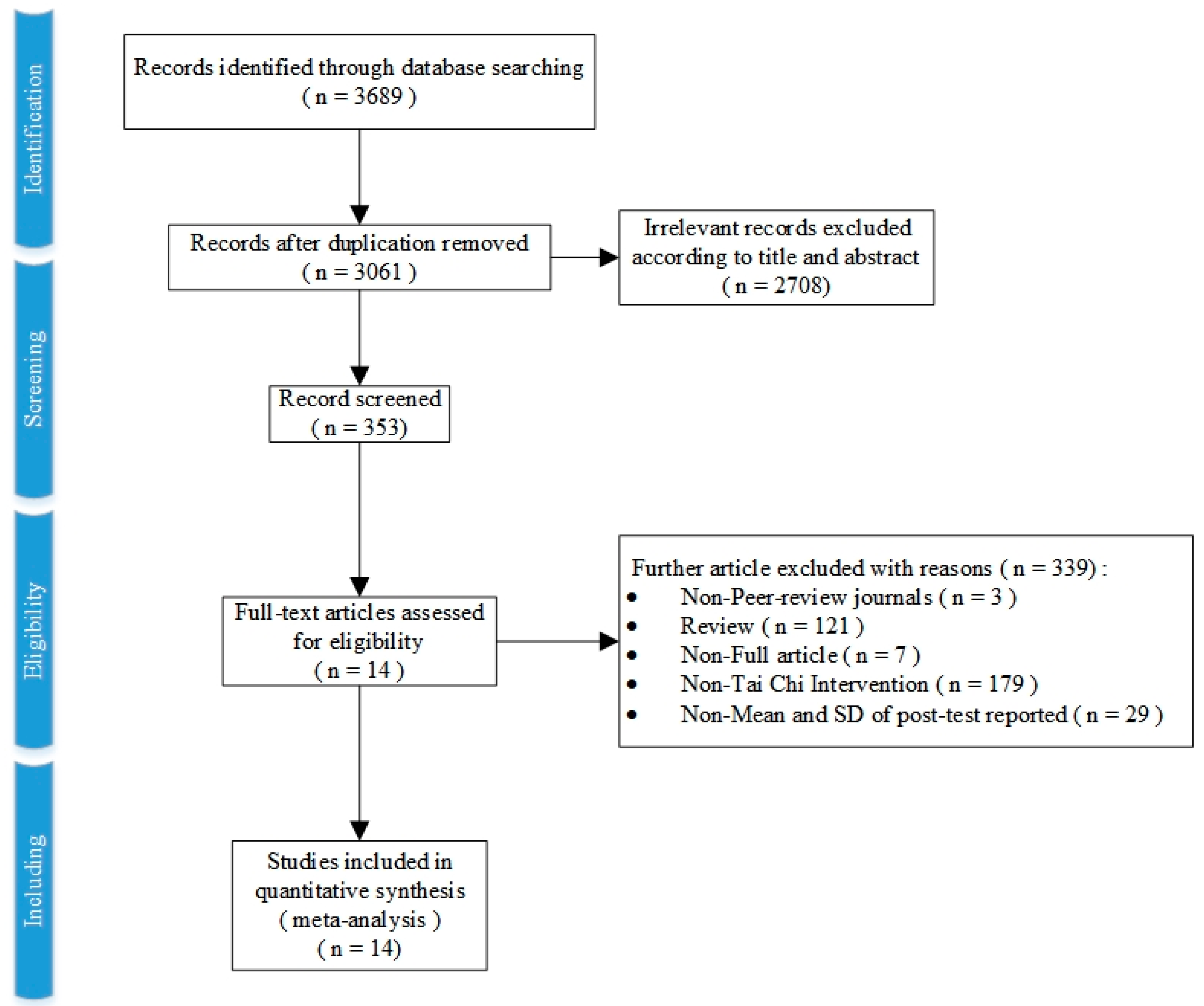
3.1. Study Selection
3.2. Study Characteristics
3.3. Study Quality Assessment
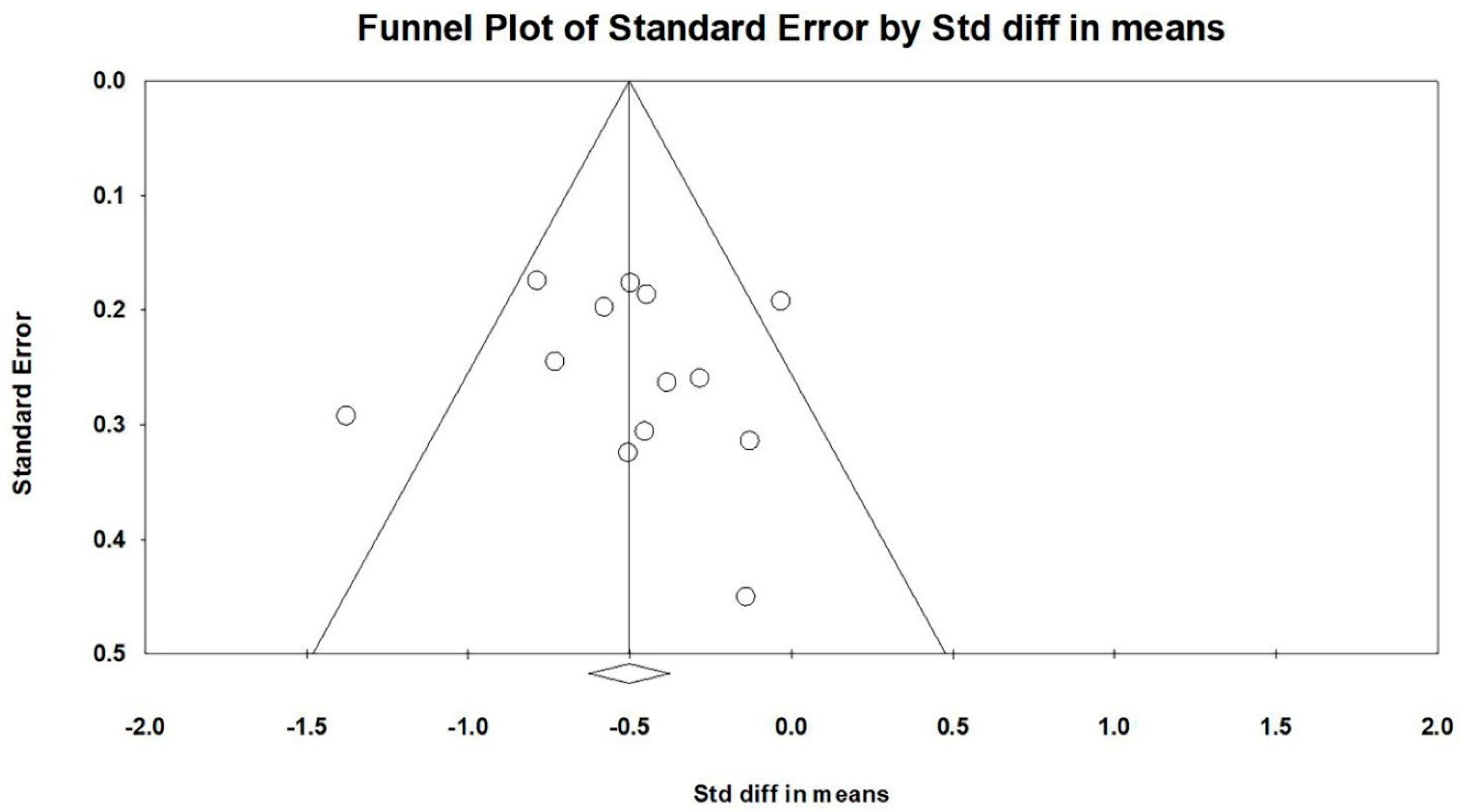
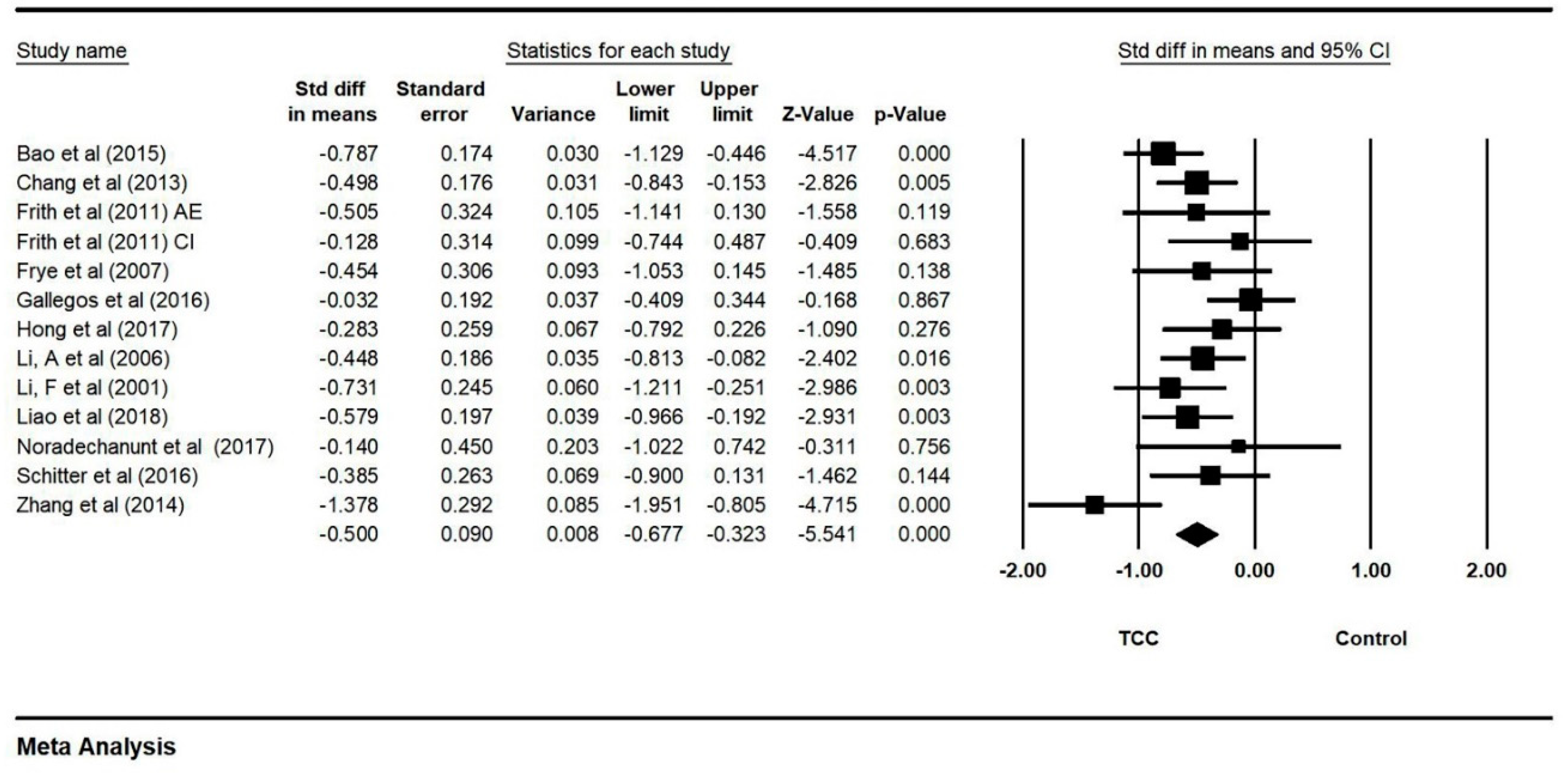
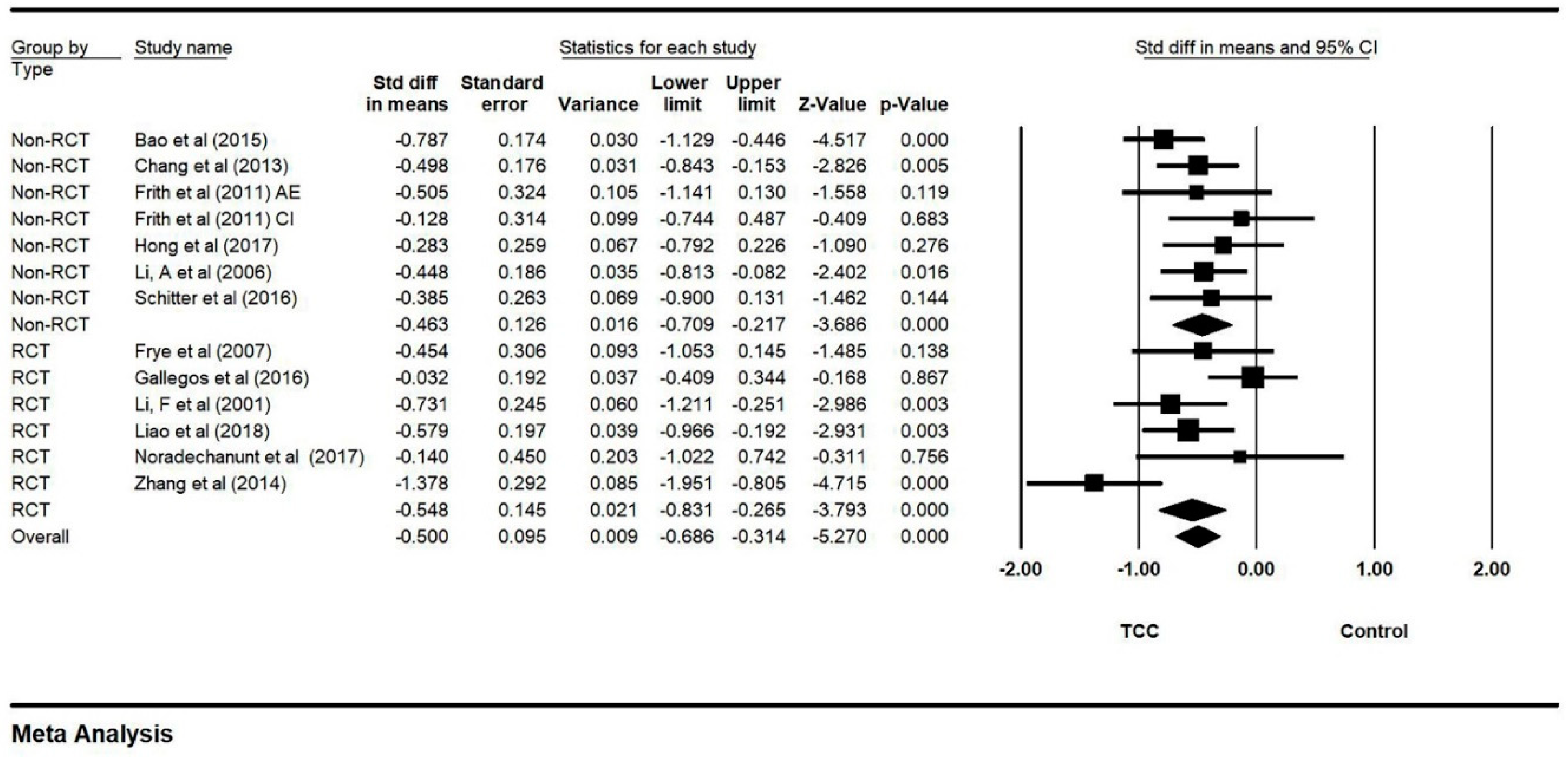
3.4. Effects of TCC Intervention on Negative Emotion
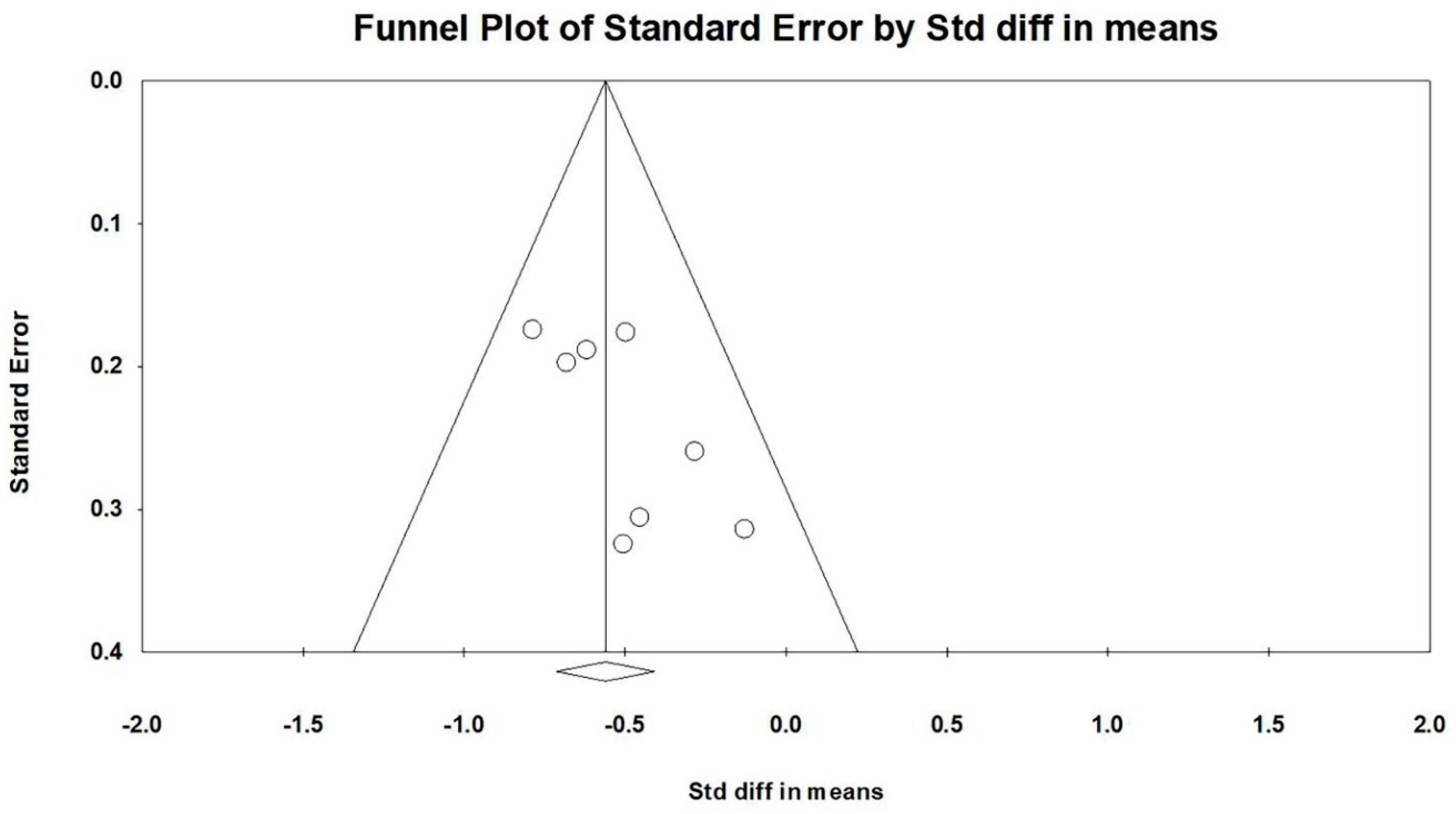
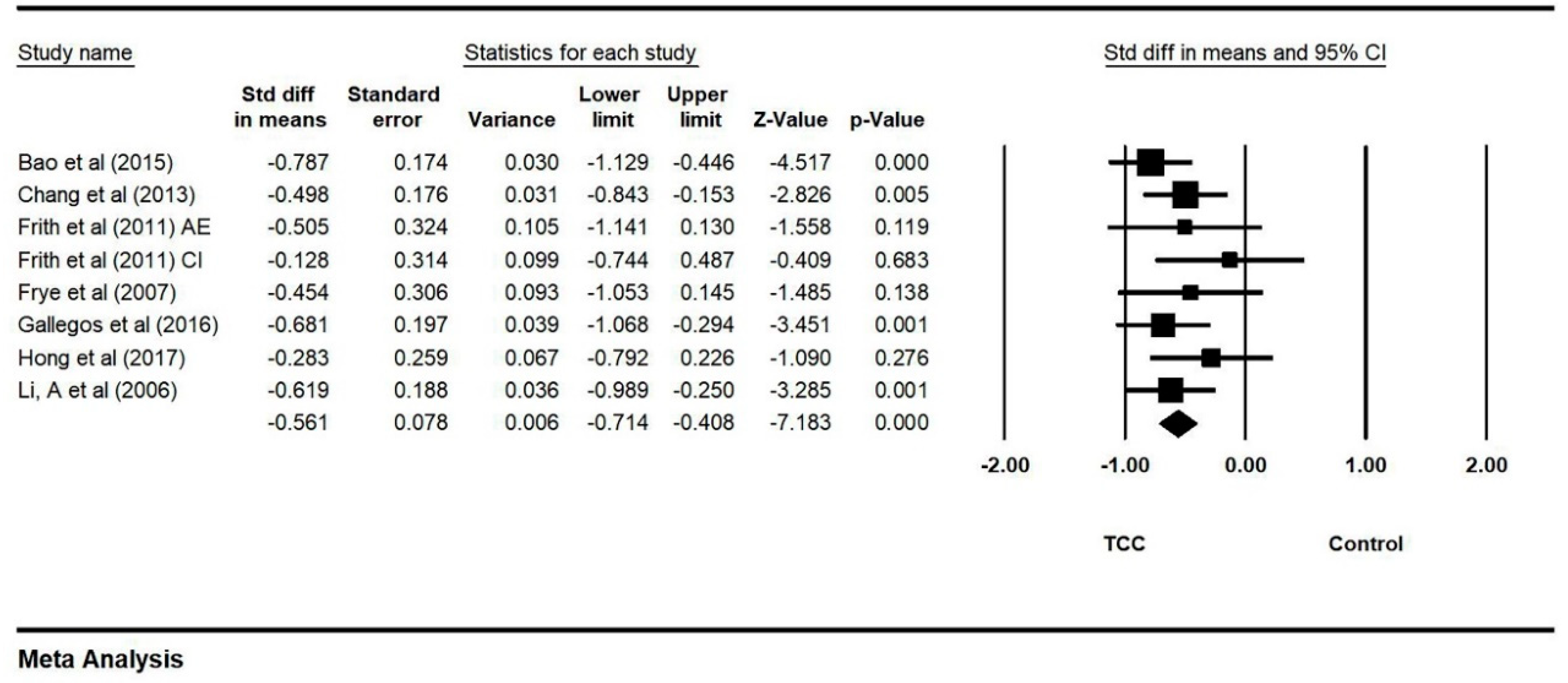
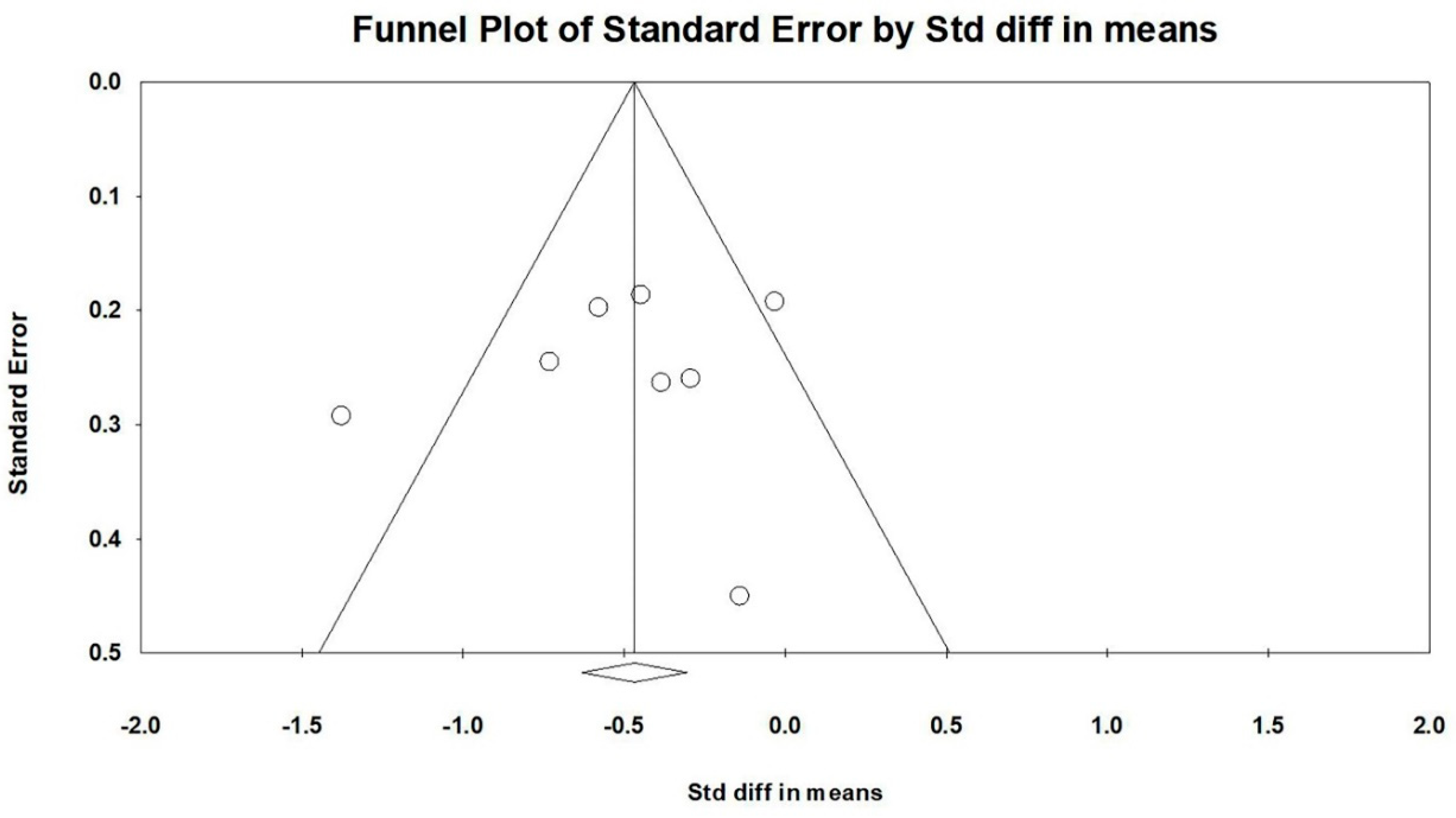
3.5. Effect of TCC Intervention on Anxiety
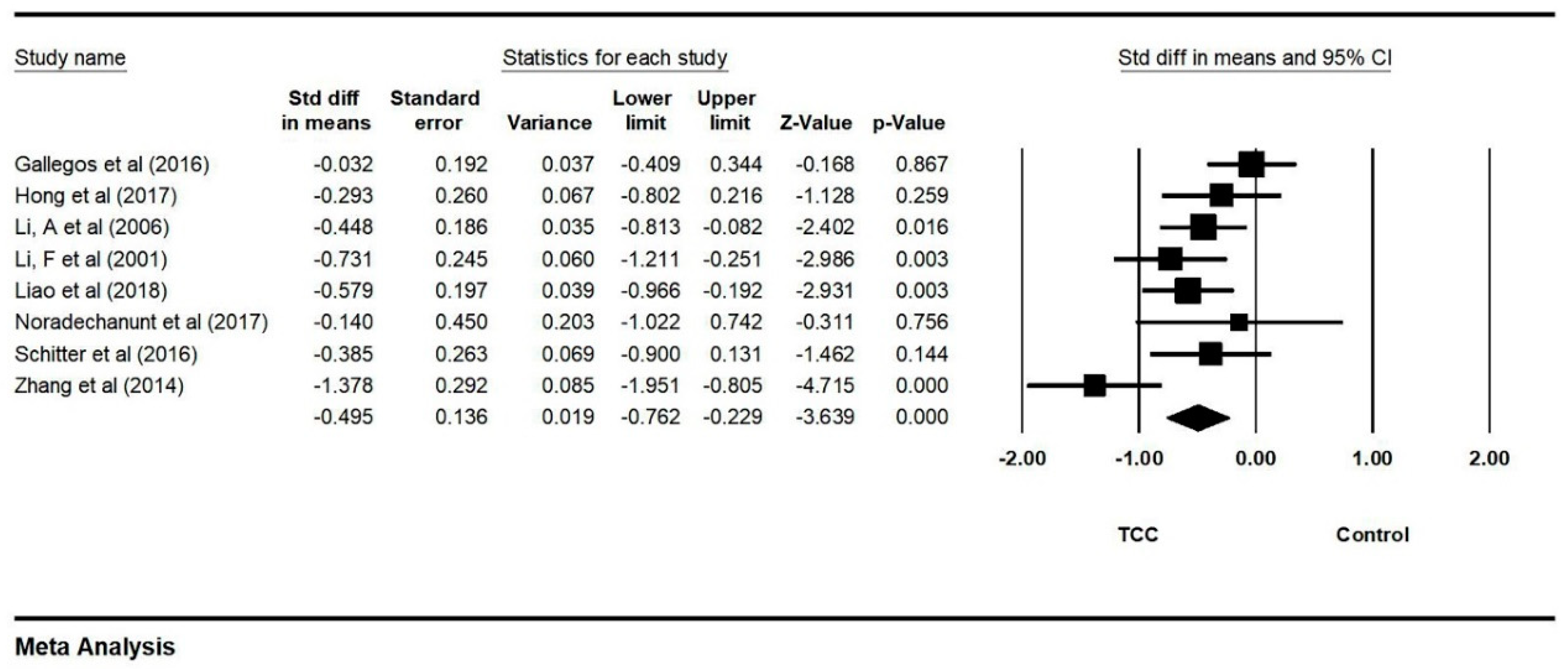
3.6. Effect of TCC Intervention on Depression
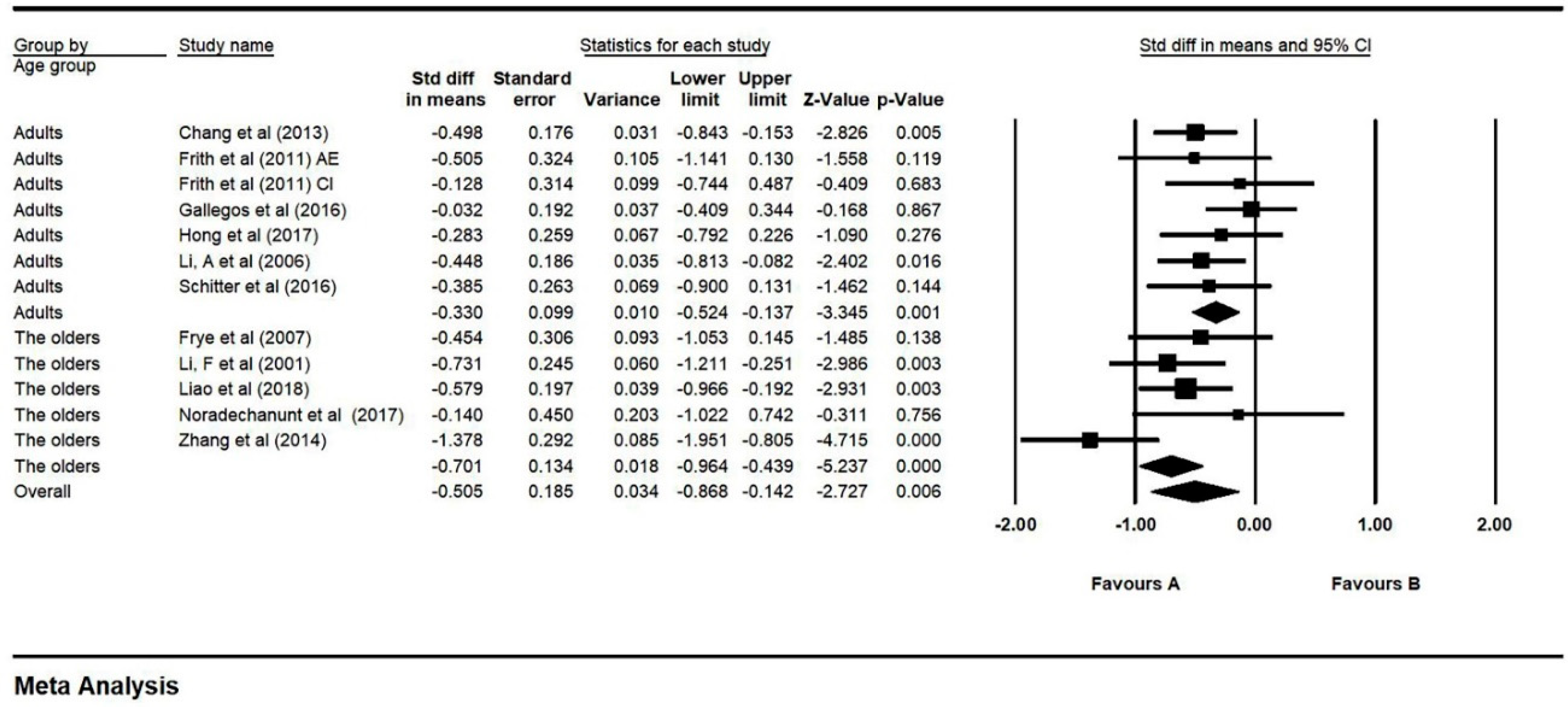
3.7. Moderator Analysis for Age
3.8. Moderator Analysis for Experimental Design
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Organization, W.H. Depression and Other Common Mental Disorders; Global Health Estimates: Geneva, Switzerland, 2017. [Google Scholar]
- Frankish, H.; Boyce, N.; Horton, R. Mental health for all: A global goal. Lancet 2018, 392, 1493–1494. [Google Scholar] [CrossRef]
- Farach, F.J.; Pruitt, L.D.; Jun, J.J.; Jerud, A.B.; Zoellner, L.A.; Roy-Byrne, P.P. Pharmacological treatment of anxiety disorders: Current treatments and future directions. J. Anxiety Disord. 2012, 26, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Rosenblat, J.D.; Simon, G.E.; Sachs, G.S.; Deetz, I.; Doederlein, A.; DePeralta, D.; Dean, M.M.; McIntyre, R.S. Treatment effectiveness and tolerability outcomes that are most important to individuals with bipolar and unipolar depression. J. Affect. Dis. 2019, 243, 116–120. [Google Scholar] [CrossRef]
- WHO. Global Strategy on Diet, Physical Activity and Health; WHO: Geneva, Switzerland; Available online: https://www.who.int/dietphysicalactivity/pa/en/ (accessed on 1 August 2019).
- Sim, M.K. Treatment of disease without the use of drugs I. Research on biofeedback training. Singap. Med. J. 1976, 17, 167. [Google Scholar]
- Li, F.; Duncan, T.E.; Duncan, S.C.; McAuley, E.; Chaumeton, N.R.; Harmer, P. Enhancing the Psychological Well-Being of Elderly Individuals Through Tai Chi Exercise: A Latent Growth Curve Analysis. Struct. Equ. Model. A Multidiscip. J. 2001, 8, 53–83. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J.; Fuller, R.; Holte, A.; Justo, J.; Sanderman, R.; Wichstrom, L. Leisure-time physical exercise: Prevalence, attitudinal correlates, and behavioral correlates among young Europeans from 21 countries. Prev. Med. 1997, 26, 845–854. [Google Scholar] [CrossRef]
- Zou, L.; Yeung, A.; Li, C.; Wei, G.X.; Chen, K.W.; Kinser, P.A.; Chan, J.S.M.; Ren, Z. Effects of Meditative Movements on Major Depressive Disorder: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2018, 7, 195. [Google Scholar] [CrossRef]
- Stonerock, G.L.; Hoffman, B.M.; Smith, P.J.; Blumenthal, J.A. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Ann. Behav. Med. 2015, 49, 542–556. [Google Scholar] [CrossRef]
- Yang, J.; Liu, Z.; Liu, S.; Li, L.; Zheng, L.; Guo, X. The emotional stability of elders with Tai Chi experience in the sequential risk-taking task. Psych J. 2019. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Loprinzi, P.D.; Yeung, A.S.; Zeng, N.; Huang, T. The beneficial effects of mind-body exercises for people with mild cognitive impairment: A systematic review with meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 1556–1573. [Google Scholar] [CrossRef]
- Zou, L.; Han, J.; Li, C.; Yeung, A.S.; Hui, S.S.; Tsang, W.W.N.; Ren, Z.; Wang, L. Effects of Tai Chi on lower limb proprioception in adults aged over 55: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 1102–1113. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, K.; Emery, L.; Harrison, M.; Harrison, M.; Greeson, J. Changes in mindfulness, well-being, and sleep quality in college students through taijiquan courses: A cohort control study. J. Altern. Complement. Med. 2011, 17, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Sasaki, J.E.; Zeng, N.; Wang, C.; Sun, L. A systematic review with meta-analysis of mindful exercises on rehabilitative outcoems among poststroke patients. Arch. Phys. Med. Rehabil. 2018, 99, 2355–2364. [Google Scholar] [CrossRef] [PubMed]
- Orr, R.; Tsang, T.; Lam, P.; Comino, E.; Singh, M.F. Mobility Impairment in Type 2 Diabetes: Association with muscle power and effect of Tai Chi intervention. Diabetes Care 2006, 29, 2120–2122. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M.; Li, T.; Du, G.; Liu, Y. Tai Chi for health benefits in patients with multiple sclerosis: A systematic review. PLoS ONE 2017, 12, e0170212. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.; Chen, S.Y.; Wong, M.K.; Lai, J.S. Tai Chi Chuan exercise for patients with cardiovascular disease. Evidence-Based Complementray and Alternative Medicine. Evid. Based Complement. Altern. Med. 2013, 2013, 983208. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Schmid, C.H.; Fielding, R.A.; Harvey, W.F.; Reid, K.F.; Price, L.L.; Driban, J.B.; Kalish, R.; Rones, R.; McAlindon, T. Effect of Tai Chi versus aerobic exercise for fibromyalgia: Comparative effectiveness randomized controlled trial. BMJ 2018, 360, 851. [Google Scholar] [CrossRef]
- Cheon, S.M.; Chae, B.K.; Sung, H.R.; Lee, G.C.; Kim, J.W. The Efficacy of Exercise Programs for Parkinson’s Disease: Tai Chi versus Combined Exercise. J. Clin. Neurol. 2013, 9, 237–243. [Google Scholar] [CrossRef]
- Hoffmann-Smith, K.A.; Ma, A.; Yeh, C.-T.; DeGuire, N.L.; Smith, J.P. The Effect of Tai Chi in Reducing Anxiety in an Ambulatory Population. J. Complement. Integr. Med. 2009, 6. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Blobaum, P. Physiotherapy Evidence Database (PEDro). J. Med. Libr. Assoc. 2006, 94, 477. [Google Scholar]
- Zheng, S.; Kim, C.; Lal, S.; Meier, P.; Sibbritt, D.; Zaslawski, C. The Effects of Twelve Weeks of Tai Chi Practice on Anxiety in Stressed But Healthy People Compared to Exercise and Wait-List Groups—A Randomized Controlled Trial. J. Clin. Psychol. 2017, 74, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Ni, X.; Chen, P. Study about the effects of different fitness sports on cognitive function and emotion of the aged. Cell Biochem. Biophys. 2014, 70, 1591–1596. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.; Tsai, G.; Hsieh, C.-J. Psychological, immunological and physiological effects of a Laughing Qigong Program (LQP) on adolescents. Complement. Ther. Med. 2013, 21, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Field, T. Exercise research on children and adolescents. Complement. Ther. Clin. Pract. 2012, 18, 54–59. [Google Scholar] [CrossRef]
- Chiang, L.C.; Ma, W.F.; Huang, J.L.; Tseng, L.F.; Hsueh, K.C. Effect of relaxation-breathing training on anxiety and asthma signs/symptoms of children with moderate-to-severe asthma: A randomized controlled trial. Int. J. Nurs. Stud. 2009, 46, 1061–1070. [Google Scholar] [CrossRef]
- Awelewa, O.O.; Caldwell, K.L.; Triplett, N.T.T.; Bergquist, J.J.; Bergman, S.; Collier, S.R. Sex Differences In Autonomic Function Exist Following Tai Chi Chuan Training In Young Adults With High Anxiety. Med. Sci. Sports Exerc. 2015, 47, 752–753. [Google Scholar] [CrossRef]
- Black, D.S.; Irwin, M.R.; Olmstead, R.; Ji, E.; Crabb Breen, E.; Motivala, S.J. Tai Chi Meditation Effects on Nuclear Factor-κB Signaling in Lonely Older Adults: A Randomized Controlled Trial. Psychother. Psychosom. 2014, 83, 315–317. [Google Scholar] [CrossRef]
- Leung, D.P.; Chan, C.K.; Tsang, H.W.; Tsang, W.W.; Jones, A.Y. Tai chi as an intervention to improve balance and reduce falls in older adults: A systematic and meta-analytical review. Altern. Ther. Health Med. 2011, 17, 40–48. [Google Scholar]
- Zou, L.; Yeung, A.; Quan, X.; Hui, S.S.; Hu, X.; Chan, J.S.M.; Wang, C.; Boyden, S.D.; Sun, L.; Wang, H. Mindfulness-Based Baduanjin Exercise for Depression and Anxiety in People with Physical or Mental Illnesses: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2018, 15, 321. [Google Scholar] [CrossRef]
- Tang, Y.-Y.; Jiang, C.; Tang, R. How Mind-Body Practice Works-Integration or Separation? Front. Psychol. 2017, 8, 866. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.W.; Berger, C.C.; Eric, M.; Darlene, F.; Jessica, M.; Laya, D.; Lejuez, C.W. Meditative therapies for reducing anxiety: A systematic review and meta-analysis of randomized controlled trials. Depress. Anxiety 2012, 29, 545–562. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, G.; Rampes, H.; Tuffrey, V.; Richardson, J.; Pilkington, K. Yoga for anxiety: A systematic review of the research evidence. Br. J. Sports Med. 2005, 39, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Singh, S.; Sibinga, E.M.; Gould, N.F.; Rowland-Seymour, A.; Sharma, R.; Berger, Z.; Sleicher, D.; Maron, D.D.; Shihab, H.M. Meditation Programs for Psychological Stress and Well-being: A Systematic Review and Meta-analysis. Deutsche Zeitschrift Fuer Akupunktur 2014, 57, 26–27. [Google Scholar] [CrossRef]
- Cho, H.; Ryu, S.; Noh, J.; Lee, J. The Effectiveness of Daily Mindful Breathing Practices on Test Anxiety of Students. PLoS ONE 2016, 11, e0164822. [Google Scholar] [CrossRef]
- Liu, J.; Xie, H.; Liu, M.; Wang, Z.; Zou, L.; Yeung, A.S.; Hui, S.S.; Yang, Q. The Effects of Tai Chi on Heart Rate Variability in Older Chinese Individuals with Depression. Int. J. Environ. Res. Public Health 2018, 15, 2771. [Google Scholar] [CrossRef]
- Park, Y.J. Effect of Tai Chi Exercise Program on Depression, Self-esteem, and Self-efficacy of Nursing College Students. J. Learn.-Cent. Curric. Instr. 2017, 17, 805–820. [Google Scholar] [CrossRef]
- Wei, G.X.; Li, Y.F.; Yue, X.L.; Ma, X.; Chang, Y.K.; Yi, L.Y.; Li, J.C.; Zuo, X.N. Tai Chi Chuan modulates heart rate variability during abdominal breathing in elderly adults. Psych J. 2016, 5, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Li, W.; Cao, H.; Klupp, N.; Liu, J.; Bensoussan, A.; Kiat, H.; Chang, D. Does Tai Chi improve psychological well-being and quality of life in patients with cardiovascular disease and/or cardiovascular risk factors? A systematic review protocol. BMJ Open 2017, 7, e014507. [Google Scholar] [CrossRef] [PubMed]
- Appelhans, B.M.; Luecken, L.J. Heart rate variability as an index of regulated emotional responding. Rev. Gen. Psychol. 2006, 10, 229–240. [Google Scholar] [CrossRef]
- Visted, E.; Sorensen, L.; Osnes, B.; Svendsen, J.L.; Binder, P.E.; Schanche, E. The Association between Self-Reported Difficulties in Emotion Regulation and Heart Rate Variability: The Salient Role of Not Accepting Negative Emotions. Front. Psychol. 2017, 8, 328. [Google Scholar] [CrossRef] [PubMed]
- Mather, M.; Thayer, J.F. How heart rate variability affects emotion regulation brain networks. Curr. Opin. Behav. Sci. 2018, 19, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Pietrelli, A.; Lopez-Costa, J.; Goñi, R.; Brusco, A.; Basso, N. Aerobic exercise prevents age-dependent cognitive decline and reduces anxiety-related behaviors in middle-aged and old rats. Neuroscience 2011, 202, 252–266. [Google Scholar] [CrossRef] [PubMed]
- Sleiman, S.F.; Henry, J.; Al-Haddad, R.; El Hayek, L.; Abou Haidar, E.; Stringer, T.; Ulja, D.; Karuppagounder, S.S.; Holson, E.B.; Ratan, R.R.; et al. Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body beta-hydroxybutyrate. eLife 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Gallegos, A.M.; Hoerger, M.; Talbot, N.L.; Krasner, M.S.; Knight, J.M.; Moynihan, J.A.; Duberstein, P.R. Toward identifying the effects of the specific components of Mindfulness-Based Stress Reduction on biologic and emotional outcomes among older adults. J. Altern. Complement. Med. 2013, 19, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Dyer, A.H.; Vahdatpour, C.; Sanfeliu, A.; Tropea, D. The role of Insulin-Like Growth Factor 1 (IGF-1) in brain development, maturation and neuroplasticity. Neuroscience 2016, 325, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Janelsins, M.C.; Davis, P.G.; Wideman, L.; Katula, J.A.; Sprod, L.K.; Peppone, L.J.; Palesh, O.G.; Heckler, C.E.; Williams, J.P.; Morrow, G.R.; et al. Effects of Tai Chi Chuan on insulin and cytokine levels in a randomized controlled pilot study on breast cancer survivors. Clin. Breast Cancer 2011, 11, 161–170. [Google Scholar] [CrossRef]
- Cassilhas, R.C.; Antunes, H.K.; Tufik, S.; de Mello, M.T. Mood, anxiety, and serum IGF-1 in elderly men given 24 weeks of high resistance exercise. Percept. Mot. Ski. 2010, 110, 265–276. [Google Scholar] [CrossRef]
- Mitschelen, M.; Yan, H.; Farley, J.A.; Warrington, J.P.; Han, S.; Herenu, C.B.; Csiszar, A.; Ungvari, Z.; Bailey-Downs, L.C.; Bass, C.E.; et al. Long-term deficiency of circulating and hippocampal insulin-like growth factor I induces depressive behavior in adult mice: A potential model of geriatric depression. Neuroscience 2011, 185, 50–60. [Google Scholar] [CrossRef]
- Jiang, P.; Dang, R.L.; Li, H.D.; Zhang, L.H.; Zhu, W.Y.; Xue, Y.; Tang, M.M. The Impacts of Swimming Exercise on Hippocampal Expression of Neurotrophic Factors in Rats Exposed to Chronic Unpredictable Mild Stress. Evid.-Based Complement. Altern. Med. 2014, 2014, 729827–729828. [Google Scholar] [CrossRef]
- Qiao, H.; An, S.C.; Xu, C.; Ma, X.M. Role of proBDNF and BDNF in dendritic spine plasticity and depressive-like behaviors induced by an animal model of depression. Brain Res. 2017, 1663, 29–37. [Google Scholar] [CrossRef]
- Binder, D.K.; Scharfman, H.E. Mini Review. Growth Factors 2009, 22, 123–131. [Google Scholar] [CrossRef]
- Marais, L.; Stein, D.J.; Daniels, W.M.U. Exercise increases BDNF levels in the striatum and decreases depressive-like behavior in chronically stressed rats. Metab. Brain Dis. 2009, 24, 587–597. [Google Scholar] [CrossRef]
- Karege, F.; Perret, G.; Bondolfi, G.; Schwald, M.; Bertschy, G.; Aubry, J.M. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002, 109, 143–148. [Google Scholar] [CrossRef]
- Sungkarat, S.; Boripuntakul, S.; Kumfu, S.; Lord, S.R.; Chattipakorn, N. Tai Chi Improves Cognition and Plasma BDNF in Older Adults with Mild Cognitive Impairment: A Randomized Controlled Trial. Neurorehabilit. Neural Repair 2018, 32, 142–149. [Google Scholar] [CrossRef]
- Naveen, G.H.; Thirthalli, J.; Rao, M.G.; Varambally, S.; Christopher, R.; Gangadhar, B.N. Positive therapeutic and neurotropic effects of yoga in depression: A comparative study. Indian J. Psychiatry 2013, 55, S400–S404. [Google Scholar] [CrossRef] [PubMed]
- Naveen, G.H.; Varambally, S.; Thirthalli, J.; Rao, M.; Christopher, R.; Gangadhar, B.N. Serum cortisol and BDNF in patients with major depression-effect of yoga. Int. Rev. Psychiatry 2016, 28, 273–278. [Google Scholar] [CrossRef]
- Cahn, B.R.; Goodman, M.S.; Peterson, C.T.; Maturi, R.; Mills, P.J. Yoga, Meditation and Mind-Body Health: Increased BDNF, Cortisol Awakening Response, and Altered Inflammatory Marker Expression after a 3-Month Yoga and Meditation Retreat. Front. Hum. Neurosci. 2017, 11, 315. [Google Scholar] [CrossRef] [PubMed]
- Voss, M.W.; Erickson, K.I.; Prakash, R.S.; Chaddock, L.; Kim, J.S.; Alves, H.; Szabo, A.; Phillips, S.M.; Wójcicki, T.R.; Mailey, E.L.; et al. Neurobiological markers of exercise-related brain plasticity in older adults. Brain Behav. Immun. 2012, 28, 90–99. [Google Scholar] [CrossRef]
- Hosang, G.M.; Shiles, C.; Tansey, K.E.; McGuffin, P.; Uher, R. Interaction between stress and the BDNF Val66Met polymorphism in depression: A systematic review and meta-analysis. BMC Med. 2014, 12, 7. [Google Scholar] [CrossRef]
- Chen, S.Z.; Jiang, H.T.; Liu, Y.; Hou, Z.H.; Yue, Y.Y.; Zhang, Y.Q.; Zhao, F.Y.; Xu, Z.; Li, Y.H.; Mou, X.D.; et al. Combined serum levels of multiple proteins in tPA-BDNF pathway may aid the diagnosis of five mental disorders. Sci. Rep. 2017, 7, 6871–6879. [Google Scholar] [CrossRef]
- Song, Q.-H.; Shen, G.-Q.; Xu, R.-M.; Zhang, Q.-H.; Ma, M.; Guo, Y.-H.; Zhao, X.-P.; Han, Y.-B. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder. Int. J. Physiol. Pathophysiol. Pharmacol. 2014, 6, 55–60. [Google Scholar] [PubMed]
- Chang, M.Y.; Yeh, S.C.; Chu, M.C.; Wu, T.M.; Huang, T.H. Associations between Tai Chi Chung program, anxiety, and cardiovascular risk factors. American journal of health promotion. Am. J. Health-Syst. Pharm. 2013, 28, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Siu, K.-C.; Padilla, C.; Rajaram, S.S. The interrelationship between balance, Tai Chi and depression in Latino older adults. Aging Clin. Exp. Res. 2017, 29, 395–401. [Google Scholar] [CrossRef]
- Herbert, A.; Esparham, A. Mind–Body Therapy for Children with Attention-Deficit/Hyperactivity Disorder. Children 2017, 4, 31. [Google Scholar] [CrossRef]
- Caldwell, K.L.; Bergman, S.M.; Collier, S.R.; Triplett, N.T.; Quin, R.; Bergquist, J.; Pieper, C.F. Effects of Tai Chi Chuan on anxiety and sleep quality in young adults: Lessons from a randomized controlled feasibility study. Nat. Sci. Sleep 2016, 8, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Bao, X.; Jin, K. The beneficial effect of Tai Chi on self-concept in adolescents. Int. J. Psychol. 2015, 50, 101–105. [Google Scholar] [CrossRef]
| Studies | Study Area | Study Design | Sample Size (N) | Female (%) | Mean Age (Years) |
|---|---|---|---|---|---|
| Bao et al. 2015 | China, Mainland | PPCGD 1 | TCC 2: 73; C 3: 69 | TCC: 52.1; C: 52.2 | TCC: 14.8; C: 14.7 |
| Chang et al. 2013 | China, Taipei | QED 4 | TCC: 64; C: 69 | TCC: 53.1; C: 65.2 | TCC: 56.5; C: 62.3 |
| Frith et al. 2011 | Australia | Field study | TCC: 29; C1 (CI 5): 30; C2 (AE 6): 34 | TCC: 62.1; C1: 53.3; C2: 50 | TCC: 37.2; C1: 30; C2: 27.7 |
| Frye et al. 2007 | USA | RCT 7 | TCC: 23; LIE 8: 28; C: 21 | Total: 54 | Total: 69.2 |
| Gallegos et al. 2016 | Spain | RCT | TCC: 68; Y 9: 85; M 10: 84; C: 45 | Total: 54.6 | Total: 20.3 |
| Hong et al. 2017 | China, Mainland | PPCGD | TCC: 60; C: 60 | TCC: 50; C: 50 | NR |
| Li, A et al. 2006 | China, Mainland | PPCGD | TCC: 59; C: 59 | Total: 47.5 | NR |
| Li, F et al. 2001 | USA | RCT | TCC: 40; C: 32 | Total: 75 | Total: 73.2 |
| Liao et al. 2018 | China, Mainland | RCT | TCC: 55; C: 52 | TCC: 65.5; C:57.7 | TCC: 71.84; C: 71.8 |
| Noradechanunt et al. 2017 | Australia | RCT | TCC: 9; Y: 11; C: 10 | TCC: 69.2; Y: 76.9; C: 76.9 | TCC: 67.2; Y: 67.6; C: 65.2 |
| Sattin et al. 2005 | USA | RCT | TCC: 92; WE 11: 82 | TCC: 95; WE: 94 | TCC: 80.4; WE: 80.5 |
| Schitter et al. 2016 | Switzerland | PPCGD | TCC: 28; C: 31 | Total: 66.7 | Total: 35.5 |
| Zhang et al. 2014 | China, Mainland | Five-arm RCT | TCC: 28; Swim 12: 29; Run 13: 27; SD 14: 30; C: 30 | TCC: 53.6; C: 46.7 | TCC: 65.5; C: 64.1 |
| Zheng et al. 2017 | Australia | Three-arm RCT | TCC: 17; Ex 15: 17; C: 16 | TCC: 64.7; Ex: 82.4; C: 87.5 | TCC: 35.4; Ex: 32; C: 34.6 |
| Studies | TCC Style | Weekly Dosage | Duration | Supervisor (Y or N) | Emotion Outcomes |
|---|---|---|---|---|---|
| Bao et al. 2015 | Yang style | 60 min × 5 | 1 year | Y 1 | PHCSCS 3 |
| Chang et al. 2013 | Cheng Style | 60 min × 3 | 12 weeks | Y | BAI 4 |
| Frith et al. 2011 | N/A 5 | 5~10 min × 3 | 5–10 min | Y | TESI 6 VAS 7 |
| Frye et al. 2007 | Yang style | 60 min × 3 | 12 weeks | Y | STAI 8 SAS 9 CES-D 10 |
| Gallegos et al. 2016 | Tsung Hwa/Canneti/Rooting/Chen style (Mixed) | 30 min × 2 | 30 × 2 min | Y | DASS-21 11 |
| Hong et al. 2017 | N/A | 60 min × 4 | 2 months | NR | SCL-90 12 |
| Li, A et al. 2006 | N/A | 30 min × 5 | 15 weeks | NR | SCL-90 |
| Li, F et al. 2001 | Condensed, classical Yang form | 60 min × 2 | 24 weeks | Y | CESD-20 13 PANAS-20 14 PWPD 15 SWLS 16 |
| Liao et al. 2018 | Yang Style | 50 min × 3 | 3 months | N/A | GDS 17 |
| Noradechanunt et al. 2017 | 12 Movement Sun style | 60 min × 2 | 12 weeks | N2 | CES-D |
| Sattin et al. 2005 | N/A | 60~90 min × 2 | 48 weeks | Y | CES-D |
| Schitter et al. 2016 | Yang style | 60 min × 2 | 12 weeks | Y | CES-D ADS-K 18 |
| Zhang et al. 2014 | N/A | 30~60 min × 3 | 18 months | Y | SECF 19 HAMA 20 HAMD 21 |
| Zheng et al. 2017 | Sim-24 | 60 min × 2 | 12 weeks | Y (First 6 weeks) | STAI PSS 22 SF-36 23 |
| Studies | Item 1 1 | Item 2 2 | Item 3 3 | Item 4 4 | Item 5 5 | Item 6 6 | Item 7 7 | Item 8 8 | Item 9 9 | Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Bao et al. 2015 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 6 |
| Chang et al. 2013 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 6 |
| Frith et al. 2011 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| Frye et al. 2007 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 7 |
| Gallego et al. 2016 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 6 |
| Hong et al. 2017 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Li, A et al. 2006 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Li, F et al. 2001 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 6 |
| Liao et al. 2018 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 7 |
| Noradechanunt et al. 2017 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 6 |
| Sattin et al. 2005 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Schitter et al. 2016 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Zhang et al. 2014 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 5 |
| Zheng et al. 2017 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 6 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, S.; Zou, L.; Chen, L.-Z.; Yao, Y.; Loprinzi, P.D.; Siu, P.M.; Wei, G.-X. The Effect of Tai Chi Chuan on Negative Emotions in Non-Clinical Populations: A Meta-Analysis and Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 3033. https://doi.org/10.3390/ijerph16173033
Zhang S, Zou L, Chen L-Z, Yao Y, Loprinzi PD, Siu PM, Wei G-X. The Effect of Tai Chi Chuan on Negative Emotions in Non-Clinical Populations: A Meta-Analysis and Systematic Review. International Journal of Environmental Research and Public Health. 2019; 16(17):3033. https://doi.org/10.3390/ijerph16173033
Chicago/Turabian StyleZhang, Shu, Liye Zou, Li-Zhen Chen, Ying Yao, Paul D. Loprinzi, Parco M. Siu, and Gao-Xia Wei. 2019. "The Effect of Tai Chi Chuan on Negative Emotions in Non-Clinical Populations: A Meta-Analysis and Systematic Review" International Journal of Environmental Research and Public Health 16, no. 17: 3033. https://doi.org/10.3390/ijerph16173033
APA StyleZhang, S., Zou, L., Chen, L.-Z., Yao, Y., Loprinzi, P. D., Siu, P. M., & Wei, G.-X. (2019). The Effect of Tai Chi Chuan on Negative Emotions in Non-Clinical Populations: A Meta-Analysis and Systematic Review. International Journal of Environmental Research and Public Health, 16(17), 3033. https://doi.org/10.3390/ijerph16173033





