Prevalence and Predictors of Vitamin D Deficiency among African Immigrants Living in Australia
Abstract
1. Introduction
2. Materials and Methods
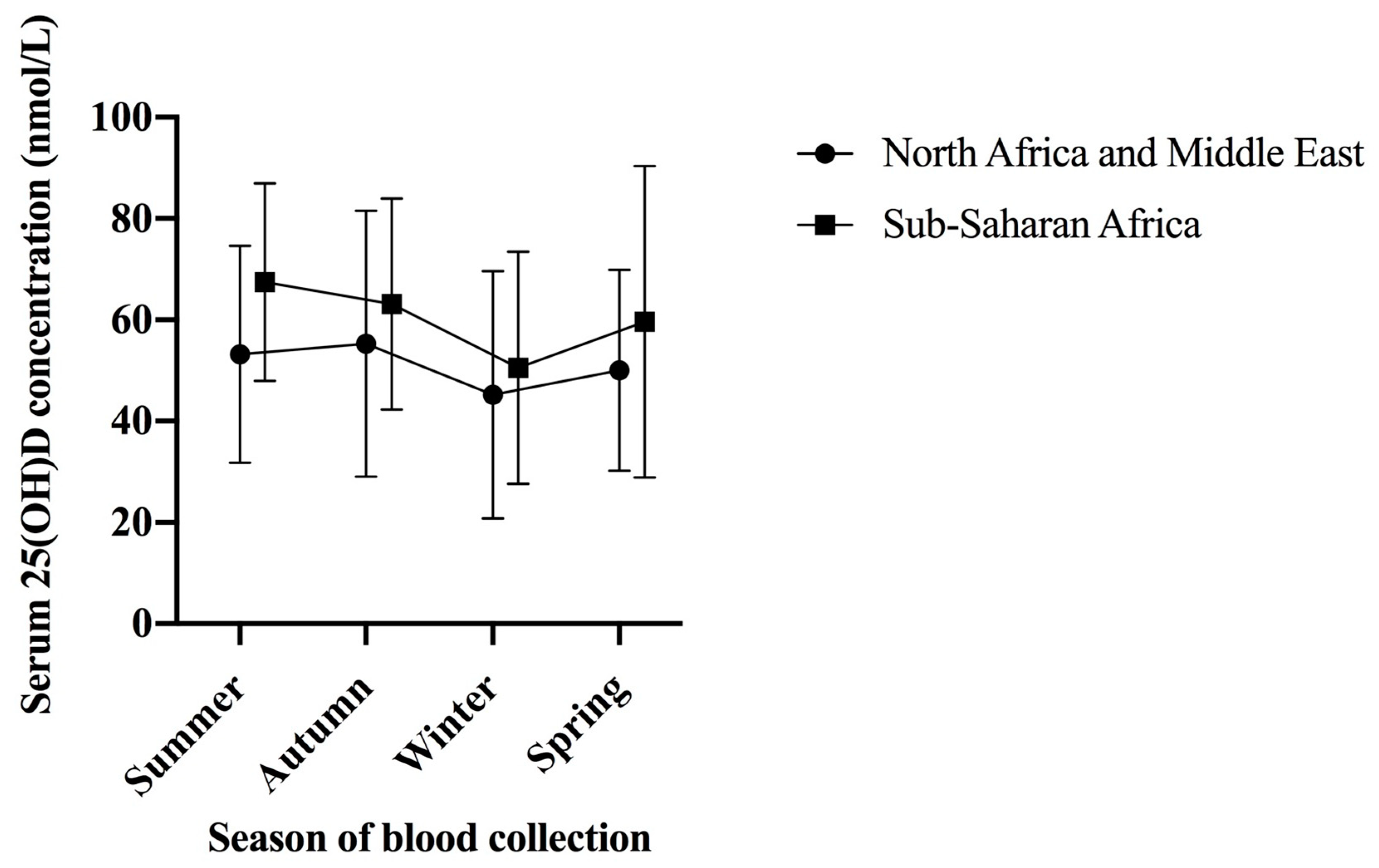
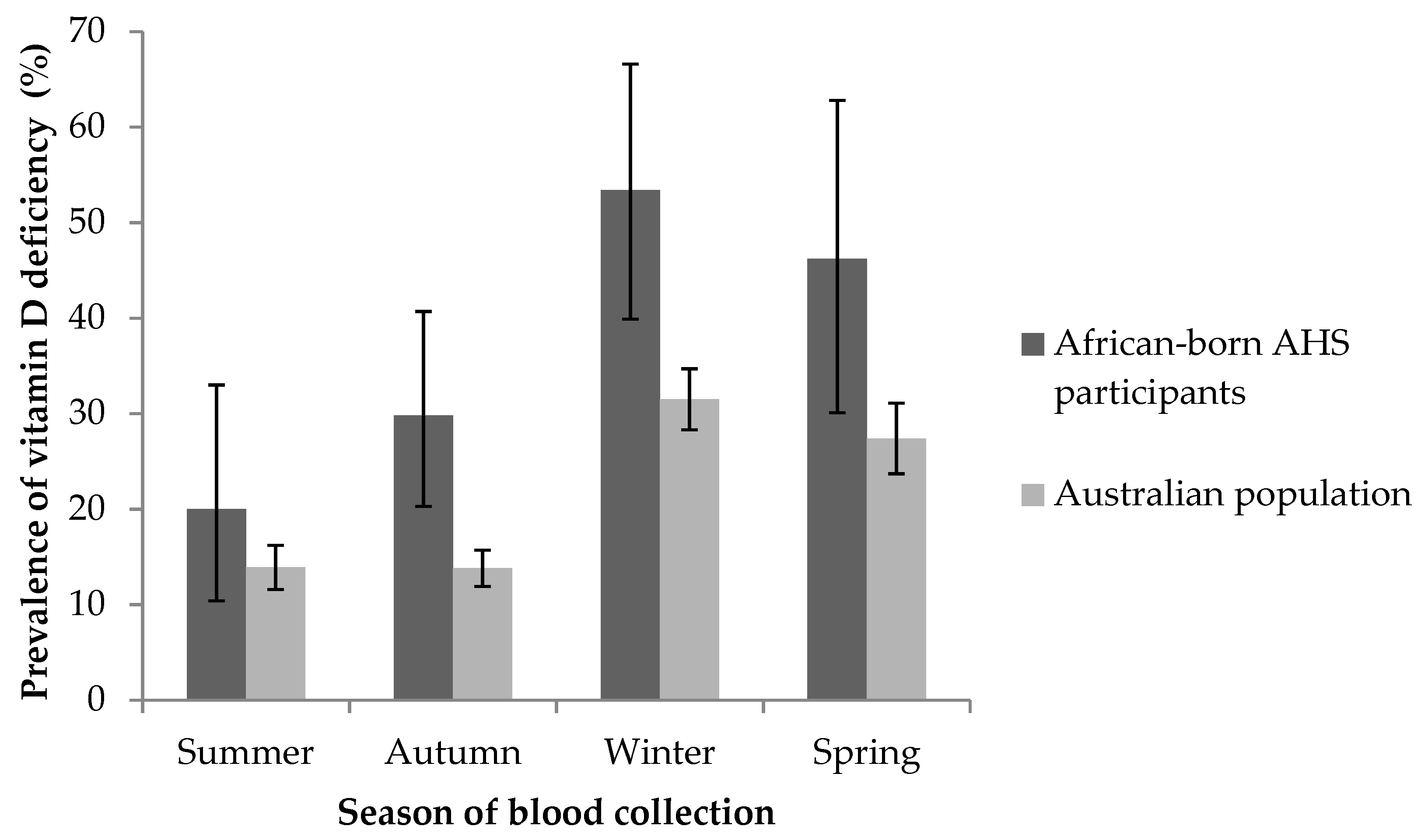
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid Biochem. Mol. Biol. 2014, 144, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Australian Health Survey: Biomedical Results for Nutrients, 2011–2012. Feature Article: Vitamin, D. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.006Chapter2002011-12 (accessed on 15 April 2014).
- Malacova, E.; Cheang, P.; Dunlop, E.; Sherriff, J.L.; Lucas, R.M.; Daly, R.M.; Nowson, C.A.; Black, L.J. Prevalence and predictors of vitamin D deficiency in a nationally representative sample of adults participating in the 2011–2013 Australian Health Survey. Br. J. Nutr. 2019, 121, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Skull, S.A.; Ngeow, J.Y.Y.; Biggs, B.A.; Street, A.; Ebeling, P.R. Vitamin D deficiency is common and unrecognized among recently arrived adult immigrants from The Horn of Africa. Intern. Med. J. 2003, 33, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Johnston, V.; Smith, L.; Roydhouse, H. The health of newly arrived refugees to the Top End of Australia: Results of a clinical audit at the Darwin Refugee Health Service. Aust. J. Prim. Health 2012, 18, 242–247. [Google Scholar] [CrossRef] [PubMed]
- McGillivray, G.; Skull, S.A.; Davie, G.; Kofoed, S.E.; Frydenberg, A.; Rice, J.; Cooke, R.; Carapetis, J.R. High prevalence of asymptomatic vitamin D and iron deficiency in East African immigrant children and adolescents living in a temperate climate. Arch. Dis. Child. 2007, 92, 1088–1093. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, M.; Wang, S.; Pal, A.; MacIntyre, C.R.; Wood, N.; Gunesekera, H. Vitamin D deficiency in refugee children from conflict zones. J. Immigr. Minority Health 2011, 13, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Benitez-Aguirre, P.Z.; Wood, N.J.; Biesheuvel, C.; Moreira, C.; Munns, C.F. The natural history of vitamin D deficiency in African refugees living in Sydney. Med. J. Aust. 2009, 190, 426–428. [Google Scholar] [PubMed]
- Gibney, K.B.; Marshall, C.; Torresi, J.; Biggs, B.A.; Leder, K.; Mihrshahi, S. The profile of health problems in African immigrants attending an infectious disease unit in Melbourne, Australia. Am. J. Trop. Med. Hyg. 2009, 80, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Renzaho, A.M.; Nowson, C.; Kaur, A.; Halliday, J.A.; Fong, D.; DeSilva, J. Prevalence of vitamin D insufficiency and risk factors for type 2 diabetes and cardiovascular disease among African migrant and refugee adults in Melbourne: A pilot study. Asia Pac. J. Clin. Nutr. 2011, 20, 397–403. [Google Scholar] [PubMed]
- Australian Bureau of Statistics. Census of Population and Housing: Selected Social and Housing Characteristics, Australia. 2001. Available online: http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/74B727D9E14BB247CA256DCC007F5048/$File/20150_2001%20(reissue).pdf (accessed on 28 October 2003).
- Australian Bureau of Statistics. Census of Population and Housing: Reflecting Australia—Stories from the Census 2016. Data Cube: Cultural Diversity. Available online: http://www.abs.gov.au/AUSSTATS/SUBSCRIBER.NSF/log?openagent&207103%20-%20cultural%20diversity.xls&2071.0&Data%20Cubes&21F50C2D0457EF67CA2581620019845C&0&2016&20.07.2017&Latest (accessed on 20 July 2017).
- Munns, C.F.; Simm, P.J.; Rodda, C.P.; Garnett, S.P.; Zacharin, M.R.; Ward, L.M.; Geddes, J.; Cherian, S.; Zurynski, Y.; Cowell, C.T. Incidence of vitamin D deficiency rickets among Australian children: An Australian Paediatric Surveillance Unit study. Med. J. Aust. 2012, 196, 466–468. [Google Scholar] [PubMed]
- Clemens, T.; Henderson, S.; Adams, J.; Holick, M.; Holick, M. Increased Skin Pigment Reduces the Capacity of Skin to Synthesise Vitamin D3. Lancet 1982, 319, 74–76. [Google Scholar] [CrossRef]
- Cancer Council Victoria. SunSmart: Tan or Have Naturally Dark Skin? You’re Still at Risk of Skin Cancer. Available online: https://www.sunsmart.com.au/skin-cancer/tan-or-have-naturally-dark-skin (accessed on 9 August 2019).
- Cancer Council Australia. Position Statement—Sun Exposure and Vitamin D—Risks and Benefits. Available online: https://wiki.cancer.org.au/policy/Position_statement_-_Risks_and_benefits_of_sun_exposure#_ga=2.119220041.1583773298.1561625835-1071210483.1460788295 (accessed on 9 August 2019).
- Australian Bureau of Statistics. Australian Health Survey: Biomedical Results for Nutrients, 2011–2012. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.006main+features12011-12 (accessed on 21 December 2015).
- Sempos, C.T.; Vesper, H.W.; Phinney, K.W.; Thienpont, L.M.; Coates, P.M. Vitamin D status as an international issue: National surveys and the problem of standardization. Scand. J. Clin. Lab. Investig. 2012, 243, 32–40. [Google Scholar]
- Mineva, E.M.; Schleicher, R.L.; Chaudhary-Webb, M.; Maw, K.L.; Botelho, J.C.; Vesper, H.W.; Pfeiffer, C.M. A Candidate Reference Measurement Procedure for Quantifying Serum Concentrations of 25-Hydroxyvitamin D3 and 25-Hydroxyvitamin D2 Using Isotope-Dilution Liquid Chromatography-Tandem Mass Spectrometry. Anal. Bioanal. Chem. 2015, 407, 5615–5624. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Australian Health Survey: Users’ Guide, 2011–2013. Available online: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4363.0.55.001Main+Features12011-13 (accessed on 7 June 2019).
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 16 February 2018).
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Australian Bureau of Statistics. 2071.0—Census of Population and Housing: Reflecting Australia—Stories from the Census. 2016. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/2071.0Main%20Features602016?opendocument&tabname=Summary&prodno=2071.0&issue=2016&num=&view= (accessed on 28 June 2017).
- Bureau of Meteorology. Sunshine: Average Daily Sunshine Hours. Available online: http://www.bom.gov.au/watl/sunshine/ (accessed on 9 August 2019).
- Binkley, N.; Krueger, D.C.; Morgan, S.; Wiebe, D. Current Status of Clinical 25-hydroxyvitamin D Measurement: An Assessment of Between-Laboratory Agreement. Clin. Chim. Acta 2010, 411, 1976–1982. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.; Neale, R. What is the optimal level of vitamin D? Separating the evidence from the rhetoric. Aust. Fam. Physician 2014, 43, 119–122. [Google Scholar] [PubMed]
- Pirrone, A.; Capetola, T.; Riggs, E.; Renzaho, A. Vitamin D deficiency awareness among African migrant women residing in high-rise public housing in Melbourne, Australia: A qualitative study. Asia Pac. J. Clin. Nutr. 2013, 22, 292–299. [Google Scholar] [PubMed]
- Yasmeen, S. Muslim Women as Citizens in Australia: Diverse Notions and Practices. Aust. J. Soc. Issues 2007, 42, 41–54. [Google Scholar] [CrossRef]
- Black, L.J.; Jacoby, P.; Nowson, C.A.; Daly, R.M.; Lucas, R.M. Predictors of Vitamin D-Containing Supplement Use in the Australian Population and Associations between Dose and Serum 25-Hydroxyvitamin D Concentrations. Nutrients 2016, 8, 356. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total Population | Vitamin D Deficient | Vitamin D Sufficient | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Sex | 0.849 | |||
| Men | 113 (48) | 40 (47) | 73 (48) | |
| Women | 123 (52) | 45 (53) | 78 (52) | |
| Age, years, mean (SD) | 45.5 (15) | 41.3 (15) | 47.9 (15) | 0.001 |
| Region of birth | 0.007 | |||
| North Africa and Middle East | 95 (40) | 44 (52) | 51 (34) | |
| Sub-Saharan Africa | 141 (60) | 41 (48) | 100 (66) | |
| Season | <0.001 | |||
| Summer/autumn (December–May) | 139 (59) | 36 (42) | 103 (68) | |
| Winter/spring (June–November) | 97 (41) | 49 (58) | 48 (32) | |
| Body mass index category | 0.036 | |||
| Underweight/healthy weight (<25 kg/m2) | 68 (29) | 26 (31) | 42 (28) | |
| Overweight (25.0 to <30 kg/m2) | 99 (42) | 27 (32) | 72 (48) | |
| Obese (≥30 kg/m2) | 69 (29) | 32 (38) | 37 (25) | |
| Smoking | 0.857 | |||
| Ex/non-smoker | 193 (82) | 69 (81) | 124 (82) | |
| Current | 43 (18) | 16 (19) | 27 (18) | |
| Education | 0.583 | |||
| Less than university | 111 (47) | 42 (49) | 69 (46) | |
| University | 125 (53) | 43 (51) | 82 (54) | |
| Physical activity | 0.032 | |||
| Low/sedentary | 154 (65) | 63 (74) | 91 (60) | |
| Moderate/high | 82 (35) | 22 (26) | 60 (40) | |
| Socioeconomic status | 0.101 | |||
| Low | 100 (42) | 42 (49) | 58 (38) | |
| High | 136 (58) | 43 (51) | 93 (62) | |
| Vitamin D status 1 | ||||
| Deficient (25(OH)D <50 nmol/L) | 85 (36) | N/A | N/A | N/A |
| Insufficient (25(OH)D 50 to <75 nmol/L) | 103 (44) | N/A | N/A | N/A |
| Sufficient (25(OH)D ≥75 nmol/L) | 48 (20) | N/A | N/A | N/A |
| Characteristic | PR (95% CI) | p-Value |
|---|---|---|
| Age, per year | 0.98 (0.97, 0.99) | 0.004 |
| Season | ||
| Summer/autumn | Ref | |
| Winter/spring | 1.89 (1.35, 2.64) | <0.001 |
| Physical activity | ||
| Moderate/high | Ref | |
| Low/sedentary | 1.64 (1.12, 2.39) | 0.011 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horton-French, K.; Dunlop, E.; Lucas, R.M.; Pereira, G.; Black, L.J. Prevalence and Predictors of Vitamin D Deficiency among African Immigrants Living in Australia. Int. J. Environ. Res. Public Health 2019, 16, 2855. https://doi.org/10.3390/ijerph16162855
Horton-French K, Dunlop E, Lucas RM, Pereira G, Black LJ. Prevalence and Predictors of Vitamin D Deficiency among African Immigrants Living in Australia. International Journal of Environmental Research and Public Health. 2019; 16(16):2855. https://doi.org/10.3390/ijerph16162855
Chicago/Turabian StyleHorton-French, Kahlea, Eleanor Dunlop, Robyn M. Lucas, Gavin Pereira, and Lucinda J. Black. 2019. "Prevalence and Predictors of Vitamin D Deficiency among African Immigrants Living in Australia" International Journal of Environmental Research and Public Health 16, no. 16: 2855. https://doi.org/10.3390/ijerph16162855
APA StyleHorton-French, K., Dunlop, E., Lucas, R. M., Pereira, G., & Black, L. J. (2019). Prevalence and Predictors of Vitamin D Deficiency among African Immigrants Living in Australia. International Journal of Environmental Research and Public Health, 16(16), 2855. https://doi.org/10.3390/ijerph16162855







