Impact of Adjuvant Modalities on Survival in Patients with Advanced Stage Endometrial Carcinoma: A Retrospective Analysis from a Tertiary Medical Center
Abstract
1. Introduction
2. Materials and Methods
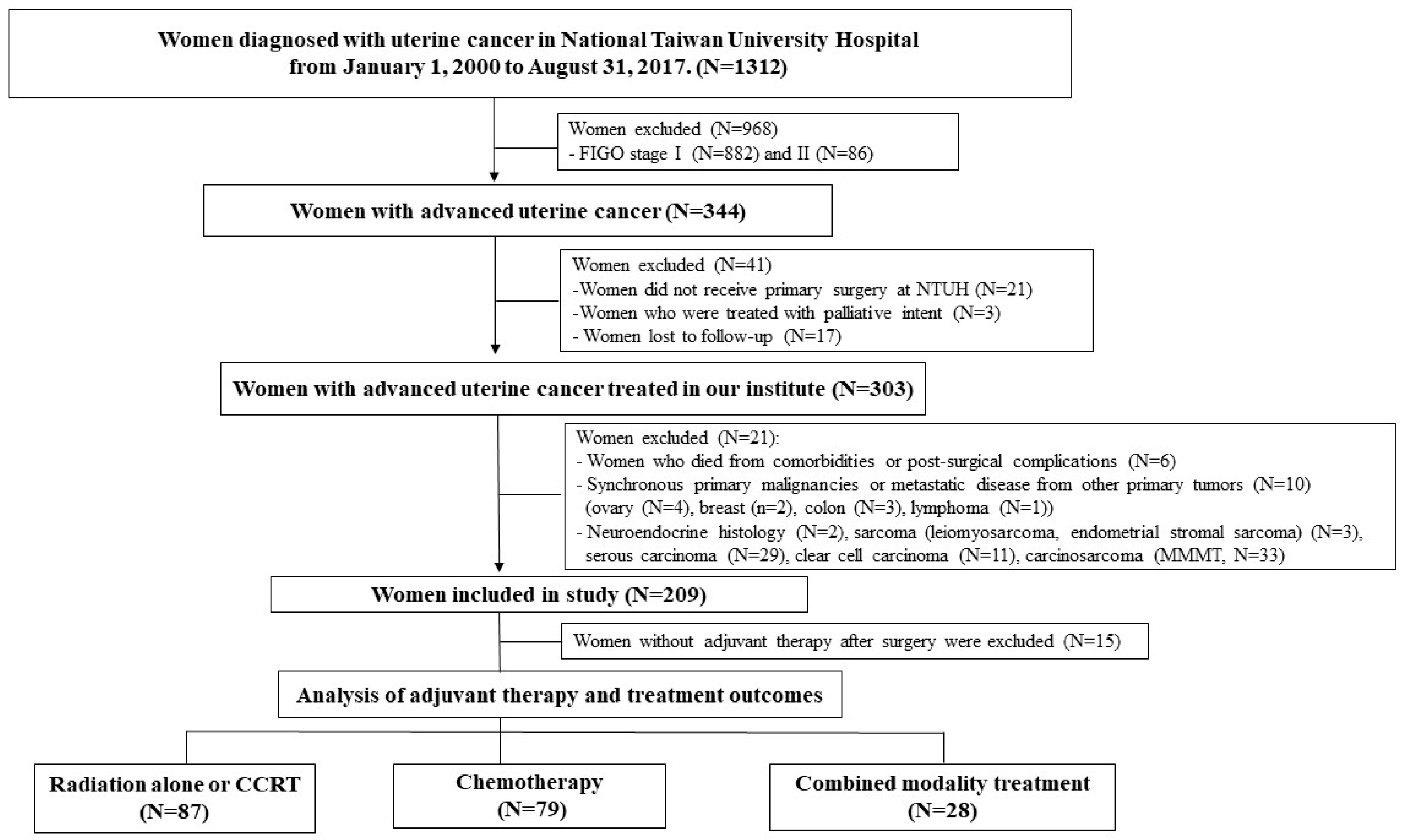
2.1. Patients
2.2. Surgery
2.3. Radiation Therapy
2.4. Chemotherapy
2.5. Combined Modality Therapy
2.6. Statistical Analyses
2.7. Details of Ethics Approval
3. Results
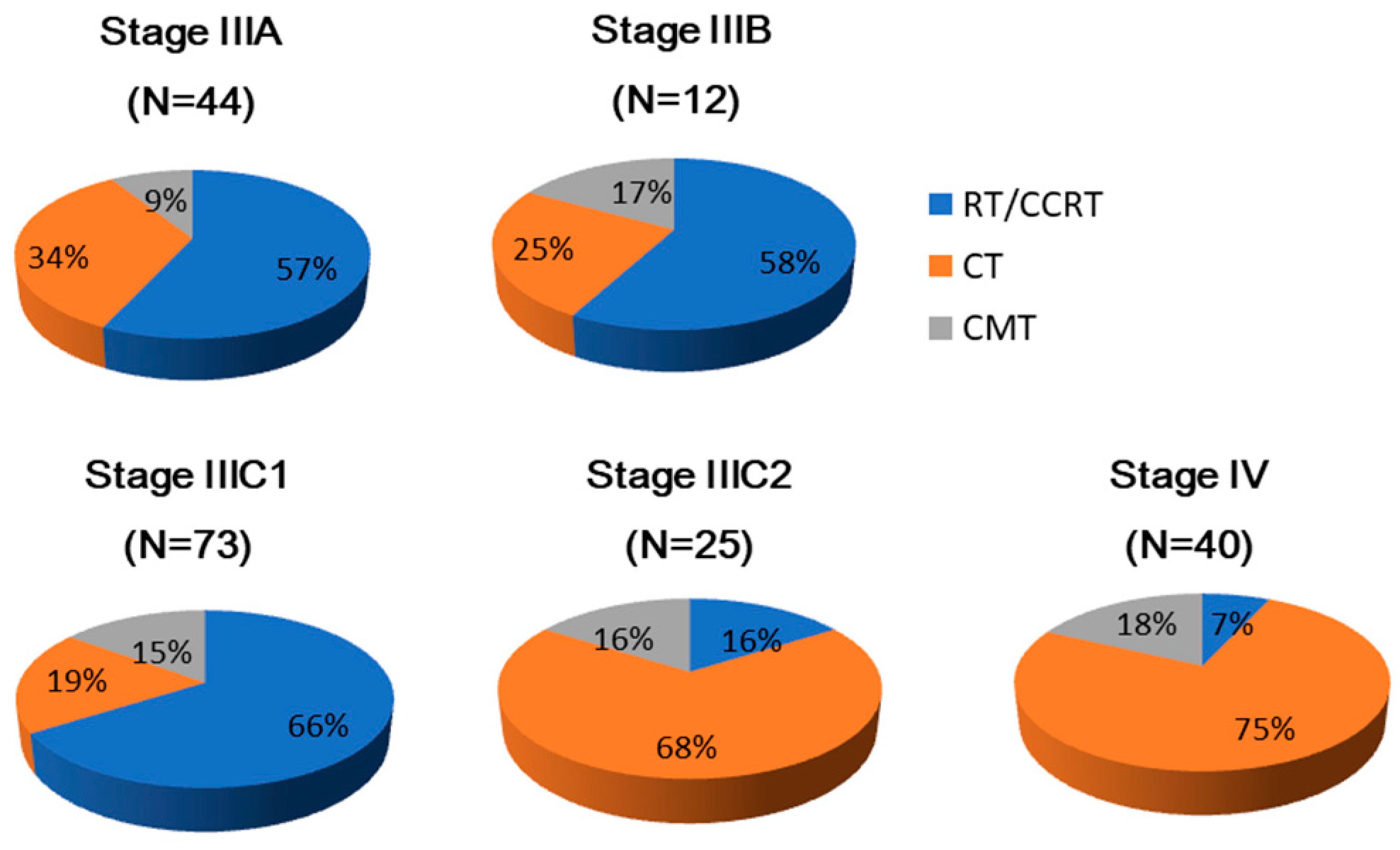
3.1. Patient Characteristics and Distribution of Adjuvant Therapies
3.2. Patient Demographics and Disease Patterns According to Tumor Grades
3.3. Risk Factors for Survival Related to Tumor Grades
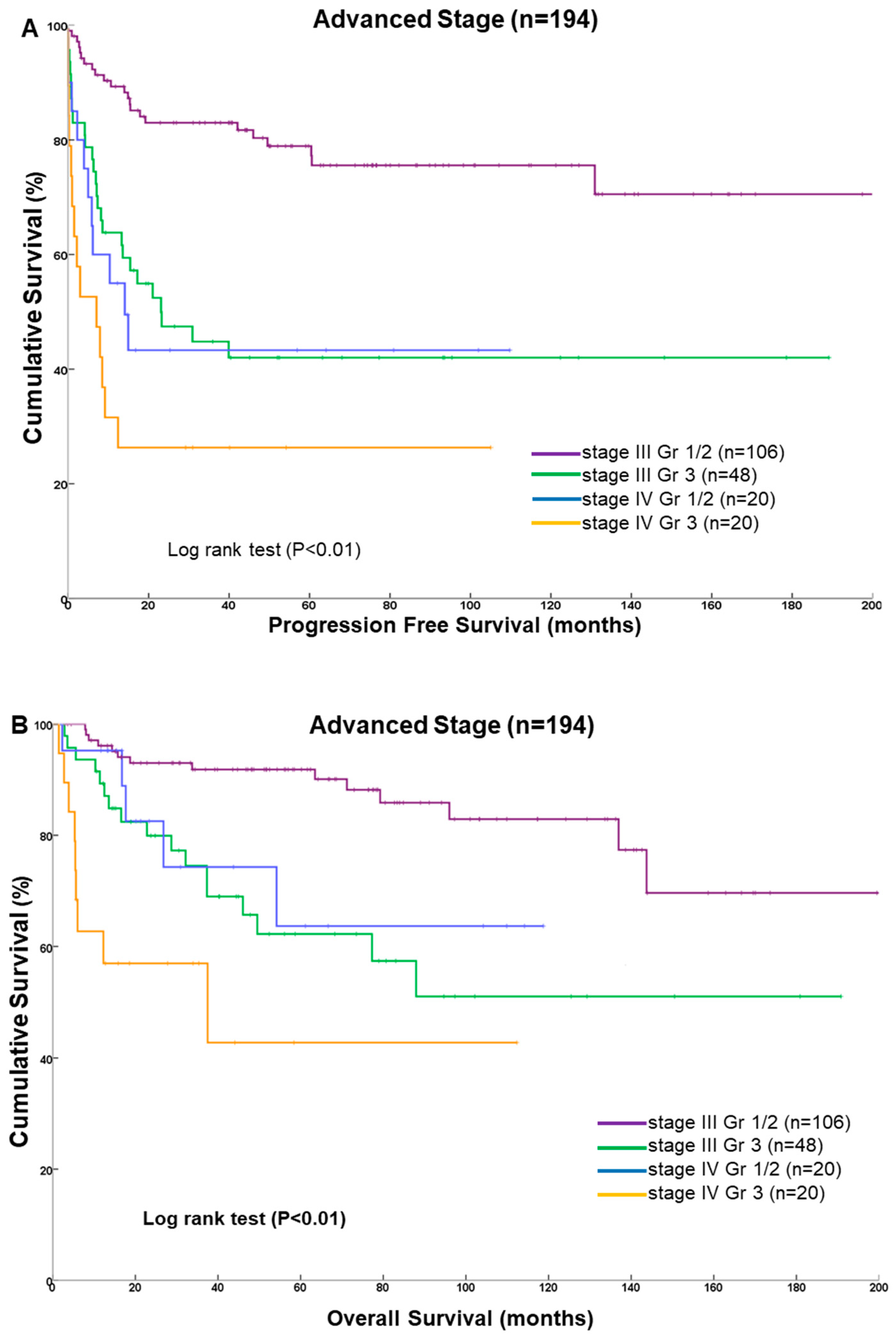
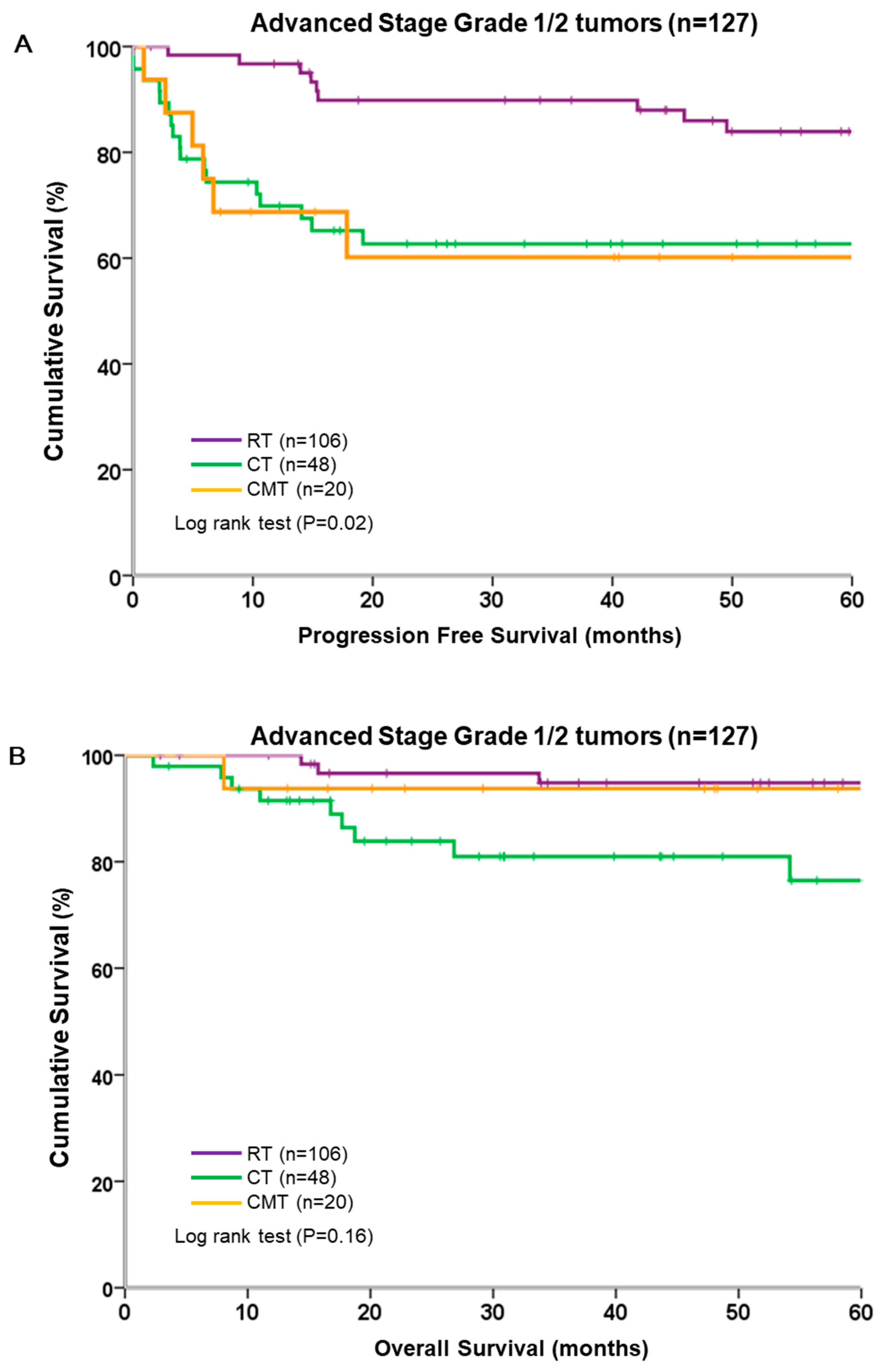
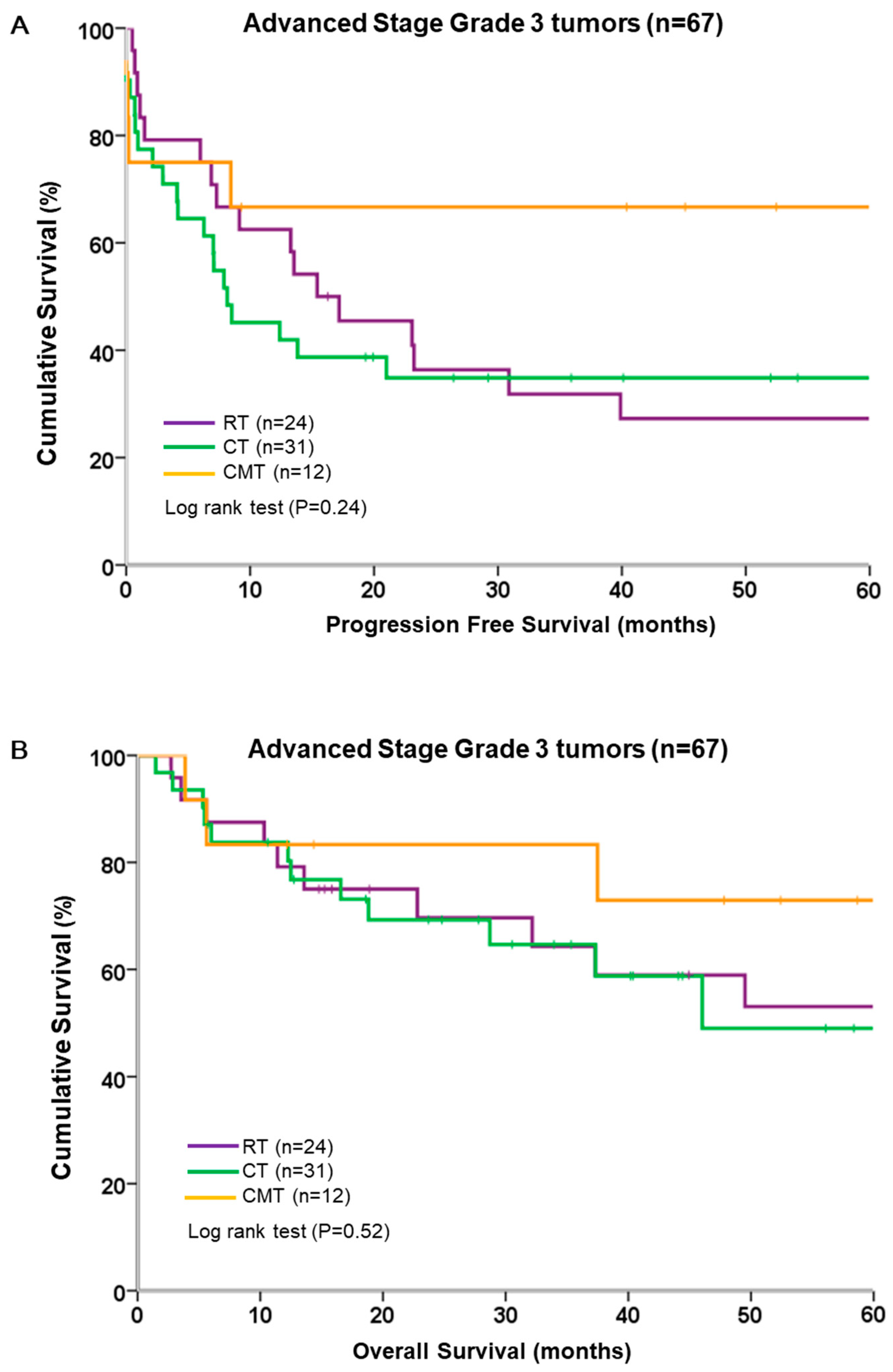
3.4. Survival Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lortet-Tieulent, J.; Ferlay, J.; Bray, F.; Jemal, A. International Patterns and Trends in Endometrial Cancer Incidence, 1978–2013. J. Natl. Cancer Inst. 2018, 110, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Cancer Registry. Incidence and Mortality Rates for the Top 10 Cancer among Females in Taiwan. 2014. Available online: http://tcr.cph.ntu.edu.tw/uploadimages/Top%2010%20cancer%20in%20Taiwan%202008-2014.pdf (accessed on 14 June 2019).
- Huang, C.Y.; Chen, C.A.; Chen, Y.L.; Chiang, C.J.; Hsu, T.H.; Lin, M.C.; Cheng, W.F. Nationwide surveillance in uterine cancer: Survival analysis and the importance of birth cohort: 30-year population-based registry in Taiwan. PLoS ONE 2012, 7, e51372. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Weng, C.S.; Huang, S.M.; Huang, N.; Chou, Y.J.; Wang, C.C.; Wang, K.L. Incidence and lifetime risk of uterine corpus cancer in Taiwanese women from 1991 to 2010. Taiwan. J. Obstet. Gynecol. 2017, 56, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Pecorelli, S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int. J. Gynaecol. Obstet. 2009, 105, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Amant, F.; Moerman, P.; Neven, P.; Timmerman, D.; Van Limbergen, E.; Vergote, I. Endometrial cancer. Lancet 2005, 366, 491–505. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Bokhman, J.V. Two pathogenetic types of endometrial carcinoma. Gynecol. Oncol. 1983, 15, 10–17. [Google Scholar] [CrossRef]
- Cao, Q.J.; Belbin, T.; Socci, N.; Balan, R.; Prystowsky, M.B.; Childs, G.; Jones, J.G. Distinctive gene expression profiles by cDNA microarrays in endometrioid and serous carcinomas of the endometrium. Int. J. Gynecol. Pathol. 2004, 23, 321–329. [Google Scholar] [CrossRef]
- Creutzberg, C.L.; Van Putten, W.L.; Koper, P.C.; Lybeert, M.L.; Jobsen, J.J.; Warlam-Rodenhuis, C.C.; Beerman, H. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: Multicentre randomised trial. Lancet 2000, 355, 1404–1411. [Google Scholar] [CrossRef]
- Keys, H.M.; Roberts, J.A.; Brunetto, V.L.; Zaino, R.J.; Spirtos, N.M.; Bloss, J.D.; Bell, J.G. A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: A Gynecologic Oncology Group study. Gynecol Oncol. 2004, 92, 744–751. [Google Scholar] [CrossRef]
- Maria, C.; Ammakkanavar, N.R.; Matei, D. Adjuvant therapy for endometrial cancer. J. Gynecol. Oncol. 2014, 25, 136–147. [Google Scholar]
- Galaal, K.; Al Moundhri, M.; Bryant, A.; Lopes, A.D.; Lawrie, T.A. Adjuvant chemotherapy for advanced endometrial cancer. Cochrane Database Syst. Rev. 2014, 5, CD010681. [Google Scholar] [CrossRef] [PubMed]
- Randall, M.E.; Filiaci, V.L.; Muss, H.; Spirtos, N.M.; Mannel, R.S.; Fowler, J.; Benda, J.A. Gynecologic Oncology Group Study. Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: A Gynecologic Oncology Group Study. J. Clin. Oncol. 2006, 24, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Maggi, R.; Lissoni, A.; Spina, F.; Melpignano, M.; Zola, P.; Favalli, G.; Fossati, R. Adjuvant chemotherapy vs radiotherapy in high-risk endometrial carcinoma: Results of a randomised trial. Br. J. Cancer 2006, 95, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.M.; Chang-Halpenny, C.; Hwang-Graziano, J. Sequential versus “sandwich” sequencing of adjuvant chemoradiation for the treatment of stage III uterine endometrioid adenocarcinoma. Gynecol. Oncol. 2015, 137, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Nam, E.J.; Kim, S.; Kim, Y.B.; Kim, Y.T. The benefit of adjuvant chemotherapy combined with postoperative radiotherapy for endometrial cancer: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.J.; Bu, P.; Feltmate, C.; Viswanathan, A.N. Adjuvant chemotherapy with external beam radiation therapy for high-grade, node-positive endometrial cancer. Int. J. Gynecol. Cancer 2014, 24, 1441–1448. [Google Scholar] [CrossRef] [PubMed]
- Matai, D.; Filiaci, V.; Randall, M.E.; Mutch, D.; Steinhoff, M.M.; DiSilvestro, P.A.; Moxley, K.M.; Spirtos, N.M. Adjuvant Chemotherapy plus Radiation for Locally Advanced Endometrial Cancer. N. Engl. J. Med. 2019, 380, 2317–2326. [Google Scholar] [CrossRef]
- De Boer, S.M.; Powell, M.E.; Mileshkin, L.; Katsaros, D.; Bessette, P.; Haie-Meder, C.; Fyles, A. Adjuvant chemoradiotherapy versus radiotherapy alone for women with high-risk endometrial cancer (PORTEC-3): Final results of an international, open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2018, 19, 295–309. [Google Scholar] [CrossRef]
- Suarez, A.A.; Felix, A.S.; Cohn, D.E. Bokhman Redux: Endometrial cancer "types" in the 21st century. Gynecol. Oncol. 2017, 144, 243–249. [Google Scholar] [CrossRef]
- Kang, S.; Kang, W.D.; Chung, H.H.; Jeong, D.H.; Seo, S.S.; Lee, J.M.; Kim, K.T. Preoperative identification of a low-risk group for lymph node metastasis in endometrial cancer: A Korean gynecologic oncology group study. J. Clin. Oncol. 2012, 30, 1329–1334. [Google Scholar] [CrossRef] [PubMed]
- Bestvina, C.M.; Fleming, G.F. Chemotherapy for Endometrial Cancer in Adjuvant and Advanced Disease Settings. Oncologist 2016, 21, 1250–1259. [Google Scholar] [CrossRef] [PubMed]
- Mundt, A.J.; McBride, R.; Rotmensch, J.; Waggoner, S.E.; Yamada, S.D.; Connell, P.P. Significant pelvic recurrence in high-risk pathologic stage I–IV endometrial carcinoma patients after adjuvant chemotherapy alone: Implications for adjuvant radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2001, 50, 1145–1153. [Google Scholar] [CrossRef]
- Sartori, E.; Laface, B.; Gadducci, A.; Maggino, T.; Zola, P.; Landoni, F.; Zanagnolo, V. Factors influencing survival in endometrial cancer relapsing patients: A Cooperation Task Force (CTF) study. Int. J. Gynecol. Cancer 2003, 13, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Onda, T.; Yoshikawa, H.; Mizutani, K.; Mishima, M.; Yokota, H.; Nagano, H.; Taketani, Y. Treatment of node-positive endometrial cancer with complete node dissection, chemotherapy and radiation therapy. Br. J. Cancer 1997, 75, 1836–1841. [Google Scholar] [CrossRef] [PubMed]
- Thigpen, J.T.; Buchsbaum, H.J.; Mangan, C.; Blessing, J.A. Phase II trial of adriamycin in the treatment of advanced or recurrent endometrial carcinoma: A Gynecologic Oncology Group study. Cancer Treat. Rep. 1979, 63, 21–27. [Google Scholar] [PubMed]
- Thigpen, J.T.; Blessing, J.A.; Homesley, H.; Creasman, W.T.; Sutton, G. Phase II trial of cisplatin as first-line chemotherapy in patients with advanced or recurrent endometrial carcinoma: A Gynecologic Oncology Group Study. Gynecol. Oncol. 1989, 33, 68–70. [Google Scholar] [CrossRef]
- Ball, H.G.; Blessing, J.A.; Lentz, S.S.; Mutch, D.G. A phase II trial of paclitaxel in patients with advanced or recurrent adenocarcinoma of the endometrium: A Gynecologic Oncology Group study. Gynecol. Oncol. 1996, 62, 278–281. [Google Scholar] [CrossRef]
- Humber, C.E.; Tierney, J.F.; Symonds, R.P.; Collingwood, M.; Kirwan, J.; Williams, C.; Green, J.A. Chemotherapy for advanced, recurrent or metastatic endometrial cancer: A systematic review of Cochrane collaboration. Ann. Oncol. 2007, 18, 409–420. [Google Scholar] [CrossRef]
- Hamilton, C.A.; Cheung, M.K.; Osann, K.; Chen, L.; Teng, N.N.; Longacre, T.A.; Chan, J.K. Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers. Br. J. Cancer 2006, 94, 642. [Google Scholar] [CrossRef]
- McGunigal, M.; Liu, J.; Kalir, T.; Chadha, M.; Gupta, V. Survival Differences Among Uterine Papillary Serous, Clear Cell and Grade 3 Endometrioid Adenocarcinoma Endometrial Cancers: A National Cancer Database Analysis. Int. J. Gynecol. Cancer 2017, 27, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.B.; Mariani, A.; Cliby, W.A.; Keeney, G.L.; Podratz, K.C.; Dowdy, S.C. Role of cytoreduction in stage III and IV uterine papillary serous carcinoma. Gynecol. Oncol. 2007, 107, 190–193. [Google Scholar] [CrossRef] [PubMed]
- Alagkiozidis, I.; Grossman, A.; Tang, N.Z.; Weedon, J.; Mize, B.; Salame, G.; Abulafia, O. Survival impact of cytoreduction to microscopic disease for advanced stage cancer of the uterine corpus: A retrospective cohort study. Int. J. Surg. 2015, 14, 61–66. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Number (%) |
|---|---|
| Age at diagnosis (years) (median, range) | 55.0 (26–81) |
| Preoperative CA-125 (U/mL) (median, range) | 62.7 (3.7–4544.7) |
| FIGO stage | |
| IIIA | 44 (22.7) |
| IIIB | 12 (6.2) |
| IIIC1 | 73 (37.6) |
| IIIC2 | 25 (12.9) |
| IVA | 3 (1.5) |
| IVB | 37 (19.1) |
| Lymph node sampling/dissection (n = 184) | |
| Pelvic alone | 132 (68.0) |
| Pelvic and para-aortic | 52 (26.8) |
| Number of pelvic lymph nodes retrieved (median, range) | 16 (1–60) |
| Number of para-aortic nodes retrieved (median, range) | 6 (1–19) |
| Residual tumor size <1 cm or >1 cm | 163 (84.0), 31 (16.0) |
| Histological grade 1, 2, 3 | 68 (35.1), 59 (30.4), 67 (34.5) |
| Lymph node metastases * | |
| Pelvic or para-aortic nodes alone | 97 (52.7), 4 (2.2) |
| Both pelvic and aortic nodes | 18 (9.8) |
| Postoperative adjuvant therapy | |
| RT † | 87 (44.8) |
| CT | 79 (40.7) |
| CMT | 28 (14.4) |
| Chemotherapeutic regimens (n = 113) | |
| Platinum and paclitaxel | 86 (44.3) |
| Platinum and anthracyclines | 16 (8.2) |
| Platinum alone | 6 (3.1) |
| Platinum with the other regimens | 3 (1.5) |
| Platinum, anthracycline, and paclitaxel | 2 (1.0) |
| Follow-up time (months) (median, range) | 45.5 (6.2–207.9) |
| Characteristics | Grade 1/2 (n = 127) | Grade 3 (n = 67) | p Value |
|---|---|---|---|
| Age (years) median (range) | 54.9 (26–76) | 55.4 (29–80.7) | 0.60 |
| BMI (kg/m2) median (range) | 24.4(14.2–42.7) | 24.9 (15.2–39.4) | 0.80 |
| CA-125 (U/mL) | 58.8 (3.7–1376) | 79.1 (6.9–4545) | 0.72 |
| FIGO stage (2009) | |||
| III IIIA | 36 (28.3%) | 8 (11.9%) | 0.04 |
| IIIB | 6 (4.7%) | 6 (9.0%) | |
| IIIC1 | 50 (39.4%) | 23 (34.3%) | |
| IIIC2 | 14 (11%) | 11 (16.4%) | |
| IV IVA | 2 (1.6%) | 1 (1.5%) | 0.52 |
| IVB | 19(15%) | 18 (26.9%) | |
| Primary tumor size | |||
| <2 cm | 22 (17.3%) | 5 (7.5%) | 0.07 |
| ≥2 cm | 105 (82.7%) | 62 (92.5%) | |
| Depth of myometrial invasion | |||
| < 1/2 | 57 (44.9%) | 18 (26.9%) | 0.04 |
| ≥1/2 | 70 (55.1%) | 49 (73.1%) | |
| LVSI | 76 (59.8%) | 61 (91 %) | 0.001 |
| Lymph node metastases * | |||
| Yes | 74 (58.3%) | 48 (71.6%) | 0.03 |
| No | 50 (39.4%) | 12 (17.9%) | |
| Postoperative adjuvant therapy | |||
| RT | 63 (49.6%) | 24 (35.8%) | 0.14 |
| CT | 48 (37.8%) | 31 (46.3%) | |
| CMT | 16 (12.6%) | 12 (17.9%) | |
| Treatment outcome | |||
| Recurrence and/or progression | 32 (25.2%) | 41 (61.2%) | <0.01 |
| Death (%) | 15 (11.8%) | 26 (38.8) | <0.01 |
| Progression-free time (months) | 47.2 (14.0–86.5) | 10.3 (1.8–40.0) | <0.01 |
| Follow-up (months) | 57.5 (22.5–96.9) | 26.3 (10.4–57.8) | <0.01 |
| Grade 1/2 | Grade 3 | |||||||
|---|---|---|---|---|---|---|---|---|
| PFS | OS | PFS | OS | |||||
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| FIGO stage | ||||||||
| IIIA | 1 | 1 | 1 | 1 | ||||
| IIIB | 2.89 (0.69,12.2) | 0.15 | 3.65 (0.32,41.6) | 0.22 | 0.80 (0.18,3.60) | 0.77 | 0.18 (0.02,1.78) | 0.44 |
| IIIC (IIIC1+IIIC2) | 1.12 (0.41,3.08) | 0.83 | 2.70 (0.55,13.2) | 0.30 | 0.38 (0.07,2.15) | 0.27 | 0.42 (0.12,1.48) | 0.05 |
| IV (IVA+IVB) | 1.32 (0.31,5.65) | 0.71 | 5.75 (0.95,34.7) | 0.06 | 1.37 (0.22,8.62) | 0.74 | 1.49 (0.36,6.10) | 0.58 |
| Myometrial invasion | ||||||||
| <1/2 | 1 | 0.18 | 1 | 0.74 | 0.48 | 1 | 0.49 | |
| ≥1/2 | 1.78 (0.77,4.10) | 1.19 (0.43,3.30) | 1.43 (0.52,3.93) | 1.39(0.55,3.51) | ||||
| Lymph nodes metastases | ||||||||
| No | 1 | 0.06 | 1 | 0.93 | 1 | 0.61 | 1 | 0.09 |
| Yes | 2.75 (0.96,7.90) | 1.23 (2.15,9.24) | 1.45 (0.35,6.11) | 9.46(0.71,125.4) | ||||
| Residual tumor size | ||||||||
| ≥1 cm | 1 | 0.03 | 1 | 0.25 | 1 | 0.45 | 1 | 0.71 |
| <1cm | 0.31 (0.10,0.90) | 0.36 (0.06,2.09) | 0.76 (0.25,1.81) | 1.24 (0.14,2.31) | ||||
| Adjuvant therapy | ||||||||
| RT | 1 | 1 | 1 | 1 | ||||
| CT | 1.59 (0.64,3.97) | 0.32 | 1.54 (0.43,5.51) | 0.51 | 0.91 (0.40,2.06) | 0.82 | 0.40 (0.11,1.38) | 0.15 |
| CMT | 2.03 (0.72,5.74) | 0.18 | 0.42 (0.05,3.93) | 0.45 | 0.31 (0.09,1.11) | 0.07 | 0.15 (0.03,0.89) | 0.04 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tai, Y.-J.; Hsu, H.-C.; Chiang, Y.-C.; Chen, Y.-L.; Chen, C.-A.; Cheng, W.-F. Impact of Adjuvant Modalities on Survival in Patients with Advanced Stage Endometrial Carcinoma: A Retrospective Analysis from a Tertiary Medical Center. Int. J. Environ. Res. Public Health 2019, 16, 2561. https://doi.org/10.3390/ijerph16142561
Tai Y-J, Hsu H-C, Chiang Y-C, Chen Y-L, Chen C-A, Cheng W-F. Impact of Adjuvant Modalities on Survival in Patients with Advanced Stage Endometrial Carcinoma: A Retrospective Analysis from a Tertiary Medical Center. International Journal of Environmental Research and Public Health. 2019; 16(14):2561. https://doi.org/10.3390/ijerph16142561
Chicago/Turabian StyleTai, Yi-Jou, Heng-Cheng Hsu, Ying-Cheng Chiang, Yu-Li Chen, Chi-An Chen, and Wen-Fang Cheng. 2019. "Impact of Adjuvant Modalities on Survival in Patients with Advanced Stage Endometrial Carcinoma: A Retrospective Analysis from a Tertiary Medical Center" International Journal of Environmental Research and Public Health 16, no. 14: 2561. https://doi.org/10.3390/ijerph16142561
APA StyleTai, Y.-J., Hsu, H.-C., Chiang, Y.-C., Chen, Y.-L., Chen, C.-A., & Cheng, W.-F. (2019). Impact of Adjuvant Modalities on Survival in Patients with Advanced Stage Endometrial Carcinoma: A Retrospective Analysis from a Tertiary Medical Center. International Journal of Environmental Research and Public Health, 16(14), 2561. https://doi.org/10.3390/ijerph16142561





