Oral Health Beliefs, Attitudes, and Practices of South Asian Migrants: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Data Extraction
2.4. Assessment of Quality
3. Results
3.1. Quality Assessment
3.2. Synthesis of Qualitative Studies
3.2.1. Design and Setting
3.2.2. Oral Health Knowledge
3.2.3. Oral Health Attitudes and Practices
3.3. Synthesis of Quantitative Studies
3.3.1. Design and Setting
3.3.2. Oral Health Knowledge
3.3.3. Oral Health Attitude
3.3.4. Oral Health Behaviors/Practices
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Section/Topic | # | Checklist Item | Reported on Page # |
|---|---|---|---|
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 1 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 1 and 2 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 2 |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. | 2 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 2 and 3 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 2 and 3 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 2 and 3 |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 2 and 3 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 3 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 3 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 3 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | 3 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | - |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | 3 and 4 |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | - |
| Results | |||
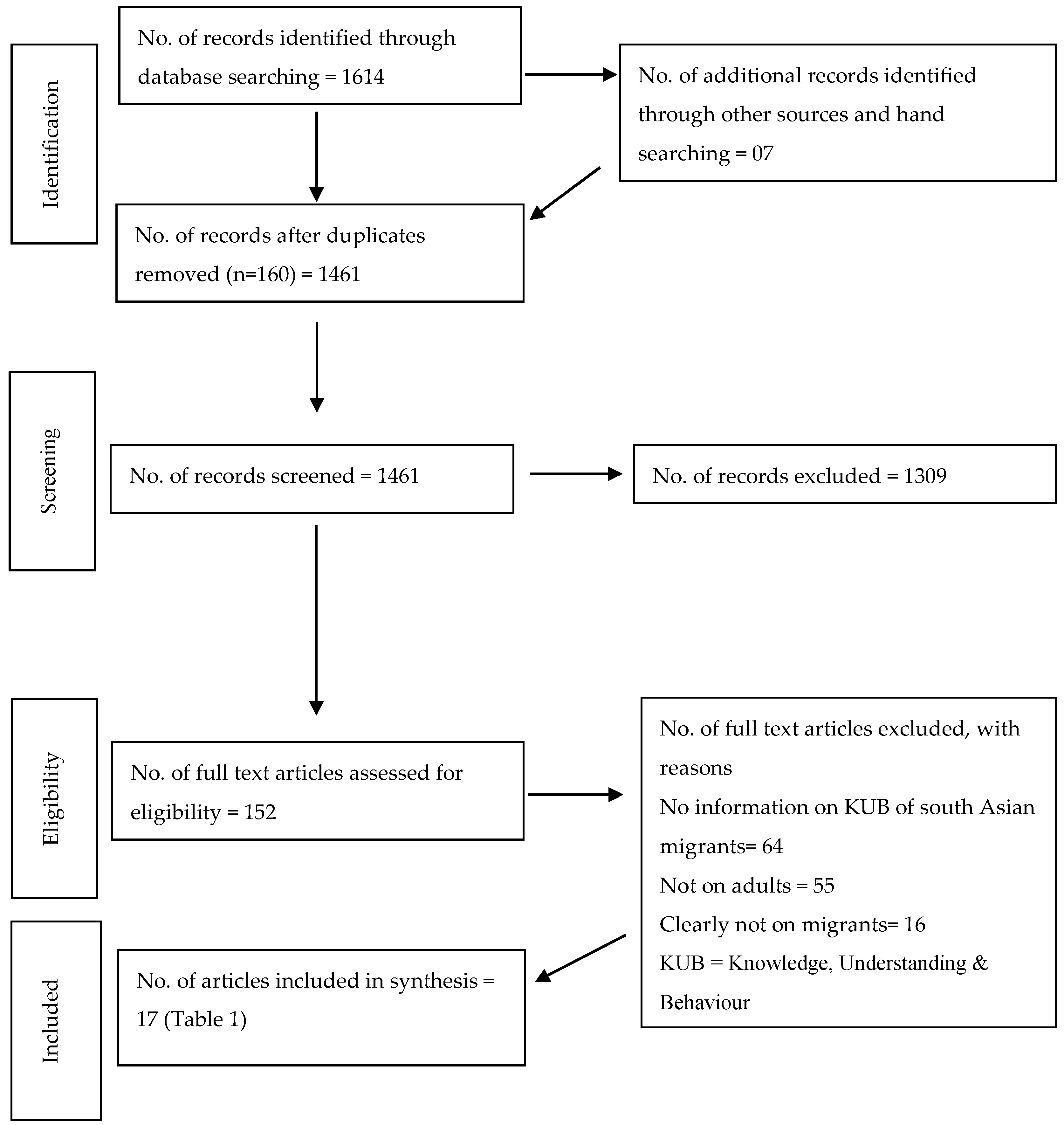
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | 4 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | 6–9, 10–16 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | 20 and 21 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present for each study: (a) simple summary data for each intervention group and (b) effect estimates and confidence intervals, ideally with a forest plot. | 6–9, 10–16 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | 10,16 |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see item 15). | 20 and 21 |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression (see item 16)). | - |
| Discussion | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). | 17–18 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | 19 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 19 |
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | 19 |
| Study Assessment Question | Williams and Gelbier [24] | Newton et al. [25] | Croucher and Sohanpal [23] | Riggs et al. [14] | Lamb et al. [15] |
|---|---|---|---|---|---|
| Research design | |||||
| 1. Are the study’s purpose and research aims clearly stated? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 2. Are the qualitative methods of inquiry appropriate for the study aims? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 3. Did the authors discuss why they decided to use qualitative methods? | No (0) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| Sampling | |||||
| 4. Is participant selection clearly described and appropriate? | Yes (1) | No (0) | Yes (1) | Yes (1) | Yes (1) |
| 5. Is the sample size discussed and justified? | No (0) | No (0) | No (0) | No (0) | No (0) |
| Data collection | |||||
| 6. Are data collection methods clearly described and justified? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 7. Are the methods appropriate given the study aims and research questions? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| Data analysis | |||||
| 8. Is the analytic process clearly described? | No (0) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 9. Were all relevant data taken into account? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 10. Did the authors consider/discuss contradictory evidence and data? | No (0) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 11. Did the study include triangulation (namely, comparison of different sources of data re: the same issue)? | No (0) | No (0) | Yes (1) | No (0) | No (0) |
| 12. Did triangulation produce convergent conclusions? | No (0) | No (0) | Yes (1) | No (0) | N/A |
| 13. If “no,” was this adequately explained? | N/A | Yes (1) | N/A | Yes (1) | No (0) |
| 14. Were the study’s findings generated by more than one analyst? | No (0) | Yes (1) | Yes (1) | No (0) | Yes (1) |
| Findings/Results | |||||
| 15. Is there a clear statement of the findings? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 16. Are the study’s findings discussed in terms of their relation to the research questions posed? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 17. Do the findings appear credible? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 18. Are sufficient data presented to support the findings? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 19. Are potential researcher biases taken into account? | No (0) | No (0) | No (0) | No (0) | No (0) |
| 20. Are conclusions explicitly linked with exhibits of data? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| Research value | |||||
| 21. Do the study’s findings contribute to the current knowledge base? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 22. Can the findings reasonably be expected to inform current practices or policies? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 23. Are these contributions discussed by the authors? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 24. Did the authors identify new research areas? | No (0) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 25. Did the authors discuss how the research findings could be used and for what populations? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| 26. Was enough descriptive detail included to allow readers to make their own judgments about potential transferability to other settings? | Yes (1) | Yes (1) | Yes (1) | Yes (1) | Yes (1) |
| Study Assessment Question | Arora et al. [8] | Robinson et al. [13] | Taylor [20] | Qui and Ni [29] | Soh [30] | Kavathe et al. [16] | Jones et al. [27] | Selikowitz and Holst [9] | Williams et al. [10] | Ghiabi et al. [21] | Cruz et al. [28] | Kay et al. [22] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Is the research question clearly stated? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Are the criteria for selecting the sample clearly defined? | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Is the method of recruitment clear? | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4. Are the characteristics of the sample adequately defined? | Yes | Yes | No | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 5. Is the final sample adequate and appropriate? | No | Yes | No | Yes | No | No | Yes | No | Yes | No | Yes | Yes |
| 6. Was the method for collecting data adequately described? | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7. Was the data collected systematically? | Yes | Yes | U/D | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8. Was the relationship between the researcher and the participant explicit? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Were the methods used in the data analysis appropriate and designed to minimize bias? | Yes | Yes | No | Yes | No | Yes | No | Yes | Yes | N/A | Yes | N/A |
| 10. Is evidence provided in support of the analysis? | Yes | Yes. | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 11. Is there evidence of efforts to establish validity? | Yes | Yes | No | Yes | No | No | No | No | Yes | Yes | Yes | N/A |
| 12. Were the conclusions drawn appropriate given the results? | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
References
- Jin, L.J.; Lamster, I.B.; Greenspan, J.S.; Pitts, N.B.; Scully, C.; Warnakulasuriya, S. Global burden of oral diseases: Emerging concepts, management and interplay with systemic health. Oral Dis. 2015, 22, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Cicciu, M.; Fiorillo, L.; Matarese, G. Association between odontoma and impacted teeth. J. Craniofac. Surg. 2017, 28, 755–758. [Google Scholar] [CrossRef] [PubMed]
- Mattos, M.G.; Fernandez, C.A.; Masterson, D.; Maia, L.C.; Neves, A.A. Is the caregivers’ oral health related to dental caries in children or adolescents? A systematic review. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. The World Oral Health report 2003: Continuous improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2008, 31, 3–24. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, G.; Cordasco, G.; Rotondo, F.; Crupi, A.; Ramaglia, L. Anticoagulant therapy in patients undergoing dental interventions: A critical review of the literature and current perspectives. Minerva Stomatol. 2015, 64, 21–46. [Google Scholar] [PubMed]
- Kandelman, D.; Arpin, S.; Baez, R.J.; Baehni, P.C.; Petersen, P.E. Oral health care systems in developing and developed countries. Periodontol. 2000 2012, 60, 98–109. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. What Is the Burden of Oral Disease? Available online: http://www.who.int/oral_health/disease_burden/global/en/ (accessed on 12 July 2018).
- Arora, G.; Mackay, D.F.; Conway, D.I.; Pell, J.P. Ethnic differences in oral health and use of dental services: Cross-sectional study using the 2009 adult dental health survey. BMC Oral Health 2017, 17, 1. [Google Scholar] [CrossRef]
- Selikowitz, H.S.; Holst, D. Dental health behavior in a migrant perspective: Use of dental services of Pakistani immigrants in Norway. Community Dent. Oral Epidemiol. 1986, 14, 297–301. [Google Scholar] [CrossRef]
- Williams, S.A.; Summers, R.M.; Ahmed, I.A.; Prendergast, M.J. Caries experience, tooth loss and oral health-related behaviours among Bangladeshi women resident in West Yorkshire, UK. Community Dent. Health 1996, 13, 150–156. [Google Scholar]
- U.S. Census Bureau. American Community Survey; U.S. Census Bureau: Silver Hill, MD, USA, 2018.
- Australian Bureau of Statistics. 3412.0—Migration, Australia, 2016–17; Australian Bureau of Statistics: Canberra, Australia, 2018.
- Robinson, P.G.; Bhavnani, V.; Khan, F.A.; Newton, T.; Pitt, J.; Thorogood, N.; Gelbier, S.; Gibbons, D. Dental caries and treatment experience of adults from minority ethnic communities living in the South Thames Region, UK. Community Dent. Health 2000, 17, 41–47. [Google Scholar]
- Riggs, E.; Gussy, M.; Gibbs, L.; Van Gemert, C.; Waters, E.; Kilpatrick, N. Hard to reach communities or hard to access services? Migrant mothers’ experiences of dental services. Aust. Dent. J. 2014, 59, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Lamb, C.E.F.; Whelan, A.K.; Michaels, C. Refugees and oral health: Lessons learned from stories of Hazara refugees. Aust. Health Rev. 2009, 33, 618–627. [Google Scholar] [CrossRef] [PubMed]
- Kavathe, R.; Islam, N.; Zanowiak, J.; Wyatt, L.; Singh, H.; Northridge, M.E. Building capacity in the Sikh Asian Indian community to lead participatory oral health projects. Prog. Community Health Partnersh. 2018, 12, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Sytematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Kennelly, J. Methodological approach to assessing the evidence. In Reducing Racial/Ethnic Disparities in Reproductive and Perinatal Outcomes: The Evidence from Population-Based Interventions; Handler, A., Kennelly, J., Peacock, N., Eds.; Springer: Boston, MA, USA, 2011; pp. 7–19. [Google Scholar]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Taylor, W. Dietary patterns, dental awareness and dental caries in the Asian community. Dent. Health 1983, 22, 5–6. [Google Scholar]
- Ghiabi, E.; Matthews, D.C.; Brillant, M.S. The oral health status of recent immigrants and refugees in Nova Scotia, Canada. J. Immigrant Minority Health 2014, 16, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Kay, E.J.; Shaikh, I.; Bhopal, R.S. Dental knowledge, beliefs, attitudes and behaviour of the Asian community in Glasgow. Health Bull. 1990, 48, 73–80. [Google Scholar]
- Croucher, R.; Sohanpal, R. Improving access to dental care in East London’s ethnic minority groups: Community based, qualitative study. Community Dent. Health 2006, 23, 95–100. [Google Scholar]
- Williams, S.A.; Gelbier, S. Access to dental health? An ethnic minority perspective of the dental services. Health Educ. J. 1988, 47, 167–170. [Google Scholar] [CrossRef]
- Newton, J.T.; Thorogood, N.; Bhavnani, V.; Pitt, J.; Gibbons, D.E.; Gelbier, S. Barriers to the use of dental services by individuals from minority ethnic communities living in the United Kingdom: Findings from focus groups. Primary Dent. Care 2001, 8, 157–161. [Google Scholar] [CrossRef]
- Ahmed, F.; Abel, G.A.; Lloyd, C.E.; Burt, J.; Roland, M. Does the availability of a South Asian language in practices improve reports of doctor-patient communication from South Asian patients? Cross sectional analysis of a national patient survey in English general practices. BMC Fam. Pract. 2015, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.V.; Srivastava, R.P.; Walsh, T.F. Oral hygiene practices in a group of Asian females. Dent. Health 1987, 26, 5–7. [Google Scholar]
- Cruz, G.D.; Chen, Y.; Salazar, C.R.; Le Geros, R.Z. The association of immigration and acculturation attributes with oral health among immigrants in New York city. Am. J. Public Health 2009, 99, S474–S480. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Ni, H. Utilization of dental care services by Asians and native Hawaiian or other Pacific Islanders: United States, 1997–2000. Adv. Data 2003, 336, 1–11. [Google Scholar]
- Soh, G. Racial differences in perception of oral health and oral health behaviours in Singapore. Int. Dent. J. 1992, 42, 234–240. [Google Scholar] [PubMed]
- Riggs, E.; Gussy, M.; Gibbs, L.; Gemert, C.; Waters, E.; Priest, N.; Watt, R.; Renzaho, A.M.N.; Kilpatrick, N. Assessing the cultural competence of oral health research conducted with migrant children. Community Dent. Oral Epidemiol. 2014, 42, 43–52. [Google Scholar] [CrossRef] [PubMed]
- The United Nations. International Migration Report 2015; The United Nations: New York, NK, USA, 2016; pp. 1–3. [Google Scholar]
- Ram, S. Indians in England: Why did they emigrate? Popul. Geogr. 1987, 9, 37–44. [Google Scholar]
- Office of National Statistics. 2011 Census: Key Statistics and Quick Statistics for Local Authorities in the United Kingdom; Office of National Statistics: Newport, UK, 2013.
- Lukacs John, R. Gender differences in oral health in South Asia: Metadata imply multifactorial biological and cultural causes. Am. J. Hum. Biol. 2011, 23, 398–411. [Google Scholar] [CrossRef]
| Search Terms |
|---|
| Oral health OR |
| Dental Health OR |
| Oral hygiene OR |
| Dental hygiene OR |
| Oral Care OR |
| Dental Care OR |
| AND |
| South Asia * OR |
| India * OR |
| Sri Lanka * OR |
| Nepal * OR |
| Bangladesh * OR |
| Bhutan * OR |
| Afghanistan * OR |
| Maldiv * OR |
| Pakistan * OR |
| AND |
| Migra * OR |
| Immigra * OR |
| Emmigra *OR |
| Ethnic * OR |
| Minorit * |
| AND |
| Knowledge OR |
| Attitude OR |
| Practice OR |
| Belief OR |
| Understanding OR |
| Behavior OR |
| Habit |
| First Author, Pub. Year (Ref.) | Study Population (Which Countries Included as South Asian) | The Country the Study Was Conducted in (South Asians Were Migrants or Ethnic Group Within This Region, State or Country) and Period of Data Collection | Number of Adults in the Sample. Stratified by South Asian Region and Age Group | Methodology | Aim of the Study | The Outcome That the Study Was Assessing and Whether They Stratified by Asian Status | Brief Description of Differences of What They Found Between the South Asian Groups Studied |
|---|---|---|---|---|---|---|---|
| Williams 1988 [24] | Bangladeshi and Pakistani as South Asians | London, April–June 1987 | N = 100 total N = 50 Bangladeshi N = 50 Pakistani Age group—not mentioned | Interviews with 20 focus groups with 5 mothers in each. | To explore the ways to improve the consumption of dental services by Muslim mothers from Bangladesh and Pakistan. | Awareness regarding the availability of services, barriers to the use of services, and establish possible ways to improve the availability of services for Muslim mothers in the UK. Results not described according to the country of birth. | Muslim mothers were well aware of the services available. Presence of a symptom was a requisite for the majority of mothers to visit a dentist and less than half recognized the significance of a regular check-up. Visiting a dentist was not the priority for Muslim mothers. Fear, lack of trust, and communication difficulties were identified as potential barriers to the uptake of services. Preference for female dentists was highlighted by the mothers. Lack of required knowledge regarding oral health was prevalent in all the groups. An absence of cultural sensitivity was emphasized. |
| Newton 2001 [25] | Out of seven ethnic groups they included, Pakistani, Indian, and Bangladeshi as South Asians | South Thames region, UK | N =193 total N = 3 Pakistani groups N = 4 Indian groups N = 5 Bangladeshi groups. Age group—not mentioned | 28 focus group interviews with each representing a particular ethnic group. | Identification of barriers for the utilization of dental services among various ethnic group residing in the UK through a qualitative approach. | Discussion and presentation of views around various pre-identified barriers such as language, trust, cost, anxiety, and cultural issues between various ethnic groups. | Language stated as a major barrier by nearly half of the participants from Bangladeshi, Pakistani, and Indian origin. Bangladeshi and Pakistani participants recommended that translation facilities should be available as one of the strategies for improving the uptake of services. Lack of trust for the dentist was cited as a major issue by Bangladeshi, Pakistani, and Indian participants. The cost was also stressed but to a lesser extent, Bangladeshi, Pakistani, and Indian participants demanded a change in the payment system. Preference for a woman dentist was observed among Bangladeshi women. Lack of cultural sensitivity by the dentist was mentioned by Indian participants. Concerns of hygiene were identified only by Pakistani and Chinese/Vietnamese groups. |
| Croucher 2006 [23] | Out of three, Indian and Bangladeshi as South Asians | East London, July–August 2001 | N = 68 total N = 9 Indian N = 13 Bangladeshi Age group = 18–40 | Rapid participatory approach, 12 focus groups who had in-depth discussions | To ascertain and compare the barriers for the use of dental services by adults in specific ethnic groups vs. the general population | Insights regarding the structure of dental care, barriers to use services, and proposals to improve access by the ethnic groups who conversed. | The long waiting list, dentist being overworked, and lengthy treatments were acknowledged by Indians whereas distance to access a dentist was acknowledged by Bangladeshi. Cost and lack of knowledge of average prices of various treatments were the other concerns specified by Indians. Dentist of the same gender was not a great requirement by an Indian woman as compared to a Bangladeshi woman. Recommendation of staff having training in local community languages was quoted by a Bangladeshi woman. Perception of “clean practice” was prevalent among the participants. Having whiskey was preferred than visiting a dentist by an Indian man to ease the dental pain. |
| Riggs 2014 [14] | Pakistani as South Asians | Australia | N = 115 total N = 3 focus groups (20) Pakistani. Individual interviews with 4 Pakistani women. Age group—not mentioned | Participatory research approach focus group (11) and individual (7) in-depth interviews. | To present the experiences detailed by Iraqi, Lebanese, and Pakistani women in dental service utilization for themselves and their children in Melbourne, Australia. | Iraqi, Lebanese, and Pakistani women were interviewed in depth for their experiences and barriers in accessing dental services in Melbourne. Participants were further probed for their oral health behaviors. | The majority did not access dentists for preventive purposes but only for treatment. Pakistani women preferred to pursue treatments in Pakistan as they believe the service would be provided by a qualified doctor at cheaper prices and there would be no language barriers. Pakistani perceive the restorative treatments as more expensive, so were more inclined to extractions. Lack of knowledge of the type of oral hygiene aid was evident as miswak was still used by some of the participants. Pakistani women felt being judged on the basis of their culture and country of origin. Halal certification was stated as one of the prerequisites for the health professional to treat them. |
| Lamb 2009 [15] | Afghanistan refugees as South Asians | Australia, July–August 2001. | N = 8 total Age group > 20 years | Semi-structured in-depth interviews | To describe the oral health understandings presented by the group of Afghan refugees. | Group of Afghan refugees were questioned for their views on oral health risk factors, the motivation for oral care, access to a dentist, pain management, and oral health education. | Numerous risk factors for oral health were acknowledged among refugees like smoking chelam, sucking naswar, breaking nuts, and stress of survival. Oral hygiene was stated as a requirement for religious purposes with some mentioned using miswak three times a day. Different oral hygiene aids were used by the study population such as salt, fingers, toothpaste, and toothbrush. Home remedies (cloves, aspirin yeast, takhak, salt water rinse) were preferred more to ease pain then to visit a dentist. Hazaras were also found to carry out extractions by themselves under unhygienic conditions. The existence of belief that the filling does not work was found. |
| First Author, Pub. Year (Ref.) | Study Population (Which Countries Included as South Asian) | The Country the Study Was Conducted in (South Asians Were Migrants or Ethnic Group Within This Region, State or Country) and Period of Data Collection | Number of Adults in the Sample. Stratified by South Asian Region and Age Group | Survey Instrument | Aim of the Study | The Outcome That the Study Was Assessing and Whether They Stratified by Asian Status | Brief Description of Differences of What They Found Between the South Asian Groups Studied |
|---|---|---|---|---|---|---|---|
| Arora 2017 [8] | Out of five groups, they included Indian and combined Pakistani/Bangladeshi as two groups as South Asians | UK, study conducted in 2009 to 2010 | N = 10,435 total N = 272 Indians N = 165 Pakistani/Bangladeshi Age group > 16 | Validated instrument Adult Dental Health Survey (ADHS) | To examine oral health differences among different ethnic groups. Really trying to ascertain whether the lifestyle factors and use of dental services contribute to the oral health disparities. | They conducted a logistic regression analysis of clinical outcomes. They presented descriptive tables on behaviors such as frequency of teeth cleaning, visits to dentist, and use of dental hygiene products by various ethnic groups. They also depicted the differences in the perception of oral health among different ethnic groups. | South Asians were less likely to consume sweets, cakes, and fizzy drinks but more likely to add sugar to hot drinks and this pattern was similar among all South Asian subgroups. A higher proportion (71.5%) of Pakistanis/Bangladeshis than Indians (64.2%) reported brushing twice a day. However, 20.4% of Pakistanis/Bangladeshis and 19.4% of Indians visit the dentist only if they have a symptom. Majority of South Asians do not use other oral hygiene products. |
| Robinson 2000 [13] | Out of seven groups, Pakistani, Indian, and Bangladeshi represented three groups as South Asians | South Thames, UK | N = 1113 total N = 123 Pakistani N = 190 Indian N = 78 Bangladeshi Age group > 16 | Questionnaire | To assess the oral health status and its determinants among various ethnic groups. | Descriptive statistics of oral health-related behaviors such as daily cleaning of teeth, the frequency of visit to the dentist, and sugar intake, were stated according to various ethnic groups. | A higher percentage of Indians reported cleaning teeth daily (98.9%) and visiting the dentist annually (99.5%) followed by Bangladeshi and Pakistani. Sugar exposure was almost comparable among all the groups. |
| Taylor 1983 [20] | Indian, Pakistani, and Bangladeshi as South Asians | Britain | N = 231 total N = 109 adults N = 45 Bangladeshi N = 34 Indian N = 30 Pakistan Age group > 14 | Questionnaire | To explore the number of aspects in regard to dental awareness, dietary patterns, and dental care amongst the Asian community. | Descriptive information of the population is provided according to various variables such as dietary patterns, tooth brushing, visits to a dentist, and dental awareness, and tabulated according to the country of origin. | Pakistani and Bangladeshi had high mean sugar intake score. Very few individuals among all the groups reported twice brushing as a habit. Majority of Pakistanis and Indians visited the dentist when in pain. |
| Qui 2003 [29] | Out of 8 groups, Asian Indians were only representing South Asians | The United States during 1997–2000 | N = 110,844 total N = 798 Asian Indians Age group > 18 | National Health Interview Surveys (NHISs) | To present the national estimates of dental service utilization by various ethnic groups. | Estimates of dental care utilization were provided for Asians and for Asian Indians. Furthermore, the percentage of Asians who had visited the dentist in the past year by various characteristics was also available, but not stratified for Asian Indians. | Asian Indians (8.1%) had never visited the dentist. Compared to other groups, d Asian Indians were least likely to visit the dentist. |
| Soh 1992 [30] | Out of three, Indians were only group of South Asians | Singapore | N = 446 total N = 34 Indian Age group > 18 | Telephone interview survey | To examine the racial difference in knowledge of preventive measures for oral health and use of the preventive services. | Chi-squared test was used to assess the racial differences for the knowledge and the behaviors of oral health such as tooth brushing, flossing, regular check-up, fluoride, and dental sealants. | Importance of flossing was less evident for Indians (64.7%) compared to other groups. Dental check-ups were considered unnecessary for the majority of Indians (88.9%) with no dental care. All Indians were found to appreciate the benefits of effective brushing and had good knowledge of the role of fluoridated toothpaste in oral health. |
| Kavathe 2018 [16] | Out of four groups, Indian and Pakistani as South Asians | New York, USA | N = 169 total N = 165 Indian N = 4 Pakistani Age group > 18 | A validated survey instrument adapted from the National Health Interview Survey, National Health and Nutrition examination survey, Behavioral Risk Factor Surveillance system, and New York City Community Health Survey. | To describe how oral health was identified as a priority for Sikh Asian Indian population by the United Sikhs through the community needs and resource assessment (2010) conducted for diabetes prevention. Furthermore, how they used it to develop a curriculum for the population. | Descriptive statistics were provided from community need and resource assessment to form the basis for oral health priority (2010) such as frequency of dental check-ups. Further, results of a descriptive study of oral conditions (2013) such as availability of dental insurance in the population and frequency of visiting the dentist were presented. Results not categorized by the place of birth. | According to community needs and resource assessment (2010), the majority (57%) never had a screening or check-up by the dentist. Descriptive study (2013), higher percentage (80.2%) were without dental insurance, a regular dentist (64.6%) or needed dental care (72.9%). |
| Jones 1987 [27] | Only Indian as South Asians | England | N = 231 total Age group = 15–59 | Structured questionnaire | To determine the oral hygiene practices among migrant Asian females of Indian origin. | Oral hygiene practices such as agents used for tooth cleaning, interdental, mouth, and tongue cleaning were determined and categorized according to age group. | A vast number of females reported the use of toothpaste (68.4%) and a toothbrush (67.5%) with the majority in the age group (20–29 years). Few (17.3%) used their finger and 1.3% used datun. Only 6.9% were found using floss as an interdental aid. Tooth cleaning appeared in only 24.2% of the sample. |
| Selikowitz 1986 [9] | Only Pakistani as South Asians | Norway, 1982 | N = 96 total Age group > 20 | Structured questionnaire | To observe the pattern of utilization of dental services among Pakistani migrants with regards to migration variables. | Statistical analysis was employed (Chi-squared test) to investigate the differences in utilization of services by the population according to various variables such as the number of years in Norway, knowledge of causes of oral diseases, and belief about consequences of dental diseases. | Utilization of dental services was observed to be similar among all the age groups. Immigrants who lived in Norway for 1–6 years were found to use more services compared to those with more than 9 years in Norway, but the difference was not statistically significant. Those who believed (55.0%) that dental diseases are dangerous were in the category of high utilization of services compared to those who did not believe (p < 0.05). |
| Williams 1996 [10] | Only Bangladeshi as South Asians | West Yorkshire, UK | N = 246 total Age group > 25 years. | Interview | To assess the oral health status of Bangladeshi-born women and the relationship with various social, demographic, and behavioral variables. | Comparison of Bangladeshi women socio-demographic variables with oral hygiene practices categorized into traditional (finger, chewing stick, soot, tobacco powder), conventional (toothpaste and toothbrush) and combination category and further with dental visiting habits. | A large number of participants were observed to follow the traditional method of tooth cleaning and never visited a dentist. Years lived in the UK was found to be positively associated with dental attendance but not associated with practices. Traditional methods were more prevalent among the ones who never visited the dentist (p < 0.01). |
| Ghiabi 2013 [21] | Only Bhutanese as South Asians | Nova Scotia, Canada | N = 96 total N = 41 Bhutanese Age group = 18–67 years. | 2008 Canadian Health Measures Survey (oral health module) | To describe the findings of oral health survey among the group of recent migrants and Bhutanese refugees in Canada. | Self-reported oral health, including the frequency of oral care such as tooth brushing, flossing, and dental visits were compared between Bhutanese refugees and other migrants in Canada. | Significant numbers of Bhutanese never floss (95.1%) and visit the dentist only in an emergency (53.7%). None of the refugees had dental insurance, however, a higher proportion was found to brush twice a day. |
| Cruz 2009 [28] | The only group as South Asians were Indian | New York, 1996–2001 | N = 1318 total N = 196 Indian Age group = 18–65 years | Validated structured questionnaire | To ascertain the relationship of oral health of immigrants with various demographic and risk factors. | Descriptive analysis of the study population sub-classified by ethnic group (Asian Indian) presented with regard to frequency of brushing, flossing, visiting a dentist, length of stay in the USA, oral health knowledge, and attitude score. | About 84.7% Asian Indians were described to have dental insurance, daily brushing practice (95.9%), and high knowledge and attitude score (58.7% and 79.1%, respectively). Around 27% visited the dentist once a year. |
| Kay 1990 [22] | Indian were only group as South Asians | Glasgow, UK | N = 69 total Age group = 18–68 years. | Semi-structured questionnaire | To explore the knowledge, attitude, and behavior with regards to oral health among Asians residing in Glasgow. | Sample assessed for their knowledge (steps to take to reduce caries, deleterious effects of sweets on teeth and related to fluoride), attitude (reasons, cost, and frequency to visit dentist) and behavior (diet, oral hygiene, and dental health). | Harmful effects of sweets were appreciated by 64% of the sample whereas 66% consume the cariogenic diet. Knowledge in relation to fluoride was low (63%) and the population only received fluoride through the paste. All respondents acknowledged the importance of oral health but the majority (48%) mentioned cost as a potential barrier and 44 participants attended the dentist when in trouble. Around 41% of the population was found to brush twice and 68% rinsed their mouth after every meal. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batra, M.; Gupta, S.; Erbas, B. Oral Health Beliefs, Attitudes, and Practices of South Asian Migrants: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 1952. https://doi.org/10.3390/ijerph16111952
Batra M, Gupta S, Erbas B. Oral Health Beliefs, Attitudes, and Practices of South Asian Migrants: A Systematic Review. International Journal of Environmental Research and Public Health. 2019; 16(11):1952. https://doi.org/10.3390/ijerph16111952
Chicago/Turabian StyleBatra, Mehak, Sabrina Gupta, and Bircan Erbas. 2019. "Oral Health Beliefs, Attitudes, and Practices of South Asian Migrants: A Systematic Review" International Journal of Environmental Research and Public Health 16, no. 11: 1952. https://doi.org/10.3390/ijerph16111952
APA StyleBatra, M., Gupta, S., & Erbas, B. (2019). Oral Health Beliefs, Attitudes, and Practices of South Asian Migrants: A Systematic Review. International Journal of Environmental Research and Public Health, 16(11), 1952. https://doi.org/10.3390/ijerph16111952





