Lung Cancer Mortality Trends in a Brazilian City with a Long History of Asbestos Consumption
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Geographical Areas
2.3. Data Extraction and Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Zanetti, R.; Ferlay, J. Cancer Incidence in Five Continents; International Agency for Research on Cancer: Lyon, France, 2017; Volume XI, Available online: http://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet.pdf (accessed on 22 April 2019).
- Instituto Nacional de Câncer, Brasil. Available online: https://www.inca.gov.br/MortalidadeWeb/pages/Modelo10/consultar.xhtml#panelResultado (accessed on 22 April 2019).
- Kim, C.H.; Lee, Y.C.; Hung, R.J.; McNallan, S.R.; Cote, M.L.; Lim, W.Y.; Chang, S.C.; Kim, J.H.; Ugolini, D.; Chen, Y.; et al. Exposure to secondhand tobacco smoke and lung cancer by histological type: A pooled analysis of the International Lung Cancer Consortium (ILCCO). Int. J. Cancer 2014, 135, 1918–1930. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.W.; Harrison, J.D.; Laurier, D.; Birchall, A.; Blanchardon, E.; Paquet, F.; Tirmarche, M. Doses and lung cancer risks from exposure to radon and plutonium. Int. J. Radiat. Biol. 2014, 90, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Vainio, H.; Boffetta, P. Mechanisms of the combined effect of asbestos and smoking in the etiology of lung cancer. Scand. J. Work Environ. Health 1994, 20, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Alberg, A.J.; Ford, J.G.; Samet, J.M. Epidemiology of Lung Cancer: ACCP Evidence-Based Clinical Practice Guidelines, 2nd ed.; American College of Chest Physicians: Glenview, IL, USA, 2007; pp. 29S–55S. [Google Scholar] [CrossRef]
- World Health Organization; International Agency for Research on Cancer (IARC). Arsenic, Metals, Fibres and Dusts. 2012. Available online: https://monographs.iarc.fr/iarc-monographs-on-the-evaluation-of-carcinogenic-risks-to-humans-19 (accessed on 18 June 2019).
- World Health Organization. Elimination of Asbestos-Related Diseases; WHO Press: Geneva, Switzerland, 2006; Available online: https://apps.who.int/iris/bitstream/handle/10665/69479/WHO_SDE_OEH_06.03_eng.pdf;jsessionid=67D1E45B29963413E8C8DF4D9A9A352F?sequence=1 (accessed on 22 April 2019).
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet Glob. Health 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Markowitz, S. Cancer of the Respiratory Tract Due to Asbestos and Zeolites. In Parkes’ Occupational Lung Disorders, Newman, T.A., Cullinan, P., Blanc, P., Pickering, A., Eds.; 4th ed.; Taylor & Francis: Boca Raton, FL, USA, 2017; pp. 259–276. ISBN 978–1–4822–4070–2. [Google Scholar]
- Markowitz, S.B.; Levin, S.M.; Miller, A.; Morabia, A. Asbestos, asbestosis, smoking, and lung cancer. New findings from the North American insulator cohort. Am. J. Respir. Crit. Care Med. 2013, 188, 90–96. [Google Scholar] [CrossRef] [PubMed]
- International Ban Asbestos Secretariat. Available online: http://ibasecretariat.org/graphics_page.php (accessed on 6 March 2019).
- Algranti, E.; Mendonça, E.M.C.; De Capitani, E.M.; Freitas, J.B.P.; Silva, H.C.; Bussacos, M.A. Non-malignant asbestos-related diseases in Brazilian asbestos-cement workers. Am. J. Ind. Med. 2001, 40, 240–254. [Google Scholar] [CrossRef] [PubMed]
- Algranti, E.; Saito, C.A.; Carneiro, A.P.; Moreira, B.; Mendonca, E.M.; Bussacos, M.A. The next mesothelioma wave: Mortality trends and forecast to 2030 in Brazil. Cancer Epidemiol. 2015, 39, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Ferster, A.P.O.; Schubart, J.; Kim, Y.; Goldenberg, D. Association between laryngeal cancer and asbestos exposure a systematic review. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 409–416. [Google Scholar] [CrossRef]
- Toporcov, T.N.; Wünsch Filho, V. Epidemiological science and cancer control. Clinics 2018, 73, e627s. [Google Scholar] [CrossRef]
- Mc Cormack, V.; Peto, J.; Byrnes, G.; Straif, K.; Boffetta, P. Estimating the asbestos-related lung cancer burden from mesothelioma mortality. Br. J. Cancer 2012, 106, 575–584. [Google Scholar] [CrossRef]
- Ministério da Saúde, Brasil. Informações de Saúde. Estatísticas Vitais. Available online: http://www2.datasus.gov.br/DATASUS/index.php?area=0205 (accessed on 6 February 2019).
- Instituto Brasileiro de Geografia e Estatística, Brasil. Available online: https://cidades.ibge.gov.br/ (accessed on 24 March 2019).
- Ministério da Saúde, Brasil. Informações de Saúde. Demográficas e Socioeconômicas. Available online: http://www2.datasus.gov.br/DATASUS/index.php?area=0206&id=6942 (accessed on 6 February 2019).
- Doll, R.; Cook, P. Summarizing indices for comparison of cancer incidence data. Int. J. Cancer 1967, 2, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Joinpoint Version 4.6.0.0. Surveillance Research Program: National Cancer Institute. 2018. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 16 October 2018).
- Holford, T.R. Understanding the effects of age, period, and cohort on incidence and mortality rates. Annu. Rev. Public Health 1991, 12, 435–457. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.R.; Wakefield, J. A review and comparison of age-cohort models for cancer incidence. Stat. Sci. 2016, 31, 591–610. [Google Scholar] [CrossRef]
- Hashim, D.; Boffetta, P.; La Vecchia, C.; Rota, M.; Bertuccio, P.; Malvezzi, M.; Negri, E. The global decrease in cancer mortality: Trends and disparities. Ann. Oncol. 2016, 27, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Yang, D.; He, J.; Krasna, M.J. Epidemiology of lung cancer. Surg. Oncol. Clin. N. Am. 2016, 25, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, D.; Dandona, R.; Dandona, L.; et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-Adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [CrossRef] [PubMed]
- GBD. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: A systematic analysis from the global burden of disease study 2015. Lancet 2017, 389, 1885–1906. [Google Scholar] [CrossRef]
- Levy, D.; Almeida, L.M.; Szklo, A. The Brazil SimSmoke policy simulation model: The effect of strong tobacco control policies on smoking prevalence and smoking-attributable deaths in a middle income nation. PLoS Med. 2012, 9, e1001336. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cavalcante, T.M.; Moura, C.E.; Claro, R.M.; Szwarcwald, C.L. Population-based evidence of a strong decline in the prevalence of smokers in Brazil (1989–2003). Bull. World Health Organ. 2007, 85, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Malta, D.C.; Stopa, S.R.; Santos, M.A.S.; Andrade, S.S.C.A.; Oliveira, T.P.; Cristo, E.B.; Silva, M.M.A. Evolução de indicadores do tabagismo segundo inquéritos de telefone, 2006–2014. Cad. Saude Publ. 2017, 33, 45–56. [Google Scholar] [CrossRef]
- Nielsen, L.S.; Baelum, J.; Rasmussen, J.; Dahl, S.; Olsen, K.E.; Albin, M.; Hansen, N.C.; Sherson, D. Occupational asbestos exposure and lung cancer—A systematic review of the literature. Arch. Environ. Occup. Health 2014, 69, 191–206. [Google Scholar] [CrossRef] [PubMed]
- Lévêque, E.; Lacourt, A.; Luce, D.; Sylvestre, M.P.; Guénel, P.; Stücker, I.; Leffondré, K. Time-dependent effect of intensity of smoking and of occupational exposure to asbestos on the risk of lung cancer: Results from the ICARE case-control study. Occup. Environ. Med. 2018, 75, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Ollier, M.; Chamoux, A.; Naughton, G.; Pereira, B.; Dutheil, F. Chest CT scan screening for lung cancer in asbestos occupational exposure: A systematic review and meta-analysis. Chest 2014, 145, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Algranti, A.; Ramos-Bonilla, J.P.; Terracini, B.; Santana, V.S.; Comba, P.; Pasetto, R.; Mazzeo, A.; Cavariani, F.; Trotta, A.; Marsili, D. Prevention of asbestos exposure in latin america within a global public health perspective. An. Glob. Health 2019, 85, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Van der Bij, S.; Vermeulen, R.C.H.; Portengen, L.; Moons, K.G.M.; Koffijberg, H. Expected number of asbestos-related lung cancers in The Netherlands in the next two decades: A comparison of methods. Occup. Environ. Med. 2016, 73, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Schonfeld, S.J.; McCormack, V.; Rutherford, M.J.; Schüz, J. Regional variations in German mesothelioma mortality rates: 2000–2010. Cancer Causes Control 2014, 25, 615–624. [Google Scholar] [CrossRef]
- Marinaccio, A.; Montanaro, F.; Mastrantonio, M.; Uccelli, R.; Altavista, P.; Nesti, M.; Costantini, A.S.; Gorin, G. Predictions of mortality from pleural mesothelioma in Italy: A model based on asbestos consumption figures supports results from age-period-cohort model. Int. J. Cancer 2005, 115, 142–147. [Google Scholar] [CrossRef]
- Pitarque, S.; Clèries, R.; Martínez, J.M.; López-Abente, G.; Kogevinas, M.; Benavides, F.G. Mesothelioma mortality in men: Trends during 1977–2001 and projections for 2002–2016 in Spain. Occup. Environ. Med. 2008, 65, 279–282. [Google Scholar] [CrossRef]
- Joly, D.J. El habito de fumar cigarrillos en la America Latina: Una encuesta en ocho ciudades. Bol. Oficina Sanit. Panam. 1975, 79, 93–111. [Google Scholar]
- Rego, R.A.; Berardo, F.A.N.; Rodrigues, S.S.R.; Oliveira, Z.M.A.; Oliveira, M.B.; Vasconcellos, C.; Aventurate, L.V.O.; José, E.C.; Moncau, J.E.C.; Ramos, L.R. Fatores de risco para doenças crônicas não-transmissíveis: Inquérito domiciliar no município de São Paulo, SP (Brasil). Metodologia e resultados preliminares. Rev. Saude Publica 1990, 24, 277–285. [Google Scholar] [CrossRef]
- Marcopito, L.F.; Rodrigues, S.S.F.; Pacheco, M.A.; Shirassu, M.M.; Goldfeder, A.J.; de Moraes, M.A. Prevalência de alguns fatores de risco para doenças crônicas na cidade de São Paulo. Rev. Saude Publica 2005, 39, 738–745. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fidler, M.M.; Soerjomataram, I.; Bray, F. A global view on cancer incidence and national levels of the human development índex. Int. J. Cancer 2016, 139, 2436–2446. [Google Scholar] [CrossRef] [PubMed]
- Youlden, D.R.; Cramb, S.M.; Baade, P.D. The international epidemiology of lung cancer: Geographical distribution and secular trends. J. Thorac. Oncol. 2008, 3, 819–831. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.I.; Weiderpass, E. Lung cancer mortality trends in 36 european countries: Secular trendsand birth cohort patterns by sex and region 1970–2007. Int. J. Cancer 2010, 126, 1454–1466. [Google Scholar] [CrossRef] [PubMed]
- Companhia Ambiental do Estado de São Paulo (CETESB). Qualidade do ar no estado de São Paulo. Available online: https://cetesb.sp.gov.br/ar/publicacoes-relatorios/ (accessed on 18 June 2019).
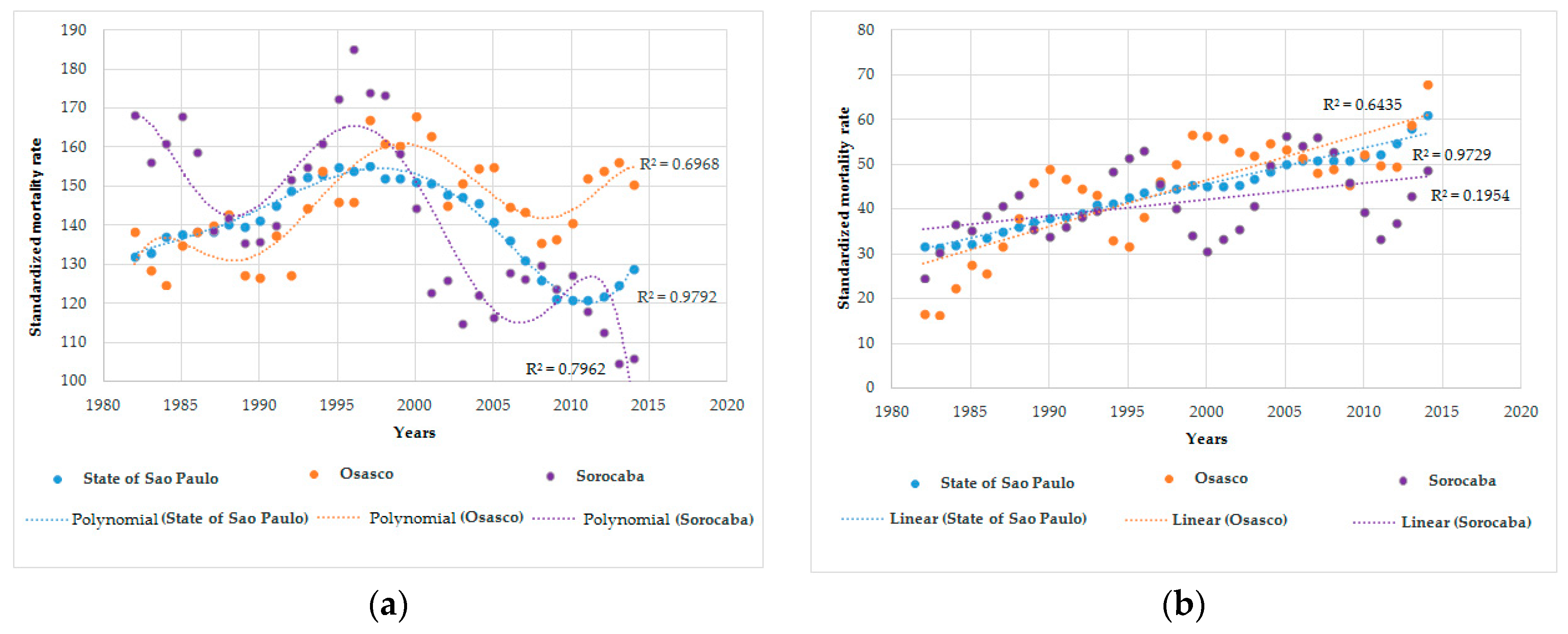
| Place | ASR 1 | AAPC 2 | ||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||
| 1980–1984 | 2012–2016 | 1980–1984 | 2012–2016 | 1980–2016 | 1980–2016 | |
| Osasco | 138.47 | 150.54 | 16.72 | 67.80 | 0.7 * (0.1 to 1.3) | 4.7 * (2.9 to 6.5) |
| Sorocaba | 168.50 | 106.9 | 24.78 | 48.78 | –1.5 *(–2.4 to -0.6) | 1.5 (-0.9 to 3.9) |
| São Paulo State | 132.09 | 129.01 | 31.75 | 60.88 | –0.1 (–0.3 to 0.1) | 2.2 *(1.9 to 2.5) |
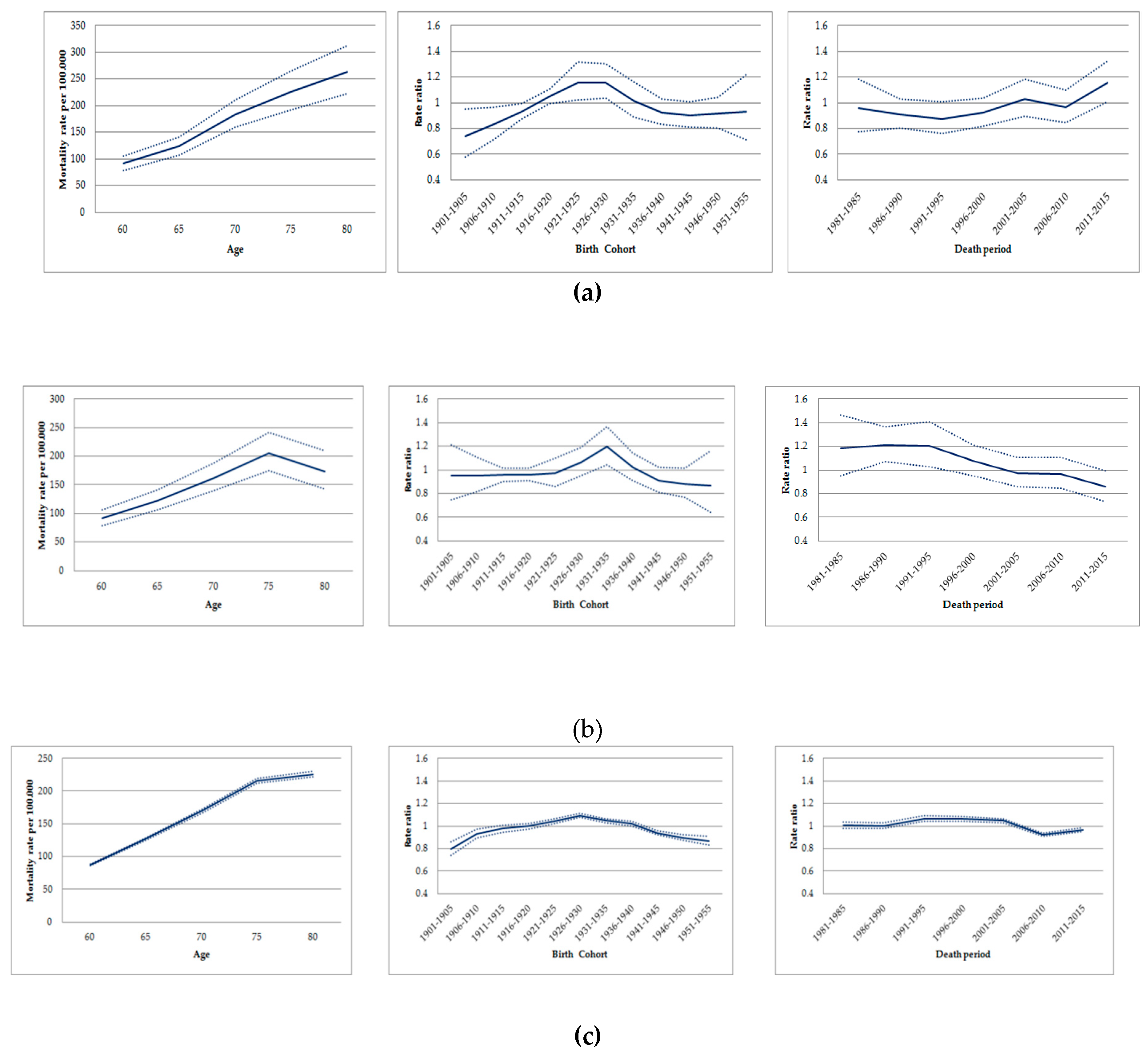
| Model | Resid | Resid | Deviance 1 | p2 |
|---|---|---|---|---|
| df | Dev | |||
| Osasco | ||||
| Age | 30 | 34.246 | ||
| Age−drift 3 | 29 | 33.273 | 0.9723 | 0.324 |
| Age−Cohort | 26 | 27.554 | 5.7197 | 0.126 |
| Age−Period−Cohort | 23 | 24.646 | 2.9079 | 0.406 |
| Age−Period | 26 | 31.494 | −6.8482 | 0.076 |
| Age−drift4 | 29 | 33.273 | −1.7794 | 0.619 |
| Sorocaba | ||||
| Age | 30 | 50.262 | ||
| Age−drift 3 | 29 | 36.342 | 13.92 | <0.001 |
| Age−Cohort | 26 | 26.611 | 9.7309 | 0.020 |
| Age−Period−Cohort | 23 | 25.494 | 1.1173 | 0.772 |
| Age−Period | 26 | 32.335 | −6.8406 | 0.077 |
| Age−drift4 | 29 | 36.342 | −4.0077 | 0.26 |
| State of São Paulo | ||||
| Age | 30 | 707.23 | ||
| Age−drift 3 | 29 | 564.93 | 142.3 | <0.001 |
| Age−Cohort | 20 | 164.08 | 400.85 | <0.001 |
| Age−Period−Cohort | 15 | 40.22 | 123.86 | <0.001 |
| Age−Period | 24 | 248 | −207.77 | <0.001 |
| Age−drift 4 | 29 | 564.93 | −316.93 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, G.A.; Algranti, E.; Conceição, G.M.d.S.; Wünsch Filho, V.; Toporcov, T.N. Lung Cancer Mortality Trends in a Brazilian City with a Long History of Asbestos Consumption. Int. J. Environ. Res. Public Health 2019, 16, 2548. https://doi.org/10.3390/ijerph16142548
Fernandes GA, Algranti E, Conceição GMdS, Wünsch Filho V, Toporcov TN. Lung Cancer Mortality Trends in a Brazilian City with a Long History of Asbestos Consumption. International Journal of Environmental Research and Public Health. 2019; 16(14):2548. https://doi.org/10.3390/ijerph16142548
Chicago/Turabian StyleFernandes, Gisele Aparecida, Eduardo Algranti, Gleice Margarete de Souza Conceição, Victor Wünsch Filho, and Tatiana Natasha Toporcov. 2019. "Lung Cancer Mortality Trends in a Brazilian City with a Long History of Asbestos Consumption" International Journal of Environmental Research and Public Health 16, no. 14: 2548. https://doi.org/10.3390/ijerph16142548
APA StyleFernandes, G. A., Algranti, E., Conceição, G. M. d. S., Wünsch Filho, V., & Toporcov, T. N. (2019). Lung Cancer Mortality Trends in a Brazilian City with a Long History of Asbestos Consumption. International Journal of Environmental Research and Public Health, 16(14), 2548. https://doi.org/10.3390/ijerph16142548





