Involving Patients and Families in the Analysis of Suicides, Suicide Attempts, and Other Sentinel Events in Mental Healthcare: A Qualitative Study in The Netherlands
Abstract
1. Introduction
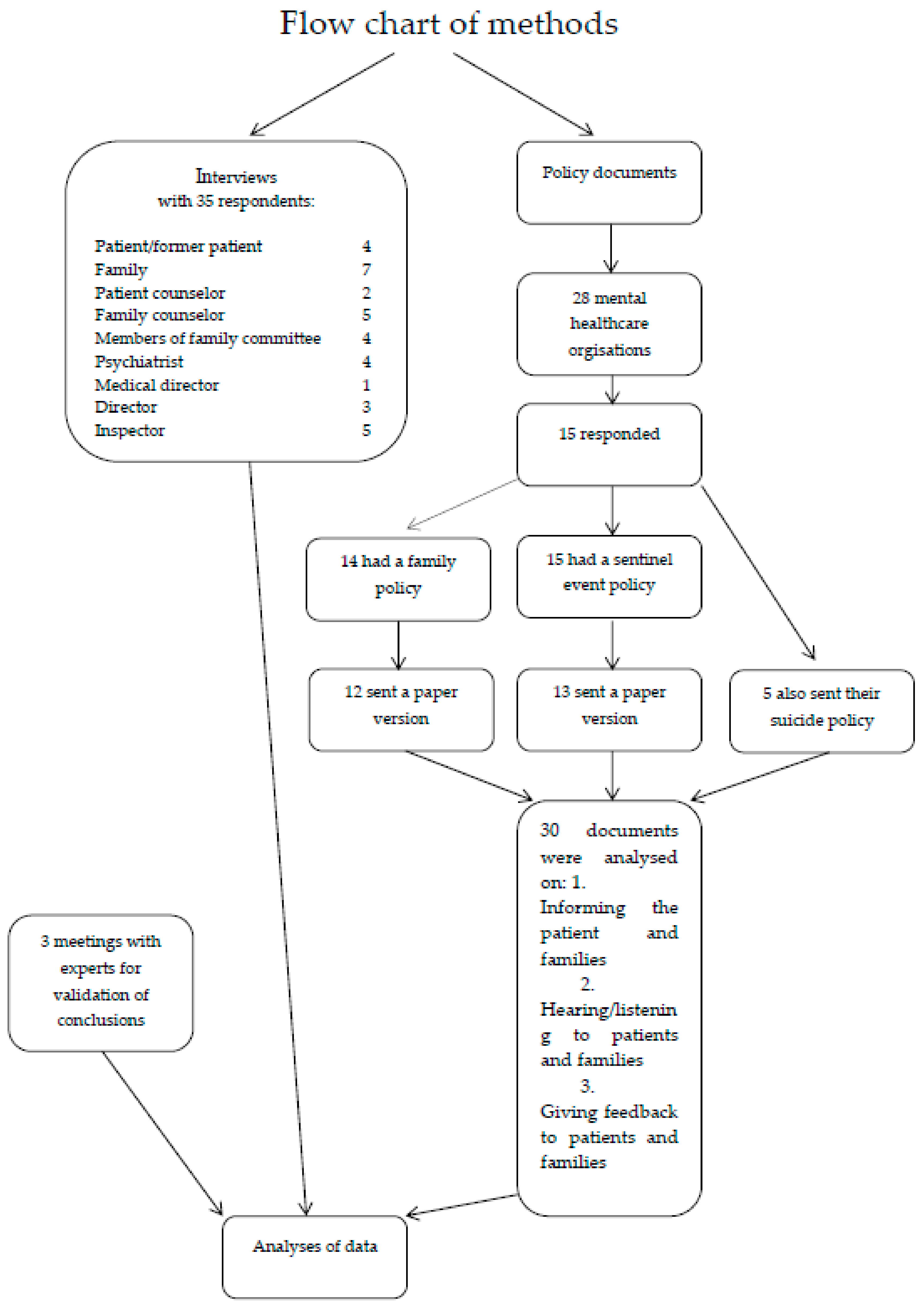
2. Materials and Methods
2.1. Policy Documents
2.1.1. Data Collection
2.1.2. Analyses of Policy Documents
2.2. Interviews
2.3. Medical Ethical Assessment
3. Results
3.1. Policy Documents
3.1.1. Family Policy
“(Care organization) attaches great importance to the contribution of the client, legal representative, or relatives involved in establishing facts and describing events.”(Family policy document of a mental healthcare organization)
“(Care organization) endorses the fact that the bottlenecks and wishes expressed by family/close relatives can also improve care.”(Family policy document of a mental healthcare organization)
3.1.2. Sentinel Event Policy
3.1.3. Suicide Protocols
“Most contacts with family logically take place in the first week, for example because employees attend the funeral or cremation of their client (in consultation with the family). It is important to schedule a conversation with family after six to eight weeks. In this interview, the results of the (first) internal suicide evaluation can be discussed with family and there is the possibility for relatives to ask questions about the treatment and counseling of the deceased client. The staff may also have questions for the next of kin that they would appreciate answers to.”(Suicide protocol of a mental healthcare organization)
3.2. Interviews
- -
- involvement during treatment;
- -
- definition of a sentinel event;
- -
- limited involvement in practice;
- -
- reasons in favor of involvement during sentinel event analyses; and
- -
- reasons against involving patients and families in sentinel event analyses
3.2.1. Involvement during Treatment
“So she had compulsive thoughts. I noticed that straight away in her non-verbal communication. Actually in all sorts of small things. Then they upped her medication and valium. I said, ‘This isn’t going to help her enough. (...) I say, ‘you can keep her here, I’m not taking her home anymore, I’m no longer taking responsibility’. Then she got a psychosis on the spot.”(Mother of a patient)
“Yeah, and I’d be stamping and everything like that, and then they grabbed me: ‘Go to your room’. A man and a woman. The carers said, ‘And now to your room. If you don’t stop, you can’t leave your room for eight hours, or then you’ll get a jab or something,’ whatever. I thought, ‘Well, I’m pretty fed up with it.’ So I secretly got blankets, on my day off, I tied them all together. And the window wasn’t supposed to open, but it was one of the newfangled ones and I’d seen what to do. And when I’d opened it earlier, they’d seen that and pulled it closed. So anyway, I pulled that window open, blankets knotted together: well it worked. Normally I’m scared of heights, but not then—I just didn’t feel afraid. It was just tunnel vision. Then I went down, but those blankets came apart, so then I fell, on a platform luckily, with parking spaces beneath, a couple of stories high, not to the ground, (...) then I fell on my back.”(Patient 1)
3.2.2. Definition of a Sentinel Event
“...but he (the patient) doesn’t want that (coercion measures), so he’s less afraid of the sentinel event than the intervention to prevent it.”(Patient counselor)
“So the jargon terms that we use, (...) certainly for people who are in mourning, are obviously incomprehensible. They often only trigger more anger and combativeness. Yes, that’s very difficult.”(Inspector)
“But we also do it when there’s a lot of fuss being made.”(Care institution director)
3.2.3. Limited Involvement in Sentinel Event Analysis in Practice
In this quote, it can clearly be seen how the family is left out at the moment details start to matter. While respondents do recognize that the perspective of family and patients can change the scope of analysis and the lessons learned, in several interviews respondents note that the perspective of patients and families not always adds up nicely with the perspective of other actors. They can also conflict. In such a case, our study shows that the contribution of family or patients quickly becomes devalued and questioned by healthcare providers or inspectors. When this happens patients and families are considered for example to be ‘overwhelmed by emotions’ (medical director).“Then we draft the improvement measures, but at that point the family is no longer involved. At least everything (the event analysis) is done. No, the points for improvement are just outlines. If more points turn up, they’ll be in the report. And then worked out in detail. That’s without the family, but they can say what they think of the broader outlines.”(Care institution director)
“So that’s what we do. But what we’ve recently discussed, the feedback for example on what has come from the analysis to the family, well, we don’t yet report that to them. And that’s the question, whether it might be useful to report it back to the family. Sometimes when the family really insist on it, but we don’t report that to them as a matter of course (...) And I think that’s the next step, that we also involve the family or patient in the evaluation and that we also give them the feedback, what came out of it (the evaluation), also to family and friends.”(Director)
3.2.4. Reasons in Favor of Involvement during Sentinel Event Analyses
“It’s also a kind of duty for the care organization, to provide aftercare to the family. (...) To give them the opportunity to tell their story again, or to hear how everything happened. So that they can learn to cope with what has happened. Yes, in that sense it’s an extra reason for paying attention to the family and relatives.”(Inspector)
“(...) you need that family for the biography and the history. (...) The family is (therefore) indispensable for a proper analysis of the event, otherwise you’re only looking at the care provided and that’s the major problem, for the crisis services too. (…). Otherwise you’re taking snapshots and not seeing the movie.”(Inspector)
“… Because you’ve seen a few reports on sentinel events and you know you’ll get answers based on the questions you put in. If you make your analysis narrow enough, nothing seems to have gone wrong.”(Family counselor)
“It’s better to share the real story with each other than to follow formal pathways. That’s pretty much our approach.”(Family counselor)
3.2.5. Reasons against Involving Patients and Families in Sentinel Event Analyses
“You often see it at the actual funeral. Because if someone was admitted here, everyone will have been very involved with the patient. So if they commit suicide, we always ask whether we should go to the funeral or not. And some families say that they are at any rate glad that they were helped and it’s a shame it went wrong, but you’re welcome to come. But of course there are families who do say, ‘this should never have happened. We never want to see you again’. So (...) how families react can be very different.”(Psychiatrist)
“I just think later, after waiting a few years first until it all… It really takes a few years before the psychosis is really gone; it‘s not right away, but I think a few years later, in my case five years later, that it’s good to think about it again.”(Patient)
“(...) PRISMA (Prevention and Recovery Information System for Monitoring and Analysis, a method of root cause analysis) is an instrument mainly for seeing if mistakes were made in the organization. So very often you have patient-related factors as a base cause an, well, whether they were manic or angry doesn’t really matter. So from the patient’s perspective, a PRISMA sounds a bit brutal and is irrelevant.”(Psychiatrist)
R1: “Yeah, admitting everything that went wrong. And being able to investigate how and why properly.”R2: “Yes, that’s very difficult, isn’t it? How can you be transparent if there‘s a family and you’re discussing it afterwards? And that someone wants to be open and wants to search, you do not. That’s way too fraught. Especially in events like these.”(Medical director and psychiatrist)
“So the inspectorate only wants to know if the patient is the victim. Whereas in ninety-nine out of a hundred cases, the staff member is the victim.”(Medical director)
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
References
- Etchegaray, J.M.; Ottosen, M.J.; Burress, L.; Sage, W.M.; Bell, S.K.; Gallagher, T.H.; Thomas, E.J. Structuring patient and family involvement in medical error event disclosure and analysis. Health Aff. 2014, 33, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Grissinger, M. Including Patients on Root Cause Analysis Teams: Pros and Cons. Pharm. Ther. 2011, 36, 778–779. [Google Scholar]
- Leistikow, I. Prevention Is Better than Cure: Learning from Adverse Events in Healthcare; CRC Press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Leistikow, I.; Mulder, S.; Vesseur, J.; Robben, P. Learning from incidents in healthcare: The journey, not the arrival, matters. BMJ Qual. Saf. 2017, 26, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Vincent, C.A.; Coulter, A. Patient safety: What about the patient? Qual. Saf. Health Care 2002, 11, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Kok, J.; Leitsikow, I.; Bal, R. Patient and family engagement in incident investigations: Exploring hospitals’ experiences and challenges. J. Health Serv. Res. Policy 2018. [Google Scholar]
- Van de Bovenkamp, H.M.; Trappenburg, M.J. The relationship between mental health workers and family members. Patient Educ. Couns. 2010, 80, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Van de Bovenkamp, H.M.; Trappenburg, M.J. Comparative review of family-professional communication: What mental health care can learn from oncology and nursing home care. Int. J. Ment. Health Nurs. 2012, 21, 366–385. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.A.; van de Bovenkamp, H.; Robben, P.B. Including citizens in institutional reviews: Expectations and experiences from the dutch healthcare inspectorate. Health Expect. 2015, 18, 1463–1473. [Google Scholar] [CrossRef] [PubMed]
- Netwerk Kwaliteitsontwikkeling GGz. Generieke Module: Samenwerking en Ondersteuning Naasten van Mensen met Psychische Problematiek; Netwerk Kwaliteitsontwikkeling GGz: Utrecht, The Netherlands, 2016. [Google Scholar]
- Barnes, L.S.; Ikeda, R.M.; Kresnow, M.J. Help-seeking behavior prior to nearly lethal suicide attempts. Suicide Life Threat. Behav. 2001, 32, 68–75. [Google Scholar] [CrossRef] [PubMed]
- New Zealand Guideline Group. The Assessment and Management of People at Risk of Suicide; New Zealand Guideline Group: Wellington, New Zealand, 2003. [Google Scholar]
- Bauer, R.; Spiessl, H.; Schmidt, T. Are there associations between caregiver information and suicidal behavior in psychiatric inpatients? Int. J. Psychiatry Clin. Pract. 2012, 16, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Expertisecentrum Informele Zorg. Familiebeleid in de GGZ: Van Moeilijkheden naar Mogelijkheden; NIZW Zorg/EIZ: Utrecht, The Netherlands, 2006. [Google Scholar]
- Expertisecentrum Mantelzorg. Familie in de GGZ: Partner in de Zorg. Van Beleid naar Uitvoering; Expertisecentrum Mantelzorg: Utrecht, The Netherlands, 2008. [Google Scholar]
- Rolland, J.S. Families, Illness, and Disability: An Integrative Treatment Model; Basic Books: New York, NY, USA, 1994. [Google Scholar]
- De Letselschaderaad. Gedragscode Openheid Medische Incidenten; Betere Afwikkeling Medische Aansprakelijkheid (GOMA); De Letselschaderaad: Den Haag, The Netherlands, 2012. [Google Scholar]
- Laarman, B.; van Schoten, S.; Friele, R. Nulmeting: Wet Kwaliteit, Klachten en Geschillen Zorg (Wkkgz); NIVEL: Utrecht, The Netherlands, 2016. [Google Scholar]
- Bouwman, R.; van Gennip, I.E.; Friele, R. Monitor Wkkgz: Stand van Zaken Implementatie “Effectieve en Laagdrempelige Klachten-en Geschillenbehandeling”; NIVEL: Utrecht, The Netherlands, 2017. [Google Scholar]
- Van Hemert, A.; Kerkhof, A.; de Keijser, J.; Verwey, B. Multidisciplinaire Richtlijn voor Diagnostiek en Behandeling van Suïcidaal Gedrag; Nederlandse Vereniging voor Psychiatrie/Nederlands Intstituut voor Psychologen/Trimbos Instituut: Utrecht, The Netherlands, 2012. [Google Scholar]
- European Commission. Reporting and learning subgroup of the European Commission PSQCWG. In Key Findings and Recommendations on Reporting and Learning Systems for Patient Safety Incidents across Europe; European Commission: Brussels, Belgium, 2014. [Google Scholar]
- IGZ. Jaarbeeld 2014; IGZ: Utrecht, The Netherlands, 2015. [Google Scholar]
- NZa. Marktscan ggz 2016; NZa: Utrecht, The Netherlands, 2017. [Google Scholar]
- Smith, E.R. Content analysis and narrative analysis. In Handbook of Research Methods in Social and Personality Psychology; Reis, H.T., Judd, C.M., Eds.; Cambridge University Press: New York, NY, USA, 2000; pp. 313–335. [Google Scholar]
- Charmaz, C. Constructing Grounded Theory, a Practical Guide through Qualitative Theory; Sage Publications: Londen, UK, 2006. [Google Scholar]
- Hsieh, H.F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Mayring, P. Qualitative content analysis. Forum Qual. Soc. Res. 2000, 1. [Google Scholar] [CrossRef]
- Netwerk Kwaliteitsontwikkeling GGz. Generieke Module Acute Psychiatrie; Netwerk Kwaliteitsontwikkeling GGz: Utrecht, the Netherlands, 2017. [Google Scholar]
- Nolan, P.; Dallender, J.; Soares, J.; Thomsen, S.; Arnetz, B. Violence in mental health care: The experiences of mental health nurses and psychiatrists. J. Adv. Nurs. 1999, 30, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Gifford, M.L.; Anderson, J.E. Barriers and motivating factors in reporting incidents of assault in mental health care. J. Am. Psychiatr. Nurses Assoc. 2010, 16, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Fitzsimons, B.; Cornwell, J. What can we learn from patients’ perspectives on the quality and safety of hospital care? BMJ Qual. Saf. 2018. [Google Scholar] [CrossRef] [PubMed]
- Bouwman, R.; Bomhoff, M.; Robben, P.; Friele, R. Is there a mismatch between the perspectives of patients and regulators on healthcare quality? A survey study. J. Patient Saf. 2017. [Google Scholar] [CrossRef] [PubMed]
- Vine, R.; Mulder, C. After an inpatient suicide: The aim and outcome of review mechanisms. Australas. Psychiatry 2013, 21, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Gillies, D.; Chicop, D.; O’Halloran, P. Root cause analyses of suicides of mental health clients: Identifying systematic processes and service-level prevention strategies. Crisis 2015, 36, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Woods, M.; Baker, R.; Charles, K.; Dawson, J.; Jerzembek, G.; Martin, G.; McCarthy, I.; McKee, L.; Minion, J.; Ozieranski, P.; et al. Culture and behaviour in the English national health service: Overview of lessons from a large multimethod study. BMJ Qual. Saf. 2014, 23, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Rutz, S.; van de Bovenkamp, H.M.; Buitendijk, S.; Robben, R.; de Bont, A. Inspectors’ responses to adolescents’ assessment of quality of care: A case study on involving adolescents in inspections. BMC Health Serv. Res. 2018, 18, 226. [Google Scholar] [CrossRef] [PubMed]
- Bouwman, R.; Bomhoff, M.; Robben, P.; Friele, R. Classifying patients’ complaints for regulatory purposes: A pilot study. J. Patient Saf. 2016. [Google Scholar] [CrossRef] [PubMed]
- Bouwman, R.; Bomhoff, M.; Robben, P.B.; Friele, R. Patients’ perspectives on the role of their complaints in the regulatory process. Health Expect. 2016, 19, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Friele, R.D.; Kruikemeier, S.; Rademakers, J.J.; Coppen, R. Comparing the outcome of two different procedures to handle complaints from a patient’s perspective. J. Forensic Legal Med. 2013, 20, 290–295. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Friele, R.D.; Sluijs, E.M. Patient expectations of fair complaint handling in hospitals: Empirical data. BMC Health Serv. Res. 2006, 6, 106. [Google Scholar] [CrossRef] [PubMed]
- Friele, R.D.; Sluijs, E.M.; Legemaate, J. Complaints handling in hospitals: An empirical study of discrepancies between patients’ expectations and their experiences. BMC Health Serv. Res. 2008, 8, 199. [Google Scholar] [CrossRef] [PubMed]
- Laarman, B.; Bomhoff, M.C.; Friele, R.; Akkermans, A.J.; Legemaate, J. OPEN: Open en Eerlijke Omgang na Klachten en Incidenten in Het Ziekenhuis. Schriftelijk Verslag van Project OPEN; NIVEL: Utrecht, The Netherlands, 2016. [Google Scholar]
| Year that policy was drawn up. |
| Year that policy was updated. |
| Frequency of review/evaluation of policy. |
| Sentinel event policy: the patient/family are informed. |
| Sentinel event policy: the experiences of the patient/family are listened to. |
| Sentinel event policy: the patient/family are given the opportunity to give feedback. |
| Family policy: the patient/family are informed. |
| Family policy: the experiences of the patient/family are listened to. |
| Family policy: family are given the opportunity to give feedback. |
| Suicide protocol (if included): the patient/family are informed. |
| Suicide protocol (if included): the experiences of the patient/family are listened to. |
| Suicide protocol (if included): the patient/family are given the opportunity to give feedback. |
| Category of Involving Patients and Families | Extent of Involvement in Family Policy (n = 12) | Extent of Involvement in Sentinel Event Policy (n = 13) | Extent of Involvement in Suicide Policy (n = 5) |
|---|---|---|---|
| 12 | 7 | 4 |
| 11 | 2 | 3 |
| 10 | 0 | 2 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouwman, R.; De Graaff, B.; De Beurs, D.; Van de Bovenkamp, H.; Leistikow, I.; Friele, R. Involving Patients and Families in the Analysis of Suicides, Suicide Attempts, and Other Sentinel Events in Mental Healthcare: A Qualitative Study in The Netherlands. Int. J. Environ. Res. Public Health 2018, 15, 1104. https://doi.org/10.3390/ijerph15061104
Bouwman R, De Graaff B, De Beurs D, Van de Bovenkamp H, Leistikow I, Friele R. Involving Patients and Families in the Analysis of Suicides, Suicide Attempts, and Other Sentinel Events in Mental Healthcare: A Qualitative Study in The Netherlands. International Journal of Environmental Research and Public Health. 2018; 15(6):1104. https://doi.org/10.3390/ijerph15061104
Chicago/Turabian StyleBouwman, Renée, Bert De Graaff, Derek De Beurs, Hester Van de Bovenkamp, Ian Leistikow, and Roland Friele. 2018. "Involving Patients and Families in the Analysis of Suicides, Suicide Attempts, and Other Sentinel Events in Mental Healthcare: A Qualitative Study in The Netherlands" International Journal of Environmental Research and Public Health 15, no. 6: 1104. https://doi.org/10.3390/ijerph15061104
APA StyleBouwman, R., De Graaff, B., De Beurs, D., Van de Bovenkamp, H., Leistikow, I., & Friele, R. (2018). Involving Patients and Families in the Analysis of Suicides, Suicide Attempts, and Other Sentinel Events in Mental Healthcare: A Qualitative Study in The Netherlands. International Journal of Environmental Research and Public Health, 15(6), 1104. https://doi.org/10.3390/ijerph15061104





