Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Procedures and Informed Consent
2.2. Study Design and Participants
2.3. Dentifrices
2.4. Assessments
- No white spot formation
- Slight white spot formation (thin rim)
- Excessive white spot formation (thicker bands)
- White spot formation with cavitation
2.5. Questionnaire Design
2.6. Trial Flow
2.7. Statistical Analyses
3. Results
3.1. General Description
3.2. Clinical Measurements
3.3. Questionnaires
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Talic, N.F. Adverse effects of orthodontic treatment: A clinical perspective. Saudi Dent. J. 2011, 23, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Pleszczyńska, M.; Wiater, A.; Bachanek, T.; Szczodrak, J. Enzymes in therapy of biofilm-related oral diseases. Biotechnol. Appl. Biochem. 2017, 64, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Ullah, R.; Zafar, M.S.; Shahani, N. Potential fluoride toxicity from oral medicaments: A review. Iran. J. Basic Med. Sci. 2017, 20, 841–848. [Google Scholar] [PubMed]
- Addy, M. Chlorhexidine compared with other locally delivered antimicrobials. A short review. J. Clin. Periodontol. 1986, 13, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Grassi, T.F.; Camargo, E.A.; Salvadori, D.M.; Marques, M.E.; Ribeiro, D.A. DNA damage in multiple organs after exposure to chlorhexidine in Wistar rats. Int. J. Hyg. Environ. Health 2007, 210, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Rotgans, J.; Hoogendoorn, H. The effect of toothbrushing with a toothpaste containing amyloglucosidase and glucose oxidase on plaque accumulation and gingivitis. Caries Res. 1979, 13, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Midda, M.; Cooksey, M.W. Clinical uses of an enzyme-containing dentifrice. J. Clin. Periodontol. 1986, 13, 950–956. [Google Scholar] [CrossRef]
- Jose, J.E.; Padmanabhan, S.; Chitharanjan, A.B. Systemic consumption of probiotic curd and use of probiotic toothpaste to reduce Streptococcus mutans in plaque around orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 67–72. [Google Scholar] [CrossRef]
- Hannah, J.J.; J.ohnson, J.D.; Kuftinec, M.M. Long-term clinical evaluation of toothpaste and oral rinse containing sanguinaria extract in controlling plaque, gingival inflammation, and sulcular bleeding during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 199–207. [Google Scholar] [CrossRef]
- Kawarai, T.; Narisawa, N.; Yoneda, S.; Tsutsumi, Y.; Ishikawa, J.; Hoshino, Y.; Senpuku, H. Inhibition of Streptococcus mutans biofilm formation using extracts from Assam tea compared to green tea. Arch. Oral Biol. 2016, 68, 73–82. [Google Scholar] [CrossRef]
- Lenander-Lumikari, M.; Loimaranta, V. Saliva and dental caries. Adv. Dent. Res. 2000, 14, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.E.; Arnold, D.; Murphy, B.; Carroll, P.; Green, A.K.; Smith, A.M.; Marsh, P.D.; Chen, T.; Marriott, R.E.; Brading, M.G. A randomised clinical study to determine the effect of a toothpaste containing enzymes and proteins on plaque oral microbiome ecology. Sci. Rep. 2017, 7, 43344. [Google Scholar] [CrossRef] [PubMed]
- Lenander-Lumikari, M.; Tenovuo, J.; Mikola, H. Effects of a lactoperoxidase system-containing toothpaste on levels of hypothiocyanite and bacteria in saliva. Caries Res. 1993, 27, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Etemadzadeh, H.; Ainamo, J.; Murtomaa, H. Plaque growth-inhibiting effects of an abrasive fluoride-chlorhexidine toothpaste and a fluoride toothpaste containing oxidative enzymes. J. Clin. Periodontol. 1985, 12, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Moran, J.; Addy, M.; Newcombe, R. Comparison of the effect of toothpastes containing enzymes or antimicrobial compounds with a conventional fluoride toothpaste on the development of plaque and gingivitis. J. Clin. Periodontol. 1989, 16, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Øgaard, B.; Alm, A.A.; Larsson, E.; Adolfsson, U. A prospective, randomized clinical study on the effects of an amine fluoride/stannous fluoride toothpaste/mouthrinse on plaque, gingivitis and initial caries lesion development in orthodontic patients. Eur. J. Orthod. 2006, 28, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.A.; Ripa, L.W. Effects of self-applied topical fluoride preparations in orthodontic patients. Angle Orthod. 2000, 70, 424–430. [Google Scholar] [PubMed]
- Madlena, M.; Banoczy, J.; Gotz, G.; Marton, S.; Kaan, M., Jr.; Nagy, G. Effects of amine and stannous fluorides on plaque accumulation and gingival health in orthodontic patients treated with fixed appliances: A pilot study. Oral Health Dent. Manag. 2012, 11, 57–61. [Google Scholar]
- Gorelick, L.; Geiger, A.M.; Gwinnett, A.J. Incidence of white spot formation after bonding and banding. Am. J. Orthod. 1982, 81, 93–98. [Google Scholar] [CrossRef]
- Ainamo, J.; Bay, I. Problems and proposals for recording gingivitis and plaque. Int. Dent. J. 1975, 25, 229–235. [Google Scholar]
- Gwinnett, A.J.; Ceen, R.F. Plaque distribution on bonded brackets: A scanning microscope study. Am. J. Orthod. 1979, 75, 667–677. [Google Scholar] [CrossRef]
- Sakamaki, S.T.; Bahn, A.N. Effect of orthodontic banding on localized oral lactobacilli. J. Dent. Res. 1968, 47, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Linton, J.L. Quantitative measurements of remineralization of incipient caries. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 590–597. [Google Scholar] [CrossRef]
- O’Reilly, M.M.; Featherstone, J.D. Demineralization and remineralization around orthodontic appliances: An in vivo study. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 33–40. [Google Scholar] [CrossRef]
- Ogaard, B.; Rølla, G.; Arends, J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 68–73. [Google Scholar] [CrossRef]
- Øgaard, B. White spot lesions during orthodontic treatment: Mechanisms and fluoride preventive aspects. Semin. Orthod. 2008, 14, 183–193. [Google Scholar] [CrossRef]
- Hadler-Olsen, S.; Sandvik, K.; El-Agroudi, M.A.; Øgaard, B. The incidence of caries and white spot lesions in orthodontically treated adolescents with a comprehensive caries prophylactic regimen—A prospective study. Eur. J. Orthod. 2012, 34, 633–639. [Google Scholar] [CrossRef]
- Bergstrand, F.; Twetman, S. A review on prevention and treatment of post-orthodontic white spot lesions—Evidence-based methods and emerging technologies. Open Dent. J. 2011, 5, 158. [Google Scholar] [CrossRef]
- Benson, P.E.; Parkin, N.; Dyer, F.; Millett, D.T.; Furness, S.; Germain, P. Fluorides for the prevention of early tooth decay (demineralised white lesions) during fixed brace treatment. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef]
- Gudipaneni, R.K.; Kumar, R.V.; Jesudass, G.; Peddengatagari, S.; Duddu, Y. Short term comparative evaluation of antimicrobial efficacy of tooth paste containing lactoferrin, lysozyme, lactoperoxidase in children with severe early childhood caries: A clinical study. J. Clin. Diagn. Res. 2014, 8, ZC18. [Google Scholar] [CrossRef]
- Jordan, C.; LeBlanc, D.J. Influences of orthodontic appliances on oral populations of mutans streptococci. Oral Microbiol. Immunol. 2002, 17, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Bimstein, E.; Becker, A. Malocclusion, Orthodontic Intervention, and Gingival and Periodontal Health. In Periodontal and Gingival Health Diseases: Children, Adolescents, and Young Adults; Martin Dunitz Ltd.: London, UK, 2001. [Google Scholar]
- Moran, J.; Addy, M.; Newcombe, R. The antibacterial effect of toothpastes on the salivary flora. J. Clin. Periodontol. 1988, 15, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Moreira, S.; Llena-Puy, C.; Forner-Navarro, L.; Martínez-Canut, P.; Amengual-Lorenzo, J. Gingival bleeding reduction using a carbamide peroxide. J. Clin. Exp. Dent. 2011, 3, 452–455. [Google Scholar] [CrossRef]
- Travess, H.; Roberts-Harry, D.; Sandy, J. Orthodontics. Part 6: Risks in orthodontic treatment. Br. Dent. J. 2004, 196, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Tenovuo, J. Clinical applications of antimicrobial host proteins lactoperoxidase, lysozyme and lactoferrin in xerostomia: Efficacy and safety. Oral Dis. 2002, 8, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Donatsky, O.; Worsaae, N.; Schiödt, M.; Johnsen, T. Effect of zendium toothpaste on recurrent aphthous stomatitis. Scand. J. Dent. Res. 1983, 91, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.A.; Kau, C.H.; English, J.D.; Lee, R.P.; Powers, J.; Nguyen, J.T. MI Paste Plus to prevent demineralization in orthodontic patients: A prospective randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 660–668. [Google Scholar] [CrossRef]
- Petti, S.; Barbato, E.; Simonetti D’Arca, A. Effect of orthodontic therapy with fixed and removable appliances on oral microbiota: A six-month longitudinal study. New Microbiol. 1997, 20, 55–56. [Google Scholar]

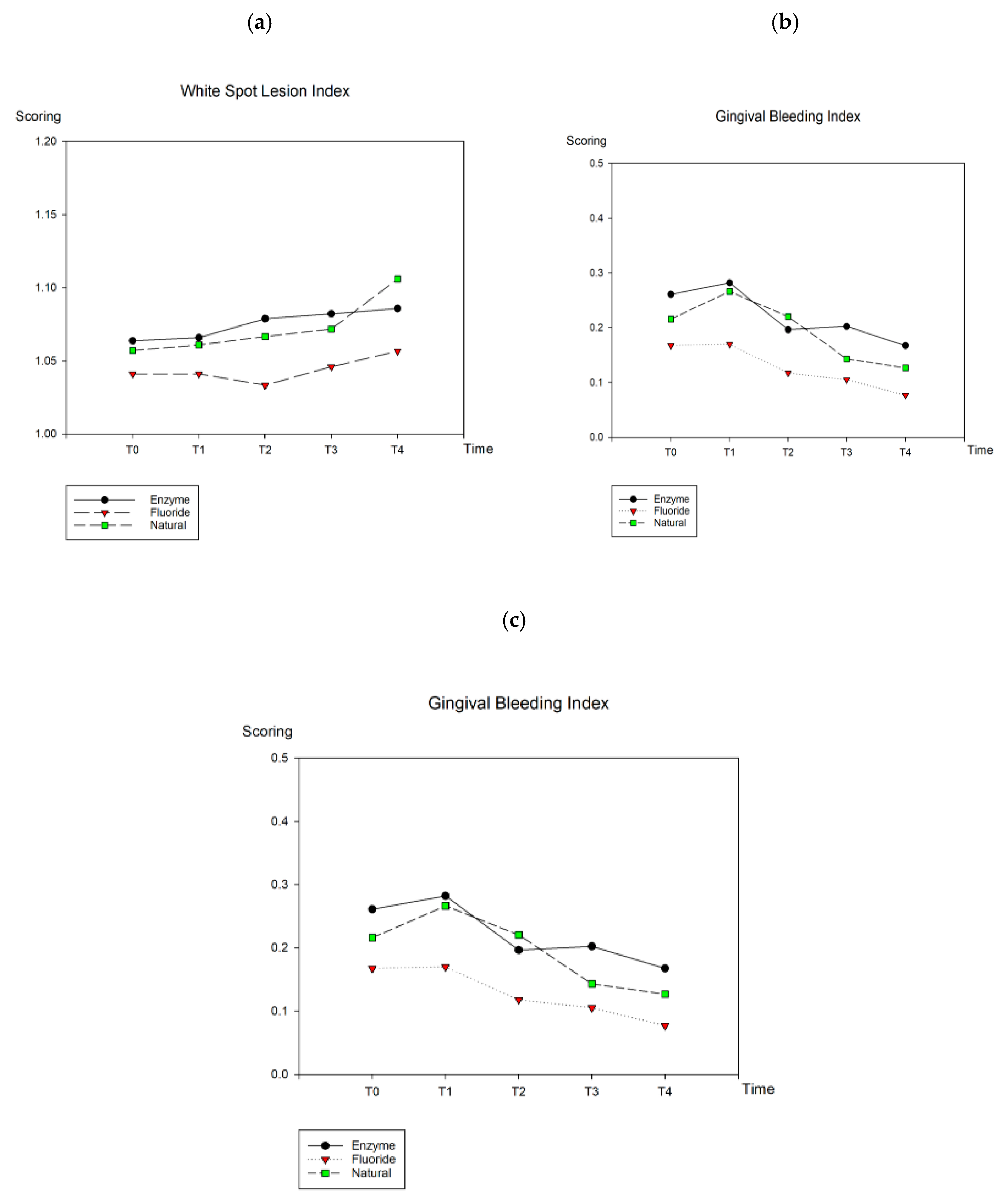
| Dentifrice | T0 | T1 | T2 | T3 | T4 | p Value |
|---|---|---|---|---|---|---|
| Enzyme | ||||||
| WSL | 1.06 ± 0.09 | 1.07 ± 0.09 | 1.08 ± 0.09 | 1.08 ± 0.09 | 1.09 ± 0.08 | NS |
| GBI | 0.26 ± 0.22 | 0.28 ± 0.27 | 0.20 ± 0.22 | 0.20 ± 0.14 | 0.17 ± 0.13 | T1–T4 * |
| VPI | 0.42 ± 0.21 | 0.37 ± 0.24 | 0.30 ± 0.22 | 0.25 ± 0.21 | 0.20 ± 0.20 | T0–T4 *; T0–T3 *; T1–T4 * |
| Fluoride | ||||||
| WSL | 1.04 ± 0.06 | 1.04 ± 0.06 | 1.03 ± 0.06 | 1.05 ± 0.07 | 1.06 ± 0.08 | NS |
| GBI | 0.17 ± 0.13 | 0.17 ± 0.17 | 0.12 ± 0.14 | 0.11 ± 0.11 | 0.08 ± 0.11 | T1–T4 *; T0–T4 * |
| VPI | 0.34 ± 0.22 | 0.32 ± 0.26 | 0.24 ± 0.21 | 0.19 ± 0.18 | 0.17 ± 0.21 | T0–T4 *; T0–T3 *; T1–T4 *; T1–T3 * |
| Natural | ||||||
| WSL | 1.06 ± 0.07 | 1.06 ± 0.07 | 1.07 ± 0.08 | 1.07 ± 0.06 | 1.11 ± 0.09 | T0–T4 * |
| GBI | 0.22 ± 0.23 | 0.27 ± 0.20 | 0.22 ± 0.19 | 0.14 ± 0.13 | 0.13 ± 0.11 | T1–T4 *; T1–T3 * |
| VPI | 0.28 ± 0.26 | 0.31 ± 0.24 | 0.26 ± 0.21 | 0.20 ± 0.17 | 0.18 ± 0.16 | NS |
| Oral Condition | Enzyme | Fluoride | Natural | Satisfaction in Improvement |
|---|---|---|---|---|
| Oral ulceration | 0.480 | 0.371 | NA 1 | 0.424 |
| Gum bleeding | 0.617 | 0.480 | NA | 0.287 |
| Tooth sensitivity | NA | NA | NA | 0.123 |
| Dry mouth | 1 | NA | 1 | 0.282 |
| Bad breath | 0.134 | 1 | NA | 0.097 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, H.-C.; Hu, H.-T.; Chang, Y.-C. Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 2243. https://doi.org/10.3390/ijerph16122243
Cheng H-C, Hu H-T, Chang Y-C. Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2019; 16(12):2243. https://doi.org/10.3390/ijerph16122243
Chicago/Turabian StyleCheng, Hsin-Chung, Hao-Ting Hu, and Ya-Chu Chang. 2019. "Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 16, no. 12: 2243. https://doi.org/10.3390/ijerph16122243
APA StyleCheng, H.-C., Hu, H.-T., & Chang, Y.-C. (2019). Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 16(12), 2243. https://doi.org/10.3390/ijerph16122243




