Association between Socioeconomic Status, Physical Health and Need for Long-Term Care among the Chinese Elderly
Abstract
1. Background
2. Methods
2.1. Introduction of Study Location
2.2. Data Collection and the Research Subjects
2.3. Measurements
2.4. Statistical Analysis Approach
2.5. Ethical Considerations
3. Results
3.1. Sample Characteristics
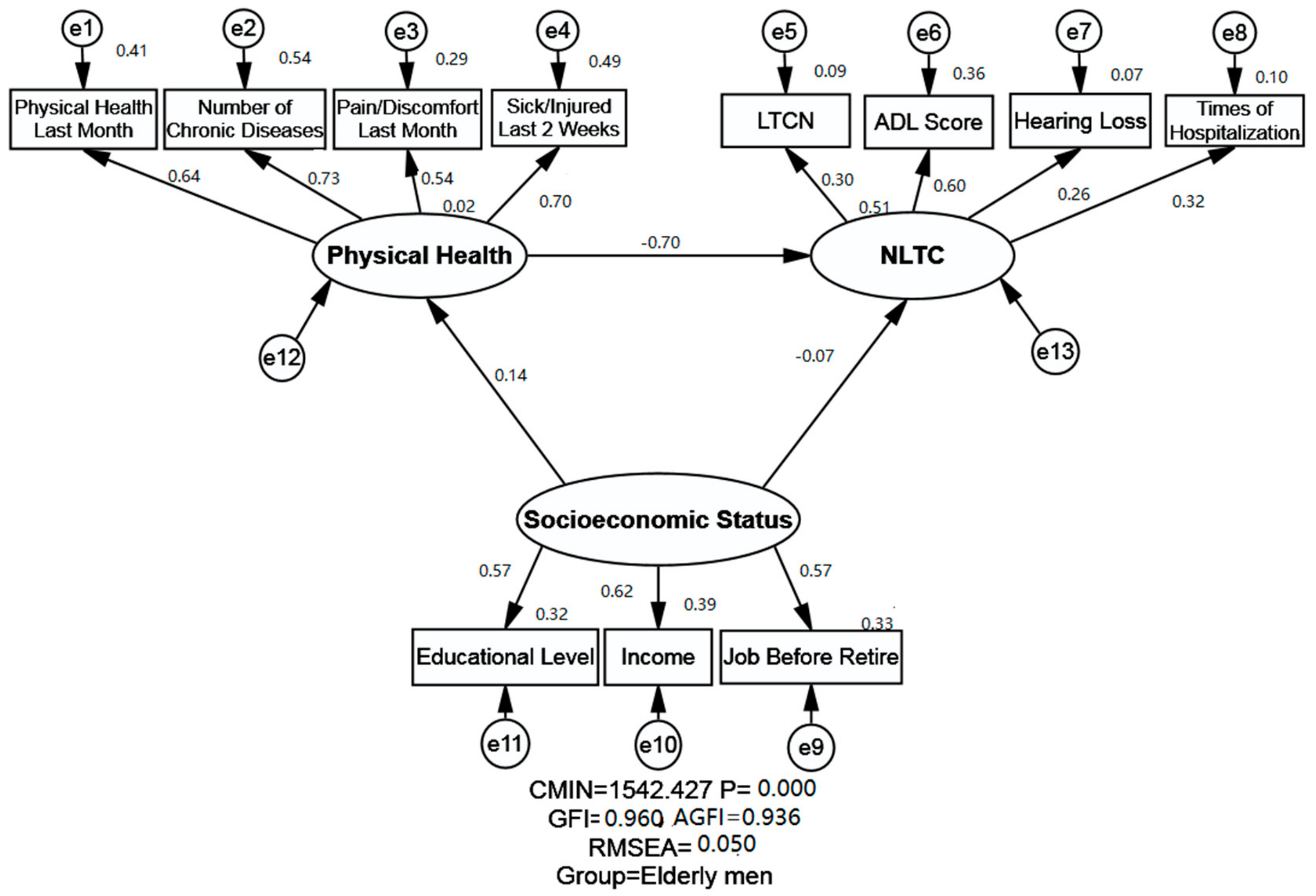
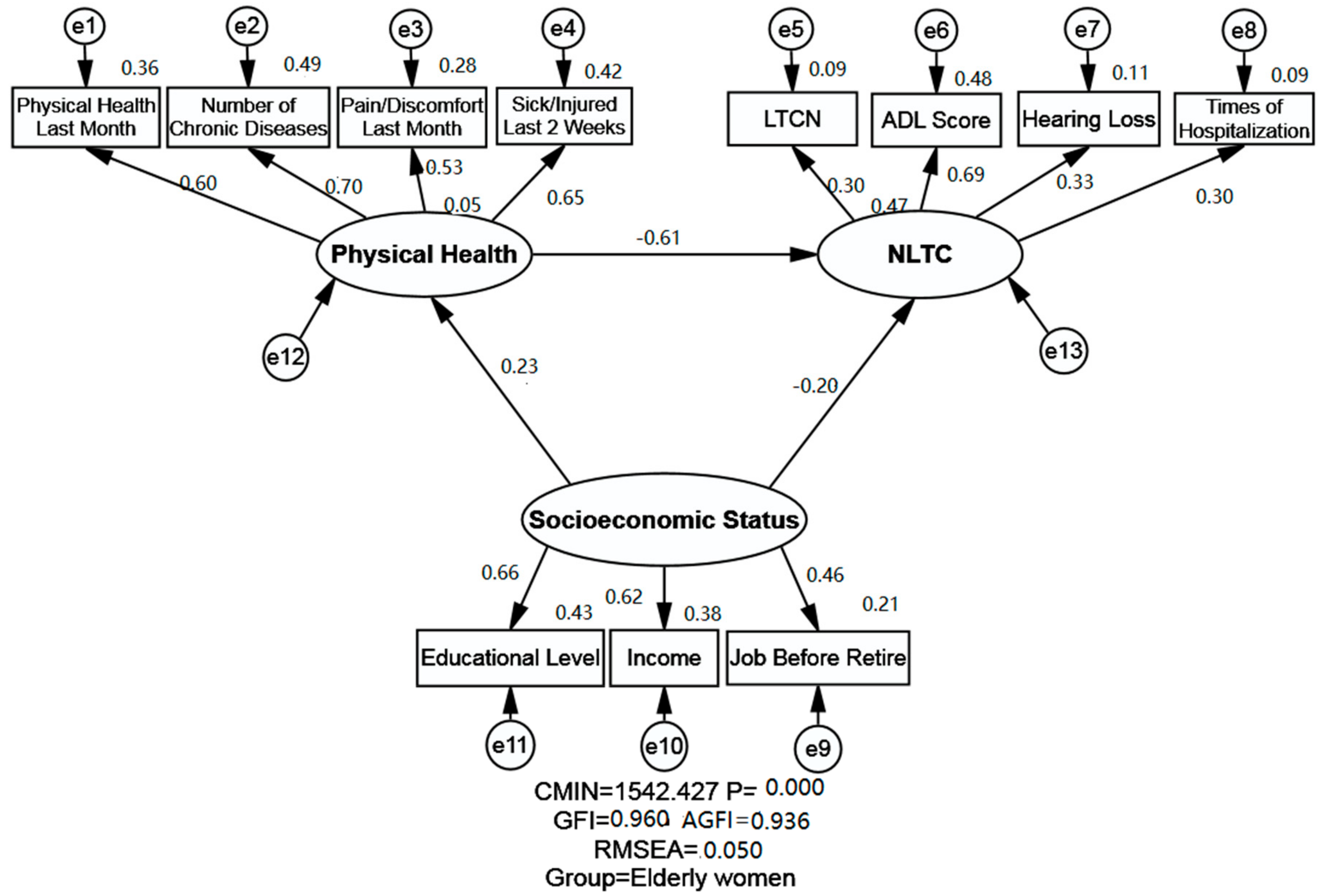
3.2. The Structural Equation Modelling Analysis
3.2.1. Measurement Invariance across the Gender
3.2.2. Model Fitness Indices
3.3. Relationship between SES, Physical Health and NLTC by Using SEM
3.3.1. Relationship between SES and NLTC
3.3.2. Relationship between Physical Health and NLTC
3.3.3. Relationship between SES and Physical Health
4. Discussion
4.1. Relationship between SES and NLTC
4.2. Relationship between Physical Health and NLTC
4.3. Relationship between SES and Physical Health
4.4. Relationship between SES, Physical Health and NLTC
4.5. Implications
4.6. Limitation and Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgement
Conflicts of Interest
References
- United Nations. World Population Prospects 2017 REVISION Volume I: Comprehensive Tables; United Nations Publications: New York, NY, USA, 2017. [Google Scholar]
- United Nations Population Fund World Population Dashboard. Available online: https://www.unfpa.org/data/world-population-dashboard (accessed on 25 April 2019).
- Population Reference Bureau 2018 World Population Data Sheet with Focus on Changing Age Structures. Available online: https://www.prb.org/2018-world-population-data-sheet-with-focus-on-changing-age-structures/ (accessed on 25 April 2019).
- National Bureau of Statistics of the People’s Republic of China Statistical Bulletin of National Economic and Social Development in 2018. Available online: http://www.gov.cn/xinwen/2019-02/28/content_5369270.htm (accessed on 25 April 2019).
- The State Council of the People’s Republic of China 241 Million Older Adults in China and Equals 17.3% of the Whole Population. Available online: http://www.gov.cn/xinwen/2018-02/26/content_5268992.htm (accessed on 8 July 2018).
- Yang, S.; Hoshi, T.; Nakayama, N.; Wang, S.; Kong, F. The effects of socio-economic status and physical health on the long-term care needs of Japanese urban elderly: A chronological study. Environ. Health Prev. Med. 2013, 18, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Fang, X.; Gao, J.; Ding, H.; Wang, C.; Xie, C.; Yang, Y.; Jin, C. Determinants of formal care use and expenses among in-home elderly in Jing’an district, Shanghai, China. PLoS ONE 2017, 12, e0176548. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Neuhaus, V.; Swellengrebel, C.H.; Bossen, J.K.; Ring, D. What are the factors influencing outcome among patients admitted to a hospital with a proximal humeral fracture? Clin. Orthop. Relat. Res. 2013, 471, 1698–1706. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kasteridis, P.; Mason, A.; Goddard, M.; Jacobs, R.; Santos, R.; Rodriguez-Sanchez, B.; McGonigal, G. Risk of care home placement following acute hospital admission: Effects of a pay-for-performance scheme for dementia. PLoS ONE 2016, 11, e0155850. [Google Scholar] [CrossRef]
- Hsu, C.Y.; Moyle, W.; Cooke, M.; Jones, C. Seated Tai Chi versus usual activities in older people using wheelchairs: A randomized controlled trial. Complement. Ther. Med. 2016, 24, 1–6. [Google Scholar] [CrossRef]
- Kuan, S.C.; Chen, K.M.; Wang, C. Effectiveness of Qigong in promoting the health of wheelchair-bound older adults in long-term care facilities. Biol. Res. Nurs. 2012, 14, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.; Xu, L.; Kong, M.; Li, S.; Zhou, C.; Li, J.; Sun, L.; Qin, W. The relationship between socioeconomic status, mental health, and need for long-term services and supports among the Chinese Elderly in Shandong Province—A cross-sectional study. Int. J. Environ. Res. Public Health 2019, 16, 526. [Google Scholar] [CrossRef]
- Hoi le, V.; Thang, P.; Lindholm, L. Elderly care in daily living in rural Vietnam: Need and its socioeconomic determinants. BMC Geriatr. 2011, 11, 81. [Google Scholar] [CrossRef]
- Hong, M.; Hong, S.; Kim, M.H.; Yi, E.H. Intention to use long-term care facilities: Differences beween Korean pre-elderly and Korean baby-boomers. J. Cross Cult. Gerontol. 2016, 31, 357–368. [Google Scholar] [CrossRef]
- Hamada, S.; Takahashi, H.; Sakata, N.; Jeon, B.; Mori, T.; Iijima, K.; Yoshie, S.; Ishizaki, T.; Tamiya, N. Household income relationship with health services utilization and healthcare expenditures in people aged 75 years or older in Japan: A population-based study using medical and long-term care insurance claims data. J. Epidemiol. 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Enroth, L.; Aaltonen, M.; Raitanen, J.; Nosraty, L.; Jylha, M. Does use of long-term care differ between occupational classes among the oldest old? Vitality 90+ study. Eur. J. Ageing 2018, 15, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Andrade, T.B.; Andrade, F.B. Unmet need for assistance with activities of daily life among older adults in Brazil. Revista De Saude Publica 2018, 52, 75. [Google Scholar] [CrossRef]
- Turner, R.J.; Brown, T.N.; Hale, W.B. Race, socioeconomic position, and physical health: A descriptive analysis. J. Health Soc. Behav. 2017, 58, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Bennett, K.K.; Buchanan, D.M.; Jones, P.G.; Spertus, J.A. Socioeconomic status, cognitive-emotional factors, and health status following myocardial infarction: Testing the reserve capacity model. J. Behav. Med. 2015, 38, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Michal, M.; Wiltink, J.; Kirschner, Y.; Schneider, A.; Wild, P.S.; Munzel, T.; Blettner, M.; Schulz, A.; Lackner, K.; Pfeiffer, N.; et al. Complaints of sleep disturbances are associated with cardiovascular disease: Results from the Gutenberg health study. PLoS ONE 2014, 9, e104324. [Google Scholar] [CrossRef] [PubMed]
- Galili, S.F.; Bech, B.H.; Vestergaard, C.; Fenger-Gron, M.; Christensen, J.; Vestergaard, M.; Ahrensberg, J. Use of general practice before and after mild traumatic brain injury: A nationwide population-based cohort study in Denmark. BMJ Open 2017, 7, e017735. [Google Scholar] [CrossRef] [PubMed]
- Pasco, J.A.; Holloway, K.L.; Stuart, A.L.; Williams, L.J.; Brennan-Olsen, S.L.; Berk, M. The subjective wellbeing profile of the ‘pretiree’ demographic: A cross-sectional study. Maturitas 2018, 110, 111–117. [Google Scholar] [CrossRef]
- Jesus-Moraleida, F.R.; Ferreira, P.H.; Ferreira, M.L.; Silva, J.P.D.; Assis, M.G.; Pereira, L.S.M. The Brazilian back complaints in the elders (Brazilian BACE) study: Characteristics of Brazilian older adults with a new episode of low back pain. Braz. J. Phys. Ther. 2018, 22, 55–63. [Google Scholar] [CrossRef]
- Schiotz, M.L.; Stockmarr, A.; Host, D.; Glumer, C.; Frolich, A. Social disparities in the prevalence of multimorbidity—A register-based population study. BMC Public Health 2017, 17, 422. [Google Scholar] [CrossRef]
- Tchicaya, A.; Lorentz, N. Socioeconomic inequalities in health-related quality of life between men and women, 5 years after a coronary angiography. Health Qual. Life Outcomes 2016, 14, 165. [Google Scholar] [CrossRef]
- Wham, C.A.; Teh, R.; Moyes, S.; Dyall, L.; Kepa, M.; Hayman, K.; Kerse, N. Health and social factors associated with nutrition risk: Results from life and living in advanced age: A cohort study in New Zealand (LiLACS NZ). J. Nutr. Health Aging 2015, 19, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Nagamine, Y.; Kondo, N.; Yokobayashi, K.; Ota, A.; Miyaguni, Y.; Sasaki, Y.; Tani, Y.; Kondo, K. Socioeconomic disparity in the prevalence of objectively evaluated diabetes among older Japanese adults: JAGES cross-sectional data in 2010. J. Epidemiol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Elfassy, T.; Grasset, L.; Glymour, M.M.; Swift, S.; Zhang, L.; Howard, G.; Howard, V.J.; Flaherty, M.; Rundek, T.; Osypuk, T.L.; et al. Sociodemographic disparities in long-term mortality among stroke survivors in the United States. Stroke 2019, 50, 805–812. [Google Scholar] [CrossRef] [PubMed]
- McCormack, G.R.; Friedenreich, C.; McLaren, L.; Potestio, M.; Sandalack, B.; Csizmadi, I. Interactions between neighbourhood urban form and socioeconomic status and their associations with anthropometric measurements in Canadian adults. J. Environ. Public Health 2017, 2017, 5042614. [Google Scholar] [CrossRef] [PubMed]
- Zahodne, L.B.; Kraal, A.Z.; Zaheed, A.; Sol, K. Subjective social status predicts late-life memory trajectories through both mental and physical health pathways. Gerontology 2018, 64, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Shandong Provincial Office of Local Chronicles the General Information about Shandong Province. Available online: http://www.sdsqw.cn/overview/2016gk/2017/1116/38480.html (accessed on 7 June 2018).
- Shandong Provincial Bureau of Statistics Statistical Bulletin of Shandong Provincial National Economic and Social Development in 2019. Available online: http://www.shandong.gov.cn/art/2019/3/2/art_2531_18021.html (accessed on 22 April 2019).
- People’s Government of Shandong Province Population Aging and Social Welfare Development for the Elderly of Shandong Province. Available online: http://www.shandong.gov.cn/art/2018/5/24/art_2056_156435.html (accessed on 28 May 2019).
- Raoufi, A.M.; Tang, X.; Jing, Z.; Zhang, X.; Xu, Q.; Zhou, C. Blood glucose monitoring and its determinants in diabetic patients: A cross-sectional study in Shandong, China. Diabetes Ther. Res. Treat. Educ. Diabetes Relat. Disord. 2018, 9, 2055–2066. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Zhou, C. Association between body mass index and suicidal ideation among seniors in Shandong, China. Compr. Psychiatry 2018, 82, 68–72. [Google Scholar] [CrossRef]
- Andrew, M.K. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 7th ed.; W.B. Saunders: Philadelphia, PA, USA, 2010; p. 198. [Google Scholar]
- Winters-Miner, L.A.; Bolding, P.S.; Hilbe, J.M.; Goldstein, M.; Hill, T.; Nisbet, R.; Walton, N.; Miner, G.D. Practical Predictive Analytics and Decisioning Systems for Medicine; Academic Press: Cambridge, MA, USA, 2015; pp. 176–204. [Google Scholar]
- Cutler, D.; Lleras-Muney, A.; Vogl, T. Socioeconomic Status and Health: Dimensions and Mechanisms; National Bureau of Economic Research: Cambridge, MA, USA, 2008. [Google Scholar]
- Lantz, P.M.; House, J.S.; Lepkowski, J.M.; Williams, D.R.; Mero, R.P.; Chen, J. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of us adults. JAMA 1998, 279, 1703–1708. [Google Scholar] [CrossRef]
- Wilkinson, R.G. Income distribution and mortality: A ‘natural’ experiment. Sociol. Health Illn. 1990, 12, 391–412. [Google Scholar] [CrossRef]
- Laszlo, K.D.; Pikhart, H.; Kopp, M.S.; Bobak, M.; Pajak, A.; Malyutina, S.; Salavecz, G.; Marmot, M. Job insecurity and health: A study of 16 European countries. Soc. Sci. Med. (1982) 2010, 70, 867–874. [Google Scholar] [CrossRef]
- Moulin, J.J.; Labbe, E.; Sass, C.; Gerbaud, L. Job insecurity, unemployment and health: Results from the health examination centers of the French general health insurance. Rev. Epidemiol. Sante Publique 2009, 57, 141–149. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, R.M.; Strazdins, L.; Lim, L.L.; Broom, D.H.; Rodgers, B. Work and health in a contemporary society: Demands, control, and insecurity. J. Epidemiol. Community Health 2003, 57, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Coenen, P.; Huysmans, M.A.; Holtermann, A.; Krause, N.; van Mechelen, W.; Straker, L.M.; van der Beek, A.J. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br. J. Sports Med. 2018, 52, 1320. [Google Scholar] [CrossRef] [PubMed]
- Engage Education Foundation Dimensions of Health. Available online: http://wiki.engageeducation.org.au/health-and-human-development/unit-3/area-of-study-1-understanding-australias-health/dimensions-of-health/ (accessed on 25 April 2019).
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Chen, F.F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Andersen, E.B.; Laake, P.; Cox, D.; Schweder, T. Analysis of covariance structures [with discussion and reply]. Scand. J. Stat. 1981, 8, 65–92. [Google Scholar]
- Fan, X.; Thompson, B.; Wang, L. Effects of sample size, estimation methods, and model specification on structural equation modeling fit indexes. Struct. Equ. Model. Multidiscip. J. 1999, 6, 56–83. [Google Scholar] [CrossRef]
- Rong, T. Amos and Research Method, 2nd ed.; Chongqing University Press: Chongqing, China, 2010. [Google Scholar]
- Laporte, A.; Croxford, R.; Coyte, P.C. Can a publicly funded home care system successfully allocate service based on perceived need rather than socioeconomic status? A Canadian experience. Health Soc. Care Community 2007, 15, 108–119. [Google Scholar] [CrossRef]
- Kong, F.L.; Hoshi, T.; Ai, B.; Shi, Z.M.; Nakayama, N.; Wang, S.; Yang, S.W. Association between socioeconomic status (SES), mental health and need for long-term care (NLTC)—A longitudinal study among the Japanese elderly. Arch. Gerontol. Geriatr. 2014, 59, 372–381. [Google Scholar] [CrossRef]
- McKevitt, C.; Fudge, N.; Redfern, J.; Sheldenkar, A.; Crichton, S.; Rudd, A.R.; Forster, A.; Young, J.; Nazareth, I.; Silver, L.E.; et al. Self-reported long-term needs after stroke. Stroke 2011, 42, 1398–1403. [Google Scholar] [CrossRef]
- Martikainen, P.; Moustgaard, H.; Murphy, M.; Einio, E.K.; Koskinen, S.; Martelin, T.; Noro, A. Gender, living arrangements, and social circumstances as determinants of entry into and exit from long-term institutional care at older ages: A 6-year follow-up study of older Finns. Gerontologist 2009, 49, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.; Boaz, T.; Andel, R.; DeMuth, A. Predictors of avoidable hospitalizations among assisted living residents. J. Am. Med. Dir. Assoc. 2012, 13, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Bishop, N.J.; Eggum-Wilkens, N.D.; Haas, S.A.; Kronenfeld, J.J. Estimating the Co-development of cognitive decline and physical mobility limitations in older, U.S. adults. Demography 2016, 53, 337–364. [Google Scholar] [CrossRef] [PubMed]
- Amemiya, A.; Kondo, N.; Saito, J.; Saito, M.; Takagi, D.; Haseda, M.; Tani, Y.; Kondo, K. Socioeconomic status and improvement in functional ability among older adults in Japan: A longitudinal study. BMC Public Health 2019, 19, 209. [Google Scholar] [CrossRef] [PubMed]
- Daniels, N.; Kennedy, B.; Kawachi, I. Health and inequality, or, why justice is good for our health. In Public Health, Ethics, and Equity; Anand, S., Peter, F., Sen, A., Eds.; Oxford University Press: New York, NY, USA, 2004; pp. 63–91. [Google Scholar]
- Fiorillo, D.; Sabatini, F. Quality and quantity: The role of social interactions in self-reported individual health. Soc. Sci. Med. (1982) 2011, 73, 1644–1652. [Google Scholar] [CrossRef]
- Erreygers, G. A dual atkinson measure of socioeconomic inequality of health. Health Econ. 2012, 22, 466–479. [Google Scholar] [CrossRef]
- Han, W.J.; Shibusawa, T. Trajectory of physical health, cognitive status, and psychological well-being among Chinese elderly. Arch. Gerontol. Geriatr. 2015, 60, 168–177. [Google Scholar] [CrossRef]
- Lotoala, F.; Breheny, M.; Alpass, F.; Henricksen, A. Health and wellbeing of older Pacific peoples in New Zealand. N. Z. Med. J. 2014, 127, 27–39. [Google Scholar]
- Zilioli, S.; Imami, L.; Slatcher, R.B. Socioeconomic status, perceived control, diurnal cortisol, and physical symptoms: A moderated mediation model. Psychoneuroendocrinology 2017, 75, 36–43. [Google Scholar] [CrossRef]
- Kopperstad, O.; Skogen, J.C.; Sivertsen, B.; Tell, G.S.; Saether, S.M. Physical activity is independently associated with reduced mortality: 15-years follow-up of the Hordaland health study (HUSK). PLoS ONE 2017, 12, e0172932. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P. Health and social cohesion: Why care about income inequality? BMJ 1997, 314, 1037–1040. [Google Scholar] [CrossRef] [PubMed]
- Kagamimori, S.; Gaina, A.; Nasermoaddeli, A. Socioeconomic status and health in the Japanese population. Soc. Sci. Med. (1982) 2009, 68, 2152–2160. [Google Scholar] [CrossRef] [PubMed]
- Jensen, R.T. Socioeconomic status, nutrition, and health among the elderly. In Perspectives on the Economics of Aging; University of Chicago Press: Chicago, IL, USA, 2004; pp. 313–332. [Google Scholar]
- Jianqun Tao, B.H.; Hongyuan, G. The first village doctor is a new attempt to reduce the poverty. People’s Trib. 2018, 15, 104–106. [Google Scholar]
- People’s Government of Shandong Province Working Programme for Establishing a National Model Province on the Integration of Medical and Nursing Care. Available online: http://www.shandong.gov.cn/art/2018/2/27/art_2267_17519.html (accessed on 28 May 2019).
- Shiue, I. Assessing quality of life in Welsh carers with and without back pain. Br. J. Community Nurs. 2015, 20, 338–343. [Google Scholar] [CrossRef]
- Chen, Y.M. Perceived barriers to physical activity among older adults residing in long-term care institutions. J. Clin. Nurs. 2010, 19, 432–439. [Google Scholar] [CrossRef]
- Arai, Y.; Zarit, S.H. Exploring strategies to alleviate caregiver burden: Effects of the national long-term care insurance scheme in Japan. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2011, 11, 183–189. [Google Scholar] [CrossRef]
- World Health Organization. Constitution of the World Health Organization; World Health Organization: Geneva, Switzerland, 1948. [Google Scholar]
| Variables | Definition | Measurements | Options |
|---|---|---|---|
| Socioeconomic Status | A broad concept that compositely assess an individual’s economic and sociological position in relation to others | Education | (1) Illiteracy, (2) Graduate from Elementary School, (3) Graduate from Junior Middle School, (4) Graduate from Senior Middle School and above |
| Annual income | (1) less than 2200 RMB (USD = 326), (2) from 2201 to 3300 RMB (USD = 489), (3) from 3301 to 6200 RMB (USD = 919), (4) from 6201 to 21400 RMB (USD = 3170), (5) more than 21400 RMB (USD = 3170). | ||
| Job before retire | (1) Professionals/ technical, (2) Leaders of government/ public institution, (3) Clerks or staff, (4) Businessman/ commercial servants, (5) Farming/ forestry/ fishing industry, (6) Transportation industry/ manual workers, (7) Privately/ individually-owned business, (8) Other jobs. | ||
| Physical Health | The efficient functioning of the body and its systems, and includes physical capacity to perform tasks and physical fitness. | How was your physical health status last month (physical health last month)? | (1) Very bad (2) Fairly bad (3) Moderately (4) Fairly good (5) Very good |
| How many chronic diseases did you have during the last six months (number of chronic diseases)? | (1) 0 (2) 1 (3) 2 (4) 3 (5) ≥4 | ||
| Did you pain or discomfort last month (pain/discomfort)? | (1) None (2) Moderate (3) Very painful/uncomfortable | ||
| Were you sick or injured during the last two weeks (sick/injured last 2 weeks) | (1) No (2) Yes | ||
| Need for long-term care | A person/environment interaction variable reflecting the individual’s physical and cognitive functioning and/or complex medical needs and the availability of household amenities and informal supports to cope with these barriers to daily living. | Long-term care needs | (1) Not needed (2) Needed |
| ADL Score | (1) 14 (2) 15 (3) 16 (4) 17 (5) 18–27 (6) ≥28 | ||
| Times of Hospitalization | (1) 0 (2) 1 (3) ≥2 | ||
| Hearing Loss | (1) Normal (2) Hearing function declined (3) Deaf |
| Variable | LTCN | ||||||
|---|---|---|---|---|---|---|---|
| Need (n = 302) | No Need (n = 6768) | Total (n = 7070) | χ2 Test | ||||
| n | % | n | % | n | % | ||
| Gender | |||||||
| Male | 124 | 4.4% | 2722 | 95.6% | 2846 | 100.0% | 0.085 p = 0.771 |
| Female | 178 | 4.2% | 4046 | 95.8% | 4224 | 100.0% | |
| Age | |||||||
| 60–64 | 57 | 3.6% | 1520 | 96.4% | 1577 | 100.0% | 31.767 p < 0.001 |
| 65–69 | 69 | 3.2% | 2060 | 96.8% | 2129 | 100.0% | |
| 70–74 | 69 | 3.9% | 1711 | 96.1% | 1780 | 100.0% | |
| >75 | 107 | 6.8% | 1477 | 93.2% | 1584 | 100.0% | |
| Variable | Gender | χ2 Test | |||||
|---|---|---|---|---|---|---|---|
| Men (n = 2846) | Women (n = 4224) | Total (n = 7070) | |||||
| n | % | n | % | n | % | ||
| Educational Level (graduated from) | |||||||
| Illiteracy | 491 | 21.6% | 1779 | 78.4% | 2270 | 100.0% | 561.142 p < 0.001 |
| Elementary School | 1294 | 44.3% | 1630 | 55.7% | 2924 | 100.0% | |
| Junior Middle School | 718 | 54.6% | 597 | 45.4% | 1315 | 100.0% | |
| Senior Middle School and above | 343 | 61.1% | 218 | 38.9% | 561 | 100.0% | |
| Income (RMB per year) | |||||||
| 0–2200 | 505 | 30.0% | 1180 | 70.0% | 1685 | 100.0% | 117.736 p < 0.001 |
| 2201–3300 | 439 | 38.1% | 714 | 61.9% | 1153 | 100.0% | |
| 3301–6200 | 607 | 43.2% | 797 | 56.8% | 1404 | 100.0% | |
| 6201–21,400 | 652 | 46.1% | 762 | 53.9% | 1414 | 100.0% | |
| >21,400 | 643 | 45.5% | 771 | 54.5% | 1414 | 100.0% | |
| Job Before Retire | |||||||
| Professionals/technical | 243 | 55.0% | 199 | 45.0% | 442 | 100.0% | 121.792 p < 0.001 |
| Leaders of government/public institution | 111 | 61.7% | 69 | 38.3% | 180 | 100.0% | |
| Clerks or staff | 87 | 53.0% | 77 | 47.0% | 164 | 100.0% | |
| Businessman/ commercial servants | 28 | 24.1% | 88 | 75.9% | 116 | 100.0% | |
| Farming/forestry/fishing industry | 2107 | 38.5% | 3372 | 61.5% | 5479 | 100.0% | |
| Transportation industry/manual workers | 174 | 45.4% | 209 | 54.6% | 383 | 100.0% | |
| Privately/individually-owned business | 14 | 43.8% | 18 | 56.3% | 32 | 100.0% | |
| Other jobs | 82 | 29.9% | 192 | 70.1% | 274 | 100.0% | |
| Physical Health Last Month | |||||||
| Very bad | 39 | 47.6% | 43 | 52.4% | 82 | 100.0% | 42.948 p < 0.001 |
| Fairly bad | 275 | 38.4% | 441 | 61.6% | 716 | 100.0% | |
| Moderate | 578 | 34.9% | 1079 | 65.1% | 1657 | 100.0% | |
| Fairly good | 1126 | 40.3% | 1666 | 59.7% | 2792 | 100.0% | |
| Very good | 828 | 45.4% | 995 | 54.6% | 1823 | 100.0% | |
| Number of Chronic Diseases | |||||||
| 0 | 1022 | 46.5% | 1178 | 53.5% | 2200 | 100.0% | |
| 1 | 1015 | 40.0% | 1522 | 60.0% | 2537 | 100.0% | 74.537 |
| 2 | 602 | 36.6% | 1045 | 63.4% | 1647 | 100.0% | p < 0.001 |
| 3 | 161 | 29.3% | 389 | 70.7% | 550 | 100.0% | |
| ≥4 | 46 | 33.8% | 90 | 66.2% | 136 | 100.0% | |
| Pain/Discomfort | |||||||
| None | 1685 | 45.0% | 2062 | 55.0% | 3747 | 100.0% | |
| Moderate | 1098 | 34.9% | 2048 | 65.1% | 3146 | 100.0% | 73.716 |
| Very painful/uncomfortable | 63 | 35.6% | 114 | 64.4% | 177 | 100.0% | p < 0.001 |
| Sick/Injured Last 2 Weeks | |||||||
| No | 188 | 46.4% | 1373 | 53.6% | 2561 | 100.0% | 62.813 |
| Yes | 1658 | 36.8% | 2851 | 63.2% | 4509 | 100.0% | p < 0.001 |
| LTCN | |||||||
| Not needed | 2722 | 40.2% | 4046 | 59.8% | 6768 | 100.0% | 0.085 p = 0.771 |
| Needed | 124 | 41.1% | 178 | 58.9% | 302 | 100.0% | |
| ADL Score | |||||||
| 14 | 2274 | 41.6% | 3193 | 58.4% | 5467 | 100.0% | 25.090 p < 0.001 |
| 15 | 171 | 35.5% | 311 | 64.5% | 482 | 100.0% | |
| 16 | 67 | 30.2% | 155 | 69.8% | 222 | 100.0% | |
| 17 | 70 | 34.1% | 135 | 65.9% | 205 | 100.0% | |
| 18–27 | 191 | 36.4% | 334 | 63.6% | 525 | 100.0% | |
| ≥28 | 73 | 43.2% | 96 | 56.8% | 169 | 100.0% | |
| Times of Hospitalization | |||||||
| 0 | 2332 | 40.2% | 3462 | 59.8% | 5794 | 100.0% | 0.001 |
| 1 | 401 | 40.3% | 595 | 59.7% | 996 | 100.0% | p = 0.999 |
| ≥2 | 113 | 40.4% | 167 | 59.6% | 280 | 100.0% | |
| Hearing Loss | |||||||
| Normal | 2087 | 38.5% | 3335 | 61.5% | 5422 | 100.0% | 33.453 p < 0.001 |
| Hearing function declined | 637 | 45.1% | 774 | 54.9% | 1411 | 100.0% | |
| Deaf | 122 | 51.5% | 115 | 48.5% | 237 | 100.0% | |
| Model | χ2 | d.f. | χ2/d.f. | GFI | AGFI | RMSEA | ΔRMSEA |
|---|---|---|---|---|---|---|---|
| M1 | 661.239 *** | 41 | 16.128 | 0.958 | 0.932 | 0.073 | - |
| M2 | 881.184 *** | 41 | 21.492 | 0.962 | 0.939 | 0.070 | 0.003 |
| M3 | 1542.427 *** | 82 | 18.810 | 0.960 | 0.936 | 0.050 | 0.020 |
| M4 | 1618.308 *** | 90 | 17.981 | 0.958 | 0.939 | 0.049 | 0.001 |
| M5 | 1626.370 *** | 93 | 17.488 | 0.958 | 0.941 | 0.048 | 0 |
| M6 | 1626.832 *** | 94 | 17.307 | 0.958 | 0.941 | 0.048 | 0 |
| M7 | 1632.518 *** | 96 | 17.005 | 0.958 | 0.941 | 0.048 | 0 |
| Variable | Direct | Indirect | Total | |||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| SES→NLTC | −0.066 | −0.197 *** | −0.096 | −0.139 *** | −0.162 | −0.336 *** |
| Physical Health→NLTC | −0.701 *** | −0.614 *** | - | - | −0.701 *** | −0.614 *** |
| SES→Physical Health | 0.137 *** | 0.227 *** | - | - | 0.137 *** | 0.227 *** |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, F.; Xu, L.; Kong, M.; Li, S.; Zhou, C.; Zhang, J.; Ai, B. Association between Socioeconomic Status, Physical Health and Need for Long-Term Care among the Chinese Elderly. Int. J. Environ. Res. Public Health 2019, 16, 2124. https://doi.org/10.3390/ijerph16122124
Kong F, Xu L, Kong M, Li S, Zhou C, Zhang J, Ai B. Association between Socioeconomic Status, Physical Health and Need for Long-Term Care among the Chinese Elderly. International Journal of Environmental Research and Public Health. 2019; 16(12):2124. https://doi.org/10.3390/ijerph16122124
Chicago/Turabian StyleKong, Fanlei, Lingzhong Xu, Mei Kong, Shixue Li, Chengchao Zhou, Jianghua Zhang, and Bin Ai. 2019. "Association between Socioeconomic Status, Physical Health and Need for Long-Term Care among the Chinese Elderly" International Journal of Environmental Research and Public Health 16, no. 12: 2124. https://doi.org/10.3390/ijerph16122124
APA StyleKong, F., Xu, L., Kong, M., Li, S., Zhou, C., Zhang, J., & Ai, B. (2019). Association between Socioeconomic Status, Physical Health and Need for Long-Term Care among the Chinese Elderly. International Journal of Environmental Research and Public Health, 16(12), 2124. https://doi.org/10.3390/ijerph16122124






